Long-Term Outcomes of Living Kidney Donors Over the Past 28 Years
in a Single Center in Taiwan
S.-F. Tsai, K.-H. Shu, H.-C. Ho, M.-J. Wu, C.-H. Cheng, J.-D. Lian, M.-C. Wen, C.-K. Su, T.-M. Yu,
Y.-W. Chuang, S.-T. Huang, and C.-H. Chen
ABSTRACT
Background.
The chronic shortage of kidneys for transplantation has increased the
number of living donations, but demand remains high, which has created a long waiting list
of end-stage kidney disease patients. Donors with decreased renal mass may suffer a higher
risk of developing proteinuria, hypertension (HTN), and chronic renal disease (CKD)
during long-term follow-up.
Methods.
We retrospectively retrieved medical data of living kidney donors at our
hospital over the past 28 years.
Results.
There were 45 male and 60 female donors with a mean donation age of 46.34
⫾
12.47 years (range
⫽ 20–70y). The mean follow-up duration was 4.67 ⫾ 4.78 years. The
serum creatinine (Cr) at donation was 0.93
⫾ 0.22 mg/dL, while the latest Cr was 1.26 ⫾
0.45 mg/dL (P
⬍ .001). The mean age at follow-up was 50.95 ⫾ 14.57 years. At last
follow-up, eight subjects (7.6%) displayed HTN requiring treatment, 10 (9.5%),
protein-uria and 55.4%, an estimated glomerular filtration rate (eGFR) of less than 60 mL/min,
including one with diabetic nephropathy at 10 years after donation who required long-term
hemodialysis. Although gender did not correlate with occurrence of HTN, proteinuria, and
CKD, the occurrence of CKD was associated with age at donation (P
⬍ .001, odds ratio
[OR]
⫽ 1.076), and age at follow-up (P ⬍ .001, OR ⫽ 1.071). HTN donors were older (P ⫽
.036, OR
⫽ 1.057) with longer follow-up durations (P ⫽ .007, OR ⫽ 1.166) and had higher
Cr values at donation (P
⫽ .044, OR ⫽ 94.4). Donors with proteinuria were not related to
gender, follow-up duration, initial Cr, warm ischemic time, or duration of admission.
eGFR was indeed worse after donation (P
⫽ .002).
Conclusions.
Our results indicated a significant proportion of living donors may develop
CKD upon long-term follow-up. The factors affecting donor risk of CKD were baseline
renal function, older age, and duration after kidney donation.
R
ENAL TRANSPLANTATION especially from livingrenal donors is the treatment of choice for end-stage renal disease.1A meta-analysis showed that proteinuria and loss of renal function may occur in living renal donors.2 However, there is only one study of Chinese living kidney
donors,3it including a small number of patients. Therefore, we performed a retrospective analysis to assess the long-term follow-up of renal function, proteinuria, and hyper-tension (HTN) among Chinese living donors, investigating possible risk factors for deterioration of renal function.
From the Division of Nephrology, Department of Internal Medicine (S.-F.T., K.-H.S., M.-J.W., C.-H.C., T.-M.Y., Y.-W.C., S.-T.H., C.-H.C.), Department of Pathology (M.-C.W.), and Divi-sion of Urology (H.-C.H., C.-K.S.), Taichung Veterans General Hospital; School of Medicine (C.-H.C.), China Medical Univer-sity; Department of Life Science (C.-H.C.), Tunghai UniverUniver-sity;
and School of Medicine (K.-H.S., M.-J.W., C.-H.C., J.-D.L., C.-H.C.), Chung Shan Medical University, Taichung, Taiwan.
