國立交通大學
機械工程學系
碩士論文
下顎前置型口內止鼾裝置之機構設計
A Study on the Mechanism Design of the
Mandibular Advancement Device
研究生:李翊猷
指導教授:洪景華 教授
共同指導教授:林聰穎 教授
下顎前置型口內止鼾裝置之機構設計
A Study on the Mechanism Design of the
Mandibular Advancement Device
研 究 生:李翊猷 Student:
Yi-Yu
Lee
指導教授:洪景華 林聰穎
Advisor: Chinghua Hung, Tsung-Yin Lin
國立交通大學
機械工程學系
碩士論文
A Thesis
Submitted to Department of Mechanical Engineering
College of Engineering
National Chiao Tung University
in Partial Fulfillment of the Requirements
for the Degree of
Master
in
Mechanical Engineering
June 2007
下顎前置型口內止鼾裝置之機構設計
研究生:李翊猷 指導教授:洪景華 林聰穎 國立交通大學機械工程學系摘要
本論文主要是針對下顎前置型之口內止鼾裝置做機構設計。透過市場調查、品質機 能展開(QFD)、概念設計、有限元素分析法、決策矩陣法,提供一完整之工程設計流程。 在著手進行工程設計流程之前,首先要對打鼾機制進行了解。打鼾是一種普遍存在 的現象,也是睡眠呼吸障礙症最顯著的表徵,忽略睡眠呼吸障礙症的治療將導致嚴重的 健康問題。透過瞭解打鼾的機制以及診斷和治療方式之發展,確定了口內止鼾裝置之高 療效以及病患高接受度,其中又以下顎前置型口內止鼾裝置為最。 市場調查包含市售產品調查及專利分析。根據市售產品調查,由於睡眠醫療逐漸受 到重視,以及美國睡眠醫療學會(AASM)發表了口內止鼾裝置為打鼾之標準治療方式, 自1995 年起逐年皆有新的可調整式下顎前置型口內止鼾裝置問世。透過專利分析發現, 目前的設計仍存在許多缺點有待改進,例如:佩帶舒適度、高價位、體積過大及不容易 調整等,而在實際使用經驗上,更有裝置損壞之問題。 依據品質機能展開法之步驟,定義出顧客需求並將其轉換為可量化之工程規格,並 評估市場現有產品規格,與其比較之後定義出最終的工程目標。接下來進行概念設計階 段,使用子系統分解法將口內止鼾裝置分解成數個次系統,搭配使用腦力激盪法來結合 出一系統化之程序,並產出四個最終概念。利用有限元素分析法對所有最終概念及一現 有產品進行整體強度分析,來比較彼此間之效能優劣。最後,使用決策矩陣法,根據顧客需求的重要程度,從所有最終概念中挑選出最符合客戶需求之設計,再與品質機能展 開法中所定義出之工程目標進行比較,其中有所差異之部分將可做為未來改善之參考依 據。
A Study on the Mechanism Design of the
Mandibular Advancement Device
Student: Yi-Yu Lee Advisor: Chinghua Hung, Tsung-Yin Lin
Department of Mechanical Engineering National Chiao Tung University
ABSTRACT
This study focuses on the mechanism design of mandibular advancement devices (MAD). A complete engineering design process including market survey, quality function deployment (QFD), conceptual design and embodiment design is used.
Before the design process proceeded, the realization of snoring is necessary. Snoring is prevalent and is the most significant feature of sleep-disordered breathing (SDB). Ignore the therapies of SDB will lead to serious problems in health. Based on the research of mechanisms, diagnosis, and treatments of snoring, oral appliances are ensured in therapeutic effect and compliance, especially the MAD.
Market survey includes commercial product reviews and patent analyses. Due to pay more attention to the sleep medicine, the oral appliances are considered as a standard treatment of snoring that promoted by American Academy of Sleep Medicine (AASM). There are more and more adjustable MADs developed since 1995. According to the patent analyses, there are many drawbacks existing in the present design, such as uncomfortable, high cost, bulky volume, and complex to adjust, etc. According to the experiences of usage, this device
is suffered from the failure problem which requires to be improved in the future.
In accordance with the procedure of QFD, the customers’ requirements are obtained and translated to the measurable engineering specifications. Evaluate the commercial product to ensure the competition specifications, and set the engineering target at the end of the QFD process. In the conceptual design phase, a systematic procedure for generating concepts combines the functional decomposition which is used to divide the MAD into several sub-functions and the brainstorming method which is used to generate concepts for sub-functions. After that, four concepts are generated by the conceptual design process. The finite element analysis (FEA) is introduced to proceed the strength simulation for all of the concepts and one commercial product to evaluate the performance between each other. Finally, the decision-matrix method is used to evaluate all of the concepts based on the customers’ requirements and their own importance to select the best one. The comparison between engineering targets and specifications of the final design is carried out to estimate the performance of the final design, and to be considered as a criterion for further design works.
ACKNOWLEDGEMENT
碩士生涯的短短兩年之中,獲得的東西很多,得到的幫助也很多,要感謝的人自然 也就不會少。首先,也是最重要的要感謝的人是曾錦煥老師,從大四開始就跟著老師學 習,除了學業上的傳授,對於待人接物的態度,面對問題時的思考,乃至於生活上大大 小小的瑣事,老師都能適時的為學生指點迷津,學生是何其有幸能在學習的道路上遇到 如此明師。 考上研究所之際,承蒙老師愛護,順利進入應用最佳化實驗室,那時候的心情除了 喜悅,還有一種準備迎接挑戰的戰戰兢兢。未料,老師您先走了一步,學生除了悲傷、 難過,也發現到自己必須趕快振作,這期間得到了許多師長及學長姐們的幫助,特別感 謝蔡忠杓老師以及洪景華老師幫忙處理許多實驗室大大小小的事務,更感謝林聰穎老師 接下了指導不才學生的這個重擔,兩年來勞心勞力真是辛苦您了。另外,也感謝許多常 回來實驗室為我們加油打氣的學長姐,因為有你們的支持,讓我充滿信心迎接挑戰。 非常感謝口試委員:徐瑞坤老師以及呂東武老師,在百忙之中撥冗前來替學生口 試,更提出了許多寶貴的見解與建議,提供學生許多思考的方向,使得論文更加充實完 整。論文撰寫期間,感謝高中同學煒鑑、婉芸以及政軒在牙醫學的專業上提供了許多寶 貴意見以及協助,因為有你們的幫忙,論文才得以順利完成。 感謝在實驗室一起奮鬥的各位夥伴,跟你們在一起的日子裡有歡笑有悲傷,歡笑時 大家一起開懷大笑;悲傷時,大家一起渡過,遇見問題時也總是能義不容辭地互相幫忙, 這種有人相挺的感覺真好,真的很高興能有你們這一群學習上、研究上以及生活上的好 夥伴。 感謝我的家人,感謝你們在背後給予的支持與鼓勵,讓我能無後顧之憂的完成學 業,順利畢業,這份榮耀也屬於你們的。最後,感謝所有曾經幫助過我的人,真的非常 謝謝你們的協助與鼓勵。TABLE OF CONTENTS
摘要 ...i
ABSTRACT ...iii
ACKNOWLEDGEMENT ... v
TABLE OF CONTENTS ...vi
LIST OF TABLES ...ix
LIST OF FIGURES ... x
NOTATIONS...xiii
ABBREVIATIONS ...xiv
CHAPTER 1 INTRODUCTION... 1
1.1 Sleep-disordered Breathing ... 1
1.1.1 Anatomy of Upper Airways ... 1
1.1.2 Levels of Sleep-disordered Breathing ... 3
1.2 Motivation ... 4
1.3 Thesis Outline ... 6
CHAPTER 2 SNORING AND OBSTRUCTIVE SLEEP APNEA... 8
2.1 Pathophysiology of Snoring ... 8
2.1.1 Stages of Sleep ... 8
2.1.2 Mechanisms of Snoring ... 10
2.2 Evaluation of Obstructive Sleep Apnea ... 12
2.2.1 Symptoms ... 12
2.2.2 Diagnosis... 15
2.3.2 Non-surgical Treatments... 21
2.3.2.1 Non-prescription Treatments... 21
2.3.2.2 Positive Airway Pressure... 21
2.3.2.3 Oral Appliance ... 23
CHAPTER 3 MANDIBULAR ADVANCEMENT DEVICE... 26
3.1 Patents ... 26
3.1.1 Fixer ... 26
3.1.2 Connector ... 27
3.1.3 Adjustor ... 30
3.1.3.1 Protraction and Retraction... 30
3.1.3.2 Elevation and Depression... 33
3.1.4 Acting Force ... 34
3.1.5 Lateral Movement ... 34
3.2 Products ... 36
CHAPTER 4 QFD AND REQUIREMENTS... 47
4.1 Introduction ... 47
4.2 QFD for MAD ... 49
CHAPTER 5 CONCEPTUAL DESIGN ... 54
