Regular Article
Magnetic resonance imaging findings in patients with
delusional disorder due to diffuse cerebrovascular
disease:A report of seven cases
KUAN-PIN SU, md,1–3CHUNG-YAO HSU, md,4 SHU-CHIANG HSIEH, md5
AND WINSTON W. SHEN, md1–3
1Department of Psychiatry,5Department of Radiology,Taipei Medical University-affiliated Wan Fang Hospital, 2Department of Psychiatry,Taipei Medical University and Hospital,4Department of Neurology,Taipei City
Psychiatric Center, and 3School of Medicine,Taipei Medical University,Taipei,Taiwan
Abstract Delusions associated with cerebrovascular diseases have been sporadically reported. Although both psychiatrists and neurologists attempted to link delusions with anatomical locations of the brain lesion, comorbid psychiatric and neurological disorders make the interpretation of delu-sions difficult. The purpose of the present paper is to report the clinical features and magnetic resonance imaging (MRI) characteristics in patients with delusional disorder due to diffuse cere-brovascular diseases, and to redefine the concept of ‘vascular delusion’. The clinical features and MRI findings were reviewed retrospectively in a series of seven patients with ‘delusional disor-der due to cerebrovascular disease’ as defined in Diagnostic and Statistical Manual of Mental
Disorders (DSMIV). The average age of onset is 64. No patient had a prior personal or family
history of major psychiatric illness. The illness is presented as acute, subacute or stepwise course. Hypertension was present in all patients. Two had diabetes mellitus, and one had atrial fibrilla-tion. Three had clinical evidence of previous cerebrovascular attacks, only one showed minor neurological deficits. Three had diffuse cortical slow wave in electroencephalogram. No patient had significant cognitive impairment but had multiple cortical and subcortical cerebrovascular lesions in MRI, with white-matter lesions (WML) in bilateral frontal areas. Delusional disorder due to diffuse cerebrovascular change is characterized by late-onset, stepwise course, and comor-bid medical and neurological diseases. The results of vascular changes in the present study did not establish a cause–effect relationship and should be considered as multifactorial in pathogen-esis. The findings suggested the hypothesis of neural circuit theory. Further studies in larger numbers of patients and newer neuroimaging techniques are needed to expand the knowledge learned from these findings.
Key words magnetic resonance imaging, organic delusional disorder, vascular delusion, white matter lesions.
INTRODUCTION
‘Organic factor’ is roughly interpreted that a mental disorder is due to a general medical condition in
Diagnostic and Statistical Manual of Mental Disorders
(DSM-IV).1 Delusion as a symptom is most
fre-quently seen in two psychiatric disorders: schizophre-nia and psychotic disorder due to a general medical condition.2 Delusional disorder due to a general
medical condition is scientifically interesting to provide a window onto the neurobiologic mechanisms of thought disorders, and to serve as models for the treatment of delusional disorder.
The symptom of delusion associated with cere-brovascular diseases has been sporadically reported. Psychiatrists and neurologists attempted to link the locations of the anatomic brain lesions with specific clinical symptoms. Some specific relationships which
Correspondence address: Kuan-Pin Su,M D, Department of Psy-chiatry, Taipei Medical University-affiliated Wan Fang Hospital, No. 111, Hsing-Lung Road Sec. 3, Taipei 116, Taiwan. Email: cobol@wanfang.gov.tw
have been hypothesized and partially tested, include delusions and hallucinations following right tem-poroparietal infarctions,3,4 delusion of parasitosis
fol-lowing right subcortical ischemic change,5 as well as
Capgras syndrome and Fregoli syndrome following right hemisphere infarctions.6,7 High prevalence of
delusional disorder in Huntington’s disease, idiopathic basal ganglia calcifications, and Parkinson’s disease suggests that delusions might be associated with the pathologic lesion of subcortical structure.8
Newer neuroimaging techniques enable the clini-cians to detect subtle structural and functional changes in the brain. More studies revealed that Alzheimer’s disease, multi-infarct dementia,9 white matter lesions
(WML)10,11 and ‘silent’ vascular disease11 may play a
role in causing delusions, particularly in the elderly. These findings further imply that delusions are due to circuit dysfunction rather than regional abnormality. However, comorbid psychiatric and neurological dis-orders make these findings hard to interpret the symptom of delusions meaningfully.8,9
The present study is intended to add to the literature about the clinical features and magnetic resonance imaging (MRI) characteristics of delusional disorder due to cerebrovascular disease, and to redefine the term ‘vascular delusion’ which is similar to the concept of vascular dementia and vascular depression.
