Date 2012/Sep/19
Ref.: GGI-0195-2012(Revision 1) Type of manuscript :Letter to editor
Manuscript title :Association between head injury and Parkinson’s disease: an observation in Taiwan
Running head:head injury and Parkinson’s disease Authors' full names:
Shih-Wei Lai, MD1,2; Kuan-Fu Liao, MD and MS 3,4,5; Cheng-Li Lin, MS6,7;
Fung-Chang Sung, PhD, MPH 6,7
(The first two authors contributed equally to this study.)
1School of Medicine, and 6Department of Public Health, China Medical
University, Taichung, 404, Taiwan
2Department of Family Medicine, and 7Management Office for Health Data,
China Medical University Hospital, Taichung, 404, Taiwan
3Department of Internal Medicine, Taichung Tzu Chi General Hospital,
Taichung, 427, Taiwan
4School of Medicine, Tzu Chi University, Hualien, 970, Taiwan
5Department of Health Care Administration, Central Taiwan University of
Science and Technology, Taichung, 406, Taiwan
Corresponding author:
Fung-Chang Sung, PhD, MPH
Professor, College of Public Health, China Medical University No. 91, Hsueh-Shih Road, Taichung 404, Taiwan
Phone: 886-4-2206-2295; fax: 886-4-2201-9901 e-mail: fcsung1008@yahoo.com
To editor,
Although the etiology of Parkinson's disease remains unsettled, an extensive evidence has shown that family history, occupational, genetic and environmental factors including head injury are associated with this disease 1-3. To date, little evidence is
available about the association between head injury and Parkinson’s disease in Taiwan. Therefore, using a nationwide representative database of National Health Insurance in Taiwan, we conducted this observational study to examine this issue. The insurance program details can be found in previous studies. Based on the International Classification of Diseases 9th Revision-Clinical Modification (ICD-9 codes), there
were 8678 patients aged 40 years or older with newly diagnosed head injury as the head injury group (ICD-9 codes 850-854 and 959.01, 4555 men and 4123 women, mean age 59.4 ± 12.3 years, mean follow-up period 6.44 ± 2.73 years), and 34712 subjects without head injury as the non-head injury group (18220 men and 16492 women, mean age 59.3 ±12.3 years, mean follow-up period 6.68 ± 2.60 years), from 2000 to 2010. Both groups were matched with sex, age and the endpoint. The endpoint for head injury patients was defined as the date of diagnosing Parkinson's disease (ICD-9 codes 332).
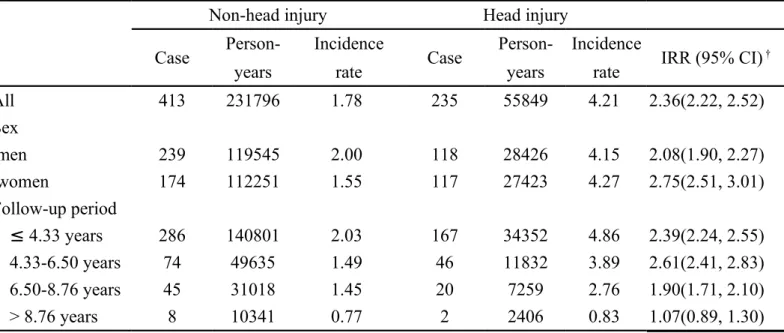
The head injury group had significantly higher incidence of Parkinson's disease than the non-head injury group did (4.21 vs. 1.78 per 1000 person-years, 95% CI
2.22-2.52). We further divided the follow-up period into 25th percentile, 50th percentile, and 75th percentile of the total follow-up time. The incidence of Parkinson's disease was the highest (4.86 per 1000 person-years) when the follow-up period was less than 4.33 years. The incidence decreased to 0.83 per 1000 person-years when the follow-up period was more than 8.76 years. That is, the incidence appears to decrease with longer follow-up time (Table 1).