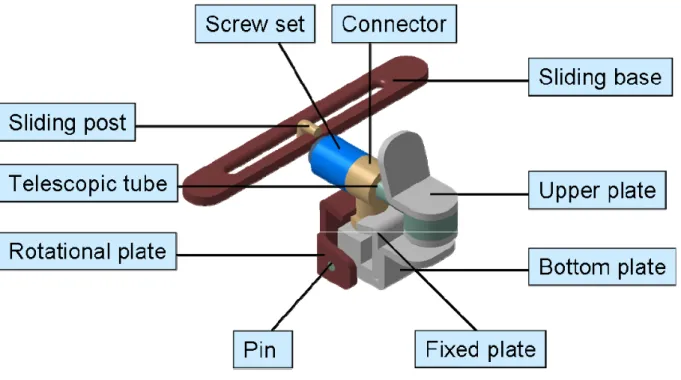
5.1 Design Method ... 54 5.2 Concepts ... 57 5.2.1 Concept 1 ... 57 5.2.2 Concept 2 ... 59 5.2.3 Concept 3 ... 60 5.2.4 Concept 4 ... 63
6.1.1 Load and Boundary Condition... 65
6.1.2 Material Properties... 66
6.1.3 Failure Criterion... 67
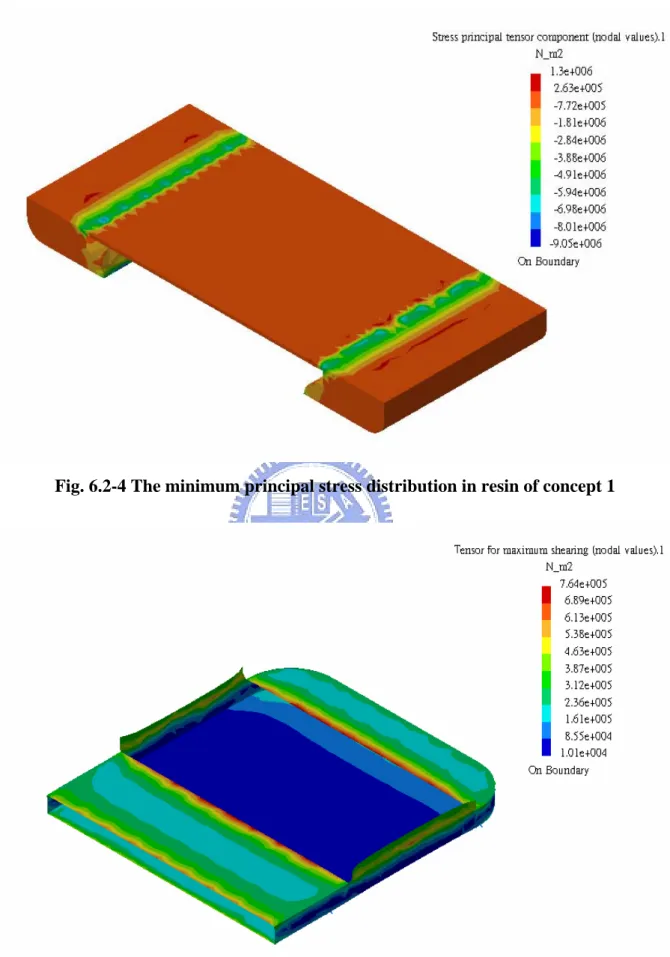
6.2 Analysis Results ... 69
6.2.1 Case I – The Results of Concept 1... 69
6.2.2 Case II – The Results of Concept 2 ... 73
6.2.3 Case III – The Results of Concept 3... 78
6.2.4 Case IV – The Results of Concept 4 ... 82
6.2.5 Case V – The Results of Commercial Product TAP-T ... 85
6.3 Concept Evaluation ... 90
6.4 Comparisons ... 92
CHAPTER 7 CONCLUSIONS AND FUTURE WORKS ... 94
7.1 Conclusions ... 94
7.2 Future Works ... 95
LIST OF TABLES
Table 2.2-1 Nocturnal and daytime symptoms of OSA [4]... 13
Table 2.2-2 Types of sleep studied for evaluation of sleep breathing disorders [4] ... 16
Table 2.2-3 Parameters measured in the Polysomnography [13]... 17
Table 2.2-4 Severity of obstructive sleep apnea [4]... 18
Table 2.3-1 Typical reasons for CPAP noncompliance [4] ... 23
Table 3.1-1 The fixers of mandibular advancement device ... 27
Table 3.1-2 The connectors of MAD ... 29
Table 3.1-3 The adjustors of MAD (Protraction and retraction) ... 32
Table 3.1-4 The adjustors of MAD (Elevation and depression) ... 33
Table 3.1-5 Types of acting force of MAD ... 34
Table 3.1-6 Types of lateral movement of MAD ... 35
Table 3.2-1 List of adjustable MAD products ... 37
Table 3.2-2 Comparison of adjustable MAD products... 38
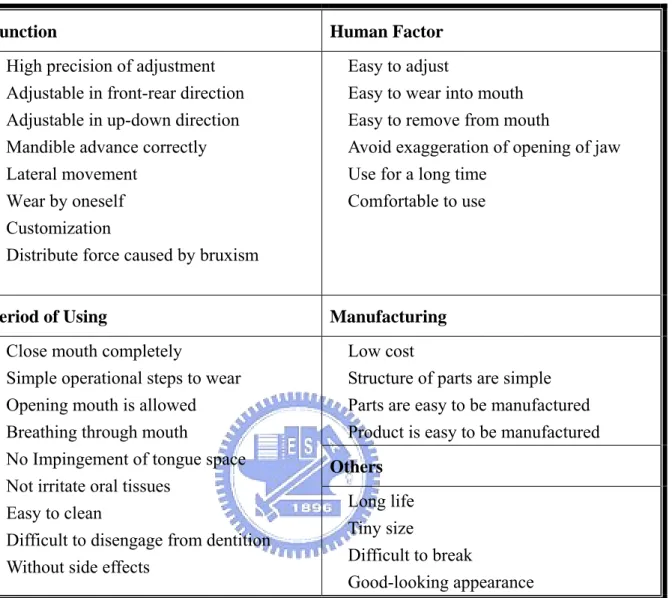
Table 4.2-1 List of customers’ requirements for MAD... 50
Table 6.1-1 Material properties for FEA ... 66
Table 6.2-1 Comparison of all finite element models... 89
Table 6.3-1 Decision matrix for concept evaluation... 91
LIST OF FIGURES
Fig. 1.1-1 Structure of the respiratory system [1] ... 2
Fig. 1.1-2 The sagittal section of the upper airway [2] ... 2
Fig. 2.1-1 EEG patterns in awake, slow-wave sleep, and REM sleep states [9] ... 9
Fig. 2.1-2 A typical night’s sleep record of an average young adult [9] ... 9
Fig. 2.1-3 Oral cavity [2] ... 11
Fig. 2.2-1 Epworth Sleepiness Scale [12] ... 14
Fig. 2.2-2 Polysomnographic report [4] ... 18
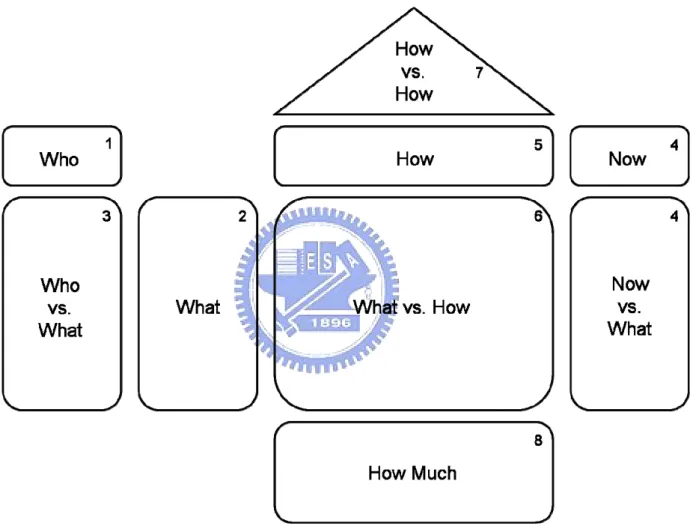
Fig. 4.1-1 The house of quality, also known as the QFD diagram... 48
Fig. 4.2-1 QFD diagram for MAD... 53
Fig. 5.1-1 Functional decomposition of MAD ... 55
Fig. 5.2-1 Conventional assembly of MAD ... 57
Fig. 5.2-2 Structure of mechanism in concept 1 ... 58
Fig. 5.2-3 Assembly view of concept 2... 59
Fig. 5.2-4 Structure of mechanism in concept 2 ... 60
Fig. 5.2-5 Assembly view of concept 3... 61
Fig. 5.2-6 Structure of mechanism in concept 3 ... 62
Fig. 5.2-7 The spring installed in concept 3 ... 62
Fig. 5.2-8 Assembly view of concept 4... 63
Fig. 5.2-9 Structure of mechanism in concept 4 ... 64
Fig. 6.1-1 Coulomb-Mohr criterion... 68
Fig. 6.2-1 The principal shear stress distribution on bonding interface of concept 1 ... 69
Fig. 6.2-2 The principal stresses distribution in resin of concept 1 ... 70
Fig. 6.2-3 The maximum principal stress distribution in resin of concept 1 ... 70
Fig. 6.2-5 The principal shear stress distribution on bonding interface of concept 1 ... 71
Fig. 6.2-6 The principal stresses distribution in resin of concept 1 ... 72
Fig. 6.2-7 The maximum principal stress distribution in resin of concept 1 ... 72
Fig. 6.2-8 The minimum principal stress distribution in resin of concept 1... 73
Fig. 6.2-9 The principal shear stress distribution on bonding interface of concept 2 ... 74
Fig. 6.2-10 The principal stresses distribution in resin of concept 2 ... 74
Fig. 6.2-11 The maximum principal stress distribution in resin of concept 2 ... 75
Fig. 6.2-12 The minimum principal stress distribution in resin of concept 2... 75
Fig. 6.2-13 The principal shear stress distribution on bonding interface of concept 2 .... 76
Fig. 6.2-14 The principal stresses distribution in resin of concept 2 ... 76
Fig. 6.2-15 The maximum principal stress distribution in resin of concept 2 ... 77
Fig. 6.2-16 The minimum principal stress distribution in resin of concept 2... 77
Fig. 6.2-17 The principal shear stress distribution on bonding interface of concept 3 .... 78
Fig. 6.2-18 The principal stresses distribution in resin of concept 3 ... 79
Fig. 6.2-19 The maximum principal stress distribution in resin of concept 3 ... 79
Fig. 6.2-20 The minimum principal stress distribution in resin of concept 3... 80
Fig. 6.2-21 The principal shear stress distribution on bonding interface of concept 3 .... 80
Fig. 6.2-22 The principal stresses distribution in resin of concept 3 ... 81
Fig. 6.2-23 The maximum principal stress distribution in resin of concept 3 ... 81
Fig. 6.2-24 The minimum principal stress distribution in resin of concept 3... 82
Fig. 6.2-25 The principal shear stress distribution on bonding interface of concept 4 .... 83
Fig. 6.2-26 The principal stresses distribution in resin of concept 4 ... 83
Fig. 6.2-27 The maximum principal stress distribution in resin of concept 4 ... 84
Fig. 6.2-28 The minimum principal stress distribution in resin of concept 4... 84
Fig. 6.2-31 The maximum principal stress distribution in resin of TAP-T ... 86
Fig. 6.2-32 The minimum principal stress distribution in resin of TAP-T ... 87
Fig. 6.2-33 The principal shear stress distribution on bonding interface of TAP-T... 87
Fig. 6.2-34 The principal stresses distribution in resin of TAP-T ... 88
Fig. 6.2-35 The maximum principal stress distribution in resin of TAP-T ... 88
NOTATIONS
σ1 Maximum Principal Stressσ3 Minimum Principal Stress
St Tensile Strength
Sc Compressive Strength
ABBREVIATIONS
AASM American Academy of Sleep Medicine ADSA American Sleep Disorders AssociationAHI Apnea-hypopnea Index