Address reprint requests to Cheng-Hsu Chen, MD, PhD, Division of Nephrology, Department of Medicine, Taichung Vet-erans General Hospital, 160, Chung-Kang Road, Section 3, Taichung, 407, Taiwan. E-mail:cschen920@yahoo.com
© 2012 by Elsevier Inc. All rights reserved. 0041-1345/–see front matter 360 Park Avenue South, New York, NY 10010-1710 doi:10.1016/j.transproceed.2011.12.024
METHODS
Selection and Description of Participants
From May 1983 through March 2011, we performed 105 of living donor kidney transplantations. We evaluated serum creatinine (Cr; mg/dL), urine, blood pressure, renal sonography, and effective renal plasma flow (ERPF). Infection, malignancy, on liver disease was excluded before donation. Because some donations took place in the 1980s, some individuals donated a kidney despite an overall estimated glomerular filtration (eGFR) of less than 80 mL/min. Renal function was evaluated by Cr (mg/dL) and eGFR, using the formula of modification of diet in renal disease (MDRD), namely, eGFR (mL/min/1.73 m2)⫽ 186 ⫻ Scr⫺1.154⫻ Age⫺0.203⫻ 0.742 (if
female).4We collected the following data: gender, age at donation,
age at follow-up, follow-up duration (years), Cr (mg/dL) initially and at follow-up, eGFR (mL/min) initially and at follow-up, bilateral ERPF before operation (mL/min), warm ischemic time (minutes), and duration of hospital stay (days). We defined pro-teinuria as documented by urine analysis ⱖ 1⫹ or daily urine protein⬎ 150 mg, and HTN as systolic blood pressure of ⱖ140 mm Hg or diastolic blood pressure ofⱖ90 mm Hg or the prescription of an antihypertensive drug. Renal functional deterioration was evaluated via the eGFR decline, the eGFR decline per year, and eGFR ⬍ 60 mL/min, HTN, or proteinuria. This study was ap-proved by our Ethics Committee (IRB number CE1115).
Statistical Methods
Data were expressed as mean values and standard deviations or percentages. Comparisons between male and female donors were performed using the Mann-Whitney U test (for continuous vari-ables) or the chi-square test (for categorical varivari-ables). Paired Student t tests were used to compare initial and follow-up renal function values (Cr and eGFR). Risk factors for HTN, proteinuria, and eGFR⬍ 60 mL/min were analyzed by logistic regression model (presented as odds ratio [OR], P values and 95% confidence intervals). Risk factors for eGFR changes and eGFR decline per year were analyzed using a general linear regression model and presented as P values. A P value⬍ .05 was considered statistically
significant. All analyses were performed with SPSS version 12.0 software.
RESULTS
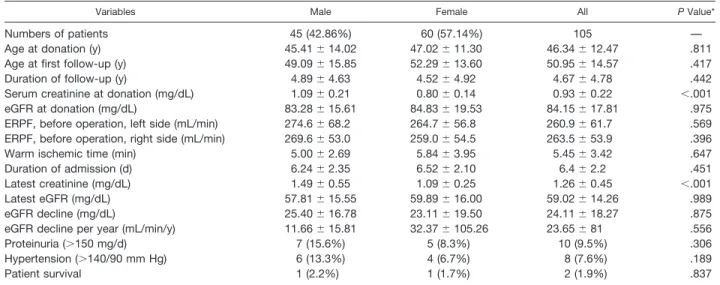
There were no differences in donor parameters between genders as shown inTable 1, some for Cr at donation (male: 1.09⫾ 0.21 mg/dL vs female: 0.80 ⫾ 0.14 mg/dL; P ⬍ .001) and Cr at follow-up (male: 1.49 ⫾ 0.55 mg/dL vs female: 1.09⫾ 0.25 mg/dL, P ⬍ .001). This observation may reflect the natural difference in muscle mass between men and women. The mean age at donation was 46.34 years and the mean follow-up duration 4.67 years. Renal function at donation was a Cr concentration of 0.93 mg/dL and an eGFR of 84.15 mL/min. Warm ischemia duration was 5.45 minutes and duration of admission was 6.4 days. There were no complications in any of the 105 donors.
After a mean follow-up of 4.67 years, mean decrement in eGFR was 24.11 mL/min. Moreover, there were 10 donors (9.5%) with proteinuria and 8 (7.6%) with HTN. Renal functional decline was found observed between donation and follow-up time with Cr concentration of⫹0.33 mg/dL (P⫽ .005) namely, from 0.93 ⫾ 0.22 to 1.26 ⫾ 0.45 mg/dL and eGFR of ⫺25.13 mL/min (P ⫽ .002) namely, from 84.15⫾ 17.81 to 59.02 ⫾ 14.26 ml/min; data not shown).
