It has long been documented that education about palliative care for terminally ill patients and their families is of great importance. Medical schools and colleges have paid much more atten-tion to end-of-life care educaatten-tion than in previous decades.1,2Many curricula on palliative care are arranged to enhance the education of terminal
patient care, with an emphasis on patient- and family-centered care.3,4 Traditional classroom-based medical training is inadequate for the task.5 With concerns for clinical competence, various kinds of undergraduate curricula on end-of-life care have been developed for better quality of palliative care.6 However, there are currently no
Effects of a Multimodule Curriculum of
Palliative Care on Medical Students
Stanley S.L. Tsai,1Wen-Yu Hu,2Hao-Hsiang Chang,3Shan-Chwen Chang,4Chin-Yu Chen,5 Tai-Yuan Chiu5*
Background/Purpose: The objective of this study was to investigate the effects of educational intervention using a multimodule curriculum of palliative care on medical students, and to explore significant factors that influence improvement in beliefs of ethical decision-making.
Methods: A total of 259 medical students enrolled in the “Family, Society and Medicine” course, and accepted a multimodule palliative care curriculum that included a 1-hour lecture, 1 hour of patient contact, 1 hour of literature reading, and 1 hour of discussion. A questionnaire was administered before and after the course to evaluate improvements in medical students’ knowledge (principles and clinical management) of palliative care and their beliefs concerning ethical decision-making in palliative care.
Results: The students showed significant improvements after the course in their knowledge of the principles of palliative care (pretest 58.4% vs. posttest 73.1%; p< 0.01) and clinical management of palliative care (pretest 58.8% vs. posttest 67.9%; p< 0.01). Although their beliefs about ethical decision-making were also improved after the course, the medical students did not have a positive belief of “artificial nutrition and hydration is not always beneficial for terminal cancer patients”, with a mean score of only 3.15 and 3.51 (pretest and posttest, respectively; range, 1–5). The logistic regression model showed that improve-ment in knowledge of either principles or clinical manageimprove-ment did not significantly improve beliefs about ethical decision-making.
Conclusion: A multimodule curriculum of palliative care for medical students can significantly improve their knowledge on principles of clinical management and beliefs about ethical decision-making in palliative care. As for changes in beliefs about ethical decision-making in palliative care, continued ethical and clinical training is required. [J Formos Med Assoc 2008;107(4):326–333]
Key Words: curriculum, ethical decision-making, palliative care, undergraduate
©2008 Elsevier & Formosan Medical Association
. . . .
1Department of Medical Education, National Taiwan University Hospital, 2School of Nursing and 3Department of Family
Medicine, National Taiwan University Hospital Bei-Hu Branch, and Departments of 4General Internal Medicine and 5Family Medicine, College of Medicine and Hospital, National Taiwan University, Taipei, Taiwan.
Received: July 3, 2007 Revised: November 26, 2007 Accepted: January 15, 2008
*Correspondence to: Dr Tai-Yuan Chiu, Department of Family Medicine, College of
Medicine and Hospital, National Taiwan University, 7 Chuang-Shan South Road, Taipei 100, Taiwan.
globally accepted standards for undergraduate or graduate training in palliative medicine.7
In Taiwan, many medical schools offer their palliative care education program mainly through lectures. Few institutions have formal curricula and very few studies have been conducted on curricu-lar evaluation. Our study assessed the impact of a 4-hour multimodule curriculum for fifth-year medical students on their knowledge and attitudes to end-of-life care. Through curricular evaluation, we identified factors that influence students’ be-liefs about ethical issues, so we can modify the curricular design to enable students to become more competent at giving better quality pallia-tive care.
Methods
Study population
This study was a cross-sectional survey conducted from 2003 to 2004. The target population con-sisted of 259 fifth-year medical students from National Taiwan University (NTU), China Med-ical University (CMU) and Chung-Shan MedMed-ical University (CSMU). These students undertook the 4-hour multimodule curriculum on pallia-tive education within the course “Family, Society and Medicine”. The study design and participant selection were approved by the hospitals’ ethics committees.
