1
Incidence of cancer in a nationwide population cohort of 7852 patients with primary Sjogren’s syndrome in Taiwan
Meng-Yu Weng1, Yu-Tung Huang2, Ming-Fei Liu1, Tsung-Hsueh Lu3
1 Section of Allergy, Immunology, and Rheumatology, Department of Internal Medicine, National Cheng-Kung University Medical College and Hospital, Tainan, Taiwan
2 Department of Gerontological Care and Management, Chang Gung Institute of Technology, Taoyuan, Taiwan
3 NCKU Research Center for Health Data and Institute of Public Health, College of Medicine, National Cheng Kung University, Tainan, Taiwan
Correspondence to: Tsung-Hsueh Lu, Institute of Public Health, College of Medicine, National Cheng Kung University, No. 1, Dah Hsueh Road, Tainan 701, Taiwan;
robertlu@mail.ncku.edu.tw
Source: Annals of the Rheumatic Diseases, Vol.71, No.4, pp.524-527 Date of Publication: 2012-04
ISSN: 0003-4967
Publisher: BMJ Publishing Group DOI: 10.1136/annrheumdis-2011-200402
2 ABSTRUCT
Objective Patients with primary Sjogren’s syndrome (pSS) have higher risk in developing non-Hodgkin’s lymphoma (NHL). However, little is known with regard to the risk in developing cancers other than NHL. We aimed in this study to compare incidence of cancer of various sites among patients with pSS with general population in Taiwan.
Methods We used National Health Insurance claims data to establish a nationwide population cohort of 7852 patients with pSS from 2000 and 2008 who did not have cancer before diagnosis of pSS. Incidence and standardized incidence ratios (SIR) for cancer of various sites were calculated.
Results Among patients with pSS, 277 (2.9%) developed cancer. The SIR for cancer among patients with pSS aged ≧25 years and 25-44 years was 1.04 (95% CI 0.91-1.18) and 2.19 (95% CI 1.43-3.21), respectively. Female patients with pSS had higher risk of NHL (SIR 7.1, 95% CI
4.3-10.3), multiple myeloma (SIR 7.1, 95% CI 2.0-14.2) and thyroid gland cancer (SIR 2.6, 95% CI 1.4-4.3) and lower risk of colon cancer (SIR 0.22, 95% CI 0.05-0.65). On the contrast, male patients with pSS did not have higher risk in developing cancer of particular site.
Conclusion Only patients with pSS aged 25-44 years had higher risk of cancer. Cancer screening for patients with pSS, especially female patients, should focus on not only NHL but also multiple myeloma and thyroid gland cancer.
3 INTRODUCTION
Primary Sjogren’s syndrome (pSS) is a chronic autoimmune disorder with polyclonal B cell
activation and lymphocytic infiltration of the exocrine glands which characterized by dry eyes and a dry mouth. The estimated annual incidence of pSS is 4 to 6 per 100,000 inhabitants according to population-based studies.1-4 Studies have shown that patients with pSS have higher incidence of non-Hodgkin’s lymphoma (NHL) compared with general population with the standardized incidence ratio (SIR) ranged from 8.7 (95% CI 4.3 to 15.5) to 48.1 (95% CI 20.7 to 94.8).5-14 However, because of small number of patients observed in previous studies, little is known whether patients with pSS also have high risk in developing cancers other than NHL.
The Taiwan National Health Insurance (NHI) program is a mandatory, compulsory, single-payer health insurance system in which all citizens are obliged to participate. The NHI program was implemented in 1995 and covered 99.5% of the population of Taiwan by the end of 2008.15 The NHI Research Database has been released to researchers in an electronically encrypted form since 1999. Because of large sample size and high quality in cancer related diagnosis in this claims data, this dataset provided good opportunity to estimate incidence of cancer among patients with
Helicobacter pylori infection,16,17 diabetes mellitus18,19 and autoimmune diseases.20-23 We therefore aimed in this study to compare the incidence of cancer of various site among pSS patients with general population in Taiwan using Taiwan NHI claims data.
4 PATIENTS AND METHODS
Data sources
The Catastrophe Illness File of NHI claims data was used for this study. To avoid financial catastrophe for families coping with major injuries/illnesses, the NHI specifies 31 categories of catastrophic illness (e.g., cancers, hemophilia, autoimmune diseases, chronic renal failure, etc.) that are exempt from co-payment. The attending physician of patient diagnosed as falling into one of these categories of catastrophic illness under the Department of Health guidelines can submit related information to complete an application for a catastrophic illness certificate (CIC).
