Retinal vein occlusion and the risk of acute
myocardial infraction: a 3-year follow-up study
C-C Hu,
1,2,3,4J-D Ho,
1,2H-C Lin
51College of Medicine, Taipei
Medical University, Taipei, Taiwan;2Department of
Ophthalmology, Taipei Medical University Hospital, Taipei, Taiwan;3Department of
Ophthalmology, Shin Kong Wu-Ho-Su Memorial Hospital, Taipei, Taiwan;4School of Medicine, Fu-Jen Catholic University, Hsingchuang, Taiwan;5School of Health Care Administration, Taipei Medical University, Taipei, Taiwan
Correspondence to: Professor H-C Lin, School of Health Care Administration, Taipei Medical University, 250 Wu-Hsing Street, Taipei 110, Taiwan;
henry11111@tmu.edu.tw Accepted 28 November 2008 Published Online First 10 February 2009
ABSTRACT
Aim: Using a nationwide population-based dataset, this study investigated the relationship between retinal vein occlusion (RVO) and subsequent acute myocardial infarction (AMI).
Methods: This study is based on a nationwide database released by the Taiwan National Health Research Institute. The study cohort consisted of all ambulatory care patients who were diagnosed as having RVO during 2000,2003 (n = 591), while the control cohort com-prised 2955 randomly selected patients extracted from the same dataset; five patients for every RVO patient, matched by age and gender. Each patient was individually tracked for 3 years from their index ambulatory care visit. Cox proportional hazard regressions were performed to compute the adjusted 3-year AMI-free survival rates, comparing these two cohorts.
Results: RVO patients had a significantly higher rate of AMI (1.86% vs 0.78%) during the 3-year follow-up period than patients in the comparison group (p = 0.032). However, after adjusting for the patients’ gender, age, geographic region and comorbid medical disorders, there was no significant difference between the central retinal vein occlusion, branch retinal vein occlusion patients and the comparison group in terms of the hazard of AMI during the 3-year follow-up period.
Conclusion: RVO did not independently increase the risk of AMI.
Retinal vein occlusive (RVO) disorders, including central retinal vein occlusion (CRVO) and branch retinal vein occlusion (BRVO), constitute a major cause of severe vision impairment and blindness.1–3
The reported prevalence of RVO ranges from 0.3% to 1.6%.4–7Although the life expectancy of patients
with retinal vein occlusion is not shortened,8 9over
50% of deaths occur in the 6 years immediately following the onset of RVO,8
and the proportion of deaths by myocardial infarction is increased.4 8 9
Most studies on the topic to date have taken myocardial infarction mortality as the outcome indicator, an approach which may underestimate episodes of myocardial infarctions.4 8–10 Although
Martin et al calculated coronary heart disease risk (cCHDR) using Framingham algorithms showing increased risk of future cardiovascular disease for RVO patients,11
without actual clinical data, they could not prove it. Furthermore, most studies have tended to use regional samples, or data from a few hospitals or select subpopulations of patients,4 8 12
and as such do not permit unequivocal conclusions. Using a nationwide population-based dataset from Taiwan, this study investigated the rate of RVO and subsequent risk of acute myocardial infarction (AMI). Based on the previous literature,
we hypothesised that RVO would be a significant predictor of AMI.
