Using Hospital Information System as A Basis for Clinical Decision Support
in Schizophrenic Patients
Chiung-Hsu, Chen
Taoyuan Psychiatric Center
forensic@typc.doh.gov.tw
Yu-Chuan, Li
Taipei Medical University
jack@tmu.edu.tw
I-Ren, Chiang
Taipei Medical University
ijchiang@tmu.edu.tw
Abstract
It was still controversial about the
effec-tiveness of treating schizophrenia patients by
second generation antipsychotics(SGAs) or first
generation antipsychotics(FGAs). We used
da-tabase extracted from our Hospital Information
System in Taoyuan Mental Hospital as a base for
clinical decision support system. Four years’
pharmacy prescription data were analyzed.
Treatment discontinuation was taken as primary
outcome for treating patients with different
an-tipsychotics. The duration of treatment, kinds
of antipsychotics, patient gender, age group of
patients were collected. Survival analysis
found the duration of treatment differed from
drug to drug statistically, and the difference
per-sisted even considering the influence of gender
and age group by Cox regression. The tool
could be applied to the other five major mental
hospitals, which had the same HIS, in Taiwan.
It was possible to use pharmacy data from
phar-macy-prescription data to construct a base for
clinical decision support system in schizophrenic
outpatients.
Keywords: Clinical decision support system,
schizophrenia, treatment discontinuation, HIS
1. Introduction
The treatment for schizophrenia had made remarking success after discovering chlorpromazine in 1950’. There were many antipsychotics with dopamine blocking activity in later years. Although they were effective in treating schizophrenic patients, they had many disadvan-tages. The most often happened side effect was ex-trapymidal symptoms. It occurred among about 70-80% patients and hence it made patients’ drug compliance poorer. The situation changed after finding Clozapine which caused fewer extrapymidal symptom side effects. Unfortunately, it might cause white blood cell count de-creased and therefore caused more severe complications. Clozapine disappeared later and it was used again owing to its remarkable effect in treating refractory schizophrenic patients in 1990’. There were so-called “Second Genera-tion Antipsychotics” from 1990’, including risperidone, olanzapine, quetiapine, ziprasidone…etc. The SGAs had treatment effects and fewer extrapymidal symptom side effects when compared with so-called “First Generation Antipsychotics”. Kane. J reported that SGAs were more effective and safer than FGAs.[1] Others found that it is
not true all the same.[2-6] Besides, it was still controver-sial whether SGAs could improve patients’ cognitive func-tion or not.[7] There were limited reports about longterm effects of SGAs, such as preventing patients’ relapse, im-proving patients’ social function, imim-proving patients’ qual-ity of life, and lowering caregivers’ burdens.[6, 8-9] There were many head-to-head studies comparing effec-tiveness of antipsychotics between one SGA and one FGA or between two SGAs. However, every study of this kind wasted many resources and a lot of manpower. There were many prospective studies comparing antipsychotics’ effectiveness with excellent data.[10-12] Since a deci-sion to continue or stop medications reflected the com-bined evaluation of efficacy and safety/tolerability of the treatment by the patient and clinician, they used “treatment discontinuation” as primary outcome[10]. This finding made it possible to do large comparison studies by infor-mation management and the results would be very helpful in clinical decision support system. This study tried to use outpatients’ pharmacy prescription database from hos-pital information system as a base for clinical decision support system about antipsychotics’ persisting use.
2. Materials and Methods
There were eight major mental hospitals which cared more than 50% of schizophrenic patients in Taiwan. The study was conducted at Taoyuan Mental Hospital which had 312 acute beds, 420 chronic beds and 280 beds for day-care. It was the largest mental hospital in east-south Asia and it served about one million and eight hundred thousands people. Taoyuan Mental Hospital had the same HIS with the other 43 large official hospitals in Taiwan. Six out of eight major mental hospitals used the same HIS. The developed tools could be applied to other hospitals easily.
Effectiveness for treating schizophrenia patients was hard to define. It included the impact of medication on controlling the various symptoms of illness, as well as the safety and tolerability of the illness.[10] The patients or the doctors would change antipsychotic if the drug is not “effective”. It needed a prospective study design and cost a lot of manpower and resources to collect all factors about effectiveness among different antipsychotics. Many of these causes were not available in Hospital In-formation System. Since “treatment discontinuation” was taken as primary outcome by large scale studies in the USA and the Europe[10-12], we took it as primary out-come in this study. This indicator was easy to define in HIS.
The data base of HIS didn’t follow the formal schema of relational database. Many attributes were put together in one column. Besides, it was complied by COBOL lan-guage which was different from current popular lanlan-guages. The supplier of HIS didn’t offer the schema of HIS data-base but only some definitions of columns. To resolve the difficulties list above, we dumped the HIS databases to Microsoft SQL server 2000 at first. Every column in da-tabase of outpatient service was analyzed step by step and be separated into different attributes. The HIS was ap-plied to Taoyuan Mental Hospital since July 2001. We focused on pharmacy prescription databases of outpatients service from Jan 1, 2002 to Dec 31, 2005. All schizo-phrenic patients with the first ICD code of “295”. The focus of medications were on major SGAs and some atypical antipsychotics, including Clozapine, risperidone, olanzapine, quetiapine, amisulpride, ziprasidone, and aripiprazole. Treatment discontinuation was the primary outcome.