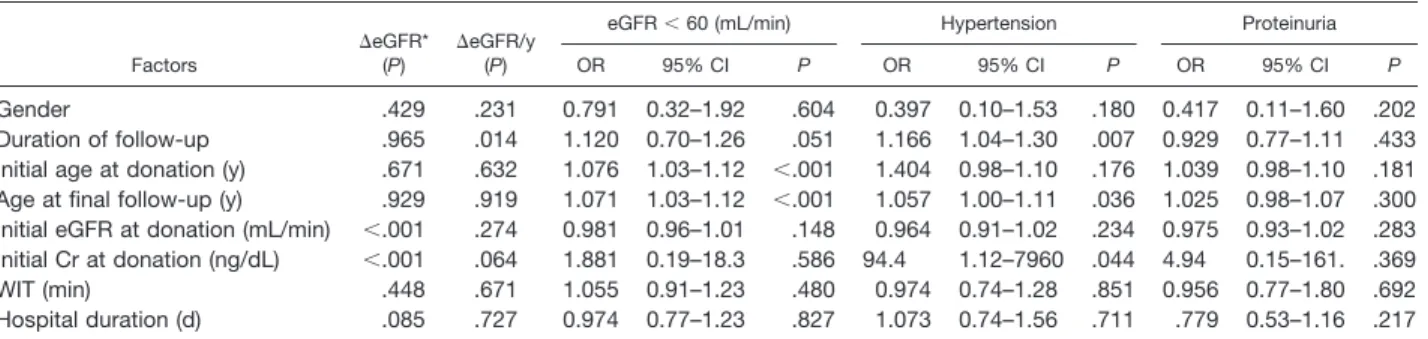
Possible factors associated with renal functional deterio-ration (eGFR decline, HTN, and proteinuria) are listed in
Table 2. Gender, warm ischemic time, and duration of admission were not related to any of the three parameters. Longer follow-up duration caused a greater decline of eGFR per year (P ⫽ .014), and HTN (P ⫽ .007, OR ⫽ 1.166). At follow-up, there was a greater likelihood of eGFR⬍ 60 min/mL (P ⬍ .001, OR ⫽ 1.071) and HTN (P ⫽ 0.036, OR ⫽ 1.057) among older compared with younger donors. Poorer baseline renal function (eGFR and Cr) was associated with greater eGFR decline (both P ⬍ .001).
Table 1. Characteristics of the Kidney Donor Population
Variables Male Female All P Value*
Numbers of patients 45 (42.86%) 60 (57.14%) 105 — Age at donation (y) 45.41⫾ 14.02 47.02⫾ 11.30 46.34⫾ 12.47 .811 Age at first follow-up (y) 49.09⫾ 15.85 52.29⫾ 13.60 50.95⫾ 14.57 .417 Duration of follow-up (y) 4.89⫾ 4.63 4.52⫾ 4.92 4.67⫾ 4.78 .442 Serum creatinine at donation (mg/dL) 1.09⫾ 0.21 0.80⫾ 0.14 0.93⫾ 0.22 ⬍.001 eGFR at donation (mg/dL) 83.28⫾ 15.61 84.83⫾ 19.53 84.15⫾ 17.81 .975 ERPF, before operation, left side (mL/min) 274.6⫾ 68.2 264.7⫾ 56.8 260.9⫾ 61.7 .569 ERPF, before operation, right side (mL/min) 269.6⫾ 53.0 259.0⫾ 54.5 263.5⫾ 53.9 .396 Warm ischemic time (min) 5.00⫾ 2.69 5.84⫾ 3.95 5.45⫾ 3.42 .647 Duration of admission (d) 6.24⫾ 2.35 6.52⫾ 2.10 6.4⫾ 2.2 .451 Latest creatinine (mg/dL) 1.49⫾ 0.55 1.09⫾ 0.25 1.26⫾ 0.45 ⬍.001 Latest eGFR (mg/dL) 57.81⫾ 15.55 59.89⫾ 16.00 59.02⫾ 14.26 .989 eGFR decline (mg/dL) 25.40⫾ 16.78 23.11⫾ 19.50 24.11⫾ 18.27 .875 eGFR decline per year (mL/min/y) 11.66⫾ 15.81 32.37⫾ 105.26 23.65⫾ 81 .556 Proteinuria (⬎150 mg/d) 7 (15.6%) 5 (8.3%) 10 (9.5%) .306 Hypertension (⬎140/90 mm Hg) 6 (13.3%) 4 (6.7%) 8 (7.6%) .189 Patient survival 1 (2.2%) 1 (1.7%) 2 (1.9%) .837
Data are expressed as n (%) for categorical variables and mean⫾ standard deviation (range) for continuous variables. EGFR, estimated glomerular filtration rate [186.3⫻ serum creatinine⫺1.154⫻ age⫺0.203⫻ 1.212 (if patient is black) ⫻ 0.742 (if female)]; ERPF, effective renal plasma flow.
