Title:
Increased Risk of Cardiovascular Events in Patients with
Herpes Zoster: A Population-Based Study
Short title
:Herpes Zoster and CVDPo-yuan Wu1,2,3, Cheng-Li Lin3,4 , Fung-Chang Sung3,4, Tzu-Chieh Chou 3,5*, Yuan-Teh Lee 6,7
1 Department of Dermatology, China Medical University Hospital, Taichung 404,
Taiwan
2 School of Medicine, China Medical University, Taichung 404, Taiwan
3 Department of Public Health, China Medical University, Taichung 404, Taiwan
4 Management Office for Health Data, China Medical University Hospital, Taichung
404, Taiwan
5 Department of Health Risk Management, College Management, China Medical
University, Taichung 404, Taiwan
6 Division of Cardiology, China Medical University Hospital, Taichung 404, Taiwan
7 Division of Cardiology, National Taiwan University Hospital, Taipei 100, Taiwan
Conflict of interest. All authors: No reported conflicts. * Corresponding author:
Tzu-Chieh Chou, PhD, MPH Associated Professor
China Medical University Department of Public Health 91 Hsueh Shih Road
Taichung 404, Taiwan Tel: 886-4-22053366-6120 Fax: 886-4-2201-9901
E-mail: choutc@mail.cmu.edu.tw
Funding source: The present study was supported by the National Sciences Council,
Executive Yuan (grant number NSC 100-2621-M-039-001), China Medical University (Grant Number CMU98-s-28, CMU-TC-38 and 1MS1), and Taiwan’s Department of Health (Grant Numbers B-111-004 and DOH101-TD-C111-005).
Words count: 262 in Abstract, 2125 in Text, 4 Tables, 26 references, 1 Supplemental Table
ABSTRACT
Objective Association between herpes zoster and cardiovascular complications
remains vague with limited study on the association between these two disorders. This study evaluated the risk of cardiovascular diseases in patients with the varicella-zoster virus reactivates later as herpes zoster
Methods From insurance claims data of Taiwan, 19,483 patients with herpes zoster
diagnosed in 1998-2008 and 77,932 subjects without herpes zoster have been identified in this study. Both cohorts were followed up until the end of 2010 to measure the incidence of arrhythmia and coronary artery disease. The herpes zoster cohort to non-herpes zoster cohort incidence rate ratio and adjusted hazard ratio (HR) of the
cardiovascular complications with 95% confidence interval (CI) were estimated.
Results The incidence of arrhythmia was 1.17-fold greater in the herpes zoster cohort
than in the non-herpes zoster cohort (13.2 vs. 11.3 per 1,000 person-years), with an adjusted HR of 1.16 (p < 0.01). The coronary artery disease incidence in the herpes zoster cohort was 1.16-fold higher than that in the non-herpes zoster cohort (9.02 vs. 7.83 per 1,000 person-years), with an adjusted HR of 1.11 (p < 0.01). Over the
stratified follow-up years, adjusted HRs were 1.22 (95% CI = 1.12-1.34) for arrhythmia and 1.14 (95% CI = 1.02-1.28) for coronary artery disease within two years after herpes zoster diagnosis. The risk measured for these disorders declined over time.
Comorbidities of hypertension, diabetes, and hyperlipidemia also contributed to these cardiovascular disorders with greater extent.
Conclusion The contribution of herpes zoster to the risk of arrhythmia and
cardiovascular diseases is less strong than that of hypertension, diabetes, and hyperlipidemia.
Keywords: Arrhythmia, Coronary artery disease, Herpes zoster, Retrospective cohort
Introduction
Heart diseases have become the most common causes of death worldwide, particularly in the industrial nations. In 2008, cardiovascular diseases accounted for 32.8% (811,940) of all deaths in the United States, and coronary artery disease (coronary artery disease) is responsible for half of these deaths. Hypertension, diabetes, smoking, dyslipidemia, family history, homocysteine, inflammation,
physical inactivity, obesity, stress, mood, and personality type are well known factors associated with the risks of coronary artery disease. Arrhythmia is an abnormality of the heart’s electrical impulses. More than 4 million US people experience
symptomatic or even life-threatening cardiac arrhythmia. Coronary artery disease, cardiomyopathy and valvular heart disease, diabetes, thyroid abnormality, and electrolyte imbalance are disorders associated with the risk of arrhythmia. Both coronary artery disease and arrhythmia are etiologies of sudden cardiac deaths.
Studies have investigated the linkage between viral infections and heart diseases. Alphaherpesvirinae infection may lead to atherosclerosis by altering the pathway of smooth muscle cell lipid metabolism in animal model . Epidemiology studies have shown that herpes simplex infection increase atrial fibrillation risk and HIV patient has high risk of acute myocardium .