Every schizophrenic patients prescribed with one of the interested antipsychotics would be counted for its
length of drug usage from the first prescribing date to the date of discontinuation Demographic data about patients such as gender, age,….etc were also gathered from HIS. We used SPSS 10.0 Chinese version in statistics. Kaplan–Meier survival curves and life table method were used to estimate the time to the discontinuation of treat-ment. Treatment groups were compared by using Cox proportional-hazards regression models. Demographic factors such as gender, age…etc were considered in Cox regression models.
3. Results
There were 2093 events during 2002 to 2005. The risperidone was the most popular use.(Table 1) We didn‘t have all interested antipsychotics until 2005. There were 1513 patients in 2093 events and 1100(72.70%) patients were prescribed with only one interested antipsychotic. There were 3(0.20%) patients prescribed with 6 kinds of interested antipsychotics. The gender difference between antipsychotics was noted Clozapine was more prescribed among males than females. Besides, the females pre-scribed with ziprasidone and aripiprazole were about twice of males.
Table 1 First prescription of antipsychotics (2002-2005)
Yr AMI ARI CLO LOD OLA QUE RIS ZIP
02 n.a. n.a. 98 69 68 45 134 n.a. 03 29 n.a. 46 40 84 71 142 26 04 36 n.a. 40 85 93 68 182 67
05 41 141 59 90 66 50 180 43
106 141 243 284 311 234 638 136 Yr= Year; AMI= amisulpride; ARI= aripiprazole; CLO= clozap-ine; LOD= lodopclozap-ine; OLA= olanzapclozap-ine; QUE= quetiapclozap-ine; RIS= risperidone; ZIP= ziprasidone; n.a.=not appliable
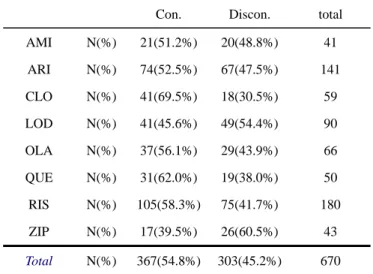
Table 2 Discontinuation rate among antipsychotics in 2005
Continuation(Con.) v.s. discontinuation(Discon.)
Con. Discon. total
AMI N(%) 21(51.2%) 20(48.8%) 41 ARI N(%) 74(52.5%) 67(47.5%) 141 CLO N(%) 41(69.5%) 18(30.5%) 59 LOD N(%) 41(45.6%) 49(54.4%) 90 OLA N(%) 37(56.1%) 29(43.9%) 66 QUE N(%) 31(62.0%) 19(38.0%) 50 RIS N(%) 105(58.3%) 75(41.7%) 180 ZIP N(%) 17(39.5%) 26(60.5%) 43 Total N(%) 367(54.8%) 303(45.2%) 670 X2=14.804 df=7 p=0.039
The later results were focused on 2005 when all in-terested antipsychotics were included for comparison. There were 670 events by 578 patients in 2005. 501 (86.68%) patients are prescribed with only one interested drug. The age distribution was compatible with schizo-phrenia patients’. The average discontinuation rate among antipsychotics was about 45.2%. Those with lo-dopine and ziprasidone had higher discontinuation rate.(Table 2)
The comparison of different antipsychotics’ survival curves by life-table method revealed statistic different be-tween drugs. (Figure 1) The Kaplan–Meier survival curves also revealed the same result. Statistical signifi-cant among different antipsychotics persisted after consid-ering demographic data such as gender and age group by Cox regression.
life table method
time(day) to discontinuation
400
300
200
100
0
cum
ula
ti
ve
s
ur
vi
va
l
1.0
.9
.8
.7
.6
.5
.4
.3
.2
.1
0.0
drug
ZIP
RIS
QUE
OLA
LOD
CLO
ARI
AMI
Overall comparison statistic= 17.961, df.=7, p=0.0121 Figure 1 Life-table survival curve of antipsychotics in 2005
4. Discussion
There were many factors affecting doctors’ prescrip-tion pattern, such as lack of efficacy, tolerability issue ow-ing to side effect, the official policy by National Health Insurance, and coping strategy developed by hospitals. Patient’s condition such as poor disease insight compro-mised drug compliance and patients dropped out later. Even under the influences of so many factors, it was said
that treatment continuation was a good indicator for treat-ment effect.[11, 12] It provided a convenient way to han-dle the complicated effects of antipsychotics’ advantages and disadvantages. We tried to use pharmacy prescrip-tion database from HIS to compare the outcome of differ-ent antipsychotics’ effect on patidiffer-ents.
