行政院國家科學委員會專題研究計畫 成果報告
四十歲以上的心房中隔缺損病人心導管關閉與開刀兩種治
療方法追蹤結果之比較
計畫類別: 個別型計畫 計畫編號: NSC93-2314-B-002-132- 執行期間: 93 年 08 月 01 日至 94 年 07 月 31 日 執行單位: 國立臺灣大學醫學院小兒科 計畫主持人: 王主科 共同主持人: 許寬立 報告類型: 精簡報告 報告附件: 出席國際會議研究心得報告及發表論文 處理方式: 本計畫可公開查詢中 華 民 國 94 年 11 月 18 日
四十歲以上的心房中隔缺損病人心導管關閉與
開刀兩種治療方法追蹤結果之比較
王主科台大醫院小兒部
NSC 93-2314-B-002-132
執行期限:93 年 8 月 1 日至 94 年 7 月 31 日
一、中文摘要
目的:
探討「心導管關閉心房中隔
缺損」的技術治療 40 歲以上的病
人是否安全,成效如何,並與同
年齡層病人之開刀結果做比較
方法與結果:
1.方法:
這是個回溯性研究,過去七
年當中(1998 至 2005 年) 40 歲以
上的心房中隔缺損病人在本院接
受心導管治療共 86 人,(40 歲至
81 歲,中位數 51 歲),另一組為
同年齡層心房中隔缺損病人在過
去十年間,排除合併其他心臟疾
病者,(1996 至 2005 年)在本院
接受開刀者共 49 人,年齡由 41
歲至 72 歲不等,比較兩組間成功
率及併發症比率之差異。
2.結果:
(1)以心導管治療的病人 86 例病
人當中,83 人有右心室擴大,84
人有心臟症狀,11 人有心律不
整,Qp/Qs 值平均為 3 ± 0.9,有
吸率不整的人年紀明顯較老(64
± 9 vs. 52 ± 7, p ‹0.01) 缺損
平均值徑為 23 ± 6.8 mm (11 至
35 mm 不等),13 人有多孔型缺
損,50 人有肺動脈高血壓 (肺動
脈平均壓 ≧ mm 20 Hg),86 人
缺損皆可用心導管關閉,84 人使
用 Amplatzer septal
occluder,1 人使用 CardioSeal,
另一人使用 Buttoned device,
有 6 人使用穿孔型關閉器
(fenestrated device),因為這
6 個人有明顯的心臟衰竭。有一
人有併發症發生心包膜充填,需
要抽出新包膜液,其餘無明顯併
發症,術後每日服用 aspirin
200mg 共 6 個月。
追蹤期間平均為 2.9 ± 1.4
年,症狀改善者有 85 人,僅有 1
人沒改善,沒有新發生的中風,4
人仍有極小滲漏,追蹤期間仍有
肺動脈壓升高者有 1 位,術前有
心律不整 11 人中,5 人仍有心律
不整。另有 2 人術後發生短暫性
的心房顫抖(atrial
fibrillation) ,住院日平均為
3 天。
(2)心導管與開刀比較
這十年當中 40 歲以上心房中
隔缺損接受開刀者共有 49 人,手
術無人死亡,但有 11 人術後發生
心包膜充填(1/86 vs. 11/49, P‹
0.01)49 人術前有 8 人有心律不
整,術後有顯著心律不整病人共
有 14 人。
結論:
經由心導管治四十歲以上
的心房中隔缺損是個相當安全
而有效的方式,與開刀的結果
相比繳,併發症較少
關鍵詞:
Adult,Atrial septal defect, transcatheter closure,Amplatzer septal occluder
Abstract:
To present the short-and mid-term results of transcatheter closure of atrial septal defect (ASD) in patients older than 40 years.
Between January 1998 and September 2005, transcatheter closure of ASD was attempted in 86 patients (18 males) above 40 years of age (aged ranging from 40 to 81 years, median 51). All except 2 patients were symptomatic. Deployment of device was performed under general anesthesia and transesophageal echocardiographic monitoring. The results of transcatheter closure were compared with those of surgery in the past 10 years.