So far, epidemiological studies have shown that prior head injury was associated with the risk of Parkinson's disease (odds ratio, range from 3.8 to 11). In this present study, the incidence rate ratio (IRR) of Parkinson's disease was 2.36 for the head injury group, when compared with the non-the head injury group. Moreover, we could not differentiate whether head injury was accompanied by loss of consciousness because there was no such record in this database. Similarly, we could not differentiate
whether head injury was only one episode or repeated. Interestingly, we found that the incidence of Parkinson's disease seemed to be decreased with longer follow-up time. How long Parkinson's disease would develop after head injury could not be
completely elucidated in this present study. The reason why the incidence of
Parkinson’s disease after dead injury was the highest in the follow-up period less than 4.33 years is still not clear, but it could be partially explained by the mechanism that those with early undiagnosed Parkinson's disease might initially present with motor
dysfunction, which further increased the likelihood of head injury. Thus, these patients with head injury should receive close surveillance for the potential of Parkinson's disease.
We conclude that head injury is associated with increased risk of Parkinson's disease in Taiwan. Further studies are needed to confirm the cause-effect relationship between head injury and Parkinson's disease.
Funding
This study was supported in part by grants from Taiwan Department of Health Clinical Trial and Research Center of Excellence (DOH101-TD-B-111-004), the Cancer Research Center of Excellence (DOH 101-TD-C-111-005), and the National Science Council (NSC 100-2621-M-039-001). The funding agencies did not
influence the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Acknowledgements
The authors thank the National Health Research Institute in Taiwan for providing the insurance claims data.
Conflict of Interest Statement
References
[1] Taylor CA, Saint-Hilaire MH, Cupples LA, et al. Environmental, medical, and family history risk factors for Parkinson's disease: a New England-based case control study. Am J Med Genet 1999; 88: 742-9.
[2] Tsai CH, Lo SK, See LC, et al. Environmental risk factors of young onset Parkinson's disease: a case-control study. Clin Neurol Neurosurg 2002; 104: 328-33. [3] Das K, Ghosh M, Nag C, et al. Role of familial, environmental and occupational factors in the development of Parkinson's disease. Neurodegener Dis 2011; 8: 345-51. [4] Lai SW, Su LT, Lin CH, Tsai CH, Sung FC, Hsieh DP. Polypharmacy increases the risk of Parkinson's disease in older people in Taiwan: a population-based study.
Psychogeriatrics 2011; 11: 150-6.
[5] Lai SW, Lin CH, Liao KF, Su LT, Sung FC, Lin CC. Association between polypharmacy and dementia in older people: A population-based case-control study in Taiwan. Geriatr Gerontol Int 2012; 12: 491-98.
[6] Bower JH, Maraganore DM, Peterson BJ, McDonnell SK, Ahlskog JE, Rocca WA. Head trauma preceding PD: a case-control study. Neurology 2003; 60: 1610-5. [7] Goldman SM, Tanner CM, Oakes D, Bhudhikanok GS, Gupta A, Langston JW. Head injury and Parkinson's disease risk in twins. Ann Neurol 2006; 60: 65-72.
Table 1. Incidence density of Parkinson's disease for head injury group and non-head injury group
Non-head injury Head injury
Case Person- Incidence Case Person- Incidence IRR (95% CI) †
years rate years rate
All 413 231796 1.78 235 55849 4.21 2.36(2.22, 2.52) Sex men 239 119545 2.00 118 28426 4.15 2.08(1.90, 2.27) women 174 112251 1.55 117 27423 4.27 2.75(2.51, 3.01) Follow-up period ≤ 4.33 years 286 140801 2.03 167 34352 4.86 2.39(2.24, 2.55) 4.33-6.50 years 74 49635 1.49 46 11832 3.89 2.61(2.41, 2.83) 6.50-8.76 years 45 31018 1.45 20 7259 2.76 1.90(1.71, 2.10) > 8.76 years 8 10341 0.77 2 2406 0.83 1.07(0.89, 1.30)
Incidence rate: per 1000 person-years