METHODS Database
This study used a nationwide database released by the Taiwan National Health Research Institute (NHRI) in 2007. The NHI database contains inpatient expenditures per admission, ambulatory care expenditures per visit, details of ambulatory care orders as well as a registry of those insured from 1996 to 2006. The NHRI used a systematic, random sampling method to extract a representative database from the entire dataset in 2005. This database comprises 1 073 891 random subjects, about 5% of all enrollees (n = 22 717 053) in the National Health Insurance programme. There were no statistically significant differences in age, gender or cost of care between the sample group and all enrollees. Study sample
Our study design consists of a study cohort and a comparison cohort. The study cohort were patients who sought ambulatory care during 2000,2003, receiving a diagnosis of RVO (ICD-9-CM codes 362.35 or 362.36) (n = 665). In order to ensure that cases selected were new episodes and avoiding the potential confounding factor of chronicity, we excluded those patients who had been diagnosed as having RVO during the previous 5-year period (n = 62) and patients previously diagnosed as having AMI (ICD-9-CM codes 410) (n = 12). Ultimately, 591 patients were eligible for inclusion in the study cohort. Our comparison cohort was extracted from the same dataset by randomly selecting five patients for every RVO one, matched by age (,50, 50–59, 60–69 and .69) gender, and the date of their ambulatory care visits (n = 2955). Patients with a previous diagnosis of RVO or AMI were excluded. A total of 3546 patients were included in the present study. Each patient was individually tracked from their index ambulatory care visit in 2000,2003 until the end of 2006 to distinguish all who had AMIs.
Regression modelling adjusted for demographic factors such as patients’ age, gender and the geogra-phical location of the community in which the patient resided, as well as comorbidities. Comorbidities were identified from the medical records 6 months before and after the index ambulatory care visit.
Statistical analysis
The SAS statistical package was used to perform the analyses in this study. Pearson x2 tests were
per-formed to examine the differences between the two cohorts in terms of sociodemographic characteristics and selected comorbid medical disorders. We then
estimated the 3-year AMI-free survival rate using the Kaplan– Meier method and used the logrank test to examine differences in AMI risk for the two cohorts. Cox proportional hazard regressions were then performed to compute the adjusted 3-year AMI-free survival rate for these two cohorts, following adjustment for the variables mentioned above. A level of 0.05 was selected to determine the significance of predictors in the models.
RESULTS
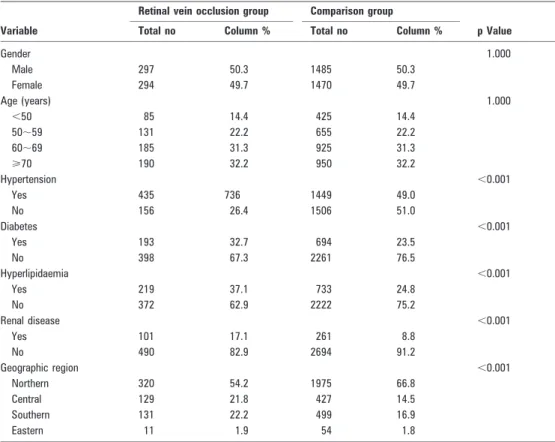
Table 1 shows the distributions of demographic characteristics and comorbid medical disorders for these two cohorts. After matching for age and gender, RVO patients were more likely to have hypertension (p,0.001), diabetes (p,0.001) hyperlipidae-mia (p,0.001) and renal disease (p,0.001) as compared with patients in the comparison group.
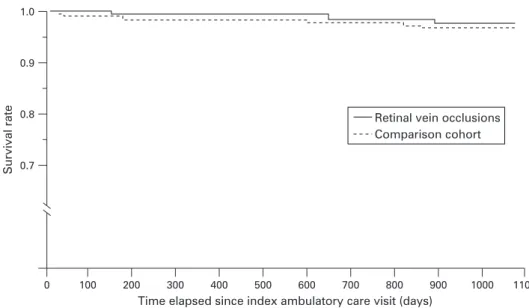
Of the total sample of 3546 patients, 33 patients (0.93%) suffered AMIs during the 3-year follow-up period, 11 (1.86% of the RVO patients) from the study cohort and 23 (0.78% of patients in the comparison cohort) from the comparison cohort (table 2). The logrank test revealed that RVO patients had significantly lower 3-year AMI-free survival rates than patients in the comparison group (p = 0.032). The results of the Kaplan– Meier survival analysis are presented in fig 1.
