Results of patients with PDA receiving surgical ligation—
Cases analyzed in different years and various kinds of hospital from the database of National Health Insurance
Yen-Hsiung Lin
ab, Li Lu
ac, Yu-Chuan Li
adGraduate Institute of Medical Informatics, Taipei Medical University
aDepartment of Pediatrics, Yu-Li Veterans Hospital
bVice Superintendent, Taipei Medical University Hospital
cVice Superintendent, Wan Fang Hospital
dyhs_lin@yahoo.com.tw
Abstract
The purpose of this report is to compare the results of surgical ligation of patent ductus arteriosus (PDA) in different years and various kinds of hospital.
The sources of data which are discussed and analyzed about surgical ligation of PDA are most from one or some medical centers up to now; however, these data cannot present the true event of a country. No any study about this issue, which source of data is from the database of National Health Insurance, which is a full data of medical record in a country or region and obtained via application for research, has been discussed and analyzed.
During a four-year period (1996~1999), 1708 patients receive surgical ligation of PDA from the database of National Health Insurance in Taiwan, 52 patients receive more than once of PDA ligation.
In this study, mean failure rate is 3.04%; the results also reveal that the annual failure rate and case numbers are declined year by year. It represents that our cardiovascular operative ability and neonatal intensive care level are advance gradually day by day.
Key words: surgical ligation, patent ductus arteriosus (PDA), failure rate, database of National Health Insurance
Introduction
Patent ductus arteriosus (PDA) is a heart defect that occurs when the ductus arteriosus does not close at birth.
The ductus arteriosus is a temporary fetal blood vessel
that connects the aorta and the pulmonary artery before birth. It should be present and open before birth when the fetus is developing in the uterus.
Since oxygen and nutrients are received from the placenta and the umbilical cord instead of the lungs, the ductus arteriosus allows blood to bypass the deflated lungs and go straight out to the body.
After birth, when the lungs need to add oxygen to the blood, the ductus arteriosus normally closes. The closure of the ductus arteriosus ensures that blood goes to the lungs to pick up oxygen before going out to the body.
Closure of the ductus arteriosus usually occurs at birth as levels of certain chemicals, called “prostaglandins”, change and the lungs fill with air. If the ductus arteriosus closes correctly, the blood pumped from the heart goes to the lungs, back into the heart, and then out to the body through the aorta. The blood returning from the lungs and moving out of the aorta carries oxygen to the cells of the body.
In some infants, the ductus arteriosus remains open and results in heart defect is known as PDA. In majority patients, a small PDA does not result in physical symptoms; however, if the PDA is huge, health complication problems may occur.
The patients with PDA present difficulty problems in management especially combined with premature infants, whether the treatment is medical or surgical.
The treatment and management of PDA depends on the size and symptoms being experienced by the affected
individual. In some patients, a PDA can be corrected itself in the first months of life. In the majority of premature infants experiencing symptoms, the first step in correcting a PDA is prescribed prostaglandin inhibitor, such as indomethacin. In premature infants whose PDA is unable to be close by medical management; however, for full term infants and adults, surgical ligation is an option for closing the ductus arteriosus. Recently, medicine has developed and reviewed alternatives to surgical closure such as interventional cardiac catheterization [7-8, 11, 16, 20-21]. A cardiologist can help individuals determine the best method for treatment based on their physical symptoms and medical history.
The sources of data which are discussed and analyzed about surgical ligation of PDA are most from one or some medical centers up to now; however, these data cannot present the true event of a country. No any study about this issue, whose source of data is from the database of National Health Insurance, which is a full data of medical record in a country or region and obtained via application for research, has been discussed and analyzed.
Literature Reviews
Although methods for treatment of PDA are various;
medical procedures, such as drugs administration [2, 5, 9-10, 13, 19] or catheter embolization [11, 16, 20] are generally precedent. However, surgical intervention for PDA closure is still envisaged while medical procedures are failed or contraindicated.
