IINNTTRROODDUUCCTTIIOONN
Spinal cord injury (SCI) can result from traumatic and nontraumatic causes, with the latter accounting for 33% to 79% of all SCI rehabilitation admissions [1,2]. The pathogenesis of nontraumatic spinal cord injury includes such etiologies as vertebral spondylosis (spinal stenosis), infection, vascular ischemia, congenital disease and tumorous compression. Spinal cord tumors can be divided into intramedullary (about 5%) or extramedullary (intradural, 40%;
extradural, 55%), and both may be primary or secondary [3]. Secondary spinal tumors are more common than primary, with extradural metastases being the most common [3]. Extradural secondary tumors, on the other hand, are metastases from other sites of the body, including the lung, breast,
prostate, kidney, the thyroid gland or the gastrointestinal tract. Cholangiocarcinomas are malignant tumors that arise from the epithelia of bile ducts, and may cause local advanced disease and regional lymphatic metastasis. Distal metastases to the thoracic spine, neck and humerus have been reported [4-6]. In this article, we present a rare case of cholangiocarcinoma which had metastasized to the cervical spine. The functional independence measurement (FIM) score on admission to inpatient rehabilitation in patients with SCI caused by metastatic disease is of paramount importance because it is a more reliable predictive variable of survival time than tumor type or level of lesion [7].
C
CAASSEE RREEPPOORRTT
A 59-year-old woman presented to the neurosurgery outpatient department with a two- month history of neck soreness, and recent history of weakness of both hand muscles. The neck
Both traumatic and nontraumatic events can cause spinal cord injury (SCI). Of the nontraumatic causes of SCI, tumors affecting the spinal cord are among the most common, especially in individuals over the age of 40 years. Secondary spinal tumors are more common than primary tumors. The most frequent origins of metastatic spinal tumor are lung, breast and prostatic cancer, and the tumors most commonly involve the thoracic spine. We describe a rare case of cervical spine metastatic adenocarcinoma, which originated from cholangiocarcinoma.
The patient initially presented with neck soreness. The symptoms of neck soreness and radicular pain usually result from irritation of spinal nerve or its root secondary to degenerative change in the elderly. This case illustrates the importance of submitting all patients with neck pain to a comprehensive examination for an underlying cause. ( Mid Taiwan J Med 2003;8:231-7)
K
Keeyy wwoorrddss
cholangiocarcinoma, rehabilitation, spinal metastases, spinal cord injury
Received : July 28, 2003. Revised : August 26, 2003.
Accepted : October 17, 2003.
Address reprint requests to : Li-Wei Chou, Department of Physical Medicine and Rehabilitation, China Medical University Hospital, 2 Yuh-Der Road, Taichung 404, Taiwan, R.O.C.
Spinal Cord Injury Caused by Cervical Spine Metastatic Cholangiocarcinoma
Yng-Yu Lin, Mu-Jung Kao, Wen-Hsin Huang1, Der-Yang Cho2, Li-Wei Chou
Department of Physical Medicine and Rehabilitation, 1Division of Gastroenterology, and 2Department of
Neurosurgery, China Medical University Hospital, Taichung, Taiwan, R.O.C.
soreness began after she hyperextended her neck while playing badminton. She initially sought traditional chiropractic treatment, but the numbness progressively radiated to the medial aspect of both forearms, and to the ring and small fingers. About one- and -a-half-months after the initial injury, she visited the neurosurgery outpatient department complaining of muscle weakness in both hands. Her medical history included an operation over the gallbladder area ten years ago and chronic insomnia. There was no contributory family history. Physical examination revealed atrophy of both thenar muscles, normal grade muscle power (MP) in all four limbs but only good grade MP of flexor muscles of both fingers, decreased sensation over bilateral C8 and T1 dermatomes, and increased deep tendon reflex (DTR) of both lower limbs. Plain film of cervical- spine and chest demonstrated increased opacity with mottled densities noted on the left side of C7 and T1 vertebrae. Cervical-spine magnetic resonance (MR) image showed low-signal intensity on T1-weighted images, high-signal intensity on long TR-weighted images at C7-T2 bony parts, and a soft tissue mass in the prevertebral and anterior epidural spaces, mainly at the level of T1 (Fig. 1). Paresthesia in both lower limbs, stool and urinary incontinence and tetraplegia developed within half a day. A foley catheter was inserted for urinary retention.