ANP Atrial Natriuretic Peptide
APAP Automatic Self-adjusting Positive Airway Pressure BPAP Bilevel Positive Airway Pressure
CDRH Center for Devices and Radiological Health CPAP Continuous Positive Airway Pressure
CSA Central Sleep Apnea
ECG Electrocardiography EDS Excessive Daytime Sleepiness
EEG Electroencephalography EMG Electromyography ENDS External Nasal Dilator Strips EOG Electrooculography ESS Epworth Sleepiness Scale FDA Food and Drug Administration
FEA Finite Element Analysis
GAHM Inferior sagittal mandibular osteotomy and genioglossal advancement with hyoid myotomy and suspension.
HR Heart Rate
IND Internal Nasal Dilators LMG Laser Midline Glossectomy LSAT Lowest Oxygen Saturation
MAD Mandibular Advancement Device MMO Maxillomandibular Osteotomy and Advancement MRD Mandibular Reposition Device
MSAS Mixed Sleep Apnea Syndrome
OA Oral Appliance
OSAHS Obstructive Sleep Apnea-hypopnea Syndrome
OSA Obstructive Sleep Apnea
OSAS Obstructive Sleep Apnea Syndrome OSDB Obstructive Sleep-disordered Breathing OSHS Obstructive Sleep Hypopnea Syndrome
PAP Positive Airway Pressure
PMMA Polymethylmethacrylate PSD Primary Snoring Disorder
PSG Polysomnography QFD Quality Function Deployment REM Rapid Eye Movement
SDB Sleep-disordered Breathing
SPL Soft Palate Lift
TMJ Temporomandibular Joint
TRD Tongue-retaining Device
UARS Upper Airway Resistance Syndrome UPPGP Uvulopalatopharyngoglossoplasty UPPP Uvulopalatopharyngoplasty USPTO United States Patent and Trademark Office
CHAPTER 1
INTRODUCTION
1.1 Sleep-disordered Breathing
Respiration plays the key role of human life which moves air in and out from the lungs. Oxygen and carbon dioxide can be exchanged between air and blood to supply the needs of all activities in human body. The passageways between the ambient environment and the gas-exchange unit, the alveoli, in the lungs are called the conducting airways. The conducting airways are divided into the upper airways and the lower airways, as shown in Fig. 1.1-1 [1] [2]. If there is some resistance occurred in these airways to reduce the quantity of inspiration into the lungs when the time of sleeping, it might be the symptom of sleep-disordered breathing.
1.1.1 Anatomy of Upper Airways
The upper airways are composed of the nose, oral cavity, pharynx, and larynx, as shown in Fig. 1.1-2. The larynx represents the transition between upper and lower airways. The primary functions of the upper airways are to humidify and warm the inspired air, and to filter out and prevent foreign materials from entering the tracheobronchial tree.
According to Fig. 1.1-2, the maxilla forms the anterior portion of the nasal cavity floor, called the hard palate. The posterior portion of nasal cavity floor is the muscular soft palate [3]. After the inspired gas passes through the nasal cavity, it enters the pharynx. The pharynx is divided into three parts which are the nasopharynx, oropharynx, and laryngopharynx. The nasopharynx is located on the posterior portion of the nasal cavity and superior to the level of soft palate. Next to the nasopharynx, the oropharynx lies between the soft palate superiorly and the base of the tongue inferiorly. The laryngopharyx, also called the hypopharynx, is the
Fig. 1.1-1 Structure of the respiratory system [1]
The resistance of the airflow through the nose is greater than that through the mouth. The reason is that the structures in the nose are designed to accomplish the filtering, warming, and humidifying functions. The raising resistance sometimes causes people to switch to mouth breathing. Therefore, the oral cavity is considered as an accessory respiratory passageway to ensure the quantity of sufficient inspiration for needs.
1.1.2 Levels of Sleep-disordered Breathing
As the sleep-disordered breathing (SDB) occurred, it may possibly affect the patient’s sleep quality possibly. The patient’s sleep fragment will cause awakening or partial awakening, or disrupt the patient’s sleep. It makes the patient feel restless and sleepiness in the daytime. SDB is a term including several different states of breathing disorder. In accordance with the degrees of the severity, from mild to severe, it can be classified progressively as follows [4]:
z Primary snoring disorder (PSD): snoring without sleep disruption and without excessive daytime sleepiness (EDS).
z Upper airway resistance syndrome (UARS): usually accompanied by snoring. Besides, increasing respiratory effort against airway resistance may lead to sleep fragmentation and cause excessive daytime sleepiness.
z Obstructive sleep hypopnea syndrome (OSHS): snoring with partial airway obstruction, but not complete apneas, associated with excessive daytime sleepiness and other symptoms of OSAHS.
z Obstructive sleep apnea-hypopnea syndrome (OSAHS): snoring with documented hypopneas and apneas, associated with excessive daytime sleepiness and other symptoms of OSAHS.
associated with excessive daytime sleepiness and other symptoms of OSAHS, practically synonymous with OSAHS.
z Mixed sleep apnea syndrome (MSAS): combination of central sleep apnea (CSA) and obstructive sleep apnea (OSA), associated with symptoms of OSAHS.
Therefore, snoring can be seen as an obvious representation of the sleep-disordered breathing during human sleep.
1.2 Motivation
Snoring, the lay term for obstructive breathing during sleep, is one of the most prevalent of obnoxious human habits. In the adult population in the United States, 59% of them have had the experience of snoring. Furthermore, 32% of them snore at least three nights a week. The person who snores more than three nights a week is called as a habitual snorer; and further, 24% of these adults snore every night or almost every night [5]. Therefore, snoring is really a serious problem that could not be disregarded and ignored.