Table 2 also describes the distribution and crude odds ratios of AMI during the 3-year follow-up period by type of RVO. It shows that 3.13% and 1.39% of CRVO and BRVO patients, respectively, suffered AMIs. The regression analysis reveals that compared with the comparison group, CRVO patients were more likely to suffer AMIs (hazard ratio (HR) = 3.27, 95% CI 1.12 to 9.57) during the 3-year follow-up period. However, no significant difference in the risk of AMIs between BRVO patients and the comparison group was observed.
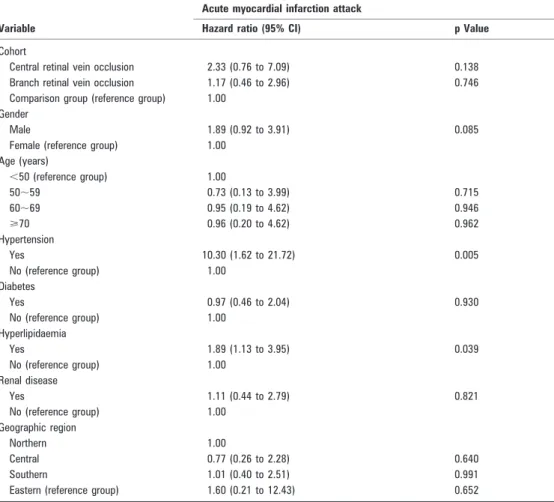
Details of the adjusted hazard ratios for AMI, by cohort, based on Cox proportional hazard regression are shown in
table 3. After adjusting for the patients’ gender, age, geographic region and comorbid medical disorders, there was no significant difference between the CRVO, BRVO patients and the comparison group in terms of the hazard of AMI during the 3-year follow-up period. As expected, patients suffering from hypertension (HR = 10.30, 95% CI 1.62 to 21.72, p = 0.005) and hyperlipidaemia (HR = 1.89, 95% CI 1.13 to 3.95, p = 0.039) had a greater likelihood of AMI.
DISCUSSION
This nationwide population-based study found that RVO patients had a significantly higher rate of AMI (1.86% vs 0.78%) than patients in the comparison group (p = 0.032) during a 3-year follow-up period. However, after adjusting for age, gender and comorbid medical disorders, RVO was no longer a predictor of AMI (p = 0.369). Our finding is consistent with a study by Mansour et al, which reported five subjects out of 78 CRVO patients developed AMI at an average follow-up of 2.8 years. Mansour likewise concluded that CRVO patients do not carry a higher risk of mortality and morbidity than matched controls derived from national surveys.10
However, our finding is not consistent with other studies concluding that RVO patients had a higher proportion of myocardial infarction deaths than the general population.8–10For
example, Rubinstein et al reported 12 acute myocardial infarction deaths (41%) out of 29 total deaths during a mean follow-up period of 9.8 years for the survivor group and 5.4 years for the deceased—about double the rate of the normal population.9
Tsaloumas et al reported that the percentage of deaths from myocardial infarction (22 MI deaths out of 95 total deaths) in the RVO population was significantly higher than among controls (23.1% vs 14.4%, p,0.05) during a mean follow-up period of 9.08 years.8When interpreting the results of such studies, it must
Table 1 Demographic characteristics and comorbid medical disorders for retinal vein occlusion and comparison group patients in Taiwan, 2000–2003 (n = 3546)
Variable
Retinal vein occlusion group Comparison group
p Value
Total no Column % Total no Column %
Gender 1.000 Male 297 50.3 1485 50.3 Female 294 49.7 1470 49.7 Age (years) 1.000 ,50 85 14.4 425 14.4 50,59 131 22.2 655 22.2 60,69 185 31.3 925 31.3 >70 190 32.2 950 32.2 Hypertension ,0.001 Yes 435 736 1449 49.0 No 156 26.4 1506 51.0 Diabetes ,0.001 Yes 193 32.7 694 23.5 No 398 67.3 2261 76.5 Hyperlipidaemia ,0.001 Yes 219 37.1 733 24.8 No 372 62.9 2222 75.2 Renal disease ,0.001 Yes 101 17.1 261 8.8 No 490 82.9 2694 91.2 Geographic region ,0.001 Northern 320 54.2 1975 66.8 Central 129 21.8 427 14.5 Southern 131 22.2 499 16.9 Eastern 11 1.9 54 1.8
Global issues
718 Br J Ophthalmol 2009;93:717–720. doi:10.1136/bjo.2008.151605be kept in mind that mortality from myocardial infarction is not equal to the incidence of myocardial infraction. This could explain why our findings differ from prior ones.