Physical examination before the emergency spinal surgery revealed grade 5/5 MP of the extensor muscles at both elbows, grade 2/5 MP of flexor and intrinsic muscles of both fingers, grade 0/5 MP of both lower limbs, decreased sensation from C8 to S5 dermatomes, decreased superficial abdominal reflex, DTR in both knees, ankle jerks and bulbocavernous reflex. Emergency surgical intervention with anterior discectomy, C6/C7, C7/T1, T1/T2, C7 corpectomy, and vertebroplasty with polymethylacrylate and anterior equnix plate fixation was performed. One week after spinal surgery, her condition had improved: grade 4/5 MP of flexor and intrinsic muscles of both fingers, grade 3/5 MP of both lower limbs, and FIM score was 50 (full score is 126). Spinal
A
Fig. 1. A: Sagittal T1-weighted MR image of cervical spine shows pathologic compression fracture at T1 vertebral body (arrow) and replacement of fatty marrow by low signal intensity tumor at the C7, T1 and T2 vertebral bodies. B:
Sagittal short-tau inversion recovery (STIR) MR image shows heterogenous high signal intensity soft tissue mass in prevertebral and anterior epidural spaces mainly at the level of T1, resulting in spinal cord compression (arrows). C: Axial gradient echo T2* image of cervical spine shows epidural and paravertebral soft tissue mass, causing compression of the spinal cord and bilateral neurofoamens (arrows).
C
B
surgery and pathology revealed a metastatic mucinous adenocarcinoma of unknown origin (Fig. 2).
A metastasis work-up was performed. At the same time, comprehensive rehabilitation programs were offered to improve her mobility and daily living disabilities. Laboratory examination revealed normal carcinoembryonic antigen (CEA) and alpha-fetoprotein (AFP) levels, cancer antigen (CA) 19-9 level of 3,2118 U/mL (normal range < 37), and a mildly elevated CA-125 level. Liver function was normal and no evidence of jaundice or elevation in alkaline phosphate was noted. However, she was seropositive for hepatitis B virus (HBV).
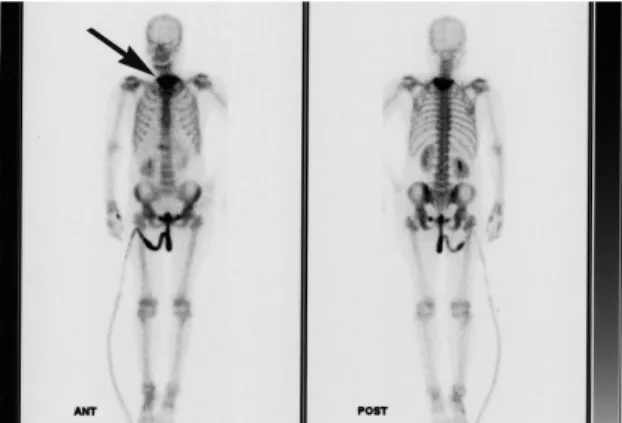
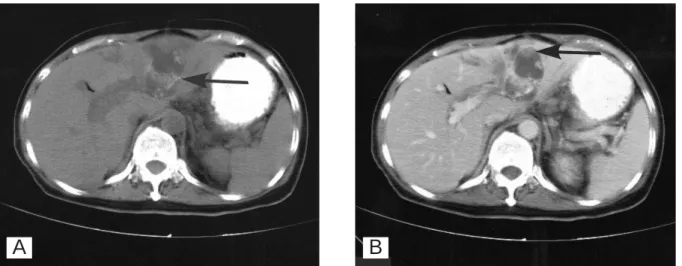
Abdominal sonography showed a mixed and hyperechoic tumor 4.8 cm in size, and dilated intrahepatic ducts (IHD) in the left lobe of the liver (Fig. 3). Colonfiberscopic study showed no significant findings. Bone scintigraphy demonstrated heterogeneous intense tracer uptake in the lower cervical/upper thoracic spinal region (about C7-T2 levels), but no evidence of abnormalities elsewhere (Fig. 4). The gallium-67 citrate whole body scan showed a "cold" area with surrounding increased tracer uptake in the left lobe of the liver; no other abnormal uptake was present elsewhere (Fig. 5). Pre-contrast and contrast abdominal computed tomography showed a low attenuated mass with amorphous
Fig. 2. Histological examination of the resected specimens disclose some tumor nests composed of mucinous glands and pieces of necrotic bony fragments embedded in fibrous tissue. The tumorous glands have high columnar lining with abundant clear cytoplasm and basally located nuclei.
Metastatic mucinous adenocarcinoma is considered.
Fig. 3. Abdominal sonography shows a mixed and hyperechoic tumor 4.8 cm in size, and dilated intrahepatic ducts in the left lobe of the liver.
Fig. 4. Technetium-99m methylene diphosphonate whole body bone scan shows heterogeneous intense tracer uptake in the lower cervical/upper thoracic spinal region (about C7-T2 levels), but no evidence of abnormalities elsewhere.
Fig. 5. Gallium-67 citrate whole body scan shows a "cold"
area with surrounding increased tracer uptake in the left lobe of the liver; no other abnormal uptake is present elsewhere.
calcification in the left lobe of the liver and intrahepatic ductal dilatation (Fig.6).