Herpes zoster is a latent neurotrophic viral disease caused by varicella-zoster virus, after its primary infection. It is a visible marker associated with the risk of occult malignancy, immunosenescence, and immunocompromise status, especially HIV infection . Herpes zoster causes post-herpetic neuralgia and release inflammatory signals . Chronic inflammation on the endothelium cells of vascular walls may lead to atherosclerosis and cause cardiovascular diseases. Several case studies have reported the vague association between herpes zoster and cardiovascular complications,
including pleuropericarditis and complete heart block . However, no well-designed study has explored the association between these two disorders using population data. Therefore, the present study aims to use population-based insurance claims data to investigate whether patients with herpes zoster are at an elevated risk of arrhythmia and coronary artery disease.
Materials and methods Data sources
A claims database of Taiwan National Health Insurance (NHI), obtained from the National Health Research Institutes (NHRI) was used in this study. NHI, a single-payer health insurance program, was reformed in 1995 by the Department of Health from 13 insurance systems as a universal insurance system. This insurance program covers approximately 99% of the total of 23.74 million people in Taiwan . In
cooperation with the Bureau of National Health Insurance (BNHI), NHRI established several data sets for public use. This study used a represented data set with a cohort of 1,000,000 people randomly sampled from all insured people with claims from 1996 to 2010. Considering that all personal identifications have been encrypted before the release of the database to protect patient privacy, this study was exempted from full ethical reviews. The criteria of the diseases were defined according to the
International Classifications of Disease, 9th Revision, Clinical Modification (ICD-9-CM).
Study subjects
Patients aged 20 years and older, who were newly diagnosed from 1998 to 2008 with herpes zoster (ICD-9-CM 0.53x), were identified as the study cohort. For each herpes zoster case, four persons were selected at random without medical claims for
herpes zoster care, with frequencies matching by their ages (every five-year span), sex, and years of diagnosis. The patients diagnosed at the baseline with arrhythmia (ICD-9-CM codes 427.0 to 427.9; 758.0 or 758.1), coronary artery disease (codes 410 to 414), heart failure disease (codes 428), and stroke (codes 430 to 438) were
excluded from the study.
Outcome measures
The herpes zoster and the non-herpes zoster cohorts were followed up until the diseases appeared or censored because of failure to follow-up, death, or the end of 2010 to measure the incidence of arrhythmia and coronary artery disease. Patients with the history of diabetes (ICD-9-CM codes 250), hypertension (codes 401-405), and hyperlipidemia (codes 272) identified at the baseline were considered as comorbidities.
Statistical analysis
The data analyses first compared the distributions of age, sex, and baseline co-morbidities between the two cohorts. Categorical variables were examined by
Chi-square test, and continuous variables were examined by t -test. Then events of
arrhythmia and coronary artery disease for each cohort were identified. The follow-up time in person-years estimated the incident density rates and the herpes zoster cohort to non-herpes zoster cohort incidence rate ratio (IRR) with 95% confidence interval (CI). Cox proportional hazards regression model was used to assess the hazard ratio (HR) and 95% CI for each disease. The incidence rates of arrhythmia and coronary artery disease were also estimated by comorbidity, and their risks were compared in association with a specific comorbidity. Furthermore, the risk changed over time by
stratifying the follow-up period into four segments (< 2, 2 to 5, 5 to 8, and > 8 years) were evaluated. Both the IRR and HR were measured for the comparison of the herpes zoster cohort with the non-herpes zoster cohort. All analyses were performed using SAS version 9.1 (SAS Institute Inc., Cary, NC, USA). All statistical tests were two-sided, and the p-value < 0.05 was considered statistically significant.
