Urological Notes
Concurrent chemoradiotherapy in patients with non-metastatic upper urinary tract urothelial carcinoma: Report from a single institution in Taiwan
Nai-Wen Kang M.D. , 1,2,3 Kuei-Li Lin M.D., M.S. , 4 Kuan-Hua Huang M.D., Ph.D. , 2,5 Kun-Hung Shen M.D. , 5,6,7 Chung-Han Ho Ph.D. 8
and Yin-Hsun Feng M.D., Ph.D. 1,3
Abbreviations & Acronyms AUC = area under the curve CCRT = concurrent chemoradiotherapy PNI = perineural invasion UTUC = urinary tract urothelial carcinoma
1
Division of Hematology and Oncology, Department of Internal Medicine, Chi Mei Medical Center,
2Chia Nan University of Pharmacy and Science,
3Department of Nursing, College of Medicine and Life Science, Chung Hwa University of Medical Technology,
4Department of Radiation Oncology,
5Division of Urology, Department of Surgery, Chi Mei Medical Center,
6Department of
Optometry, College of Medicine and Life Science, Chung Hwa University of Medical Technology, Tainan,
7
Department of Urology, Taipei Medical University, Taipei, and
8
Department of Medical Research, Chi Mei Medical Center, Tainan, Taiwan yinhsun.feng@gmail.com DOI: 10.1111/iju.14112
The standard treatment for non-metastatic upper UTUC is radical nephroureterectomy with removal of an ipsilateral bladder cuff.
1Removal of the kidney might affect the patient ’s quality of life, especially in patients with declined renal function on the contralateral kidney. In addi- tion, not all of the patients can achieve R0 resection. The combined therapeutic modalities with chemotherapy and radiotherapy can be considered in curative intention for patients with incom- plete surgical resection or for those not medically fit for surgery. As these tumors have relatively low incidence, there are insufficient data to reach a consensus on the optimal treatment choice other than complete resection. The present study reports the clinical outcome of platinum-based CCRT for patients with non-metastatic UTUC in Taiwan. A total of 21 patients with non-meta- static UTUC were included at Chi Mei Medical Center from January 2011 to August 2015.
Patients with regional lymph node involvement were included, but patients with distant metasta- sis proven by imaging studies were ineligible. The patients in the present study were either med- ically un fit to receive surgery or had gross post-surgical residual tumor.
The patients underwent platinum-based CCRT. The cytotoxic agents used for CCRT were weekly intravenous cisplatin 30 mg/m
2on day 1 during radiotherapy. For patients with impaired renal function (serum creatinine >1.5 mg/dL or creatinine clearance <60 mL/min), weekly intravenous carboplatin AUC = 1.5 on day 1 was administered instead. After that, patients received sequential chemotherapy with two cycles of platinum-based regimen GC (gemcitabine 1000 mg/m
2i.v. on days 1, 8 and 15, and cisplatin 70 mg/m
2i.v. on day 1).
For patients with impaired renal function (serum creatinine >1.5 mg/dL or creatinine clear- ance <60 mL/min), cisplatin was replaced by carboplatin AUC = 4. For radiation therapy, computed tomography-based planning facilitated the accuracy of the treatment. The clinical target volume should include either the renal fossa (for residual tumor after operation) or gross tumor only (for patients who did not receive operation), along with the course of the ureter to the bladder wall at the ipsilateral trigone, and the field also encompassed the para- caval and para-aortic lymph nodes at risk of harboring metastatic disease. Irradiation dose of 45–50 Gy in 1.8–2 Gy daily was used for postoperative subclinical and microscopic disease;
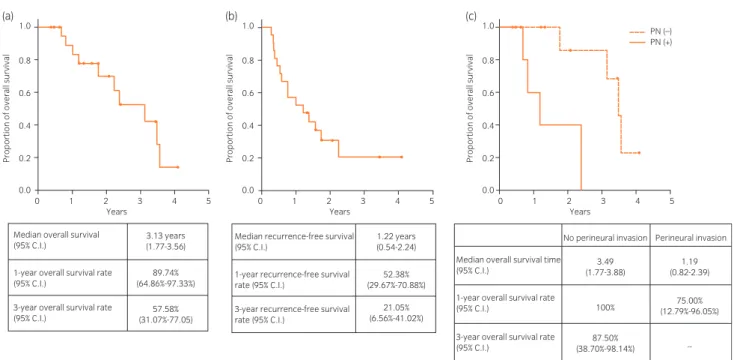
for unresectable gross tumors or postoperative residual tumors, a boost of 5–10 Gy to the gross tumor was used. Patient characteristics are shown in Table S1. These patients were fol- lowed until 31 December 2016. The median follow-up period was 3.5 years. A total of 10 (47.6%) patients died. The median overall survival was 3.13 years (Fig. 1a), and the median recurrence-free survival was 1.22 years (Fig. 1b). The 3-year overall survival rate and 3-year recurrence-free survival rate were 57.58% and 21.05%, respectively. We also showed overall survival stratified by tumor location, renal function, lymph node involvement, surgical margin status, lymphovascular invasion and PNI. Among these factors, the median overall survival was signi ficantly shorter only in the patients with PNI than the patients without PNI (1.19 years vs 3.49 years, P = 0.0076; Fig. 1c). The adverse effects of chemoradiotherapy are listed in Table S2.