Loud snoring usually makes others feel noisy and uncomfortable. Snoring also influences the sleep quality of snorers’ bed partners, because of the noise they do not get to sleep easily. The loudest snorer in the Guinness World Record is a Swedish, Kare Walkert, whose snoring sound reached the peak level of 93 decibels recorded in 1993 [6]. According to an investigation in the United States [5], 17% of snorers say that their snoring is very loud and can be heard in adjacent rooms. More than one-half of those who snore (57%) report that their snoring has bothered others. In addition, snoring not only disturbs others beside snorers in surrounding environment but also affects snorers themselves in physical conditions. Snoring causes the reduce of sleep quality leading to several medical problems, such as excessive daytime sleepiness, high blood pressure, increased risk for cardiovascular disease and cerebral vascular accident, and etc. These problems and related influences cost about 100 billion
annually in lost productivity, medical bills, and industrial accidents [7]. It requires some improvements urgently.
As described above, snoring is an extremely prevalent disorder that can lead to medical and social problems, and that forms impediments to good interpersonal relationships. In order to prevent these problems from becoming more and more serious, there are more and more researches making efforts on it. At first, there are some self-help remedies which are worth trying, such as weight deduction, avoiding getting overtired, avoiding alcoholic drinks and sleeping pills before bedtime, stopping any tobacco use, and sleeping sideways rather than on your back. Common therapies for snoring can be generally divided into surgical treatments and non-surgical treatments. Surgical treatments mean that doing an operation on the upper airway to reduce obstructions in the passageway of the air. For example, to resect as much excessive soft tissues as possible, to implant pillars on the soft palate, to advance the maxilla and mandible, etc. For non-surgical treatments, drugs and several types of devices have been proposed. But the curative effects on pharmacologic agents have not been proven as effective [4]. There are many non-prescription devices offered for sale on the market, but very limited data are available to support a beneficial effect of these devices on snoring and use in treating obstructive sleep apnea. Besides, two other therapies are considered as standard treatments for snoring and OSA which are supported by extensive scientific evidence for safety and efficacy. One is the positive airway pressure (PAP) appliance, and another is the oral appliance (OA). Those devices of PAP and OA are prescription devices that should be fitted and adjusted by doctors.
Although, lots of therapies in treating snoring and OSA have been proposed already, they still have some problems, such as the efficacy and safety of therapies, the compliance and complications after treated, the failure of the device, the breakdown of the mechanism. Those shortages mentioned above are required to be solved.
1.3 Thesis Outline
In this study, a complete engineering design process is performed to bring out a new design of mechanism in the mandibular advancement device. According to the market survey, QFD process is used to generate the engineering specifications and to ensure that all engineering specifications are conformed with the customer requirements. Based on the results of QFD, a conceptual design process will be proceeding to generate new concepts. The final target of this study is to generate a new, feasible, and durable mandibular advancement device after completed whole design process.
Chapter 2 introduces the pathophysiology of snoring by which the mechanisms of snoring will be realized. Furthermore, the diagnosis and treatments are presented to assist the overall understanding in the medical field. Finally, to make sure of the mandibular advancement device is one of effective therapies and treatment with high efficacy.
Chapter 3 focuses on the present developments on the mandibular advancement devices. According to the survey of patents and products on market, the patent analysis, the functions of components in mandibular advancement devices, and the comparisons of products will be proposed in this chapter.
Chapter 4 introduces the QFD method to proceed a procedure from collecting customers’ requirements, evaluating the relative importance, evaluating the competitive products, generating the engineering specifications, and defining the target specifications at the end.
Chapter 5 applies the functional decomposition and the brainstorming method to provide a systematic procedure to generate complete concepts of the MAD. Brainstorming method is used to generate concepts for every sub-function initially, and then the complete conceptual design is generated by combining those concepts of sub-functions.
Chapter 6 introduces the Finite Element Analysis method to simulate the stresses under a force, and evaluate the strength of four concepts generated from chapter5 and one commercial product. The decision-matrix method is also introduced in this chapter in order to evaluate all the concepts for selecting the best one.
Finally, chapter 7 makes some conclusions for this study and promotes some recommendations for further researches in the future.
CHAPTER 2
SNORING AND OBSTRUCTIVE SLEEP APNEA
2.1 Pathophysiology of Snoring
Snoring and obstructive sleep apnea may be considered under the scope of obstructive sleep-disordered breathing (OSDB), which is a type of sleep-disordered breathing. It means that snoring occurs because of the obstructions formed in the airways. Snoring can be defined as an inspiratory noise produced by vibration of the soft parts of the oropharyngeal wall [8]. When portions of the soft parts collapse, that will form the obstructions in the airways and lead to snoring.
2.1.1 Stages of Sleep
The stages of sleep were discovered in the 1950s [7] in the experiment of brain wave using the electroencephalogram (EEG) during sleep. Neurophysiologists recognize two phases of sleep, slow-wave sleep and paradoxical sleep. The initial phase, called slow-wave sleep, can be divided into four stages, each successive stage having a particular EEG pattern. As the proceeding of slow-wave sleep from light sleep (stage 1) to deep sleep (stage 3 and 4), the EEG patterns have slower frequency and higher amplitude progressively, and the patterns are the alpha rhythm, theta rhythm, and delta rhythm in sequence [9], as shown in Fig. 2.1-1. Besides, the tension in the skeletal-muscles become progressively more relaxed as slow-wave sleep progresses until the stage 4 is achieved.
Sleep always begins with the slow-wave sleep progression from stage 1 to stage 4 which normally takes 30 to 45 minutes and then reverses itself. After the slow-wave sleep, the second phase of sleep, paradoxical sleep, also called rapid eye movement (REM) sleep, comes up. During the REM sleep, the EEG pattern characterizes as resemblance to the alert and
time, and the sleeper is difficult to be aroused by others. The REM sleep period usually lasts 10 to 15 minutes. At this time, the lower muscle tone leads to paralysis of skeletal-muscle except the eye muscles and the muscles of respiration. If sleep uninterrupted, it continues slow-wave sleep and REM sleep by turns, called the sleep cycle, until awakening, as shown in Fig. 2.1-2.
Fig. 2.1-1 EEG patterns in awake, slow-wave sleep, and REM sleep states [9]
2.1.2 Mechanisms of Snoring
The origin sounds of snoring generation is from the collapsible part of the airway without rigid support. Snoring generation involves the soft palate, uvula, tonsils, base of tongue, pharyngeal muscles, and pharyngeal membranes, as shown in Fig. 2.1-3. Five causes below, acting either alone or combination, contribute to snoring:
z Poor muscle tone in the palate, tongue, and pharynx:
This is the cause of most adult snoring. In deep sleep stages, such musculature fails to participate in the respiratory cycle to open the airway during inspiration. The dilator effect of the pharyngeal muscles and the protrusive effect of the genioglossus muscle are inadequate. Thus, the tongue falls backward into the airway and vibrates against the floppy pharynx during inspiration. Snoring may appear as soon as the snorer falls asleep in stage 1, increasing progressively with deepening of slow-wave sleep and reaching a peak in stage 4.
z Space-occupying masses or tissues in the pharynx:
Children who snoring almost have enlarged tonsils and adenoids. Many adults also have large tonsils which form the obstruction in the airway and are notable in obese persons. Those excessive bulky pharyngeal tissues cause narrowing of the air passageways and lead to snoring.
z The receding mandible:
It may not be effective in keeping the tongue sufficiently forward when the muscles relaxed in sleeping time.
z Excessive length of the soft palate and uvula:
The long soft palate narrows the nasopharyngeal aperture. As it dangles in the relaxed situation, its lower edge often lies below the horizontal plane of the tongue
and it acts as a noisy flutter valve during inspiration. If the patient lies in the supine position, that will lead to a more apparent snoring. Besides, a long uvula makes matters even worse.
z Obstructed nasal airways:
The rising resistance of airflow in the nose requires extra effort to inspire the air. This increases the vacuum in the airway and produces a negative pressure to draw together the floppy tissues in the collapsible parts where they vibrate and cause snoring. Therefore, many persons who ordinarily do not snore may snore when they catch a cold or get an allergy attack.
Fig. 2.1-3 Oral cavity [2]
As described above, those are the causes of snoring and they may be influenced by several factors, such as anatomy [10], age, sex, hormones, Genetic factors, and etc. These factors may affect the thickness of soft tissue in the upper airway, the muscle tone during rest,
the pharyngeal cross sectional area, the upper airway dilator activity, and etc [11]. Without doubt, anatomy is the most important factor when dealing with the patient with snoring and it can be divided into the factors which related to the soft tissue or the skeleton; and further, it is more obvious than other factors that leading to snoring.
2.2 Evaluation of Obstructive Sleep Apnea
Apnea is a Latin medical term meaning “without breathing.” When the interruption to breathing occurs during sleeping time and is caused by an obstruction in the airway, it is “obstructive sleep apnea.” Obstructive sleep apnea is the most severe state of obstructive sleep-disordered breathing and usually accompanies severe snoring and other symptoms either in sleeping time or in daytime. Sleep apnea was first discovered in the search for the pathophysiological process behind the pickwickian syndrome with nocturnal polygraphic monitoring of abnormal breathing patterns during sleep in 1960s. At present, several methods have been developed to diagnose the probability of suffering from OSA.