Of the 86 patients, Enlargement of right ventricle was documented on the echocardiography in 83. Atrial arrhythmia was present in 11 patients. Patients with atrial arrhythmia was significantly older than those without. (64 ± 9 vs. 52 ± 7 years, P < 0.01) The
mean Qp/Qs ratio was 3.11 ± 0.99
(ranging from 1.5 to 6.4). The mean stretched diameter of the defect was 23 ± 6.8 mm. (ranging from 11 to 35 mm) Thirteen patients had multiple defects. Pulmonary hypertension was present in 50 patients. The procedure was successful in all 86 patients. Amplatzer septal occluder (ASO) was used in 84
patients, CardioSeal device in 1 and Buttoned device in remaining 1. Six underwent ASD closure with a fenestrated device because of presence of significant heart failure. Five underwent implantation using 2 ASO devices. During the procedure, 2 experienced supraventricular tachycardia which was treated with cardioversion. One complicated with tamponade requiring drainage. One had a distal embolism to a finger tip 2 days after the procedure. The mean follow-up period is 2.9 ± 1.4 years. Four had
small residual shunt in the latest follow-up of whom 2 had multiple defects. Pulmonary hypertension and right ventricular enlargement persisted in 1 and 4 patients respectively, in the latest echocardiographic follow-up. Symptomatic improvement was documented in all except 1. Of the 11 patients with atrial arrhythmias, 6 patients recovered to sinus rhythm and 5 had persisted atrial arrhythmias in the latest follow-up. Two had new onset atrial arrhythmia 3-months following the procedure. In the past 10 years, surgery for ASD was performed in 49 patients. Eleven of them developed post-operative pericardial effusion. (1/86 vs. 11/49, P ‹0.001 ). Eight patients had
Transcatheter closure of ASD in patients above 40 years of age is safe and effective where patients may benefit from the procedure. Surgery carries a higher risk of postoperative pericardial effusion than transcatheter closure.
Abbreviations:
Atrial septal defect (ASD)
Transesophageal echocardiography (TEE)
Key words:
Adults, atrial septal defect, transcatheter closure, Amplatzer septal occluder
二、緣由與目的 Introduction:
Atrial septal defect (ASD) which accounts for 6 to 10 % of congenital heart disease, is the most common congenital heart disease diagnosed in adulthood. There were debates regarding the benefit of ASD closure in patients older than 40 years, since atrial arrhythmia may persist despite surgical closure of the defect. Recently, transcatheter closure of secundum-type ASD has gain wide acceptance as an alternative to surgery. Transcatheter closure is believed to be less traumatic to cardiac structure and the incidence of atrial arrhythmia following transcatheter closure could therefore be less than that after surgery. We conducted this study to investigate short and mid term results of transcatheter closure of ASD in patients above 40 years of age. The results were compared with those of secundum type
ASD patients who underwent open heart surgery with ages above 40 years in the past 10 years.
Methods:
Patients and Methods:
This is a retrospective study. Data were collected by reviewing medical records. During a 7.8-year period (between January 1998 and September 2005), a total of 86 patients (23 males) who underwent attempted transcatheter closure of ASD in this institutions were above 40 years of age. Of the 86 patients, their ages ranged from 40 to 81 years. (median 51 years). Three patients had a past history of cerebreval vascular accident. One had underwent surgery for ASD complicated with dehisence of a patch and a large residual shunt. Three underwent coronary stent implantation prior to attempted ASD closure. Seventy-nine patients had cardiac symptoms including palpitation, dyspnea, exercise intolerance or chest pain. Nineteen patients had significant atrial arrhythmia and 6 experienced supraventricular tachycardia requiring anti-arrhythmic treatment. One patient had severe heart failure and pneumonia requiring prolonged respiratory support.