METHODS
We retrospectively reviewed the chart records of patients admitted to the neuropsychiatric ward of Taipei city Psychiatric Center, Taipei, Taiwan, which is assigned as a center for the northern Taiwan catch-ment region, from January 1991 to June 1997. We collected clinical data including gender, age at onset, types of delusion, associated hallucination, psychiatric
history, medical history, neurologic examination, mental status evaluation, electroencephalographic (EEG) examination, and brain MRI for multiple cere-brovascular lesions. If a diagnosis was initially made by DSM-III-R12criteria, it would be upgraded according
to the DSM-IV.1The patients meeting diagnostic
crite-ria of delusional disorder due to cerebrovascular disease were included.
Exclusions from the study were patients with the diagnoses of other major psychiatric disorders such as delirium, dementia, schizophrenia, mood disorders, or other non-vascular cortical/subcortical neurologic disorders such as Alzheimer’s disease, multiple sclero-sis, Parkinson’s disease, Huntington’s disease. Patients with incomplete clinical data or uncertain diagnosis were also excluded.
RESULTS
Seven patients with delusional disorder due to a general medical condition were identified. Table 1 lists the clinical features of all seven patients with both prominent delusions and behavioral problems. Three cases were female. The ages at the time of onset of the disease ranged from 52 to 78 years. Mean ages of the whole group, the male subgroup, and the female subgroup were 64, 67 and 61, respectively. No patient had a prior history or family history of major psychi-atric disorders. The illness was presented as an acute, subacute or stepwise course. Delusions should be the predominant features if both delusions and hallucina-tions were presented.
As indicated in Table 2, all patients had striking multiple cortical and subcortical cerebrovascular lesions in MRI. Three cases had clinical evidence of cerebrovascular accidents, but only one showed minor neurologic deficits. Three cases had diffuse cortical
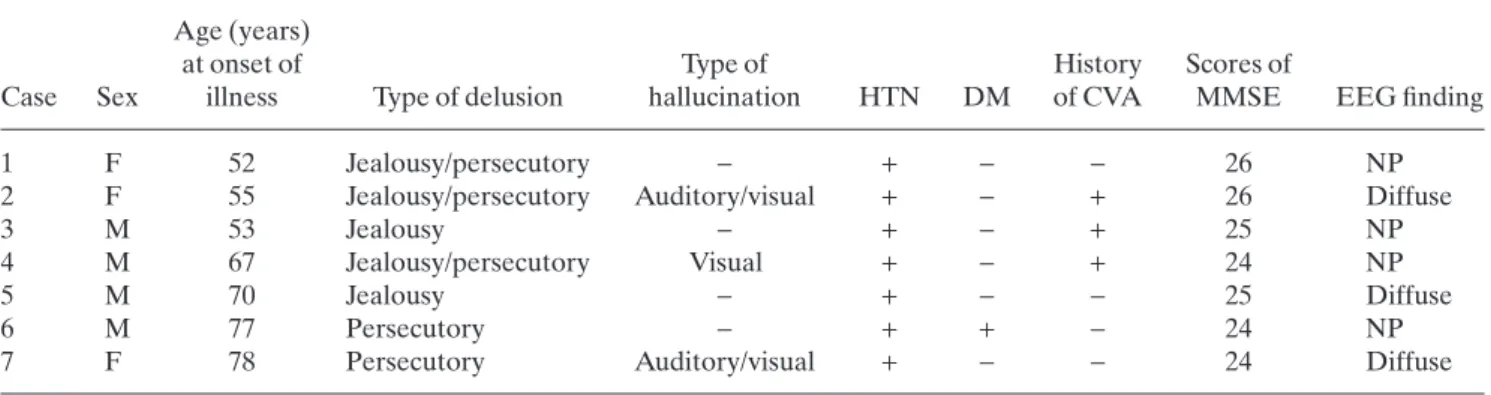
Table 1. Clinical features of patients with delusions due to diffuse cerebrovascular disease Age (years)
at onset of Type of History Scores of
Case Sex illness Type of delusion hallucination HTN DM of CVA MMSE EEG finding
1 F 52 Jealousy/persecutory - + - - 26 NP
2 F 55 Jealousy/persecutory Auditory/visual + - + 26 Diffuse
3 M 53 Jealousy - + - + 25 NP
4 M 67 Jealousy/persecutory Visual + - + 24 NP
5 M 70 Jealousy - + - - 25 Diffuse
6 M 77 Persecutory - + + - 24 NP
7 F 78 Persecutory Auditory/visual + - - 24 Diffuse
M, male; F, female; CVA, cerebrovascular accident; HTN, hypertension; DM, diabetes mellitus; diffuse, diffuse cortical dys-function; NP, no positive finding.