Applications are formally reviewed by committee, and if approved, patients are then exempted from co-payment.24
Cohort of patients with pSS
In this study, the cohort of patients with pSS confined to those approved CIC for pSS aged ≧25 years between 2000 and 2008. To get an CIC for pSS, the attending physician of the patient is required to provide relevant clinical and laboratory information as part of the application for review, and the review committee will assess applications according to the criteria of the
American-European Consensus Group for pSS.25
We excluded patients with both a CIC for pSS and a CIC for any other autoimmune disease, such as systematic lupus erythematosus, rheumatoid arthritis, other connective tissue diseases, etc., who should instead be classified as having secondary Sjӧgren syndrome. Patients who had CIC for cancer before having CIC for pSS were also excluded.
Identification of cancer
Cancer is one of 31 categories of catastrophic illness defined by NHI. To approve for CIC for cancer, the attending physician should provide pathology evidence and imaging studies supporting the diagnosis of cancer which including radiographs, bone scans, computed tomography, or magnetic resonance imaging scans. The records are reviewed by a committee and only patients who meet the criteria for the diagnoses are issued CIC. The ICD-9-CM codes were used to define cancer of various sites.
Statistical analysis
5
We first calculated incidence of cancer (case per 1000 person-years) among patients with pSS by sex and age (25-44, 45-64 and ≧65 years). To examine whether patients with pSS had higher risk in developing cancer we computed the standardized incidence ratios (SIRs) and 95% confidence intervals (95% CI) for cancer among patients with pSS. The expected number of cancer was estimated according to incidence of cancer among general population matched for sex, age and periods (2000-2002, 2003-2005 and 2006-2008). We also calculated SIRs by follow-up years (<1, 1-2, 3-4 and ≧5 years) to determine if risk of identifying cancer associated with length of follow-up.
6 RESULTS
A total of 7852 patients (6911 females and 941 males) with pSS aged ≧25 years were identified between 2000 and 2008. The average follow-up years were 3.5 years. The mean age (SD) at time of approving CIC for pSS was 54 (14) years and most patients were in 45-64 years of age (Table 1).
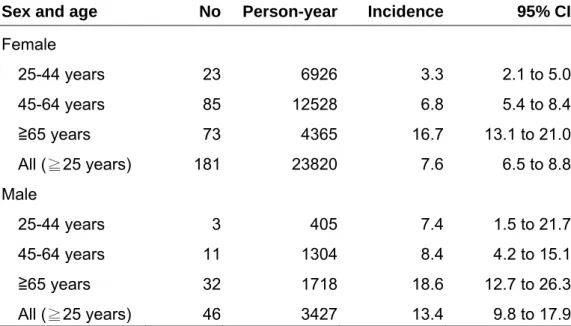
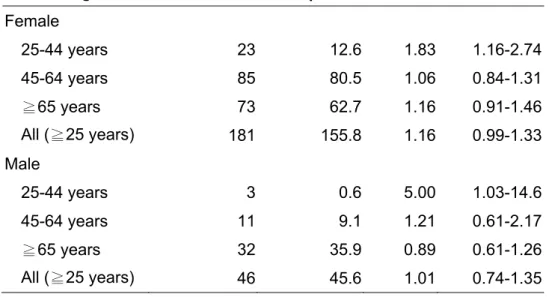
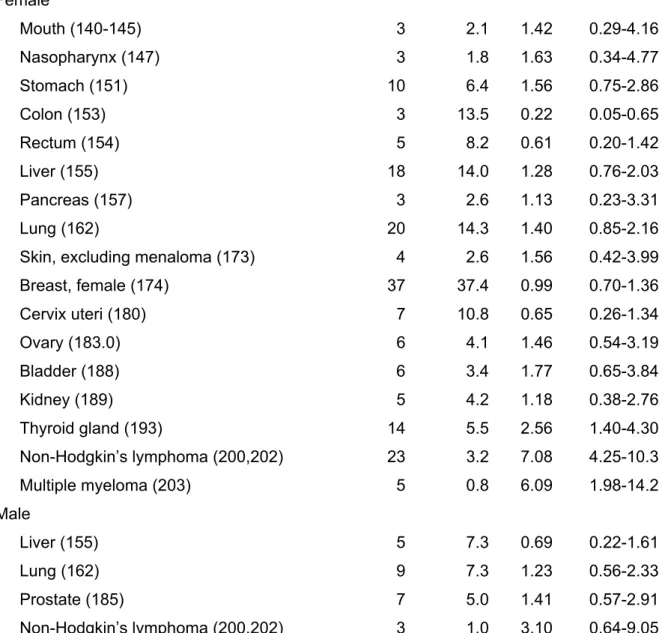
A total of 227 (2.9%) patients with pSS were diagnosed of having cancer after the approval of CIC for pSS during the observation period of 27,246 person-years. The incidence of cancer among patients with pSS increased with age and male patients had higher incidence than female patients (Table 2). Only patients with pSS aged 25-44 years had significantly higher SIR (Table 3). The longer the years the patients were followed the lower the risk the patients been identified with cancer (Table 4). Table 5 presents SIR and 95% CI for cancer of various sites with number of incident cancer at least three. Female patients with pSS had higher risk of NHL, multiple myeloma and thyroid gland cancer and lower risk of colon cancer. On the contrast, male patients with pSS did not have higher risk in developing cancer of particular site.