2.2.1 Symptoms
Typical symptoms of obstructive sleep apnea include snoring, observed apnea, excessive daytime sleepiness, or a combination of them. When any signs are expressed that relate to sleep apnea, the patient and observer should be questioned about other known symptoms, as shown in Table 2.2-1.
Since the patient is asleep, he or she is often not aware of many nocturnal signs. The bed partner of patient or other observer is needed to determine the severity of snoring, snorting, struggling to breathe, irregular breathing, and observed apnea. Abnormal movements during sleep, such as thrashing in bed and arm or leg jerks, would be known only by an observer. Patients just feel restlessness after they wake.
severe sleep apnea. Associate with arousals, decreased esophageal pressure, and hypoxemia, the increased atrial natriuretic peptide (ANP) stimulates urinary excretion. This symptom is more common in children than in adults that causes enuresis.
Table 2.2-1 Nocturnal and daytime symptoms of OSA [4]
Nocturnal Symptoms
Snoring, snorting, struggling to breathe, irregular breathing, and observed apnea
Trashing in bed, disrupted sleep Nocturnal gasping or choking Frequent awakenings
Nocturnal palpitations Insomnia
Daytime Symptoms
Nonrestorative sleep, morning fatigue Excessive daytime sleepiness
Memory deficits, forgetfulness Troubled concentration
Morning headaches
Morning dry mouth or sore throat Depression, irritability
Impotence, sexual dysfunction
Daytime tiredness or fatigue is a common complaint of OSA patients. The cause of excessive daytime sleepiness is due to a combination of arousals, sleep fragmentation, and reductions in delta and REM sleep. Patients may also complain of inability to concentrate and of deterioration of memory and judgment. The EDS also leads to psychiatric disorder, such as depression and irritability, and the suddenly fall asleep which will cause car accidents during
driving time. A widely used short questionnaire, the Epworth Sleepiness Scale (ESS), has been developed to measure the severity of daytime sleepiness, as shown in Fig. 2.2-1. The lowest score is zero and the highest twenty-four, and above ten is considered abnormal.
Fig. 2.2-1 Epworth Sleepiness Scale [12]
Morning headaches are attributable to the presence of sleep apnea. The nocturnal oxygen desaturation is the cause of morning headaches. There are still other morning symptoms such as the morning dry mouth or sore throat that is due to mouth breathing and snoring.
Impotence, sexual dysfunction, and loss of sex drive are also linked to the presence of sleep apnea with a severe state. It is not known if the cause of impotence is similar to other symptoms. Sexual dysfunction is usually reversible with treatment of the sleep-disordered breathing.
Many symptoms are known to discriminate patients with or without OSA probability. If someone snoring with those symptoms, he or she should seek the further examination from a sleep specialist as soon as possible.
2.2.2 Diagnosis
A sleep study should be applied to the patient with sleep-disorder breathing. The aims of testing are to establish the diagnosis, to determine the frequency and severity of abnormal respiratory events, and to evaluate the physiologic consequences during sleep. The American Academy of Sleep Medicine (AASM, formerly the American Sleep Disorders Association [ADSA]) has defined four types of sleep testing: standard polysomnography (PSG), which requires the presence of a trained technician, and three variations of unattended studies [4], see Table 2.2-2.
Table 2.2-2 Types of sleep studied for evaluation of sleep breathing disorders [4]
Type 1 Type 2 Type 3 Type 4
Monitors 7 or more 7 or more 4 or more 1-2
EEG Required Required Optional Not measured
EOG Required Required Optional Not measured
Chin EMG Required Required Optional Not measured ECG/HR ECG ECG or HR ECG or HR Optional
Airflow Required Required
2 of effort
or 1 airflow Optional Respiratory effort 2 channels 2 channels 1 of effort Optional
Oximetry Required Required Required Usual/optional Leg movement Usual/optional Optional Optional Not measured
Personnel Present Absent Absent Absent
Intervention Possible Not possible Not possible Not possible EEG: electroencephalography, EOG: electrooculography, EMG: electromyography, ECG: electrocardiography, HR: heart rate
Among all the types of studies, the type-1 sleep study is the overnight polysomnography which is routinely indicated for the diagnosis of sleep-disordered breathing [13]. Polysomnography, which is performed in a sleep laboratory with a technician present, is a continuous recording of sleep for at least six hours during a patient’s normal sleeping time. As the study proceeding, the following parameters listed in Table 2.2-3 are routinely measured [13].
Table 2.2-3 Parameters measured in the Polysomnography [13]
No. Items No. Items
1 Electroencephalogram (EEG) 7 Thoracic movement
2 Electrooculogram (EOG) 8 Abdominal movement
3 Chin electromyogram (EMG) 9 Leg electromyogram
4 Electrocardiogram (ECG) 10 Snoring sound
5 Nasal/oral airflow 11 Body position
6 Blood oxygen saturation (SaO2)
EEG, EOG, and chin EMG are used together to determine sleep stage, wakefulness, and arousals from sleep. The ECG is used to detect arrhythmias during sleep. Nasal and oral airflow can detect not only apnea and hypopnea but also flow limitation associated with upper airway resistance. Blood oxygen saturation is measured with finger sensor and oximeter to determine the degree of desaturation. Other parameters are also measured by specific devices to detect and record data for later analysis. Then, all detected parameters will be used to construct a polysomnographic report, as shown in Fig. 2.2-2.
In clinical definitions, apnea is defined as a cessation in breathing for at least ten seconds without airflow measured on the airflow sensor. If the event is obstructive during apnea, there is effort to breathe. Several clinical definitions of hypopnea are in clinical use and there is no clear consensus. An AASM position paper defines hypopnea as an abnormal respiratory event with at least a 30% reduction in thoracoabdominal movement or airflow lasting at least ten seconds, and with 4% oxygen desaturation or greater [14]. The number of apneic plus hypopneic episodes per hours is defined as the apnea-hypopnea index (AHI). Based on the AHI and lowest oxygen saturation (LSAT) can determine the severity of OSA, as shown in Table 2.2-3.
Fig. 2.2-2 Polysomnographic report [4]
Table 2.2-4 Severity of obstructive sleep apnea [4]
AHI LSAT
Mild 5 – 14 86% – 90%
Moderate 15 – 29 70% – 85%
Severe ≥ 30 < 70%
Besides the sleep study, the clinician makes judgments also by the clinical history of patient and the physical examination. According to the results of diagnose in many directions, clinicians will make the more helpful suggestion to patients with sleep-disordered breathing based on their own experiences. Therefore, the right remedies will more suitable for each case.
2.3 Treatments
Various treatments of snoring and OSA have been proposed. All the treatments can be generally classified into surgical treatments and non-surgical treatments. Operations to treat snoring and OSA are the treatments which belong to surgical, others are non-surgical. Those non-surgical treatments include behavior modification, pharmacologic treatment and various mechanical devices to reduce or eliminate snoring and OSA. Standard treatments for OSA proven by AASM include upper airway surgery and the use of positive airway pressure appliance and oral appliance [15].
2.3.1 Surgical Treatments
The surgical modifications of the upper airway for the treatment of OSA can be divided into three categories: classic procedures, specialized procedures, and tracheotomy [19]. Before the surgery, the anatomic regions of obstruction should be identified first. The pharynx can be functionally divided into two portions: the retropalatal pharynx, the region of the pharynx posterior to the soft palate, and the retrolingual pharynx, the region of the pharynx posterior to the vertical portion of the tongue. Based on the above basis, patterns of pharyngeal obstruction, narrowing, or collapse can be classified into the following way [20]:
z Type I: narrowing or collapse in restropalatal region only.
z Type III: narrowing or collapse in retrolingual region only.
Classic surgical techniques have been developed to alter the soft tissue and skeleton of nose, such as nasal-septal reconstruction, cauterization, and outfracture of turbinates. Classic pharyngeal procedures such as tonsillectomy have been used to enlarge the pharyngeal space. However, these procedures were frequent failure so that new surgical approaches were developed.
Fujita [21] introduced the Uvulopalatopharyngoplasty (UPPP) as the first specialized surgical procedure to treat OSA in 1981. UPPP is a procedure that operates on the tonsil to enlarge the retropalatal airway. The procedure trims the posterior and anterior tonsillar pillars, and resects the uvula and posterior portion of the palate. Then, another operation, the Uvulopalatopharyngoglossoplasty (UPPGP), combines a modified UPPP with limited resection of the tongue base. Laser midline glossectomy (LMG) and lingualplasty are two procedures that create an enlarged retrolingual airway by laser extirpation of a midline. The difference between LMG and linguaplasty is that additional tongue tissue is extirpated in LMG. GAHM is an abbreviation used to represent the whole procedure of inferior sagittal mandibular osteotomy and genioglossal advancement with hyoid myotomy and suspension. The two components of the procedure create an enlarged retrolingual airway. In GAHM, the hyoid bone is advanced and suspended from the mandible by a fascial trip that will not change the dental occlusion. The last one in specialized surgical procedure, the maxillomandibular osteotomy and advancement (MMO), provides maximal enlargement of the retrolingual airway and some enlargement of the retropalatal airway. Moving the maxilla forward simultaneously with mandible permits greater forward motion of the mandible because of the maintenance of dental occlusion.
and maintain the stoma. The tracheostomy tube is with sufficiently small diameter that, when plugged, it permits air inspiration through upper airway from nose and mouth to the lungs pass around the tube.