The pathogenesis of RVO remains unclear but may be multi-factoral. The finding of association between RVO and hyperch-olesterolaemia and symptomatic ischaemic heart disease suggests that RVO may be associated with systemic atherosclerotic disease.12Retinal arteriolar sclerotic signs, such as arteriovenous
nicking and focal narrowing, have been shown to be risk factors for RVO.5 13RVO typically occurs at arteriovenous crossings where
the arteriole and venule share a common adventitial sheath, and the sclerotic retinal arteriolar walls may compress underlying venules.14 This compression in turn can transform the normal
laminar venous blood flow into turbulent flow, facilitating the formation of venous thrombus and downstream venous occlu-sion.15
The pathogenesis of AMI is caused by the disruption of atherosclerotic plaques of the coronary arteries and the ensuing thrombus formations which result in coronary artery obstruc-tions.16 So, the occurrence of AMI is directly associated with
coronary artery atherosclerosis, while the occurrence of RVO is indirectly associated with retinal arteriolar atherosclerosis at the arteriovenous crossings. We assume this to be the reason why in this study RVO did not independently increase the risk of AMI.
In our earlier-published report regarding RVO and the risk of stroke, patients with any type of stroke (ICD-9-CM codes 430,438) were included—specifically, both haemorrhagic and occlusive type strokes—and we concluded there was no overall association of RVO with stroke except in the 60–69-year subgroup. RVO patients age 60–69 years had a 2.34-fold (95% CI 1.05 to 5.24) higher risk of suffering a stroke.17
In this study, RVO did not independently increase the risk of AMI. The reason why RVO has different effects on AMI and stroke risk may be partly attributed
to the dual mechanism (haemorrhagic and occlusive) of strokes rather than the single mechanism (occlusive) of AMI.
One strength of this study is our use of nationwide population-based data, precluding possible selection bias. We believe that most patients in Taiwan experiencing RVO search for medical help soon after disease onset, given (1) the number of ophthalmologists on the relatively small island of Taiwan (the ophthalmologist-to-population ratio is 1:14 375, compared with 1:23 523 in the UK), (2) negligible barriers to medical access (the National Health Insurance System in Taiwan allows patients to visit any ophthalmology clinic or hospital department of ophthalmology freely, without referral by a general practitioner), (3) there are no waiting lists to see a doctor, (4) patients pay only about $5 to 15 per visit in a country where gross per capita income in the year 2000 was approximately $15 00018and (5) the inherent severity
and alarming nature of RVO.
Our findings need to be interpreted in the context of the following limitations. First, diagnoses of RVO, AMI or any other comorbid medical conditions that are totally dependent upon administrative claims data may be less accurate than diagnoses obtained through a standardised procedure. Second, data on variables which might contribute to AMI, such as smoking, dietary habits and body mass index, were not available. Third, we used the ICD-9-CM diagnosis code 362.35 (central retinal vein occlusion) as the definition for CRVO and diagnosis code 362.36 (venous tributary (branch) occlusion) as the definition for BRVO, with these two codes representing RVO as a whole. However, since this was a retrospective study, and the diagnosis codes were determined by a variety of doctors, we have reason to believe that some patients with CRVO and BRVO may have been given less specific diagnosis codes, including 362.3 (retinal vascular occlusion) or 362.30 (retinal vascular occlusion, unspecified). Figure 1 AMI-free survival rates For
patients with retinal vein occlusions and comparison cohort in Taiwa.