Description of multimodule curriculum
A fifth-year medical student at the NTU College of Medicine is required to complete a medical clerkship at the National Taiwan University Hos-pital (NTUH), which includes the 6-week course “Family, Society and Medicine”. Within the 6-week course, a 4-hour multimodule curriculum at the hospice and palliative care unit was arranged. Sixty fifth-year medical students from CMU and CSMU, who will receive internship training at NTUH, also attended this 4-hour course. The 4-hour multimodule curriculum consisted of:
• 1-hour lecture provided by a well-trained pal-liative care specialist. Knowledge and beliefs
in palliative care, typical clinical conflicts con-cerning palliative care, and associated regula-tions and laws were introduced. The structure of the lecture was uniform and standardized. • 1-hour patient visit at the hospice and
pallia-tive care unit was arranged by a senior doctor. Verbal and nonverbal communication and interaction with terminal cancer patients were practiced during the visit. Patient consent for the meetings was obtained prior to the visits. • 1 hour of literature reading concerning
human-ity was performed in a group discussion. • 1 hour of discussion for students to share
learn-ing feedback with palliative care specialists, mainly in a patient-centered fashion.
Measurements
A structured, three-part questionnaire was admin-istered to all subjects. The three-part questionnaire included questions on demographic characteris-tics, palliative care knowledge, and beliefs about ethical decision-making in palliative care. The en-tire questionnaire was tested for content validity by a panel composed of five palliative care spe-cialists, all of whom were experienced in care of the terminally ill.
Each item that related to palliative care knowl-edge in the questionnaire was appraised by “yes”, “no” and “unknown”, while beliefs about ethical decision-making in palliative care were appraised by “strongly disagree” (1) to “strongly agree” (5). A content validity index (CVI) was used to deter-mine the validity of the structured questionnaire. The questionnaire yielded a CVI of 0.920, com-puted by summing 0.238 from the “4” ratings and 0.682 from the “5” ratings on all items.
In addition, 10 students at the same year level filled out the questionnaire to confirm its face va-lidity and ease of application. Demographic char-acteristics assessed by the questionnaire included age, experience in providing palliative care, and information on palliative care. The other two parts included:
• Palliative care knowledge. This measure con-sisted of the principles (6 items) and clinical management (9 items) of hospice and palliative
care, such as symptom management and psycho-logic and spiritual care to be given to individu-als and their families. This 15-item measure was designed with careful scrutiny of the literature in this area. The main reference was the Palliative Care Quiz for Nursing that was originally de-veloped by Ross.8 All of the items were also grounded on the basis of real-life experiences of the investigators who were involved in pal-liative care. The scoring consisted of “true” (1) and “false/unknown” (0). Kruder-Richardson formula 20 (KR-20) was used to assess the in-ternal consistency of this knowledge measure and showed a coefficient of 0.69.
• Beliefs about ethical decision-making in pal-liative care. This part included “breaking the bad news” of terminal illness, discharge plan-ning for a symptom-controlled patient, artifi-cial nutrition concern, and sedation in terminal cancer care.9–12 Measurement of these issues was through a four-item set using a five-point Likert scale from “strongly disagree” (1) to “strongly agree” (5). Internal consistency was demonstrated with a Cronbach’s alpha coeffi-cient of 0.71.
Statistical analysis
Data management and statistical analysis were performed using the SPSS version 10.0 (SPSS Inc., Chicago, IL, USA). A frequency distribution was used to describe the demographic data and the distribution of each variable. The mean and stan-dard deviations were used to analyze the degree of each variable about knowledge and beliefs in palliative care. ANOVA was used to correlate the posttest scores of students with gender, religion, family history of cancer, and experience of pallia-tive care. Paired t test analyses were used to assess differences in palliative care knowledge and be-liefs about ethical decision-making on pre- and posttest assessments. Spearman analysis was used to assess the correlation between students’ beliefs about ethical decision-making and palliative care knowledge. Univariate and multivariate analysis were used to identify factors that significantly in-fluence beliefs about ethical decision-making on
pre- and posttest assessments. A logistic regression model was used to establish the key factor(s) that influence students’ beliefs about ethical decision-making in palliative care. A p value < 0.05 was considered significant.