A routine ECG and precordial echocardiography were performed on admission. A consent was obtained prior to cardiac catheterization. Under local
anesthesia, femoral artery and vein were connulated. A hemodynamic study was routinely performed. The Qp/ Qs ratio was calculated. An angiogram at right upper pulmonary vein was performed to delineate the morphology of ASD and to exclude the presence of an anomalous pulmonary venous drainage. Selective coronary artery angiography was performed in patients who were suspected to have coronary artery lesions on an aortogram. Then general anesthesia was instituted. Transesophaged echocardiography (TEE) was used to image the morphology of ASD and monitor the implantation procedure. Forty-five patients underwent balloon sizing. After July 2004, balloon sizing was not routinely performed. There were 43 patients underwent closure without balloon sizing. Sizing of the defect was performed using a balloon catheter (Meditec or AGA). The stretched diameter was measured on a digitalized cineangiography. The methods of sizing are similar to those described in literature. A sizing plate was also used to confirm the measurement from the cineaugiography. The rims around the defects were measured on TEE images. The distances from the rim of the defect to pulmonary veins, coronary sinus and mitral valve should be > 5 mm. Of the 86 patients,
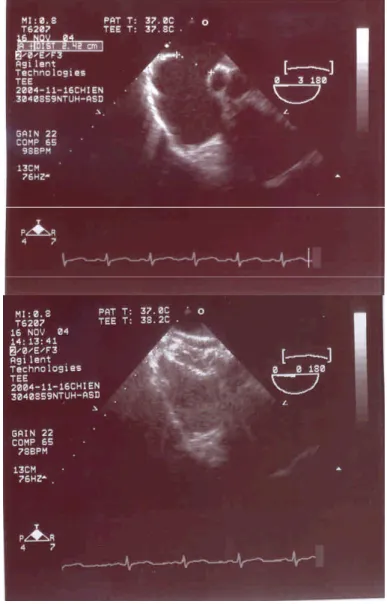
Amplatzer septal occluder was used in 84, CardioSeal in 1 and Buttered device in the remaining 1. (Figure 1)
The size of the Amplatzer septal occluder selected was within 2 mm of the stretched diameter. For those without balloon sizing, the device selected was 4-6 mm and 7-10 mm larger than maximal diameter of ASD on TEE images if the maximal diameter of the defect ‹14 mm and ›14 mm respectively.
The technique of deployment of the device was similar to those reported in literature. Before releasing the device from the delivery cable, TEE were used to assess the position of the device, mitral valve function and presence of residual shunt. Following the implantation procedure, patients were sent to intensive care unit or recovery room to monitor vistal signs for a few hours. Another 3 doses of antibiotics were given. A physical examination, ECG, chest radiography and echocardiography were performed on the next day. Aspirin 3-5 mg/kg per day was given for 6 months. Echocardiography was performed at 1 month, 3 months, 6 months, 12 months & yearly, thereafter. Clinical assessment was performed after echocardiography in each patient. A holter monitor was performed after 2-6 months after the
procedure if appliable. The results of surgery in ASD patients above 40 years of ages in the past 10 years were compared with those of transcatheter treatment.
三、結果 Results:
Sustained superaventricular tachyarrhythmia was documented in 6 patients prior to intervention. Eleven patients had atrial arrhythmia. Patents with atrial arrhythmia was significantly older than those without. ( 64 ± 9 vs.
52 ± 7 years, P ‹ 0.01 ) Right
ventricular dilation was documented on the echocardiography in 83 patients. The mean Qp/Qs ratio was 3.11 ± 0.99
(ranging from 1.5 to 6.4). Thirteen patients had multi-perforated defects. Eight patients had an atrial septal aneurysm. Fifty patients had elevated pulmonary artery pressure (mean pulmonary artery pressure ≧ 20 mmHg). In the 45 patients undergoing balloon sizing, the mean stretched diameter of the defect was 23 ± 6.8 mm
(ranging from 11 mm to 35.7 mm). Amplatzer septal occluder was were used in 43. The mean diameter of the device was 25 ± 7.8 mm. In the
remaining 43 patients without balloon sizing, the mean maximal diameter of the defect on the TEE images was 20.3
± 6.3 mm. The mean diameter of device used was 26.2 ± 7.8 mm. Transcatheter
closure of ASD was successfully performed in all 86 patients. Amplatzer septal occluder (ASO) was used in 84, Cardioseal device in 1 and Buttoned device in the remaining 1 patient. Five had implantation of 2 ASO devices. A fenestrated device was deployed in 6 patients with significant heart failure. One had atrial flutter and severe heart failure who underwent DC shock before intervention. The mean right atrial pressure decreased from 21 to 12 mmHg following deployment of a fenestrated device.
In the past 10 years, surgery of ASD was performed in 123 patients of which 49 patients were above 40 years of ages. There was no mortality among the 49 patients. Comparison of results between transcatheter closure and surgery there was no significant difference.
Supraventricular tachycardia occurred in 4 during the procedure which was managed by injection of adenosine. One complicated with tramponade which was caused by inadvertent perforation of left upper pulmonary vein during positioning of a guide wire. Pericardiocentesis was performed without any sequalae. One with frequent ventricular ectopics had a
distal embolism to a finger tip 2 days after the procedure.