7 DISCUSSION
The findings of this study suggest that incidence of cancer among patients with pSS increased with age and male patients had higher incidence than female patients. However, compared with same sex-age group, only patients with pSS aged 25-44 years had higher risk of cancer. Consistent with previous studies, patients with pSS in this study also had higher risk in developing NHL. With regard to cancers other than NHL, this study found that female patients with pSS also had higher risk of multiple myeloma and thyroid gland cancer and lower risk of colon cancer.
One of the strengths of this study was that this was the first study using nationwide population cohort and having the largest sample size compared with previous studies which allowed us to calculate incidence of cancer among patients with pSS by sex-age group and to estimate risk of cancer other than NHL.
However, several limitations existed in this study. First, there were no laboratory data availabe in claims data we thus could not analyze detail risk factors in developing cancer. Second, we included only patients with CIC for pSS, some patients with pSS diagnosis in ambulatory care claims data without CIC for pSS were not included in the cohort. Third, in the same token, some patients with cancer might not apply for CIC for cancer, which would not be identified in this study.
Fourth, the average follow-up years (3.5 years) in this study was relatively short. Fifth, unlike the study of Lazarus et al12 which included cancer either before or after diagnosis of pSS, we excluded those having cancer before date of getting CIC for pSS. In other words, some patients who had pSS and then carcinogenesis changes long before applying CIC for pSS were excluded from this study.
In consideration of above-mentioned limitations, the risk of cancer was underestimated in this study.
Consistent with previous studies, we also confirmed that patients with pSS had higher risk of having NHL. However, the SIR for NHL in this study is lower than previous studies.5-14 The main reason for underestimation of SIR for NHL was the short follow-up years observed in this study.
Similar to study of Zhang et al.,14 we also found that patients with pSS had higher risk of having thymus cancer in this study. We did not present the SIR for thymus cancer in Table 5 because only two thymus cancers were identified.
This is the first study to suggest that patients with pSS had higher risk for multiple myeloma and
8
thyroid cancer. No study, to best of our knowledge, ever proposed possible associations between pSS and multiple myeloma and thyroid cancer. 是否要再加幾句話?不加也可以,流病研究不用太細 說明As pSS, thymus cancer and thyroid cancer all involve glands, maybe there are some
mechanisms correlate pSS and glandular cancers.
One accidental finding of this study was that patients with pSS had lower risk of having colon cancer. Similar finding was found among patients with rheumatoid arthritis with SIR of 0.94 (95% CI 0.93-0.96) in Taiwan.20 One possible explanation was that many patients with pSS might also have myoglagia (引用文獻) and regularly use NSAID, (引用文獻) which result in lower risk of colon cancer.
Further studies are needed to confirm this hypothesis.
In conclusion, according to the findings of this study, patients with pSS overall did not have higher risk of cancer, only patients with pSS aged 25-44 years had increase risk of cancer.
Physicians caring for patients with pSS should screen not only NHL, a well known cancer with higher risk among patients with pSS, but also multiple myeloma and thyroid gland cancer. Further studies are needed to investigate possible mechanisms associate with pSS and glandular cancers.
9 REFERENCES
1. Pillemer SR, Matteson EL, Jacobsson LTH, Martens PB, Melton LJ, O’Fallon WM, Fox PC.
Incidence of physician-diagnosed primary Sjӧgren’s syndrome in residents of Olmsted County, Minnesota. Mayo Clin Proc 2001;76:593–9.
2. Plesivcnik Novljan M, Bozman B, Hocevar A, Grmek M, Kveder T, Tomsic M. Incidence of primary Sjӧgren’s syndrome in Slovenia. Ann Rheum Dis 2004;63:874–6.
3. Alamanos Y, Tsifetaki N, Voulgari PV, Venetsanopoulou AI, Siozos C, Drosos AA.
Epidemiology of primary Sjӧgren’s syndrome in north-west Greece, 1982-2003. Rheumatology 2006;45:187–91.