Results
We analyzed 259 paired evaluations using paired t test from students who rotated from September 1, 2003 to October 30, 2004. The students showed significant improvements after the ward curricu-lum. The majority of students were male (74.9%) and 20–32 years old. Most of them had no specific religious beliefs (60.2%). There were 108 (41.7%) students with a positive family history of cancer, while 237 students (91.5%) had never experienced palliative care (Table 1).
On questions relating to palliative care knowl-edge, the mean score for all 15 items before the curriculum was 8.21 (accuracy rate, 54.7%) and 10.50 after (accuracy rate, 70.0%). The difference between the pre- and posttest mean was 2.29 (z= −11.926, p < 0.0001). There were significant improvements in 14 out of 15 items, except for “hospice and palliative care definition”.
Principles of palliative care
On a per item basis, six items regarding principles of palliative care had a mean score of 3.50 (58.3%) and 4.38 (73.0%) for pre- and posttests, respec-tively. Table 2 shows a 15.3% improvement in this part of the questionnaire. The paired t test showed that five out of six items had significant improve-ments (p< 0.01), while the Wilcoxon signed rank test showed a significant difference (z= −9.902, p< 0.001). The five items were: “palliative care is appropriate only in situations where there is evi-dence of a downhill trajectory or deterioration”, “to rid personal emotion is essential to provide palliative care”, “the principles of palliative care are compatible with those of aggressive treat-ment”, “accumulation of feeling of loss inevitably makes the palliative caregiver collapse”, “pallia-tive care adapts ‘natural death’, neither shortens
nor prolongs patient life”. Among these, students showed the lowest posttest positive rate of 51% on “to rid personal emotion is essential to provide palliative care” (Table 2).
Clinical management of palliative care
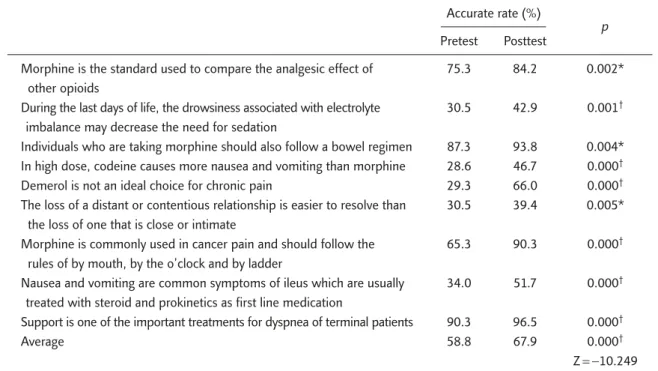
Table 3 shows nine items regarding the clinical management of palliative care, which had a mean score of 5.29 (58.8%) and 6.11 (67.9%) in pre-and posttests. All of the items showed a signifi-cant improvement, while a signifisignifi-cant difference was also observed under the McNemar χ2 test. However, some items showed less than half the accuracy rate, such as “during the last days of life, the drowsiness associated with electrolyte imbal-ance may decrease the need of sedation”, “in high dose, codeine causes more nausea and vomiting than morphine”, and “the loss of a distant or con-tentious relationship is easier to resolve than the loss of one that is close or intimate” (Table 3).
Beliefs about ethical decision-making in palliative care
The third part of the questionnaire consisted of four ethical issues concerned with terminal care: breaking bad news, discharge planning, artificial hydration and nutrition, and sedation for refrac-tory symptoms. All of the items showed a signifi-cant improvement with the paired t test, except
Table 2. Improvement in palliative care knowledge principles after the curriculum Accurate rate (%)
p
Pretest Posttest
Palliative care is appropriate only in situations where there is 45.9 68.3 0.000* evidence of a downhill trajectory or deterioration
To rid personal emotion is essential to provide palliative care 27.4 51.0 0.000†
The principles of palliative care are compatible with those of 73.7 85.3 0.000* aggressive treatment
Accumulation of feeling of loss inevitably makes the 29.7 47.9 0.000†
palliative caregiver collapse
Palliative care adapts ‘natural death’, neither shortens nor 78.0 87.6 0.002* prolongs patient life
Palliative care is an alternative for curative nonresponsive patients 95.4 98.5 0.057
Average 58.4 73.1 0.000†
Z= −9.902
*p< 0.01; †p< 0.001.