Table 2 Crude hazard ratios for acute myocardial infarction during the 3-year follow-up period for retinal vein occlusion and comparison group patients in Taiwan (n = 3546)
Development of acute myocardial infarction
Comparison group
Retinal vein occlusion
Total Central retinal vein occlusion Branch retinal vein occlusion
No (%) No (%) No (%) No (%)
3-year follow-up period
Yes 23 (0.78) 11 (1.86) 5 (3.13) 6 (1.39)
No 2932 (99.22) 580 (98.14) 155 (96.87) 425 (98.61)
Crude hazard ratio (95% CI) 1.00 2.20* (1.04 to 4.67) 3.27* (1.12 to 9.57) 1.80 (0.73 to 4.45) *p,0.05.
Nevertheless, adding these patients (n = 174) into the analyses did not change our findings.
Fourth, there are patients with asymptomatic RVO occurring in small veins. These asymptomatic RVO cases can only be picked up using retinal photography. This study can only include symptomatic RVO patients. Therefore, there is likely to be some misclassification of RVO cases and controls in this study that might bias our results.
Lastly, there were only 34 patients who suffered AMI over a 3-year period. The number is relatively small, and the follow-up duration is relatively short. Additional studies with larger samples may be needed to verify our negative findings.
In summary, this study found that RVO patients have a significantly higher incidence of AMI and lower AMI-free survival rates during a 3-year follow-up period. After adjusting for possible confounding factors, however, a diagnosis of RVO was not associated with an increased hazard of subsequent AMI. Our findings imply that RVO does not independently increase the hazard of AMI, but rather the high rates of hypertension and hyperlipidaemia among RVO patients result in a higher rate of AMI than the general population. We suggest that RVO patients, in particular those with other cardiovascular comorbidites, undergo comprehensive haematological examination to help clinicians identify those who are potentially at risk of AMI in the near future. Competing interests: None.
REFERENCES
1. Branch Vein Occlusion Study Group. Argon laser scatter photocoagulation for prevention of neovascularization and vitreous haemorrhage in branch vein occlusion. A randomized clinical trial. Arch Ophthalmol 1986;104:34–41.
2. The Central Vein Occlusion Study Group. Natural history and clinical management of central retinal vein occlusion. Arch Ophthalmol 1997;115:486–91. 3. Attebo K, Mitchell P, Smith W. Visual acuity and the causes of visual loss in
Australia. The Blue Mountains Eye Study. Ophthalmology 1996;103:357–64. 4. Cugati S, Wang JJ, Knudtson MD, et al. Retinal vein occlusion and vascular
mortality: pooled data analysis of 2 population-based cohorts. Ophthalmology 2007;114:520–4.
5. Wong TY, Larsen EK, Klein R, et al. Cardiovascular risk factors for retinal vein occlusion and arteriolar emboli: the Atherosclerosis Risk in Communities & Cardiovascular Health studies. Ophthalmology 2005;112:540–7.
6. Xu L, Liu WW, Wang YX, et al. Retinal vein occlusions and mortality: the Beijing Eye Study. Am J Ophthalmol 2007;144:972–3.
7. Klein R, Klein BE, Moss SE, et al. The epidemiology of retinal vein occlusion: the Beaver Dam Eye Study. Trans Am Ophthalmol Soc 2000;98:133–41.
8. Tsaloumas MD, Kirwan J, Vinall H, et al. Nine year follow-up study of morbidity and mortality in retinal vein occlusion. Eye 2000;14:821–7.
9. Rubinstein K, Jones EB. Retinal vein occlusion: long-term prospects: 10 years’ follow-up of 143 patients. Br J Ophthalmol 1976;60:148–50.
10. Mansour AM, Walsh JB, Henkind P. Mortality and morbidity in patients with central retinal vein occlusion. Ophthalmologica 1992;204:199–203.