*Compared between males and females.
Donors with higher baseline Cr values showed higher blood pressure (P⫽ .044, OR ⫽ 94.4).
DISCUSSION
The prognosis for living renal transplant donors has been widely discussed. A meta-analysis of 36 studies from 27 countries including 5048 donors was performed by Garg et al in 2006.2 Surprisingly, the meta-analysis only included one study on a Chinese population, namely that conducted by Chen et al in 1992.3There were only 76 patients in the Chinese study and data were analyzed 20 years ago. There-fore, it is necessary to investigate the prognosis of living Chinese donors in the present era. After a mean follow-up of 4.67 years, eGFR had declined to 59.02 mL/min, which was far worse than the mean rate among all 36 studies in the systemic review, namely, 86 mL/min after a 6-year follow-up.2The reason that the donor prognosis was far worse in our population may be explained by our use of the eGFR
estimates (MDRD-eGFR [mL/min/1.73 m2] ⫽ 186 ⫻
Scr⫺1.154 ⫻ Age⫺0.203 ⫻ 0.742 [if female]).4 The original eGFR is not suitable for Chinese patients, and we corrected the abbreviated (glomerular filtration rate ⫽ 175 ⫻ Scr⫺1.234⫻ Age⫺0.179 ⫻ 0.79 (if female)) as suggested by Ying-Chun Ma et al.5The use of eGFR led to a misclassi-fication of stage of chronic kidney disease (CKD) due to ethnic physiological differences, which was also detected in a study by Yazawa et al.6
The first study of a Chinese population with a relatively large number of donors (n⫽ 141) with 5-year follow-up was performed by Gong et al in 2011.7There was no significant renal functional deterioration at the end of the 5-year follow up compared with pre-donation renal status, which was similar to the findings of the abovementioned system-atic review.2 Nevertheless, our donors did show a worse eGFR after a mean follow-up of 4.67 years after donation (P⫽ .002). There are two possible reasons for the conflict-ing results. First, ours was a 28-year experience of livconflict-ing renal transplantation in a single hospital. The well-accepted guidelines for the care of living donors were published by the Amsterdam Forum in 2005.8An eGFR of more than 80 mL/min is considered to be an essential criterion for donor eligibility at the moment. The mean eGFR at donation in
the present study was 84.14 mL/min in recent years, but it was just 67.46 mL/min before 2005; 65.5% of donors had an eGFR ⬍ 80 mL/min. After 2005, 46.2% of donors had an eGFR of ⬍80 mL/min. The selection criteria have im-proved over time, but they were still less strict for living kidney donors. Second, an eGFR of 119.5 mL/min before donation was reported by Gong et al in 20117; it was much lower (84.15 mL/min) among our population. After unine-phrectomy, the residual kidney must work harder, produc-ing a greater likelihood of hyperfiltration injury.
Preoperative eGFR has long been viewed as the chief indication of deterioration of eGFR,8 –10 which was also observed in this study. If the eGFR is too low or the Cr is too high at donation, the decline of eGFR will be greater during follow-up (P⬍ .001). In addition, a higher initial Cr value may cause worse HTN (P⫽ .044, OR ⫽ 0.044). There was a trend (P ⫽ .064) to a higher Cr leading to a faster decline in eGFR among our donors. Therefore, worse initial renal function, whether defined by lower eGFR or higher Cr, leads to a greater decline of eGFR after dona-tion.
Older age at donation and older age at follow-up both significantly correlated with the development of CKD among donors (eGFR⬍ 60 mL/min; both P ⬍ .001). There was a trend (P⫽ .051) for more CKD to be observed with longer follow-up durations. These factors indicated that renal function in the donor’s remaining kidney may be more susceptible to the deterioration that accompanies the aging process. Greater glomerular hypertension in older com-pared with younger donors causes more glomerulosclerosis and further renal functional deterioration.11Age at dona-tion denotes baseline renal funcdona-tion, and duradona-tion of follow-up denotes duration of hyperfiltration injury. Age at last follow-up can be regarded as the final indicator of renal function, which is the sum of baseline renal function and hyperfiltration injury. Even young donors with good base-line renal function suffer from renal functional impairment after a long follow-up period.