Table 1. Characteristics of the students (n= 259)
n (%) Gender Male 194 (74.9) Female 65 (25.1) Age (yr) 20–22 85 (32.8) 23–25 165 (63.7) 26–28 4 (1.6) ≥ 29 5 (1.9) Religion None 156 (60.2) Traditional faith 34 (13.2) Buddhist 24 (9.2) Daoist 8 (3.1) Christian 26 (10.1) Others 11 (4.2) School
College of Medicine, NTU 199 (76.8)
CMU 29 (11.2)
CSMU 31 (12)
Family or friends have had cancer
Yes 108 (41.7)
No 151 (58.3)
Family or friends have received palliative care
Yes 22 (8.5)
No 237 (91.5)
NTU = National Taiwan University; CMU = China Medical University; CSMU = Chung Shan Medical University.
“it is ethical for terminal patients to receive seda-tion for refractory symptoms”. Most of the students seemed to disagree much with “artificial hydration and nutrition have no benefit to terminal patients” (pretest, 3.15; post-test, 3.51; range, 1–5), while “discharge planning and home care are ethical for terminal patients” was the issue most accepted by the students (Table 4).
Correlation between palliative care knowledge and beliefs about ethical decision-making in palliative care
Spearman analysis was used to assess the correla-tion between improvement in beliefs about ethi-cal decision-making and students’ posttest scores
of palliative care knowledge (principles and clinical management). A significant correlation between “truth telling is helpful to a good death” and prin-ciples of palliative care knowledge (r= 0.160, p < 0.05) was noted. A similar finding was noted between “artificial hydration and nutrition have no benefit to terminal patients” and principles of palliative care knowledge (r= 0.160, p < 0.05), and between “artificial hydration and nutrition have no benefit to terminal patients” and clinical management of palliative care knowledge (r= 0.165, p< 0.01). The remainder showed no obvi-ous correlations. However, improvement in “dis-charge planning and home care are ethical for terminal patients” and “it is ethical for terminal Table 3. Improvement in palliative care knowledge with regard to clinical management after the curriculum
Accurate rate (%)
p
Pretest Posttest
Morphine is the standard used to compare the analgesic effect of 75.3 84.2 0.002* other opioids
During the last days of life, the drowsiness associated with electrolyte 30.5 42.9 0.001†
imbalance may decrease the need for sedation
Individuals who are taking morphine should also follow a bowel regimen 87.3 93.8 0.004* In high dose, codeine causes more nausea and vomiting than morphine 28.6 46.7 0.000†
Demerol is not an ideal choice for chronic pain 29.3 66.0 0.000†
The loss of a distant or contentious relationship is easier to resolve than 30.5 39.4 0.005* the loss of one that is close or intimate
Morphine is commonly used in cancer pain and should follow the 65.3 90.3 0.000†
rules of by mouth, by the o’clock and by ladder
Nausea and vomiting are common symptoms of ileus which are usually 34.0 51.7 0.000†
treated with steroid and prokinetics as first line medication
Support is one of the important treatments for dyspnea of terminal patients 90.3 96.5 0.000†
Average 58.8 67.9 0.000†
Z= −10.249
*p< 0.01; †p< 0.001.
Table 4. Improvement in beliefs of ethical decision-making in palliative care after the curriculum Accurate rate (%)
p
Pretest Posttest
Truth telling is helpful to a good death 4.270 4.380 0.008*
Discharge planning and home care are ethical for terminal patients 4.360 4.490 0.002* Artificial hydration and nutrition have no benefit to terminal patients 3.150 3.510 0.001* It is ethical to give sedation to terminal patients for refractory symptoms 4.160 4.250 0.085
patients to receive sedation for refractory symp-toms” did not correlate with the posttest scores of palliative care knowledge (principles and clinical management) (Table 5).