Selection bias was inevitable in such study design and could not be managed by statistics. Those patients pre-scribed with clozapine were quite different from those
with aripiprazole in clinical setting. There were more males in refractory schizophrenic patients and it might ex-plain the gender difference between clozapine and other antipsychotics. The ratio of female to male was about two in patients prescribed with ziprasidone and aripipra-zole. It might be due to the least likely causibility of hy-perprolactinemia by these two antipsychotics. However, when stratifying the age group and gender, we could have separated the different reasons for prescription antipsy-chotics. It could be further developed as a clinical deci-sion support system. For examples: a 27 year-old female diagnosed as schizophrenia for years came to outpatient service for her relapsing psychotic symptoms, which an-tipsychotic was preferred? With this clinical decision support system, the doctor chose “gender= female” and “age group= 20-30” on the screen and the computer would show him that those with the same characteristic taken dif-ferent antipsychotics have difdif-ferent survival curves. He could make decision by himself referring this system fi-nally.
Further efforts were needed. We calculated the treatment duration by start-date and end-date. However, there were patients who take some antipsychotic at first, change to another antipsychotic later, and take the original antipsychotic finally. In this kind of situation, we overly estimated the treatment duration and hence this system gave us an optimistic suggestion. It might compromise patients’ best interest. We would try to review every visit of patients and separate those discontinuited visits in later studies.
Some might recommend to do the same thing from NHI database. The availability of different antipsy-chotics of interested differed from hospitals to hospitals. There might be only one choice in one hospital and six choices in the other hospitals. However, it was possible
if we limited our topic on some major mental hospitals. The other five major mental hospitals had the same HIS and this result could be applied to other hospital easily. We could also try to set up a clinical decision support system by using databases of six major mental hospital with the same HIS to get more objective results. .
5. Conclusion
We could see the brightening future to use pharmacy database to construct a clinical decision support system in schizophrenia outpatients, disregarding the underdevel-oped electric medical records. It would be more promis-ing if we further manage the data and collect databases from the other five major mental hospitals with the same HIS.
6. Reference
[1] Kane J, Honigfeld G, Singer J, Meltzer H. Clozapine for the treatment-resistant schizophrenic: a double-blind comparison with chlorpromazine. Arch Gen Psychiatry 1988;45: 789-96.
[2] Leucht S, Pitschel-Walz G, Abraham D, Kissling W. Efficacy and extrapyramidal side-effects of the new antipsychotics olan-zapine, quetiapine, risperidone, and sertindole compared to con-ventional antipsychotics and placebo: a meta-analysis of ran-domized controlled trials. Schizophr Res 1999;35:51-68.
[3] Geddes J, Freemantle N, Harrison P, Bebbington P. Atypical antipsychotics in the treatment of schizophrenia: systematic over-view and meta-regression analysis. BMJ 2000;321: 1371-6. Wahlbeck K, Tuunainen A, Ahokas A, Leucht S. Dropout rates in randomised antipsychotic drug trials. Psychopharmacology (Berl) 2001;155: 230-3.
[4] Davis JM, Chen N, Glick ID. A metaanalysis of the efficacy of second-generation antipsychotics. Arch Gen Psychiatry 2003; 60: 553-64.
[5] Leucht S, Wahlbeck K, Hamann J, Kissling W. New genera-tion antipsychotics versus low-potency convengenera-tional antipsy-chotics: a systematic review and meta-analysis. Lancet 2003; 361: 1581-9.
[6] Leucht S, Barnes TRE, Kissling W, Engel RR, Correll C, Kane JM. Relapse prevention in schizophrenia with new-generation antipsychotics: a systematic review and explora-tory meta-analysis of randomized, controlled trials. Am J Psy-chiatry 2003; 160: 1209-22.
[7] Keefe RS, Silva SG, Perkins DO, Lieberman JA. The effects of atypical antipsychotic drugs on neurocognitive impairment in schizophrenia: a review and meta-analysis. Schizophr Bull 1999; 25:201-22.
[8] Rosenheck R, Perlick D, Bingham S, et al. Effectiveness and cost of olanzapine and haloperidol in the treatment of schizo-phrenia: a randomized controlled trial. JAMA 2003; 290: 2693-702.
[9] Csernansky JG, Mahmoud R, Brenner R. A comparison of risperidone and haloperidol for the prevention of relapse in pa-tients with schizophrenia. N Engl J Med 2002; 346: 16-22.
[10] Swartz MS, Perkins DO, Stroup TS, McEvoy JP, Nieri JM, Haak DC. Assessing clinical and functional outcomes in the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia trial. Schizophr Bull 2003; 29: 33-43.
[11] Lieberman JA. Stroup TS. McEvoy JP. Swartz MS. Rosen-heck RA. Perkins DO. Keefe RS. Davis SM. Davis CE. Lebowitz BD. Severe J. Hsiao JK. Clinical Antipsychotic Trials of Inter-vention Effectiveness (CATIE) Investigators. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005; 353: 1209-23.
[12] Fleischhacker WW. Keet IP. Kahn RS. EUFEST Steering Committee. The European First Episode Schizophrenia Trial (EUFEST): rationale and design of the trial. Schizophrenia Re-search. 78(2-3):147-56, 2005 Oct 15.