There were some limitations to this study. It was retro-spective with a relatively small population in one single center.
Table 2. Multivariate Analysis of Risk Factors With Renal Function Deterioration
Factors
⌬eGFR* (P)
⌬eGFR/y (P)
eGFR⬍ 60 (mL/min) Hypertension Proteinuria
OR 95% CI P OR 95% CI P OR 95% CI P
Gender .429 .231 0.791 0.32–1.92 .604 0.397 0.10–1.53 .180 0.417 0.11–1.60 .202 Duration of follow-up .965 .014 1.120 0.70–1.26 .051 1.166 1.04–1.30 .007 0.929 0.77–1.11 .433 Initial age at donation (y) .671 .632 1.076 1.03–1.12 ⬍.001 1.404 0.98–1.10 .176 1.039 0.98–1.10 .181 Age at final follow-up (y) .929 .919 1.071 1.03–1.12 ⬍.001 1.057 1.00–1.11 .036 1.025 0.98–1.07 .300 Initial eGFR at donation (mL/min) ⬍.001 .274 0.981 0.96–1.01 .148 0.964 0.91–1.02 .234 0.975 0.93–1.02 .283 Initial Cr at donation (ng/dL) ⬍.001 .064 1.881 0.19–18.3 .586 94.4 1.12–7960 .044 4.94 0.15–161. .369 WIT (min) .448 .671 1.055 0.91–1.23 .480 0.974 0.74–1.28 .851 0.956 0.77–1.80 .692 Hospital duration (d) .085 .727 0.974 0.77–1.23 .827 1.073 0.74–1.56 .711 .779 0.53–1.16 .217
eGFR, estimated glomerular filtration rate; OR, odds ratio; CI, confidence interval; Cr, creatinine; WIT, warm ischemia time. *Change between donation and time of follow-up.
In conclusion, stricter criteria should be established for living donor among the Chinese population to obtain better renal function. Younger donors with good baseline renal function will enjoy better renal function after donation. However, our long-term follow-up data indicated that even young donors eventually experience renal functional im-pairment with longer duration of follow-up.
REFERENCES
1. US Renal Data System: USRDS 2007 annual data report: atlas of chronic kidney disease and end-stage renal disease in the United States. Bethesda, MD: National Institutes of Health, Na-tional Institute of Diabetes and Digestive and Kidney Diseases; 2007
2. Garg AX, Muirhead N, Knoll G, et al: Donor Nephrectomy Outcomes Research (DONOR) Network. Proteinuria and reduced kidney function in living kidney donors: a systematic review, meta-analysis, and meta-regression. Kidney Int 70:1801, 2006
3. Chen HW, Lai MK, Chu SH, et al: Long-term follow-up of living related donors at a single center in Taiwan. Transplant Proc 24:1440, 1992
4. Giovannetti S, Barsotti G: In defense of creatinine clearance. Nephron 59:11, 1991
5. Ying-Chun M, Li Z, Jiang-Hua C, et al: Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol 17:2937, 2006
6. Yazawa M, Kido R, Shibagaki Y, et al: Kidney function, alb uminuria and cardiovascular risk factors in post-operative living kidney donors: a single-center, cross-sectional study. Clin Exp Nephrol 15:514, 2011
7. Gong NQ, Ming CS, Zeng FJ, et al: Renal function of donors and recipients after living donor kidney transplantation in a Chinese cohort. Chin Med J (Engl) 124:1290, 2011
8. Delmonico F; Council of the Transplantation Society: A report of the Amsterdam Forum on the care of the live kidney donor: data and medical guidelines. Transplantation 27(6 suppl): S53, 2005
9. Davis C: Evaluation of the living kidney donor: current perspectives. Am J Kidney Dis 43:508, 2004
10. Lindeman RD, Tobin J, Shock NW: Longitudinal studies on the rate of decline in renal function with age. J Am Geriatr Soc 33:278, 1985
11. Saxena AB, Myers BD, Derby G, et al: Adaptive hyperfil-tration in the aging kidney after contralateral nephrectomy. Am J Physiol Renal Physiol 291:629, 2006