slow wave in EEG. All seven patients had hyperten-sion. Two had diabetes mellitus, and one had atrial fib-rillation. In all seven cases, intellectual impairment was not recognized in the test results for cognitive function and in the interviews with the families and their primary health carer.
CASE DESCRIPTIONS
To better illustrate the clinical manifestation of delu-sions associated with cerebrovascular diseases, we offer the following two case reports.
Case 1
A 62-year-old, right-handed Aboriginal Taiwanese woman was brought to the hospital because of increasing persecutory and jealous delusion associ-ated with aggressive behaviors. The medical history showed that she had diabetes mellitus, hypertension, and heart disease without any medical control. At the age of 52 years, she experienced an episode of hy-pertensive crisis and started to complain that her husband, a 76-year-old veteran, had sexual relation-ships with her daughter-in-law and granddaughter. Six months before admission, the patient had another episode of hypertensive crisis and suddenly believed that her husband and her daughter-in-law planned to kill her, although these beliefs were not true. She was admitted to the hospital to prevent her from killing her husband and then later herself.
In the mental status examination, the patient was alert but irritable, and was cooperative for only a few minutes in the interview. She described her delusions in vivid details with anxious affect. She was orientated to time (month and year), and had intact recent memory by remembering three objects in 5 min. Speech and language functions were normal.
Her blood pressure was 150/90 mmHg. The results of her basic neurologic examinations were normal. The mini-mental status examination (MMSE) score was 26, and the DSM-III-R12 diagnosis was organic
delusional disorder.
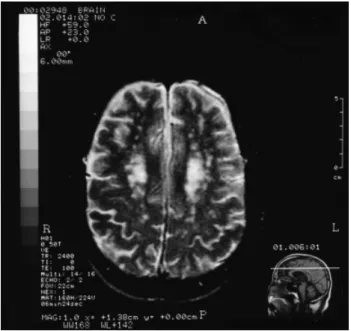
The EEG findings were normal. As shown in Fig. 1, the MRI findings showed multiple lacunar infarcts in bilateral pontine bases, putamen, and WML of periventricular space, mainly at middle and supraven-tricular level (centrum semiovales), relatively worse in right side of the brain. Her behavior problems improved after the treatment with haloperidol 5 mg/day for 2 weeks, but her delusions persisted.
Case 4
A 67-year-old right-handed man was admitted to our hospital for the assessment of behavioral disturbances associated with jealous delusion. He had a past his-tory of hypertension. A cerebrovascular accident prompted an admission to the neurologic intensive care unit 1 year before admission. Although the patient did not have any neurologic deficit, he started to have delusion of jealousy and delusion of losing his sexual function. His wife and his daughter brought him to the hospital because he had become impulsive and irritable in dealing with other people.
In the mental status examination, the patient was alert and cooperative. He had delusions but he was not concerned with this symptom. His affect was restricted in range. He had trouble remembering the exact date. He had intact recent memory, shown by his ability to recall three objects in 5 min. The abilities in speech, language comprehension, and naming objects were intact.