Cholangiocarcinoma was therefore considered.
Magnetic resonance cholangiopancreatography (MRCP) showed marked dilatation of the left lobe of the IHD; a tumoral nodule was also seen in the left lobe of the IHD. The preliminary diagnosis was cholangiocarcinoma. We arranged an excision of the tumor to confirm cholangio- carcinoma, but postponed the procedure because the patient was intubated with an endotracheal tube and was on ventilator treatment for accidentally complicated aspiration pneumonia.
She became comatous due to sepsis, and she underwent conservative treatment for the hepatic mass. She remained unconscious and ventilator- dependent until she died of cardiopulmonary failure about five months after the onset of spinal cord injury.
D
DIISSCCUUSSSSIIOONN
Spinal Cord Injury Caused by Tumors Back pain is reported in more than 80% of patients with a tumor involving the spine [8].
Radicular pain may also occur as a result of compression of nerve roots. Complaints may precede the diagnosis by days to months, but once neurological signs exist, progression is usually rapid. Early recognition is important as ambulatory ability and maintenance of bowel and
bladder control at the time therapy is begun correlate highly with the ultimate functional outcome of the patient [9].
Spinal cord tumors (primary and secondary) are most common at the thoracic level (70%), followed by the lumbarsacral level (20%), and the cervical spine [1]. The most common causes of neck pain and radiculopathy are herniated nucleus pulposus and cervical spondylosis. However, if the patient has persistent symptoms or the patient's condition worsens despite appropriate treatment, then further investigation is warranted.
Plain radiography of the spine to detect vertebral body metastases is relatively insensitive because at least 50% of the bone must be destroyed before a lesion can be seen clearly [10].
Plain radiographs are inexpensive and noninvasive, but show lesions in only 60% of patients with metastatic bone disease.
Radionuclide scans are highly sensitive but nonspecific.
Magnetic resonance imaging (MRI) is more sensitive than bone scintigraphy in detecting metastases. Pathologic fractures typically have a low-signal intensity on T1-weighted images and a high-signal intensity on T2-weighted images.
However, these same changes can also appear in benign lesions, such as acute osteoporotic compression fracture. Yuh et al found that complete loss of signal intensity in the bone
Fig. 6. A: Pre-contrast abdominal CT scan shows a low attenuated mass with amorphous calcification (arrow) in the left lobe of the liver and intrahepatic ductal dilatation. B: Post-contrast scan reveals mural nodular enhancement of the tumor (arrow).
A B
marrow on T1-weighted images provides a high level of accuracy in diagnosing malignant fractures [11]. The cervical MR images of our patient were characteristic of malignant fracture.
Cholangiocarcinoma
Cholangiocarcinomas are rare compared with hepatocellular carcinoma (HCC), comprising less than 10 percent of primary malignancies of the liver [12].
Cholangiocarcinomas are malignant tumors that arise from the epithelia of bile ducts, and are classified most practically as intrahepatic, perihilar, or distal. Their clinical features depend on the location of tumor, and often include obstructive jaundice, abdominal pain, abdominal mass and anorexia.
Cholangiocarcinomas have a slight male predominance and they typically occur in the fifth to seventh decades of life [12]. Known risk factors include primary sclerosing cholangitis, ulcerative colitis, choledochal cysts, biliary infection caused by Clonorchis sinensis (a liver fluke), stones and choledocholithiasis, and exposure to the radiologic contrast agent thorium dioxide (Thorotrast) [13]. Recently, some authors reported that infection with hepatitis C virus or HBV may be associated with the pathogenesis of intrahepatic cholangiocarcinoma [14,15].
There is an increase in CA 19-9 in over 80 percent of patients with cholangiocarcinoma [12].
Our patient had extremely high levels of CA19-9 and normal AFP. Overall, the history, risk factors, laboratory studies and the spinal pathology of our patient led us to suspect that the primary lesion originated in the biliary tract.
Computed tomography (CT) is critical for evaluating suspected cholangiocarcinoma, and magnetic resonance cholangiopancreatography (MRCP) has become a commonly employed noninvasive technique for imaging the biliary tree and tumor extent, which are important features in planning surgical reconstruction.
Hepatic resection is the best therapeutic option to treat cholangiocarcinoma while chemotherapy and radiation play an adjuvant role.
In the study by Takehiro Okabayahi, the median
survival time was 19.6 months [16], while other studies have shown that resection such as hepatic lobectomy planed in our case increases the survival rate by 1 to 3 years.
Rehabilitation of Patients with Spinal Cord Injury Caused by Metastatic Disease Spinal metastases develop in 5% to 10 % of patients with cancer [17]. Optional treatment protocols include radiation therapy, chemotherapy, surgical treatment and combined therapy. Increased emphasis on the maintenance of function and quality of active life for patients diagnosed with spinal metastases is paramount.
