For Peer Review
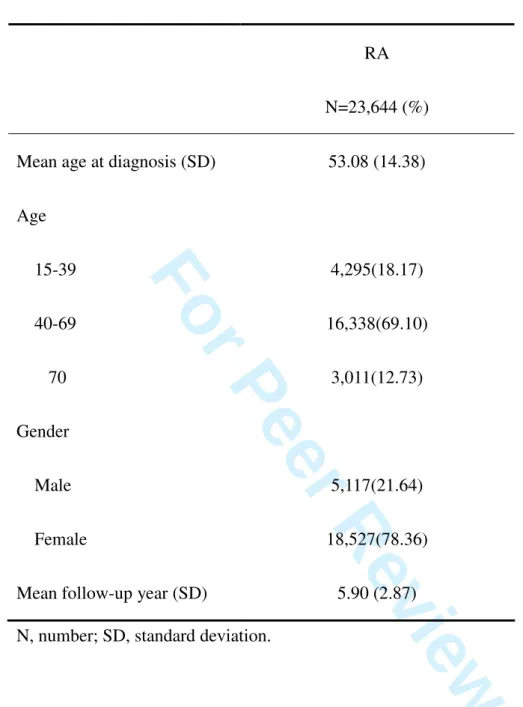
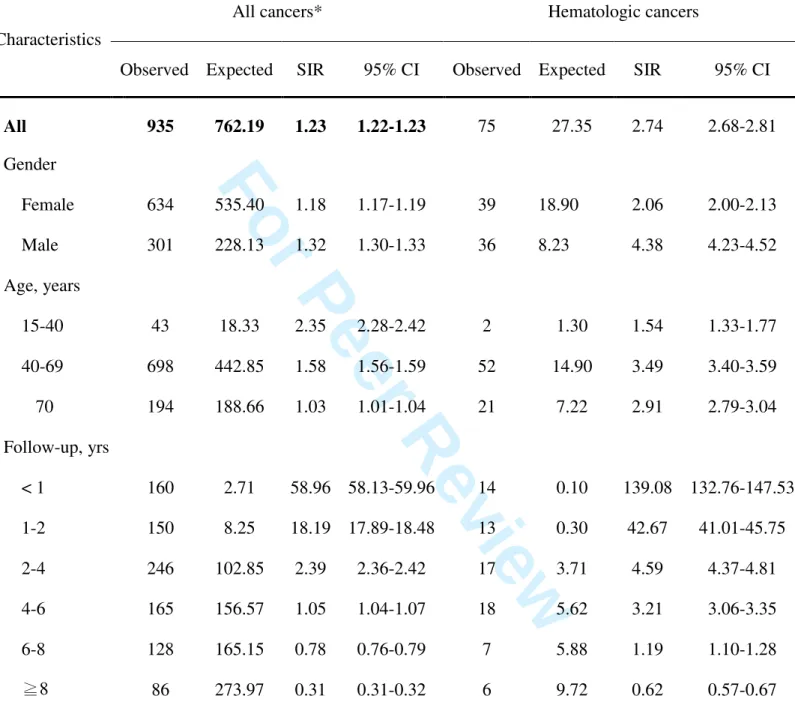
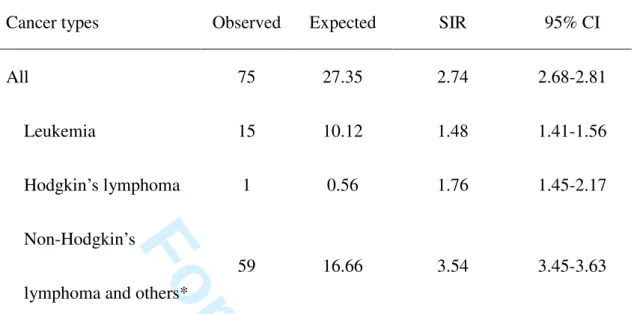
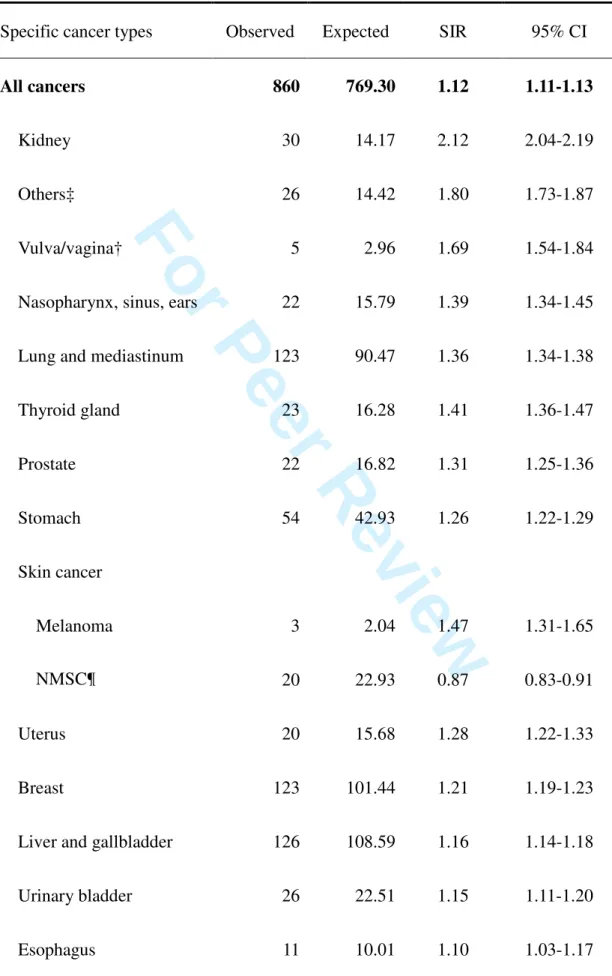
The risk of cancer in rheumatoid arthritis patients: a nationwide cohort study in Taiwan
Journal: Arthritis and Rheumatism Manuscript ID: ar-10-0893.R1
Wiley - Manuscript type: Full Length Date Submitted by the
Author: n/a
Complete List of Authors: Chen, Yi-Ju; Taichung Veterans General Hospital, Dermatology;
National Yang-Ming University, Faculty of Medicine
Chang, Yun-Ting; National Yang-Ming University, Faculty of Medicine
Wang, Chang-Bi; Taichung Veterans General Hospital, Division of Gastroeneterology
Wu, Chun-Ying; China Medical University, College of Public Health;
National Yang-Ming University, Faculty of Medicine; Taichung Veterans General Hospital, Division of Gastroeneterology Keywords: Cohort Study, Epidemiology, Rheumatoid Arthritis
For Peer Review
1
The risk of cancer in rheumatoid arthritis patients: a nationwide cohort study in Taiwan
Yi-Ju Chen, M.D., Ph.D.,
1,2Yun-Ting Chang, M.D., Ph.D.,
2,3Chang-Bi Wang, M.S.,
4Chun-Ying Wu, M.D., Ph.D., M.P.H.
2,4,51
Department of Dermatology, Taichung Veterans General Hospital, Taichung;
2
Faculty of Medicine, National Yang-Ming University, Taipei;
3
Department of Dermatology, Taipei Veterans General Hospital, Taipei
4
Department of Public Health, College of Public Health, China Medical University, Taichung;
5