Results
Study cohorts and incidence of cardiovascular events
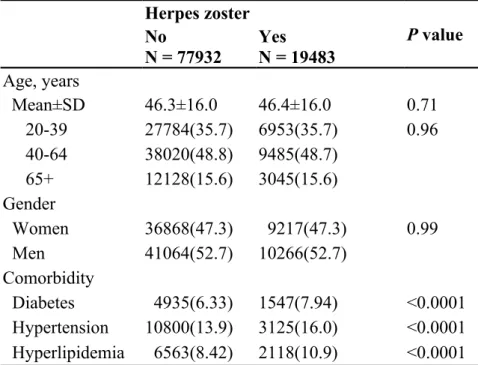
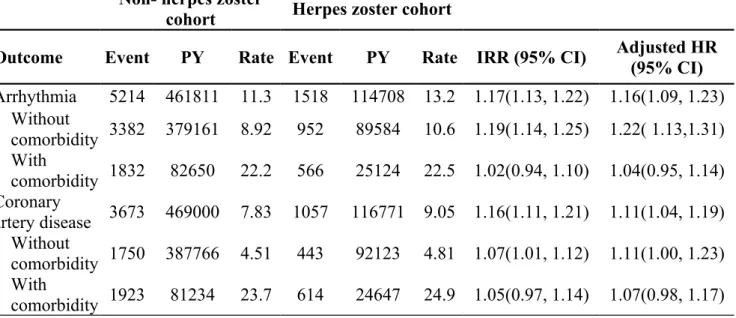
The present study identified 19,483 patients in the herpes zoster cohort and 77,932 persons in the non-herpes zoster cohort, with a mean age of 46.4 (SD = 16.0) years and 52.7% men in both cohorts (Table 1). The incidence of arrhythmia was 1.17-fold greater in the herpes zoster cohort than that in the non- herpes zoster cohort (13.2 vs. 11.3 per 1,000 person-years), with an adjusted HR of 1.16 (95% CI = 1.09 to 1.23) (Table 2). The incidence of coronary artery disease was also 1.16-fold higher in the herpes zoster cohort than that in the non-herpes zoster cohort (9.05 vs. 7.83 per 1,000 person-years), with an adjusted HR of 1.11 (95% CI = 1.04 to 1.19). At the baseline, the herpes zoster cohort was more prevalent with diabetes, hypertension, and
hyperlipidemia than the non-herpes zoster cohort (p < 0.0001, Table 1). For those free of the specific comorbidity, the incidence of the herpes zoster cohort was significantly higher than that of non-herpes zoster cohort (HR 1.22 and 1.11 in arrhythmia and coronary artery disease, respectively, Table 2).
Comorbidity associations and risk over follow-up period
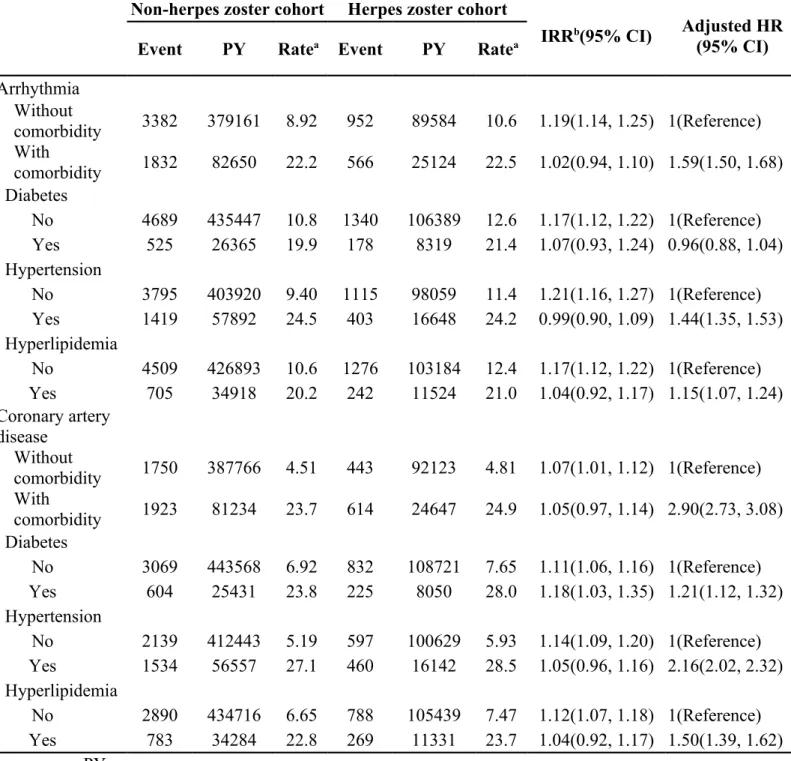
Table 3 shows that the incidence of arrhythmia and coronary artery disease increased with the existence of the selected comorbidities in both cohorts. The
differences in incidence increases associated with the existence of comorbidities were not significant between the two cohorts; incidence rates of arrhythmia and coronary artery disease associated with comorbidities were higher than associated with herpes zoster. However, Cox model measured adjusted HR associated with the comorbidity was generally significant for the herpes zoster cohort, compared with the non-herpes zoster cohort. The HR of coronary artery disease was 2.90 (95%CI=2.73-3.08) in those with comorbidities, and the greatest in those with hypertension (2.16, 95% CI=2.02–2.32).