11. Martin SC, Butcher A, Martin N, et al. Cardiovascular risk assessment in patients with retinal vein occlusion. Br J Ophthalmol 2002;86:774–6.
12. Lim LL, Cheung N, Wang JJ, et al. Prevalence and risk factors of retinal vein occlusion in an Asian population. Br J Ophthalmol 2008;92:1316–19.
13. Cheung N, Klein R, Wang JJ, et al. Traditional and novel cardiovascular risk factors for retinal vein occlusion: the multiethnic study of atherosclerosis. Invest Ophthalmol Vis Sci 2008;49:4297–302.
14. Opremcak EM, Bruce RA. Surgical decompression of branch retinal vein occlusion via arteriovenous crossing sheathotomy: a prospective review of 15 cases. Retina 1999;19:1–5.
15. Verougstraete C. Is change of the vessel wall a risk factor for venous thrombosis? Lancet 1999;353:2158.
16. Libby P. Current concepts of the pathogenesis of the acute coronary syndromes. Circulation 2001;104:365–72.
17. Ho JD, Liou SW, Lin HC. Retinal vein occlusion and the risk of stroke development: a five-year follow-up study. Am J Ophthalmol. In press.
18. Anon. Data from Directorate-General of Budget, Accounting and Statistics, Executive Yuan, Republic of China (Taiwan), 2008.
Table 3 Adjusted hazard ratio and 95% CI for AMI during the 3-year follow-up period for retinal vein occlusion and comparison group patients in Taiwan
Variable
Acute myocardial infarction attack
Hazard ratio (95% CI) p Value
Cohort
Central retinal vein occlusion 2.33 (0.76 to 7.09) 0.138
Branch retinal vein occlusion 1.17 (0.46 to 2.96) 0.746
Comparison group (reference group) 1.00 Gender
Male 1.89 (0.92 to 3.91) 0.085
Female (reference group) 1.00 Age (years) ,50 (reference group) 1.00 50,59 0.73 (0.13 to 3.99) 0.715 60,69 0.95 (0.19 to 4.62) 0.946 >70 0.96 (0.20 to 4.62) 0.962 Hypertension Yes 10.30 (1.62 to 21.72) 0.005 No (reference group) 1.00 Diabetes Yes 0.97 (0.46 to 2.04) 0.930 No (reference group) 1.00 Hyperlipidaemia Yes 1.89 (1.13 to 3.95) 0.039 No (reference group) 1.00 Renal disease Yes 1.11 (0.44 to 2.79) 0.821 No (reference group) 1.00 Geographic region Northern 1.00 Central 0.77 (0.26 to 2.28) 0.640 Southern 1.01 (0.40 to 2.51) 0.991
Eastern (reference group) 1.60 (0.21 to 12.43) 0.652
Global issues
doi: 10.1136/bjo.2008.151605
10, 2009
2009 93: 717-720 originally published online February
Br J Ophthalmol
C-C Hu, J-D Ho and H-C Lin
study
myocardial infraction: a 3-year follow-up
Retinal vein occlusion and the risk of acute
http://bjo.bmj.com/content/93/6/717.full.html
Updated information and services can be found at:
These include:
References
http://bjo.bmj.com/content/93/6/717.full.html#related-urls
Article cited in:
http://bjo.bmj.com/content/93/6/717.full.html#ref-list-1
This article cites 16 articles, 7 of which can be accessed free at:
service
Email alerting
the box at the top right corner of the online article.
Receive free email alerts when new articles cite this article. Sign up in
Collections
Topic
(5452 articles)
Epidemiology
(1163 articles)
Retina
Articles on similar topics can be found in the following collections
Notes
http://group.bmj.com/group/rights-licensing/permissions
To request permissions go to:
http://journals.bmj.com/cgi/reprintform
To order reprints go to:
http://group.bmj.com/subscribe/