2.3.2 Non-surgical Treatments
Non-surgical treatments include behavior modification, pharmacologic treatment and the use of mechanical devices. Behavior modification is the self-help remedy which contains alteration of sleep position, avoidance of alcohol and sedative medication, and weight-reduction programs. Pharmacologic treatments are not recommended to treat OSA because of the lack of clinical trials and the conclusions on efficacy, but some of them may effective to reduce the side effect of OSA [22]. At present, drugs should be considered as either second line therapies or as adjuvant therapies [23]. Further, several mechanical devices are used to remedy the snoring and OSA, and will be introduced below.
2.3.2.1 Non-prescription Treatments
Non-prescription treatments mean that the therapies performed without a prescription or even a medical evaluation. Those treatments include some pharmacologic products, several mechanical products, and others. There are so many commercial products become popular to many snorers. As described above, the efficacy of pharmacologic products are not obvious. Mechanical products, such as external nasal dilator strips (ENDS) and internal nasal dilators (IND), are also with limited evidence to suggest the use of them [24]. Most of these products are without obvious efficacy and the use of them may also delay proper evaluation and treatment of the snoring and OSA. Therefore, go to see a doctor and evaluate the condition of snoring and OSA maybe better than use the product without prescription.
invasive treatment for OSA [4]. Types of PAP treatment include continuous PAP (CPAP), bilevel PAP (BPAP), and automatic self-adjusting PAP (APAP). The most widespread application of PAP is the treatment of OSA with CPAP. The application of CPAP prevents collapse of the upper airway by promoting the balance of the forces that keep the airway open versus that innately collapse it. The basic CPAP appliance is composed of an electronically controlled compressor and a pressure gauge, which can be adjusted to personal settings. The pressure setting is established by a titration study with attended PSG to adjust to the optimal pressure for maintaining airway patency. The sufficient pressure for preventing apnea is variational in all sleep stages and all sleep postures. Use the titration to find a fixed single pressure for subsequent nightly usage. The CPAP treatment is high efficacy but without enough acceptance and tolerance. The reasons for the CPAP noncompliance are listed in Table 2.3-1.
Table 2.3-1 Typical reasons for CPAP noncompliance [4] No. Reasons 1 Nasal stuffiness and discharge
Rhinitis, irritative, from cold/dry air
Rhinosinusitis, bacterial/viral/fungal, from poor hygiene or contagion Uncorrected nasal, septal, turbinate deformities
Untreated allergies, sinusitis, polyps, masses
2
Mask problems
Poor fit, discomfort, claustrophobia Air leakage, dry eyes, conjunctivitis Skin rashes/abrasions
3
Equipment problems
Noisy or cumbersome devices High air-pressure-level discomfort Travel problems
Social/spousal aversion 4 Failure to gain sufficient recognizable benefit 5 Failure to understand medical necessity
6 Failure to receive educational, instructional, and motivational counseling at onset 7 Cost, insurance noncoverage
2.3.2.3 Oral Appliance
The application of the oral appliance for the treatment of obstructive sleep apnea was first introduced in 1984 [25]. Various oral appliances have been developed for the treatment of snoring or OSA. With different designs, they can be classified into three basic categories as follows:
z Mandibular advancement devices (MADs): it also termed as the Mandibular reposition devices (MRDs). These are removable devices which are worn at night during sleep. Most devices require dental impression, bite registration, and fabrication by a dental laboratory. Those devices are fixed to upper and lower teeth and are adjusted to advance the mandible. The amount of protrusion is adjusted to meet the therapeutic requirements, comfort, and tolerance. Many devices have a fixed degree of advancement. Some are adjustable in a limited degree.
z Tongue-retaining device (TRD): it is designed to keep the tongue in an anterior position during sleep. The tongue is held in place by a negative pressure in a soft plastic bulb, which protrudes out of the mouth. The lips are closed over a flange which fits between the lips and teeth to hold the device.
z Soft palate lift (SPL): these removable devices are also for nighttime use during sleep. A posterior extension is fitted up upper teeth to lift the soft palate and uvula out of the pharyngeal airway. These devices have not demonstrated efficacy in reducing either snoring or OSA.
All oral appliances produce downward rotation of the mandible, many of them also move forward the mandible by design. In a comparative study, a strong patient preferences appeared for the MAD. The MAD was an effective treatment and the TRD and SPL were less tolerable and significant improvements [26].
Oral appliances may improve upper airway patency during sleep by enlarging the upper airway or by decreasing upper airway collapsibility. The mechanism action of oral appliances is at least three ways. First, they bring the mandible and base of tongue forward. Second, they stabilize the mandible to prevent it from falling open during sleep. And third, they alter the mandibular position through downward rotation, thereby causing an increase in cross
sectional airway size and muscle tone. After the oral appliance therapy, snoring is improved in 73% to 100% of patients [27]. Those patients with mild to severe OSA have a 52% chance of being able to control their sleep apnea to reach a level of AHI less than 10 by using oral appliances [28]. Whole OAs are less effective than CPAP but may be better accepted by patients than CPAP in whom used both treatments. The common side effects of oral appliance, such as excessive salivation, dryness of the mouth, or transient discomfort, may prevent early acceptance. The major long-term problems are temporomandibular joint (TMJ), or jaw discomfort and limited movement of the teeth. Those effects can be minimized if the appliance is adjusted to so as to avoid excessive advancement of the mandible.
The standard treatments of snoring and OSA promoted by AASM include surgery, CPAP, and oral appliance. Among all of three, CPAP and oral appliance are noninvasive treatments. The CPAP is more effective than oral appliance, but the compliance of oral appliance is better than CPAP. Further, some drawbacks of CPAP in the equipment, interface, or appearance will lead to intolerable to use or inconvenience of usage in some occasions. Therefore, this study will focus on the oral appliance, even the mandibular advancement device, to innovate.
CHAPTER 3
MANDIBULAR ADVANCEMENT DEVICE
3.1 Patents
The patent review of this study is based on the patents published in the United States since 1976. They can be searched from the patent full-text and full-page image databases in the United States Patent and Trademark Office (USPTO) [29]. According to the patents, the development and trend in specific techniques can be realized. In this study, the aim of patent search focuses on the mechanisms of anti-snoring devices especially the mandibular advancement devices. Referring to the patent review, the analysis results can be classified into several categories by functions which will be discussed in following subsections. In general, patents are invented to improve the disadvantages existed in prior arts. The disadvantages refer to the analysis including uncomfortable to use, low compliance, high cost, can not or complex to adjust, bulky volume, lack of customizability, and etc.
3.1.1 Fixer
The function of the fixer is used to install the mandibular advancement device in the oral cavity by fixing on the teeth. The usage of most MADs is inserting into the mouth during sleep and removing after getting up. Because of the requirement of removability, the fixer is usually designed just to fit but not mount on the teeth. Thermoplastic materials are usually used to form the fixer like a mouthpiece. Some appliances add clasps on to make MAD more stable during wearing time. Finally, a little parts of MADs are directly fixed on the teeth by mounting. Those devices are usually used to treat the malocclusion, but the advancement of the mandible also can eliminate snoring (Table 3.1-1).
Table 3.1-1 The fixers of mandibular advancement device
Thermoplastic material
Thermoplastic material and Clasp
Mount directly
U.S. Patent No. 5365945 [30] U.S. Patent No. 5427117 [31] U.S. Patent No. 5645423 [32]
3.1.2 Connector
In the two-pieces MAD, the connector connects the upper and lower mouthpiece adjustably. Different from the two-pieces MAD, the one-piece MAD which is entirety made by one material does not need the connector and cannot be adjusted. Therefore, all the MADs discussed here are the two-piece MAD which various connectors are used (Table 3.1-2).
z Button
An elastic button-like connector couples with a aperture to interconnect upper and lower mouthpiece. This kind of connector connects two mouthpieces in a fix degree of advancement without the function of adjustment during using. The decision of degree of advancement is applied during the impression process by the therapist. z Screw
The screw connector means either the traditional screw or the dual-thread screw. Using screws as the connector to connect the upper and lower mouthpiece can be very tight and high strength. However, it is usually not convenient to use because it
needs be wrenched by a screw driver. z Wire
Wire connector can be shaped to the oral cavity to prevent the movement space of tongue from being occupied by connected and adjusted mechanism. The strength of the wire may be concerned according to its failure.
z Surface contact
An object is fixed to one mouthpiece and contacts with another one. This condition can be considered as that upper and lower mouthpieces are connected by contacting. Therefore, contacting is the connector in this kind of appliance.
z Post
The post is coupled with the aperture restrainedly or freely depended on the shape of the post. It may be single or numerous locating in the anterior or posterior portion or both on the mouthpiece.
z Interlocking member
Interlocking member, for example the Velcro, is a connector with two phases that are engaged by contacting and are disengaged by tearing. It can be connected in any position that is convenient to use and adjust. But it is also easy to be separated which leads to the poor strength.
z Elastic band
Elastic band is a flexible material used to pull the mandible advancement. Because of the flexibility, the movement of the mandible still keeps large degrees of freedom after advanced. It means it is unstable.
upper and lower mouthpieces to drive the mandible advancement. The link may be a scope-like structure that is variational in length.