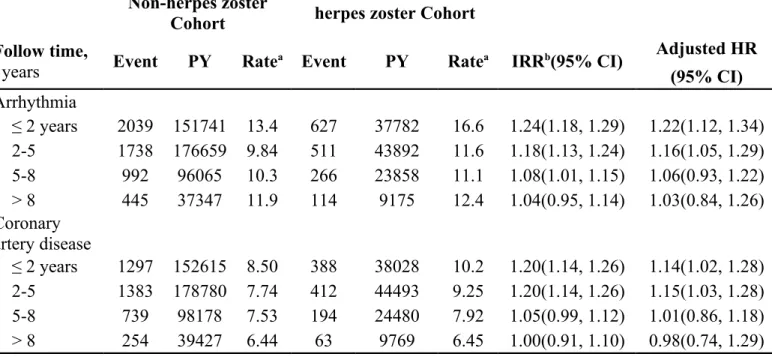
Table 4 shows the trend of adjusted HRs of arrhythmia and coronary artery disease for the herpes zoster cohort compared with the non-herpes zoster cohort in the follow-up period. The adjusted HR of arrhythmia declined from 1.22 in the first 2-year follow-up to 1.03 after 7-year. The adjusted HR of coronary artery disease declined from 1.14 to 0.98, correspondingly.
Discussion
Inflammatory process is a well-established pathogeneses in exacerbating
atherosclerosis . C-reactive protein (CRP) is a marker of inflammation and plays an important prognostic role in the risk of coronary artery disease for patients . Some viruses such as CMV, HAV and HSV have been associated with coronary artery disease in cross-sectional and prospective studies . Clinically, the first case study on the association between herpes zoster and cardiovascular disease (angina pectoris) was reported in 1939 . Sporadic occurrences of chickenpox-related cardiovascular events in children and young adults have been reported recently, including pericarditis , myocarditis and myoepicarditis , cardiac tamponade, and pericardial effusion . The cardiovascular complications of herpes zoster have also been reported as varicella
zoster myoepicarditis in a previously healthy young man , complete heart block in a 64-year-old white male and myocardium infarction symptom that finally diagnosed as myocarditis in a sixteen-year-old male . However, there has been no population-based epidemiology study on the association between varicella-zoster virus and heart disease.
The present study used a representative population sample and found that patients with the history of herpes zoster were at higher risk of arrhythmia and coronary artery disease. Our study showed that diabetes, hypertension, and hyperlipidemia remain as prominent risk factors of arrhythmia and coronary artery disease in both the herpes zoster and non-herpes zoster cohorts. After adjusting for the factors, such as age and sex, the HRs of arrhythmia and coronary artery disease are 1.22 and 1.14,
respectively. The highest risk appeared within five years after the virus was
reactivated as herpes zoster. This study is the first epidemiologic study that reveals the association between herpes zoster and cardiovascular complications. Our further data analysis showed that, among those who had developed arrhythmia, the incidence of coronary artery disease increased dramatically to 69.3 per 1,000 person-years in the herpes zoster cohort and 64.9 per 1,000 person-years in the non-herpes zoster cohort (Supplemental Table 1). In contrast, the risks associated with stroke were much less. A number of possible explanations link herpes zoster to coronary artery disease. Biasucci et al. found the elevated levels of IL-6, the main inductor of hepatic
synthesis of CRP, in unstable angina patients . Zue et al. showed that interleukin (IL)-1β, IL-6, tumor necrosis factor (TNF)-α, IL-8, and IL-10 increase significantly in acute herpes zoster and post herpetic neuralgia patients compared with the healthy controls . Ridker et al. also reported that high serum high sensitivity CRP (hs-CRP) level is a strong predictor of cardiovascular mortality in the general population .
Atherosclerosis is a chronic inflammatory vascular disease on the endothelium cells of vascular walls, leading to cardiovascular disorders. Cytokine, LDL, and inflammatory cells participate in the mechanism of atherosclerosis. As a result, herpes zoster increases the possibility of atherosclerosis formation via IL-6 and other
cytokines.
Herpes zoster causes long-term neurologic complications, such as post herpetic neuralgia. It may increase the risk of depression even without the depression history. A recent meta-analysis has associated depression with CRP and IL-6, which increased the atherosclerosis process . However, stress also affects myocardial metabolism without passing through the inflammation pathway . Alternatively, varicella-zoster virus reactivations may infect the sympathetic and autonomic ganglia. The infection affects the autonomic nervous system of the colon due to the centripetal spread from the dorsal ganglion . The reactivation may involve multi-loci, including dermatome and symptomatic ganglia that innervate the heart, leading to a cardiovascular disease.