Several reports have documented functional improvement in these patients following comprehensive, multidisciplinary, physician-led rehabilitation programs [2,7,18]. Parsch et al confirmed these findings and stated that FIM score at admission to inpatient rehabilitation proved to be an even more reliable predictive variable of remaining survival time than tumor type or level of lesion [7]. The median survival time of their 68 patients was 11 months after the onset of neurologic deficits. Patients with poor FIM scores (< 65) demonstrated by fuzzy classification had shorter-term survival times (< 10 months) [7].
In conclusion, our patient presented with cholangiocarcinoma which had metastasized to the cervical spine. Her initial symptom was neck soreness. She recovered after the spinal operation, but remained tetraparesic; the FIM score was 50 (full score is 126) one week after operation. This case illustrates the importance of submitting all patients with neck pain to comprehensive research for an underlying cause.
R
REEFFEERREENNCCEESS
1. Kirshblum S, O'Dell MW, Ho C, et al. Rehabilitation of persons with central nervous system tumors.
[Review] Cancer 2001;92(4 Suppl):1029-38.
2. McKinley WO, Seel RT, Hardman JT. Nontraumatic spinal cord injury: incidence, epidemiology, and functional outcome. Arch Phys Med Rehabil 1999;80:
619-23.
3. Adamus RD, Victor M, Ropper AH. Disease of the spinal cord. In: Victor M, Ropper AH, eds. Adams and
Victors's Principle of Neurology. USA: McGraw-Hill, 2001:1330-2.
4. Hardeman SH, Collins B, Lowe VJ, et al.
Cholangiocarcinoma metastatic to the neck: first report of a case. Ear Nose Throat J 2002;81:776-8.
5. Yeh CN, Chen MF, Chen TC, et al. Peripheral cholangiocarcinoma with thoracic spine metastasis: a successful surgically treated case. Int Surg 2001;86:
225-8.
6. Carlisle RT, Roberts CS. Pathologic fracture of the humerus due to metastatic cholangiocarcinoma. South Med J 1999;92:1216-9.
7. Parsch D, Mikut R, Abel R. Postacute management of patients with spinal cord injury due to metastatic tumor disease: survival and efficacy of rehabilitation.
[Review] Spinal Cord 2003;41:205-10.
8. Dreghorn CR, Newman RL, Hardy GJ, et al. Primary tumors of the axial skeleton. Experience of the Leeds Regional Bone Tumor Registry. Spine 1990;15:137- 40.
9. Hahn SM. Oncology emergency. In: Goldman L, Bennett JC, eds. Cecil Textbook of Medicine. USA:
W.B. Sauders Company, 2000:1075.
10.Kamholtz R, Sze G. Current imaging in spinal metastatic disease. [Review] Semin Oncol 1991;18:
158-69.
11. Yuh WTC, Zachar CK, Barloon TJ, et al. Vertebral compression fractures: distinction between benign and
malignant causes with MR imaging. Radiology 1989;172:215-8.
12. Watkins KT, Curley SA. Liver and bile ducts. In:
Abeloff HD, Armitage JD, eds. Clinical Oncology.
USA: Churchill Livingstone, 2000:1722-3.
13. Sohn TA, Lillemoe KD. Tumors of the gallbladder, bile duct and ampulla. In: Fedman M, Friedman LS, eds. Sleisenger & Fordtran's Gastrointestinal and Liver Disease. Philadelphia: Saunders, 2002:1159-61.
14.Liu X, Zou S, Qiu F. Pathogenesis of hilar cholangiocarcinoma and infection of hepatitis virus.
Zhonghua Wai Ke Za Zhi 2002:40:420-2. (Chinese) 15. Donato F, Gelatti U, Tagger A, et al. Intrahepatic
cholangiocarcinoma and hepatitis C and B virus infection, alcohol intake, and hepatolithiasis: a case- control study in Italy. Cancer Causes Control 2001;12:
959-64.
16. Okabayashi T, Yamamoto J, Kosuge T, et al. A new staging system for mass-forming intrahepatic cholangiocarcinoma: analysis of preoperative and postoperative variables. Cancer 2001;92:2374-83.
17. Bilsky MH, Shannon FJ, Sheppard S, et al. Diagnosis and management of a metastastic tumor in the atlantoaxial spine. Spine 2002;27:1062-9.
18. McKinley WO, Conti-Wyneken AR, Vokac CW, at el.
Rehabilitation functional outcome of patients with neoplastic spinal cord compressions. Arch Phys Med Rehabil 1996;77:892-5.
1 2
1 2
40
, 2003;8:231-7
404 2
2003 7 28 2003 8 26
2003 10 17