UTUCs are extremely rare. There are insufficient data in the literature regarding the treatment and still no consensus on the optional treatment choice. Radical nephroureterectomy with removal of an ipsilateral bladder cuff is accepted as the curative therapy for non-metastatic UTUC, providing local tumor control and survival bene fit. The present retrospective study was designed to investigate the efficacy of CCRT in this population unfit for operation. Most of the patients had stage III and stage IV disease with lymph node involvement or were medically un fit to receive surgery. The 3-year overall survival rate and 3-year recurrence-free survival rate was 57.58% and 21.05%, respectively. Margulis et al. reported that the 3-year recurrence-free survival rate after radical nephroureterectomy is 51.5% for stage T3 disease and 15.7% for stage T4 disease.
2A prospective randomized study would be the most optimal method to show the role of CCRT in UTUC. However, given the rarity of this malignancy, the development of a prospective randomized study might be difficult without collaboration among multiple
© 2019 The Japanese Urological Association
83
International Journal of Urology (2020) 27, 83--92
institutions. In conclusion, for non-metastatic UTUCs, CCRT can be considered for patients with unfavorable prognostic fac- tors or who are medically un fit for surgery.
Conflict of interest
None declared.
References
1 Cai G, Liu X, Bin W. Treatment of upper urinary tract urothelial carcinoma.
Surg. Oncol. 2011; 20: 43–55.
2 Margulis V, Shariat SF, Matin SF et al. Outcomes of radical nephroureterec- tomy: a series from the upper tract urothelial carcinoma collaboration. Cancer 2009; 115: 1224–33.
Supporting information
Additional Supporting Information may be found in the online version of this article at the publisher’s web-site:
Table S1. The clinicopathological parameters of these 21 patients. *Just 16 cases with surgical resection had resected tumor samples for pathological evaluation.
Table S2. The adverse effects of chemoradiotherapy.
Urological Note
(a)
1.0Median overall survival
(95% C.I.) 3.13 years
(1.77-3.56) 1.22 years
(0.54-2.24) No perineural invasion
3.49 (1.77-3.88)
1.19 (0.82-2.39)
75.00%
(12.79%-96.05%)
-- 100%
87.50%
(38.70%-98.14%)
Perineural invasion
52.38%
(29.67%-70.88%)
21.05%
(6.56%-41.02%) 89.74%
(64.86%-97.33%)
57.58%
(31.07%-77.05) 1-year overall survival rate
(95% C.I.)
3-year overall survival rate (95% C.I.)
Median overall survival time (95% C.I.)
1-year overall survival rate (95% C.I.)
3-year overall survival rate (95% C.I.)
Median recurrence-free survival (95% C.I.)
1-year recurrence-free survival rate (95% C.I.)
3-year recurrence-free survival rate (95% C.I.)
(b)
0.8
Proportion of overall survival
0.6
0.4
0.2
0.0
0 1 2 3 4
Years
5 0 1 2 3 4
Years
5 1.0
0.8
Proportion of overall survival
0.6
0.4
0.2
0.0
(c)
0 1 2 3 4
Years
5
1.0 PN (–)
PN (+) 0.8
Proportion of overall survival
0.6
0.4
0.2
0.0