The results of basic neurologic examination were normal. The scores in neuropsychologic tests re-vealed 75 in verbal IQ, and 76 in performance IQ. His
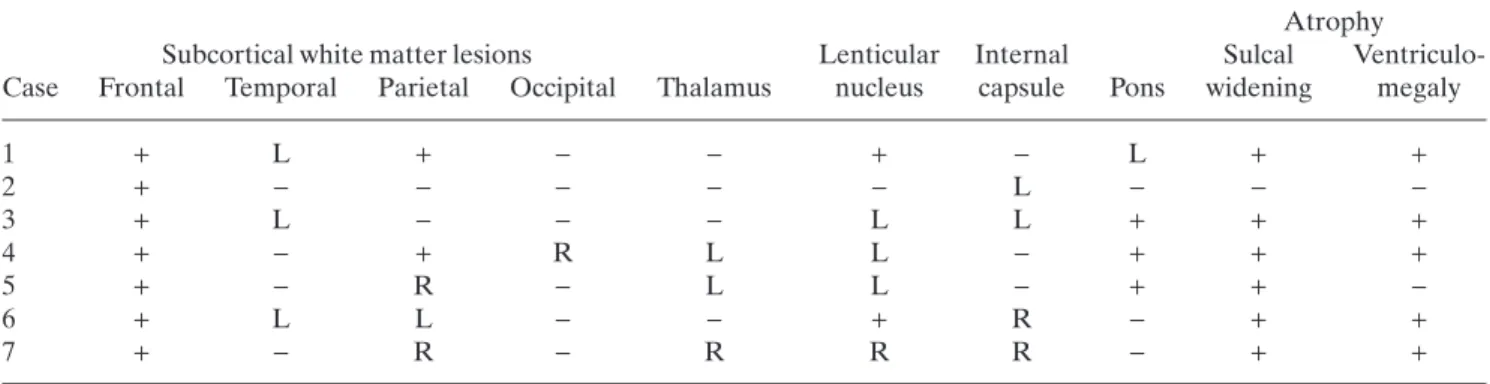
Table 2. Magnetic resonance image finding in seven patients with delusions due to diffuse cerebrovascular disease Atrophy
Subcortical white matter lesions Lenticular Internal Sulcal Ventriculo-Case Frontal Temporal Parietal Occipital Thalamus nucleus capsule Pons widening megaly
1 + L + - - + - L + + 2 + - - - L - - -3 + L - - - L L + + + 4 + - + R L L - + + + 5 + - R - L L - + + -6 + L L - - + R - + + 7 + - R - R R R - + +
MMSE score was 24, and his DSM-III-R12 diagnosis
was delusional disorder.
The results of laboratory investigations including EEG, were normal. Magnetic resonance image (Fig. 2) showed generalized atrophy, diffuse confluent WML, and multiple small lacunar infarcts in both sides of lenticular nuclei and the left pons. His delusions
im-proved after receiving treatment with 200 mg/day of sulpiride for 3 weeks.
DISCUSSION
All the subjects in the present study had extensive WML, which were especially located in anterior, pos-terior horn and subfrontal areas. The cerebrovascular lesions in thalamus, basal ganglion, internal capsule and pons were also frequently found. White matter lesions represent cerebrovascular changes histopatho-logically although their exact clinical significance is still in dispute.13,14
Cerebrovascular lesions present various aspects of neuropsychiatric symptoms, primarily because they tend to be more pathologically diffuse as shown in EEG and MRI findings. Although delusions in diffuse cerebrovascular lesions are not yet well defined in the literature, vascular dementia is relatively well recognized.15–19 In contrast, vascular depression is
also thought to occur in those patients although its descriptions are still inconclusive.20–23
The genesis of these neuropsychiatric symptoms related to vascular lesions is still unknown. Alexander
et al. proposed five structural-functional loops acting
as parallel units.24 Dementia might result from more
extensive interruption of ascending pathways from brainstem to subcortical structures as well as of path-ways from frontal lobe to posterior cortical regions.25
Depression may be related with the damage to the striato–pallido–thalamo–cortical pathways.26,27The
most important neural circuits associated with delu-sions were hypothesized to be the anterior cingulate
Figure 1. T2-weighted imaging (TR/TI/ excitation= 3000/0/80) from a subject with delusional disorder due to diffuse cerebrovascular disease (Case 1) shows that multiple lucunar infarcts in bilateral centrum semiovales, periventricular and subcortical white matter.