4. Weng MY, Huang YT, Liu MF, et al. Incidence and mortality of treated primary Sjögren’s syndrome in Taiwan: a population-based study. J Rheumatol 2011;38:706-8.
5. Kassan SS, Thomas TL, Moutsopoulos HM, et al. Increased risk of lymphoma in sicca syndrome. Ann Intern Med 1978;89:888-92.
6. Kauppi M, Pukkala E, Isomaki H. Elevated incidence of hematologic malignancies in patients with Sjogren’s syndrome compared with patients with rheumatoid arthritis (Finland). Cancer Causes Control 1997;8:201-4.
7. Valesini G, Priori R, Bavoillot D, et al. Differential risk of non-Hodgkin’s lymphoma in Italian patients with primary Sjogren’s syndrome. J Rheumatol 1997;24:2376-80.
8. Davidson BK, Kelly CA, Griffiths ID. Primary Sjogren’s syndrome in the North East of England:
a long-term follow-up study. Rheumatology1999;38:245-53.
9. Voulgarelis M, Dafni UG, Isenberg DA, et al. Malignant lymphoma in primary Sjogren's syndrome: a multicenter, retrospective, clinical study by the European Concerted Action on Sjogren's Syndrome. Arthritis Rheum 1999;42:1765-72.
10. Pertovaara M, Pukkala E, Laippala P, et al. A longitudinal cohort study of Finnish patients with primary Sjögren’s syndrome: clinical, immunological, and epidemiological aspects. Ann Rheum Dis 2001;60:467-72.
11. Theander E, Henriksson G, Ljungberg O, et al. Lymphoma and other malignancies in primary Sjogren's syndrome: a cohort study on cancer incidence and lymphoma predictors. Ann
1 0 Rheum Dis 2006;65:796-803.
12. Lazarus MN, Robinson D, Mak V, et al. Incidence of cancer in a cohort of patients with primary Sjogren's syndrome. Rheumatology 2006;45:1012-5.
13. Anderson LA, Gadalla S, Morton LM, et al, Population-based study of autoimmune conditions and the risk of specific lymphoid malignancies. Int J Cancer 2009;125:398-405
14. Zhang WS, Feng S, Yan S, et al. Incidence of malignancy in primary Sjogren's syndrome in a Chinese cohort. Rheumatology 2010;49:571-7.
15. Bureau of National Health Insurance. National health insurance profile 2010. [Internet.
Accessed November 23, 2010.] Available from:
http://www.nhi.gov.tw/english/webdata.asp?menu=11&menu_id=29 0&webdata_id=2974
16. Wu CY, Kuo KN, Wu MS, et al. Early Helicobacter pylori eradication decreases risk of gastric cancer in patients with peptic ulcer disease. Gastroenterology 2009;137:1641-8.
17. Wu CY, Wu MS, Kuo KN, et al. Effective reduction of gastric cancer risk with regular use of nonsteroidal anti-inflammatory drugs in Helicobacter pylori-infected patients. J Clin Oncol 2010;28:2952-7.
18. Chen HF, Chen P, Li CY. Risk of malignant neoplasms of liver and biliary tract in diabetic patients with different age and gender stratification. Hepatology 2010;52:155-63.
19. Chen HF, Chen P, Li CY. Risk of malignant neoplasm of pancreas in relation to diabetes: a population-based study in Taiwan. Diabetes Care 2011;34:1177-9.
20. Chen YJ, Bhang YT, Wang CB, et al. The risk of cancer in patients with rheumatoid arthritis: a nationwide cohort study in Taiwan. Arthritis Rheum 2011;63:352-8.
21. Liang JA, LM Sun, JJ Yeh, et al. Malignancies associated with systemic lupus erythematosus in Taiwan : a nationwide population-based cohort study. Rheumatol Int 2010 doi:
10.1007/s00296-010-1684-y
22. Hang YL, Chen YJ, Lin MW, et al. Malignancies associated with dermatomyositis and
polymyositis in Taiwan: a nationwide population-based study. Br J Dermatol 2009;161:854-60.
23. Chen YJ, Wu CY, Huang YL, et al. Cancer risks of dermatomyositis and polymyositis: a nationwide cohort study in Taiwan. Arthrtis Res Ther 2010;12:R70.
11
24. Bureau of National Health Insurance. Catastrophic illness patients. [Internet. Accessed November 23, 2010.] Available from:
http://www.nhi.gov.tw/english/webdata.asp?menu=11&menu_id=596&webdata_id=3180
25. Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, et al.
Classification criteria for Sjogren’s syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis 2002;61:554-8.