Discussion:
There are several advantages of transcatheter closure of ASD over surgery including avoidance of scar and cardiopulmonary by pas. A varieties of devices have been used to close the ASD, among which ASO is the most popular device used. There were many reports on the favorable results of ASD closure using ASO. However, the reports of transcatheter closure in adults or older patients were seldom. One recent study confirmed the improvement in exercise tolerance following ASD closure in patients. older than 40 years. This study showed that transcatheter closure is quite effective and safe for this age group patients given the low complication rate. Arrhythmia is frequently observed in patients prior to closure which could persist after surgery. New arrhythmia was not rare after surgery for ASD in adults. In this study, significant atrial arrhythmia was documented on routine ECG in 11/84 which subsided after transcatheter closure in 4, but persisted in the remaining 4. New-onset atrial arrhythmia was documented in 4. This implied that transcatheter closure of ASD in patients > 40 years did not
guarantee prevention of arrhythmia. Arrhythmia may persist after ASD closure. However, comparing the results between transcatheter closure and surgery, the incidence of new-onset arrhythmia seems higher in patients undergoing surgery.
Although surgery is considered as a safe procedure in the treatment of ASD, the complication rate is not rare in whom pericardial effusion is the most common. Impaired right ventricular function is also observed following surgery. Taking the hospitalization time, scar. And the need for cardiopulmonary bypass into consideration, transcatheter closure could be superior to surgery, particularly in those above 40 year of ages who may have associated pulmonary hypertension or diabetes.
Arrhythmia in ASD is considered to be originated from right atrial dilation. Normalization of right heart dimension is generally observed within a few weeks following ASD closure in children, but it may take more than 12 months in adults. This could imply that normalization of right heart dimension after ASD closure in older adult may take a longer time that arrhythmia could persist for months. The mechanism of developing new onset arrhythmia is not clear. Changes in right heart geometry
and electric activity following ASD closure could play a role.
It is concluded that transcatheter closure is feasible and safe in patients above 40 years. The complication rate is less in transcatheter closure than in surgery.
Acknowlegement:
This study was supported by a grant from national science council, Taiwan. NSC 93-2314-B002-132
Figure Legend:
Figure1. A defect measure 24 mm an TEE images. A 34 mm device was deployed with success.
Figure2. Atrial flutter/ fibrillation occurred 9 months after ASD closure with the Amplatzer septal occluder in a 66-year-old male patients.
Reference:
1. Jemielity M, Dyszkiewicz W, Paluszkiewicz L, Perek B, P Buczkowski, A Ponizynski. Do patients over 40 years of age benefit from surgical closure of atrial septal defects? Heart 2001;85:300-03.
2. Fiore AC, Naunheim KS, Kessler KA, Pennington DG, McBride LR, Barner HB, Kaiser GC, Willman V. Surgical closure of atrial septal defect in patients older than 50 years of age. Arch Surg 1988;123(8):965-7.
3. Dave KS, Pakrashi BC, Woolder GH, et al. Atrial septal defect in adults: clinical and hemodynamic results of surgery. Am J Cardiol 1973;31:7-14. 4.Konstantinides S, Geibel A, Kasper w, et al. The natural course of atrial septal defect in adults-a still unsettled issue. Klin Wochenschr 1991;69:506-10. 5. Konstantinides S, Geibel A, Olsckewski M, et al. A comparison of surgical and medical therapy for atrial septal defect in adults. N Engl J Med 1995;333:469-73.
6. Murphy JG, Gersh BJ, McGoon MD, et al. Long term outcome after surgical repair of isolated atrial septal defects. Follow-up at 27 to 32 years. N Engl J Med1990;323:1645-50.
7. Cheng TO. The natural course of atrial septal defect in adults-a still unsettled issue. Clin Invest 1992;70:85.
8. Ward C. Secundum atrial septal defect: routine surgical treatment is not of proven benefit. Br Heart J 1994;71:219-23.
9. Perloff JK. Surgical closure of atrial septal defect in adults. N Engl J Med 1995;333:513-14.
10. Gault JH, Morrow AG, Gay WA, et al. Atrial septal defect in patients over the age of forty years. Circulation 1968;37:261-71.
11. Knight M, Lenox S. Results of surgery for atrial septal defect in patients of 40 years and over. Thorax 1972;27:577-82.
12. Gatzoulis MA, Freeman MA, Siu SC, Webb GD, Harris L. Atrial arrhythmia after surgical closure of atrial septal defects in adults. N Engl J Med 1999;340:839-46. 13. Berger F, Vogel M, Kramer A, et al. Incidence of atrial flutter / fibrillation in adults with atrial septal defect before and after surgery. Ann Thorac Surg 1999;68:75-8.