Figure 2. T2-weighted imaging (TR/TI/excitation= 2400/0/ 100) from a subject with delusional disorder due to diffuse cerebrovascular disease (Case 4) shows that brain atrophy with multiple lucunar infarcts in the periventricular white matter.
loop and dorsolateral prefrontal cortical loop, with connections to caudate, globus pallidus, substantia nigra, and thalamus.28These structures are thought to
perform as a functional unit, which was clearly sup-ported by the MRI findings in the present study.
To define the concept of vascular delusions, the neuropsychiatrists need to look for the disruption in parallel distributed or dynamic circuits rather than on the localization of the lesion per se.29 However, the
problems in neural connections cannot be identified by the use of present neuroimaging techniques. The concept of vascular delusions has the same limitations as that of vascular dementia and vascular depression. To single out vascular factors as the sole cause of the symptom is an oversimplification. In vascular demen-tia and depression, the lesions of vascular structures are increasingly recognized as one of the contributory rather than the primary causes.23,30–32 In a similar
concept, delusions in diffuse cerebrovascular disease should also be speculated in multifactorial instead of a single factor. Future studies should focus on this eti-ologic issue.
All patients in the present study were brought to our hospital because of behavioral disinhibition, prominent delusions, and impaired judgment. No patient had lesions shown in the frontal lobes, but all patients had extensive subfrontal WML. The frontal lobe lesions, which are even neurologically silent, may produce clinical changes in behavior and judgment.33
Subcortical WML, which might disconnect the frontal areas from the remaining brain regions, result in frontal dysfunction. These findings in our patients suggest that the subfrontal connection is impaired in producing some of the abnormal behaviors. However, the findings may be a sampling bias of cases collected in the present study.
In conclusion, the delusional disorder due to diffuse cerebrovascular change could be clinically defined as shown in these seven cases. Patients would have: (i) a later age of onset, (ii) less past and family history, (iii) an acute, subacute and stepwise course, and (iv) more comorbid medical or neurologic disorders. Delusional patients with ‘organic’ factors should receive thorough medical, neurologic and psychiatric evaluations and neuroimaging studies such as MRI. According to the vascular brain disease model of delusion, the result of neuroimaging studies cannot establish a cause–effect relationship of the disease, but suggest the contributory factors for clinical corrections if possible.
The weakness of the present study includes the small number of subjects and the bias of sampling in case selection. The results of the present study may limit the generalization of interpreting the data. As
indicated previously, further studies in larger number of patients with vascular delusions are needed to expand the preliminary knowledge obtained from this study.
REFERENCES
1. American Psychiatric Association. Diagnostic and Sta-tistical Manual of Mental Disorders, 4th edn. American Psychiatric Association, Washington DC, 1994.
2. Cummings JL. Psychosis in neurologic disease: Neurobi-ology and pathogenesis. Neuropsychiatr. Neuropsychol. Behav. Neurol. 1992; 5: 144–150.
3. Peroutka SJ, Sohmer B, Kumar AJ et al. Hallucinations and delusions following a right temporoparietooccipital infarction. Johns Hopkins Med. J. 1982; 151: 181–185. 4. Levine DN, Finklestein S. Delayed psychosis after right
temporoparietal stroke or trauma: Relation to epilepsy. Neurology 1982; 32: 267–273.
5. Flynn FG, Cummings JL, Scheibel J et al. Monosympto-matic delusions of parasitosis associated with ischemic cerebrovascular disease. J. Geriatr. Psychiatry Neurol. 1989; 2: 134–139.
6. Feinberg TE, Shapiro RM. Misidentification-reduplication and the right hemisphere. Neuropsychiatr. Neuropsychol. Behav. Neurol. 1989; 2: 39–48.
7. de Pauw KW, Szulecka TK, Poltock TL. Fregoli syn-drome after cerebral infarction. J. Nerv. Mental Dis. 1987; 175: 433–437.