Factors influencing improvement in beliefs about ethical decision-making
Several factors in the study such as “family or friends have had cancer”, “willingness to provide palliative care”, “posttest’s accurate rate of princi-ples toward palliative care knowledge”, and “un-derstanding the laws about palliative care” were significantly correlated with improvement in be-liefs about ethical decision-making, after univariate analysis. The study had also intended to investigate the possible factors that influence improvement in ethical decision-making. However, no factor was found to significantly influence improvement in beliefs about ethical decision-making in a logistic regression model (p< 0.05).
Discussion
To the best of our knowledge, this study is one of the first to investigate improvement in medical students’ knowledge and attitudes concerning be-liefs about ethical decision-making in palliative care, especially in the Asia-Pacific region. In this study, we demonstrated that fifth-year medical students can have obvious improvements not only
in their palliative care knowledge (principles and clinical management), but also in their beliefs about ethical decision-making in palliative care after a concise 4-hour workshop on palliative care. Through an appropriate short-term curriculum design, the students learned more about pal-liative care knowledge and beliefs about ethical decision-making. The results are compatible with previously documented studies.13–16Our curricu-lum targeted fifth-year medical students because this is the very beginning of their involvement with the clinical environment and is also the best tim-ing to deliver active clinical traintim-ing.17,18Students at this level are more open to humanist compe-tency, which is undermined gradually by the clini-cal environment of subsequent internship training and residency training.
While there were many improvements in pal-liative care knowledge, not so many were made in terms of beliefs about ethical decision-making. This is possibly because more time is required to achieve concept change than knowledge improve-ment. Concept change usually involves changes in traditional values, social attitude toward diseases, and culture. We also noted that posttest scores of palliative care knowledge significantly correlated with improvements made in beliefs about ethical decision-making, such as “truth telling is helpful to a good death” and “artificial hydration and nu-trition have no benefit to terminal patients”. In other words, the better the students scored in the Table 5. Spearman’s correlation between palliative care knowledge (principles and clinical management) and
improvement in beliefs of ethical decision-making
Palliative care knowledge, r (p)
Total, r (p) Principles Clinical management
Improvement in…
truth telling is helpful to a good death 0.206* (0.001) 0.096 (0.123) 0.157†(0.011)
discharge planning and home care are ethical for 0.099 (0.111) −0.025 (0.692) 0.008 (0.904) terminal patients
artificial hydration and nutrition have no benefit to 0.185* (0.003) 0.176†(0.004) 0.255* (0.000)
terminal patients
it is ethical to give sedation to terminal patients for 0.129 (0.038) −0.066 (0.294) 0.055 (0.377) refractory symptoms
principles of palliative care knowledge, the more improvements were made in the belief that “truth telling is helpful to a good death” and “artificial hydration and nutrition have no benefit to terminal patients”.
In our curriculum, we use a multimodule de-sign that consisted of a lecture, bedside learning, relevant literature reading, and discussion. We be-lieve that students who underwent such curricu-lum will learn more about palliative care.19While every student will eventually have clinical prac-tice, this is the first time an integrated curriculum has been developed with both clinical practice and basic medical science together in end-of-life care in Taiwan.
Such a curriculum is easy to implement in other medical schools and clinical settings because the design concept is based on utilization of resources that already exist. Moreover, the curriculum is pur-posely condensed so that it can be easily exported to other medical schools. By implanting this riculum, we hope to establish a standard for cur-ricula development and outcome measurement in palliative medicine education earlier so that we can promote palliative medicine more broadly.
This study was conducted to understand the various factors that affect fifth-year medical stu-dents’ learning improvement with regard to be-liefs of ethical decision-making in palliative care. However, we found no significant factors corre-lating with these after the statistical analysis. There might be many other factors remaining to be taken into consideration and further efforts would be required to create the appropriate study and ques-tionnaire design.
We are also interested in the pattern of infor-mation retention after this curriculum. Further as-sessment in subsequent years of medical training, including residency training and clinical practice,20 toward curriculum design, and follow-up studies of students’ knowledge, attitudes, and skill reten-tion will provide more evidence to modify the curriculum.