1 2
Table 1 Characteristics of 7852 patients with primary Sjögren’s syndrome in Taiwan
Age at diagnosis ± SD, years
Male 62 ± 14
Female 53 ± 13
Age, male, number (%)
25-44 years 125 (13)
45-64 years 356 (38)
≧65 years 460 (49)
All (≧25 years) 941 (100)
Age, female, number (%)
25-44 years 1881 (27)
45-64 years 3636 (53)
≧65 years 1394 (20)
All (≧25 years) 6911 (100)
Duration of follow-up, mean ± SD, years
Male 3.4 ± 2.4
Female 3.6 ± 2.4
1 3
Table 2 Incidence and 95% confidence intervals (95% CI) for cancer in patients with primary Sjögren’s syndrome in Taiwan by sex and age
Sex and age No Person-year Incidence 95% CI Female
25-44 years 23 6926 3.3 2.1 to 5.0
45-64 years 85 12528 6.8 5.4 to 8.4
≧65 years 73 4365 16.7 13.1 to 21.0
All (≧25 years) 181 23820 7.6 6.5 to 8.8
Male
25-44 years 3 405 7.4 1.5 to 21.7
45-64 years 11 1304 8.4 4.2 to 15.1
≧65 years 32 1718 18.6 12.7 to 26.3
All (≧25 years) 46 3427 13.4 9.8 to 17.9
1 4
Table 3 Standardized incidence ratio (SIR) and 95% confidence intervals (95% CI) for cancer in patients with primary Sjögren’s syndrome in Taiwan by sex and age
Sex and age Observed Expected SIR 95% CI Female
25-44 years 23 12.6 1.83 1.16-2.74
45-64 years 85 80.5 1.06 0.84-1.31
≧65 years 73 62.7 1.16 0.91-1.46
All (≧25 years) 181 155.8 1.16 0.99-1.33
Male
25-44 years 3 0.6 5.00 1.03-14.6
45-64 years 11 9.1 1.21 0.61-2.17
≧65 years 32 35.9 0.89 0.61-1.26
All (≧25 years) 46 45.6 1.01 0.74-1.35
1 5
Table 4 Standardized incidence ratio (SIR) and 95% confidence intervals (95% CI) for cancer in patients with primary Sjögren’s syndrome in Taiwan by years of follow-up
Years of follow-up Observed Expected SIR 95% CI Female
<1 year 55 19.1 2.89 2.17-3.76
1-2 years 66 31.6 2.09 1.61-2.66
3-4 years 41 45.5 0.90 0.65-1.22
≧5 years 19 59.6 0.32 0.19-0.50
Male
<1 year 17 4.8 3.56 2.07-5.70
1-2 years 14 6.0 2.32 1.27-3.89
3-4 years 11 10.3 1.07 0.54-1.92
≧5 years 4 24.5 0.16 0.04-0.42
1 6
Table 5 Standardized incidence ratio (SIR) and 95% confidence intervals (95% CI) in patients with primary Sjögren’s syndrome in Taiwan by cancer site
Cancer site (ICD-9 code) Observed Expected SIR 95% CI Female
Mouth (140-145) 3 2.1 1.42 0.29-4.16
Nasopharynx (147) 3 1.8 1.63 0.34-4.77
Stomach (151) 10 6.4 1.56 0.75-2.86
Colon (153) 3 13.5 0.22 0.05-0.65
Rectum (154) 5 8.2 0.61 0.20-1.42
Liver (155) 18 14.0 1.28 0.76-2.03
Pancreas (157) 3 2.6 1.13 0.23-3.31
Lung (162) 20 14.3 1.40 0.85-2.16
Skin, excluding menaloma (173) 4 2.6 1.56 0.42-3.99
Breast, female (174) 37 37.4 0.99 0.70-1.36
Cervix uteri (180) 7 10.8 0.65 0.26-1.34
Ovary (183.0) 6 4.1 1.46 0.54-3.19
Bladder (188) 6 3.4 1.77 0.65-3.84
Kidney (189) 5 4.2 1.18 0.38-2.76
Thyroid gland (193) 14 5.5 2.56 1.40-4.30
Non-Hodgkin’s lymphoma (200,202) 23 3.2 7.08 4.25-10.3
Multiple myeloma (203) 5 0.8 6.09 1.98-14.2
Male
Liver (155) 5 7.3 0.69 0.22-1.61
Lung (162) 9 7.3 1.23 0.56-2.33
Prostate (185) 7 5.0 1.41 0.57-2.91
Non-Hodgkin’s lymphoma (200,202) 3 1.0 3.10 0.64-9.05