8. Cummings JL. Organic delusions. Br. J. Psychiatry 1985; 146: 184–197.
9. Flint AJ. Delusion in dementia: A review. J. Neuropsy-chiatry Clin. Neurosci. 1991; 3: 121–130.
10. Breitner JCS, Husain MM, Figiel GS et al. Cerebral white matter disease in late-onset paranoid psychosis. Biol. Psychiatry 1990; 28: 266–274.
11. Miller BL, Lesser IM, Boone K et al. Brain white-matter lesions and psychosis. Br. J. Psychiatry 1989; 155: 73– 78.
12. American Psychiatric Association. Diagnostic and Sta-tistical Manual of Mental Disorders, 3rd edn revised. American Psychiatric Association, Washington DC, 1987.
13. Braffman BH, Zimmerman RA, Trojanowski JQ et al. Pathological correlation with gross and histopathologi-cal change: II. Hyperintense white-matter foci in elderly. Am. J. Neuroradiol. 1988; 9: 629–636.
14. Brant-Zawadzki M, Fein G, Van Dyke C et al. MR imaging of the aging brain: Patchy white-matter lesions and dementia. Am. J. Neuroradiol. 1985; 6: 675–682. 15. Hachinski V. Vascular dementia: A radical redefinition.
Dementia 1994; 5: 130–132.
16. Wetterling T, Kanitz RD, Borgis KJ. The ICD-10 criteria for vascular dementia. Dementia 1994; 5: 185–188. 17. Wallin A, Blennow K. The clinical diagnosis of vascular
dementia. Dementia 1994; 5: 181–184.
18. Cummings JL. Vascular subcortical dementias: Clinical aspects. Dementia 1994; 5: 177–180.
19. Liu CK, Miller BL, Cummings JL et al. A quantitative MRI study of vascular dementia. Neurology 1992; 42: 138–143.
20. Alexopoulos GS, Meyers BS, Young RC et al. ‘Vascular depression’ hypothesis. Arch. Gen. Psychiatry 1997; 54: 915–922.
21. Alexopoulos GS, Meyers BS, Young RC et al. Clinically defined vascular depression. Am. J. Psychiatry 1997; 154: 562–565.
22. Angeleri F, Angeleri VA, Foschi N et al. Depression after stroke: An investigation through catamnesis. J. Clin. Psychiatry 1997; 58: 261–265.
23. Krishnan KRR, Hays JC, Blazer DG. MRI-defined vas-cular depression. Am. J. Psychiatry 1997; 154: 497–501. 24. Alexander GE, DeLong MR, Strick PI. Parallel
organi-zation of functionally segregated circuits linking basal ganglia and cortex. Ann. Rev. Neurosci. 1986; 9: 357–381. 25. Filley CM, Gross KF. Psychosis with cerebral white matter disease. Neuropsychiatr. Neuropsychol. Behav. Neurol. 1992; 5: 119–125.
26. Krishnan KRR. Neuroanatomic substrates of depres-sion in the elderly. J. Geriatr. Psychiatry Neurol. 1993; 6: 39–58.
27. Robinson RG, Kubo KL, Starr LB, Rao K, Price TR. Mood disorders in stroke patients: importance of loca-tion of lesion. Brain 1984; 107: 81–93.
28. Cummings JL. Organic psychosis: Delusional disorders and secondary mania. Psychiatr. Clin. North. Am. 1986; 9: 293–311.
29. Andreasen NC, Paradiso S, O’Leary DS. ‘Cognitive metria’ as an integrative theory of schizophrenia: A dys-function in cortical-subcortical-cerebellar circuitry? Schizophr. Bull. 1998; 24: 203–218.
30. Brust JCM. Vascular dementia is overdiagnosed. Arch. Neurol. 1988; 45: 799–801.
31. O’Brien MD. Vascular dementia is underdiagnosed. Arch. Neurol. 1988; 45: 797–798.
32. Geldmacher DS, Whitehouse PJ. Multi-infarct dementia. In: Bloom FE, Kupfer DJ (eds). Neuropsychopharma-cology: the Fourth Generation of Progress. Raven Press, New York, 1993; 1513–1520.
33. Stuss DT, Benson DF. Neuropsychological studies of the frontal lobes. Psychol. Bull. 1984; 95: 3–28.