Table 3.1-2 The connectors of MAD
Button Wire Surface contact
U.S. Patent No. 5313960 [33] U.S. Patent No. 5409017 [34] U.S. Patent No. 5566683 [35]
Post Interlocking member Screw
U.S. Patent No. 5499633 [36] U.S. Patent No. 5642737 [37]
Elastic band Linkage
3.1.3 Adjustor
In aforementioned descriptions, connectors are used to connect the upper mouth piece and lower mouthpiece to form the MAD. The adjustor is either as a part of the connector or as an individual component to perform the function of adjustment. The way of adjustment can be divided into two types: continuous adjustment and position-fixed adjustment. The direction of adjustment makes the mandible not only protraction and retraction but also elevation and depression (Table 3.1-3).
3.1.3.1 Protraction and Retraction z Series of aperture
This is one of position-fixed adjustments. The series of apertures are usually coupled with the screw or the post, and they are equal in interval. Choose one of those apertures as the preferred position to connect.
z Screw
The screw works as a continuous adjustor with high precision. It can satisfy the requirement of adjustment in a small amount. The screw usually works as a component of the connector to adjust its position.
z Dual-thread screw
The dual-thread screw is a combination of two screws in the opposite threaded direction. The performance of the dual-thread screw is double to the traditional screw.
z Conjugate shape
Identical shape arranges in series to connect with its conjugate shape face-to-face worked as a position-fixed adjustor. The commonly used shape is the saw-shaped
surfaces together. z Interlocking member
This kind of adjustor may be considered as a continuous adjustor or a position-fixed adjustor with tiny interval between one and one interlocking members. It is easy to operate by touching the interlocking member together anywhere you preferred. z Elastic band
The degree of advancement depends on the length of the elastic band. Some additional components are used to adjust the length. The force applied on the mandible may be changed by replacing the elastic band in different stiffness.
z Slot
The connector slides in the slot to adjust the position of the mandible continuously. A fastener is usually used to fasten the connector on the slot in a preferred position. z Replace component
Various components are applied for replacing to change the position of the mandible. This kind of adjustment is position-fixed and may be inconvenient to use because of lots substitute components should be prepared.
Table 3.1-3 The adjustors of MAD (Protraction and retraction)
Series of aperture Elastic band Dual-thread screw
U.S. Patent No. 5365945 [30] U.S. Patent No. 5755219 [38] U.S. Patent No. 5409017 [34] Conjugate shape Interlocking member Screw
U.S. Patent No. 5570704 [41] U.S. Patent No. 5642737 [32]
Slot Replace component
3.1.3.2 Elevation and Depression
The adjustment of elevation and depression of the mandible is not usually designed as a function of the MAD. The purpose of this function is to make the product suitable for most people. The methods which used to adjust the elevation and depression of mandible include replacing component, screw, slot, and surface contact (Table 3.1-4).
Table 3.1-4 The adjustors of MAD (Elevation and depression)
Replace component Screw
U.S. Patent No. 5947724 [43] U.S. Patent No. 6055986 [44]
Slot Surface contact
3.1.4 Acting Force
The force acting on mandible to advance it can be divided into the pulling force and the pushing force. The pulling force usually acts from the anterior portion of upper mouthpiece to the posterior portion of the lower mouth piece, the pushing force acts oppositely. However, most connectors are connected between the same portion of upper and lower mouthpiece. The force acts as a perpendicular force on the connector, and it is used to prevent the mandible backward which is similar to the pushing force. Therefore, the acting force includes the perpendicular force, pushing force, and pulling force. In the mechanical terminology, they are shear force, compression force, and tensile force acting on the connector respectively (Table 3.1-5).
Table 3.1-5 Types of acting force of MAD
Perpendicular force Pushing force Pulling force
U.S. Patent No. 5365945 [30] U.S. Patent No. 6418933 [39] U.S. Patent No. 5755219 [38]
3.1.5 Lateral Movement
A function of allowing limited lateral movement during using the MAD is required. The lateral movement can prevent facial muscles from stiff and avoid the TMJ dysfunction. That will make the patients feel more comfortable and tolerated in using the MAD. The methods which have promoted to patents include using slots, linkages, surface contact, and elastic bands. Using the slot and the linkage to perform this function are better than the surface
ensure the therapeutic effect will not be affected by non-limited motion (Table 3.1-6).
Table 3.1-6 Types of lateral movement of MAD
Slot Surface contact
U.S. Patent No. 5868138 [47] U.S. Patent No. 5427117 [31]
Linkage Elastic band
U.S. Patent No. 6012920 [48] U.S. Patent No. 5755219 [38]
According to the patent reviews, more systematic results of analysis are presented. Those results can help to realize the disadvantages in prior products and find out the requirements. Further, those will be very useful for patent around that will prevent the new design from infringing other intelligence properties.
3.2 Products
The U.S. Food and Drug Administration (FDA) is responsible for protecting the public health by assuring the safety, efficacy, and security of human and veterinary drugs, biological products, medical devices, food supply, cosmetics, and products that emit radiation in the United States [49]. The mission of Center for Devices and Radiological Health (CDRH), one department of FDA, is to assure that new medical devices are safe and effective before they are on market. The FDA has classified all the medical devices into three classes. Each of those devices is assigned to one of three classes based on the level of control necessary to assure safety and effectiveness of the device. Everyone who wants to market Class I, II, and some III devices intended for human use in the U.S. must submit a premarket notification, 510(k), to FDA at least 90 days before marketing unless the device is exempt from 510(k) requirements. The oral appliances are assigned to the Class II devices [50] that must receive a 510(k) from FDA for the treatment of snoring or OSA. Therefore, all the OAs for snoring and/or OSA can be searched within which devices have received the 510(k) clearance and are available in the CDRH 510(k) database.
For the purpose of searching for all related products of the snoring or OSA treatment, the more effective method is to search by category rather than by other terms. Each category is referring to an individual product code. The intraoral devices for snoring and/or OSA are referring to the following product codes: “LRK”, Anti-Snoring Device; “LQZ”, Jaw Repositioning Device. There are totally 72 products in these two categories including all kinds of oral appliances. Depending on sifting all the products carefully, there are at least 16 products which are the adjustable two-pieces mandibular advancement devices. These devices with their specification are collected and listed in Table 3.2-1 and Table 3.2-2.