Many reports [2, 9, 13, 19] suggest that medical closure of PDA is not always successful, including reopening the PDA after drugs administration [12, 23], hemolysis happening or occlusion devices dropping in pulmonary artery after catheter embolization [3, 22].
On the other hand, many newer and safer surgical procedures are present, such as video-assisted thoracotomy (VAT) [15, 18], minimally invasive surgery [14], surgery in NICU [4, 6], and so on.
Nonetheless, failure of surgical ligation for PDA still occurs due to various reasons, such as insufficient facility of some hospitals, inexperienced ability of
neonatal care and cardiovascular surgery, etc.
Unfortunately, failure of surgical ligation of PDA also occurs in Taiwan, even the majority of these operations are performed in equal level of medical center and we have sufficient ability of neonatal care and cardiovascular surgery. We use the database of National Health Insurance to search and discuss the results about failure rate of surgical ligation for PDA.
Materials and Methods
In Taiwan, National Health Insurance is compulsive and general; most of the database of National Health Insurance is partial and selected, which cannot be used to compare each other. By exception, the medical records of major diseases are complete. Because all patients with PDA belong to one of major diseases, and the database of major diseases is full without any selection, we can use this database to analyze the results of surgical ligation of PDA in Taiwan.
In this study, failure for surgical ligation of PDA is defined that enrolled patients who receives more than once surgical ligation in this four-year period; under this condition, the failure rate will be countered to the first year and the first hospital.
In addition, patients who receive surgical ligation of PDA and stay at hospital more than one month due to major disease belongs to continuous admission, which may present more than once at the database of National Health Insurance; in this situation, surgery is successful.
Therefore, we collected and analyzed the data of surgical ligation of PDA from the database of National Health Insurance in different years and various kinds of hospital.
Results
During a four-year period (1996~1999), 1708 patients receive surgical ligation of PDA from the database of National Health insurance in Taiwan. 52 patients who receive more than once of PDA ligation are compatible with the definition of failed PDA surgery in this period;
the mean failure rate is 3.04%.
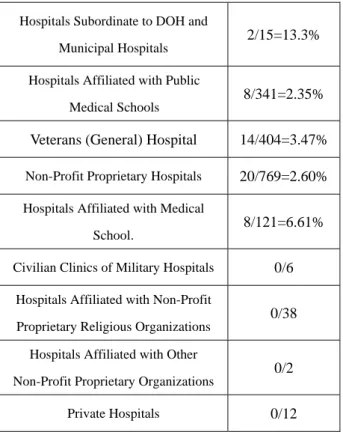
The failure rate of different years and various kinds of
hospital in this four-year period are also presented at table 1 and table 2, respectively. At table 2, no failure case of surgical ligation is noted in some kinds of hospital.
Table 1: The annual failure rate
#Denominator: All sample number - repeat sample number + actual failure case number
1996 20/378#(403-55+30)=5.29%
1997 13/416#(441-47+22)=3.12%
1998 10/406#(442-62+26)=2.46%
1999 9/508#(556-86+38)=1.77%
Table 2: The failure rate of various kinds of hospital
Hospitals Subordinate to DOH and
Municipal Hospitals 2/15=13.3%
Hospitals Affiliated with Public
Medical Schools 8/341=2.35%
Veterans (General) Hospital 14/404=3.47%
Non-Profit Proprietary Hospitals 20/769=2.60%
Hospitals Affiliated with Medical
School. 8/121=6.61%
Civilian Clinics of Military Hospitals 0/6 Hospitals Affiliated with Non-Profit
Proprietary Religious Organizations 0/38 Hospitals Affiliated with Other
Non-Profit Proprietary Organizations 0/2
Private Hospitals 0/12
Discussion
The mean failure rate of PDA ligation during this four-year period from the database of National Health Insurance is 3.05%, which is accordant to world-class level (4%~26%) [17, 20].