There were several limitations inherent to this study. First, the study was conducted on only one intervention group. There was no control group
because every student was required to undergo this curriculum. Second, although this program improved the students’ knowledge of and atti-tudes on palliative care, the evaluation method was limited due to the short-term curriculum de-sign. The maturation effect should also have been considered. Lastly, concept changes required more time to observe. A longitudinal study would allow for a better understanding of concept changes over time. Therefore, continued observation and eval-uation of knowledge retention and attitude towards palliative care after the curriculum is necessary.
In conclusion, a multimodule curriculum of palliative care for medical students can signifi-cantly improve their knowledge, including prin-ciples and clinical management, and the beliefs of ethical decision-making toward palliative care. As for the change in the beliefs of ethical decision-making toward palliative care, continued ethical and clinical training is required.
Acknowledgments
The authors are indebted to the faculty of the Department of Family Medicine, National Taiwan University Hospital, particularly Ms Y.C. Chen and P.Y. Kuo for their assistance in preparing the manuscript.
References
1. Lo B, Snyder L. Care at the end of life: guiding practice where there are no easy answers. Ann Intern Med 1999; 130:772–4.
2. Sullivan AM, Lakoma MD, Block SD, et al. The status of medical education in end-of-life care: a national report.
J Gen Intern Med 2003;18:685–95.
3. Porter-Williamson K, von Gunten CF, Garman K, et al. Improving knowledge in palliative medicine with a required hospice rotation for third year medical students. Acad
Med 2004;79:777–82.
4. Ury WA, Arnold RM, Tulsky JA, et al. Palliative care cur-riculum development: a model for a content and process-based approach. J Palliat Med 2002;5:539–48.
5. Fins JJ, Nilson EG. An approach to educating residents about palliative care and clinical ethics. Acad Med 2000; 75:662–5.
6. Oneschuk D, Hanson J, Bruera E, et al. An international survey of undergraduate medical education in palliative care. J Pain Symptom Manage 2000;20:174–9.
7. Mari LW, Rod DM. A systemic review of teaching and learning in palliative care within the medical undergraduate curriculum. Med Teach 2004;26:683–90.
8. Ross HH. The palliative care quiz for nursing (PCNQ): the development of an instrument to measure nurses’ knowl-edge of palliative care. J Adv Nurs 1996;23:126–37. 9. Hu WY, Chiu TY, Chuang RB, et al. 2002 A professional
perspective: solving family-related barriers to truthfulness in cases of terminal cancer in Taiwan. Cancer Nursing 2002;25:486–92.
10. Hu WY, Chiu TY, Cheng YR, et al. Why Taiwanese hospice pa-tients want to stay in the hospital: health care professionals’ beliefs and solutions. Support Care Cancer 2004;12:285–92. 11. Chiu TY, Hu WY, Chuang RB, et al. Terminal cancer
patients’ wishes and the influencing factors toward the artificial provision of nutrition and hydration in Taiwan.
J Pain Symptom Manage 2004;27:206–14.
12. Chiu TY, Hu WY, Lue BH, et al. Sedation for refractory symptoms of terminal cancer patients in Taiwan. J Pain
Symptom Manage 2001;21:467–72.
13. Doreen O, John H, Eduardo B, et al. An international survey of undergraduate medical education in palliative medicine.
J Pain Symptom Manage 2000;20:174–9.
14. MacLeod R, Nash A. Taking the lid off: observations on the process of palliative care education for general practitioners.
Postgrad Edu Gen Pract 1992;3:28–33.
15. Ross D, O’Mara A, Pickens N, et al. Hospice and palliative care education in medical school. J Cancer Educ 1997;12: 152–6.
16. Kaye J, Loscalzo G. Learning to care for dying patients.
J Cancer Educ 1998;13:52–7.
17. Hayes R, Stoudemire A, Kinlaw K, et al. Changing attitudes about end of life decision making of medical students during third year clinical clerkships. Psychosomatics 1999; 40:205–11.
18. Weissman D, Griffie J. Integration of palliative medicine at the medical college of Wisconsin 1990–1996. J Pain
Symptom Manage 1998;15:195–201.
19. Forbes J. Towards an optimal teaching programme for supportive care, Support Care Cancer 1994;2:7–15. 20. Irwin W. Teaching terminal care at Queen’s University
Belfast—teaching arrangement and assessment of topic.