Table 3.2-1 List of adjustable MAD products
Model Applicant Approval Date
Klearway® Dr. Alan A. Lowe, Inc. 05/25/1995 Silencer® Silent Knights Ventures, Inc. 10/30/1995 Adjustable PM Positioner® Jonathan A. Parker, D.D.S. 02/08/1996
Herbst Appliance® Univ. Dental Assoc. Dept. of
Orthodontics 03/20/1996
TAP® Airway Management Inc. 01/24/1997
Silent Nite® Glidewell Laboratories 09/18/1997
EMA® Frantz Design, Inc. 09/29/1997
Adjustable TheraSnore® DISTAR, Inc. 11/12/1997
Snoring Control Device® Kenneth Hilsen 01/09/1998
Snore-Aid plus® Dental Imagineers, LLC 07/22/1999
NORAD® Dennis R. Bailey, DDS 05/28/2002
SUAD® Strong Dental Inc. 07/08/2003
OASYS Oral/Nasal Airway System® Mark Abramson, D.D.S., Inc. 08/26/2003 MDSA TM RJ & VK Bird Pty Ltd. 10/27/2004
SomnoMed MAS ® Somnomed Ltd 07/12/2005
TAP-T® Airway Management Inc. 07/12/2006
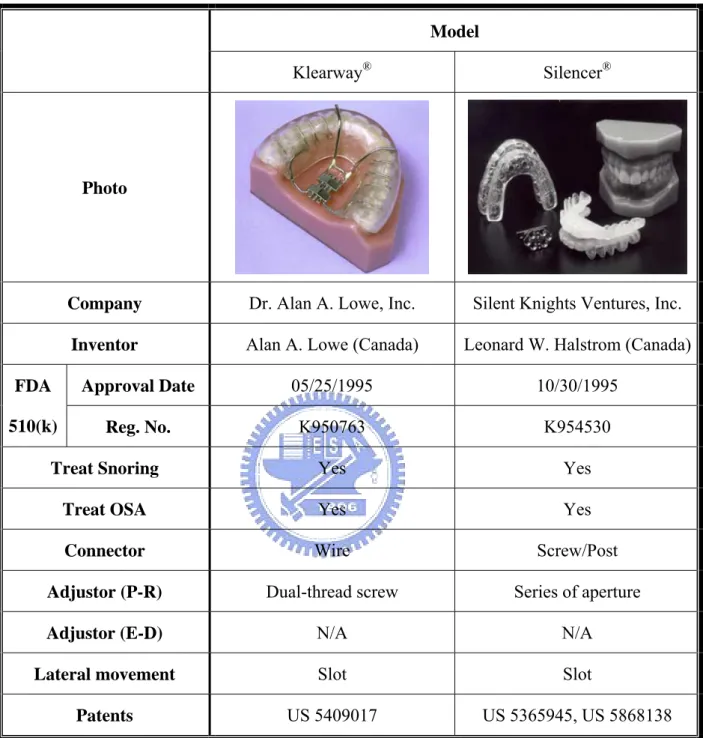
Table 3.2-2 Comparison of adjustable MAD products
Model
Klearway® Silencer®
Photo
Company Dr. Alan A. Lowe, Inc. Silent Knights Ventures, Inc. Inventor Alan A. Lowe (Canada) Leonard W. Halstrom (Canada)
Approval Date 05/25/1995 10/30/1995
FDA
510(k) Reg. No. K950763 K954530
Treat Snoring Yes Yes
Treat OSA Yes Yes
Connector Wire Screw/Post
Adjustor (P-R) Dual-thread screw Series of aperture
Adjustor (E-D) N/A N/A
Lateral movement Slot Slot
Patents US 5409017 US 5365945, US 5868138 (All rights of the pictures belong to individual incorporation respectively)
Table 3.2-2 Comparison of adjustable MAD products (cond.)
Model
Adjustable PM Positioner® Herbst Appliance®
Photo
Company Jonathan A. Parker, D.D.S.
Univ. Dental Assoc. Dept. of Orthodontics
Inventor Jonathan A. Parker (U.S.) (No data)
Approval Date 02/08/1996 03/20/1996
FDA
510(k) Reg. No. K955503 K955822
Treat Snoring Yes Yes
Treat OSA Yes Yes
Connector Wire Linkage
Adjustor (P-R) Dual-thread screw Screw
Adjustor (E-D) N/A Elastic band
Lateral movement Linkage Linkage
Patents US 5816799 (No data)
Table 3.2-2 Comparison of adjustable MAD products (cond.)
Model
TAP® Silent Nite®
Photo
Company SCHEU-DENTAL GmbH Glidewell Laboratories Inventor W. Keith Thornton (U.S.) (No data)
Approval Date 01/24/1997 09/18/1997
FDA
510(k) Reg. No. K964516 K972424
Treat Snoring Yes Post (Hook)
Treat OSA Yes Screw
Connector Post (Hook) Slot
Adjustor (P-R) Screw N/A
Adjustor (E-D) Slot US 6305376
Lateral movement Surface contact Elastic band
Patents US 6305376 (No data)
Table 3.2-2 Comparison of adjustable MAD products (cond.)
Model
EMA® Adjustable TheraSnore®
Photo
Company Frantz Design, Inc. DISTAR, Inc. Inventor Don E. Frantz (U.S.) Thomas E. Meade (U.S.)
Approval Date 09/29/1997 11/12/1997
FDA
510(k) Reg. No. K971794 K973038
Treat Snoring Yes Yes
Treat OSA Yes Yes
Connector Elastic band Elastic band
Adjustor (P-R) Replace component Replace component Adjustor (E-D) Replace component Replace component Lateral movement Elastic band Elastic band
Patents US 5947724, US 6109265 US 5947724, US 6109265 (All rights of the pictures belong to individual incorporation respectively)
Table 3.2-2 Comparison of adjustable MAD products (cond.)
Model
Snoring Control Device® Snore-Aid plus®
Photo
Company Ridgewood Dental Associates Dental Imagineers, LLC Inventor Kenneth L. Hilsen (U.S.) William A. Belfer (U.S.)
Approval Date 01/09/1998 07/22/1999
FDA
510(k) Reg. No. K963591 K991449
Treat Snoring Yes Yes
Treat OSA No Yes
Connector Interlocking member Post +Surface contact Adjustor (P-R) Interlocking member Elastic band (Bind posts)
Adjustor (E-D) N/A Surface contact
Lateral movement Surface contact Surface contact
Patents US 5611355 US 20030234022
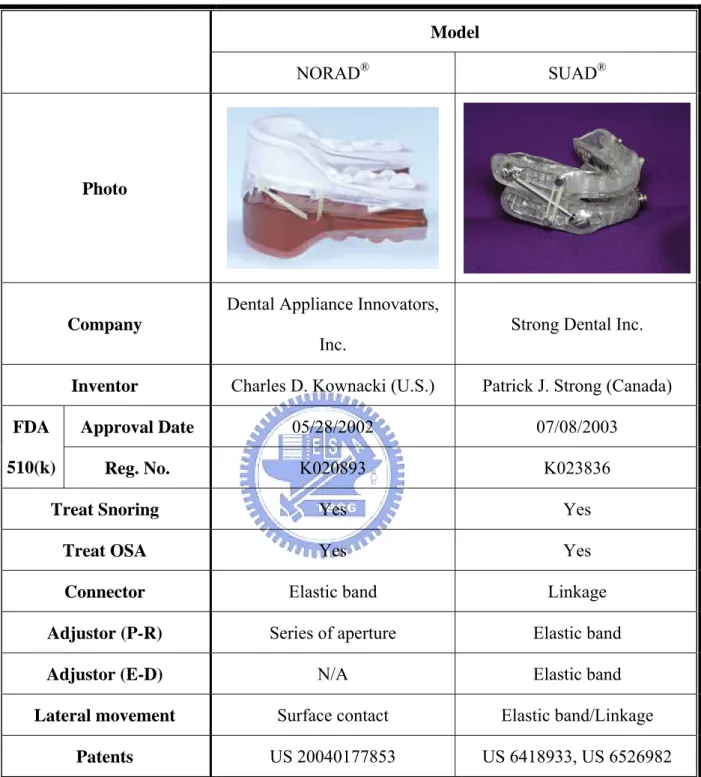
Table 3.2-2 Comparison of adjustable MAD products (cond.)
Model
NORAD® SUAD®
Photo
Company
Dental Appliance Innovators,
Inc. Strong Dental Inc.
Inventor Charles D. Kownacki (U.S.) Patrick J. Strong (Canada)
Approval Date 05/28/2002 07/08/2003
FDA
510(k) Reg. No. K020893 K023836
Treat Snoring Yes Yes
Treat OSA Yes Yes
Connector Elastic band Linkage
Adjustor (P-R) Series of aperture Elastic band
Adjustor (E-D) N/A Elastic band
Lateral movement Surface contact Elastic band/Linkage Patents US 20040177853 US 6418933, US 6526982 (All rights of the pictures belong to individual incorporation respectively)
Table 3.2-2 Comparison of adjustable MAD products (cond.)
Model
OASYS® MDSA®
Photo
Company Mark Abramson, D.D.S., Inc. RJ & VK Bird Pty Ltd. Inventor (No data) John Gaskell (Australia)
Approval Date 08/26/2003 10/27/2004
FDA
510(k) Reg. No. K030440 K042161
Treat Snoring Yes Yes
Treat OSA Yes Yes
Connector Wire Post (Hook)
Adjustor (P-R) Screw/Slot (Telescope) Screw
Adjustor (E-D) Surface contact N/A
Lateral movement Surface contact Surface contact
Patents (No data) US 6845774
![Fig. 2.1-2 A typical night’s sleep record of an average young adult [9]](https://thumb-ap.123doks.com/thumbv2/9libinfo/8040996.161890/26.892.217.720.757.1053/fig-typical-night-sleep-record-average-young-adult.webp)
![Fig. 2.1-3 Oral cavity [2]](https://thumb-ap.123doks.com/thumbv2/9libinfo/8040996.161890/28.892.266.671.507.940/fig-oral-cavity.webp)
![Table 2.2-3 Parameters measured in the Polysomnography [13]](https://thumb-ap.123doks.com/thumbv2/9libinfo/8040996.161890/34.892.120.818.156.463/table-parameters-measured-polysomnography.webp)
![Table 2.3-1 Typical reasons for CPAP noncompliance [4] No. Reasons 1 Nasal stuffiness and discharge](https://thumb-ap.123doks.com/thumbv2/9libinfo/8040996.161890/40.892.118.815.143.829/table-typical-reasons-noncompliance-reasons-nasal-stuffiness-discharge.webp)