The case numbers of failed PDA ligation in this four-year period are decreased year by year (from 20 to 9);
furthermore, the failure rate of PDA ligation is also declined (from 5.29% to 1.77%). So, we think that the ability of cardiovascular surgery is more advance in Taiwan day by day.
On the other hand, most patients of receiving PDA ligation are premature infants, who are necessary to be cared by experienced neonatologist and intensive neonatal nursing care. The case numbers of receiving PDA ligation are gradually increasing during this four-year period (from 378 to 508), it also represents that our ability of neonatal intensive care is more advance than we were.
The failure rate of PDA ligation in municipal hospital is much higher than other kinds of hospital (13.3% vs.
2.35%~6.61%). We think that patients receiving PDA ligation in municipal hospital are much few than others (15 vs. 121~769), it might be due to insufficient facility or inexperienced ability of cardiovascular surgery and intensive neonatal care. The much few patients receiving PDA ligation might be the reason mentioned above, which might result in distorting failure rate.
We also find out that almost half (769/1708=45%) of the patients received PDA ligation in non-profit proprietary hospitals. This ratio is compatible with the distribution of using the majority resource of health insurance ligation in non-profit proprietary hospitals [1].
Future Foresight
Since the reasons of failed surgery for PDA ligation are various, including insufficient facility of hospital, inexperienced ability of cardiovascular surgery and neonatal intensive care, severity of disease itself, general condition of affected patients, and so on. Most of these reasons are not presented in the database of National Health Insurance in Taiwan due to confidentiality or technical problems. We cannot figure out the details of these reasons from the database of National Health Insurance in order to analyze and discuss the influence of these reasons.
In addition, current coding information about hospitals from the database of National Health Insurance has been modified, and it cannot present the result of single hospital. If the sufficient information of each hospital is able to be obtained from the database, we can further analyze the failure rate of each hospital and compare the
results of surgery in hospital itself with others.
For most patients who receive surgical ligation of PDA do not response to medical procedures, including catheter embolization, drugs administration (oral or intravenous), or contraindicated; in the future, we can also analyze and discuss the results of difference in medical procedures to surgical methods from the database of National Health Insurance.
Fortunately, the stage 2 and 3 of IC card for National Health Insurance which enrolls most private information, such as personal basic data and medical record, will be achieved in the near future. More and more useful information will be obtained and can be discussed and analyzed to conclude more useful results for medical institution and the publics in Taiwan.
Reference
1. 表 57 與 58, 特約醫事服務機構住院費用申報狀 況 — 按 權 屬 別 分 : 全 民 健 康 保 險 統 計 , http://www.nhi.gov.tw/01intro/intro_3.htm
2. Alpert BS, Lewins MJ, Rowland DW, et al (1979),
“Plasma indomethacin levels in preterm newborn infants with symptomatic patent ductus arteriosus”, J Pediatr, 95(4), pp578-582.
3. Chisholm JC, Salmon AP, Keeton BR (1995),
“Persistent hemolysis after transcatheter occlusion of a patent ductus arteriosus: surgical ligation of the duct over the occlusion device”, Pediatr Cardiol, 16(4), pp194-196.
4. Eggert LD, Jung AJ, MCGough EC (1982), “Surgical treatment of patent ductus arteriosus in preterm infants.
Four-year experience with ligation in the newborn intensive care unit”, Pediatr Cardiol, 2(1), pp15-18.
5. Friedman WF, Kirskcklau MJ, Printz MP, Pitlick PT, Kirkpatrick SE (1976), “Pharmacologic closure of patent ductus arteriosus in the premature infants”, N Engl J Med, 295(10), pp526-529.
6. Gould DS, Montenegro LM, Gaynor JW (2003), “A comparison of on-site and off-site patent ductus arteriosus ligation in premature infants”, Pediatrics, 112(6 Pt 1), pp1298-1301.
7. Gray DT, Fyler DC, Walker AM (1993), “Clinical outcomes and costs of transcatheter as compared with surgical closure of patent ductus arteriosus. The Patient Ductus Arteriosus Closure Comparative Study Group”, N Engl J Med, 329(21), pp1517-1523.
8. Gray DT, Weinstein MC (1998), “Decision and cost-utility analyses of surgical versus transcatheter closure of patent ductus arteriosus: should you let a smile be your umbrella?”, Med Decis Making, 18(2), pp187-201.
9. Halliday HL, Hirata T, Brady JP (1979), “Indomethacin therapy for large patent ductus arteriosus in the very low birth weight infant: Results and complications”, Pediatrics, 64(2), pp154-159.
10. Heymann MA, Rudolph AM, Sliverman NH (1976),
“Closure of the ductus arteriosus in premature infants by inhibition of prostaglandin synthesis”, N Engl J Med, 295(10), pp530-533.
11. Hwang B, Lee PC, Weng ZC (2000), “Comparison of the one-and-a-half-year results of closure of patent ductus arteriosus by transcatheter coils placement with surgical ligation”, Angiology, 51(9), pp757-563.
12. Itabashi K, Ohno T, Nishida H (2003), “Indomethacin responsiveness of patent ductus arteriosus and renal abnormalities in preterm infants treated with indomethacin”, J Pediatr, 143(2), pp203-207.
13. Ivey HH, Kattwinkel J, Park TS, Krovetz LJ (1979),
“Failure of indomethacin to close persistent ductus arteriosus in infants weighing under 1,000 grams”, Br Heart J, 41(3), pp304-307.
14. Iwase J, Tajima K, Io A (2003), “Less invasive surgical closure of patent ductus arteriosus in extremely low birth weight infants”, Jpn J Thorac Cardiovasc Surg, 51(12), pp651-655.
15. Jacobs JP, Giroud JM, Quintessenza JA (2003), “The modern approach to patent ductus arteriosus treatment:
complementary roles of video-assisted thoracoscopic surgery and interventional cardiology coil occlusion”, Ann Thorac Surg, 76(5), 1421-1427; discussion
1427-1428.
16. Latson LA, Hofschire PJ, Kugler JD (1989),
“Transcatheter closure of patent ductus arteriosus in pediatric patients”, J Pediatr, 115(4), pp549-553.
17. LeBlanc JG, Russell JL, Sett SS (2000), “The evolution of ductus arteriosus treatment”, Int Surg, 85(1), 1-5.
18. Mavroudis C, Backer CL, Gevitz M (1994),
“Forty-six years of patient ductus arteriosus division at Children's Memorial Hospital of Chicago.
Standards for comparison”, Ann Surg, 220(3), pp402-409; discussion 409-410. Review.
19. Neal WA, Kyle JM, Mullett MD (1977), “Failure of indomethacin therapy to induce closure of patent ductus arteriosus in premature infants with respiratory distress syndrome”, J Pediatr, 91(4), pp621-623.
20. Podnar T, Masura J. (1999), “Transcatheter occlusion of residual patent ductus arteriosus after surgical ligation”, Pediatr Cardiol, 20(2), pp126-130.
21. Prieto LR, DeCamillo DM, Konrad DJ (1998),
“Comparison of cost and clinical outcome between transcatheter coil occlusion and surgical closure of isolated patent ductus arteriosus”, Pediatrics, 101(6), pp1020-1024.
22. Rao PS, Kim SH, Choi JY (1999), “Follow-up results of transvenous occlusion of patent ductus arteriosus with the buttoned device”, J Am Coll Cardiol, 33(3), pp820-826.
23. Rhodes PG, Ferguson MG, Reddy NS (1988),
“Effects of prolonged versus acute indomethacin therapy in very low birth-weight infants with patent ductus arteriosus”, Eur J Pediatr, 147(5), pp481-484.