One of the highlights of this study is the large comparison cohort of the herpes zoster cohort with stratified age and gender. The effects of diabetes, hypertension, and hyperlipidemia on cardiovascular diseases have been adjusted according to the Cox proportional hazards regression model. However, this study has some limitations. First, the diagnoses of herpes zoster, coronary artery disease, and arrhythmia are based on the ICD code of the claims data. No image or electrocardiogram (EKG) proven data is assembled in the administrative claims database. However, the patients in Taiwan are free to seek a cardiologist for assistance if they experience
cardiovascular symptoms. General practitioners are more likely to transfer a patient to a specialist if a cardiovascular disease is suspected. Similarly, the patients in Taiwan go directly to a dermatologist because skin lesions and herpes zoster are not difficult
to diagnose. Second, the incidence of coronary artery disease may be underestimated when patients do not seek for medical care for mild unnoticeable symptoms.
However, both cohorts may have similar disadvantages. Third, we do not have the knowledge of herpes zoster history in the controls before the claims data were
electronically established in 1996. Thus, misclassification may occur for both cohorts. In conclusion, the risk of arrhythmia and coronary artery disease associated with herpes zoster is weaker than that with diabetes, hypertension, and hyperlipidemia. However, herpes zoster is an easy visual marker for immunologic depression. This study shows that herpes zoster potentially increases cardiovascular presentations, especially within five years after herpes zoster is diagnosed. Therefore, greater cautions must be observed by those who have developed arrhythmia.
References
Table 1. Demographic characteristics and comorbidity in cohorts with and without herpes zoster
Herpes zoster No P value
N = 77932 Yes N = 19483 Age, years Mean±SD 46.3±16.0 46.4±16.0 0.71 20-39 27784(35.7) 6953(35.7) 0.96 40-64 38020(48.8) 9485(48.7) 65+ 12128(15.6) 3045(15.6) Gender Women 36868(47.3) 9217(47.3) 0.99 Men 41064(52.7) 10266(52.7) Comorbidity Diabetes 4935(6.33) 1547(7.94) <0.0001 Hypertension 10800(13.9) 3125(16.0) <0.0001 Hyperlipidemia 6563(8.42) 2118(10.9) <0.0001
Table 2. Incidence, incidence rate ratio, and hazard ratio of arrhythmia and coronary artery disease in herpes zoster cohort compared with non-herpes zoster cohort
Non- herpes zostercohort Herpes zoster cohort
Outcome Event PY Rate Event PY Rate IRR (95% CI) Adjusted HR(95% CI)
Arrhythmia 5214 461811 11.3 1518 114708 13.2 1.17(1.13, 1.22) 1.16(1.09, 1.23) Without comorbidity 3382 379161 8.92 952 89584 10.6 1.19(1.14, 1.25) 1.22( 1.13,1.31) With comorbidity 1832 82650 22.2 566 25124 22.5 1.02(0.94, 1.10) 1.04(0.95, 1.14) Coronary artery disease 3673 469000 7.83 1057 116771 9.05 1.16(1.11, 1.21) 1.11(1.04, 1.19) Without comorbidity 1750 387766 4.51 443 92123 4.81 1.07(1.01, 1.12) 1.11(1.00, 1.23) With comorbidity 1923 81234 23.7 614 24647 24.9 1.05(0.97, 1.14) 1.07(0.98, 1.17) PY, person-years
aRate, incidence rate per 1,000 person-years bIRR, incidence rate ratio
Table 3. Incidence, incidence rate ratio and hazard ratio of arrhythmia and coronary artery disease in herpes zoster cohort compared with non-herpes zoster cohort by comorbidity
Non-herpes zoster cohort Herpes zoster cohort
IRRb(95% CI) Adjusted HR
(95% CI)
Event PY Ratea Event PY Ratea
Arrhythmia Without comorbidity 3382 379161 8.92 952 89584 10.6 1.19(1.14, 1.25) 1(Reference) With comorbidity 1832 82650 22.2 566 25124 22.5 1.02(0.94, 1.10) 1.59(1.50, 1.68) Diabetes No 4689 435447 10.8 1340 106389 12.6 1.17(1.12, 1.22) 1(Reference) Yes 525 26365 19.9 178 8319 21.4 1.07(0.93, 1.24) 0.96(0.88, 1.04) Hypertension No 3795 403920 9.40 1115 98059 11.4 1.21(1.16, 1.27) 1(Reference) Yes 1419 57892 24.5 403 16648 24.2 0.99(0.90, 1.09) 1.44(1.35, 1.53) Hyperlipidemia No 4509 426893 10.6 1276 103184 12.4 1.17(1.12, 1.22) 1(Reference) Yes 705 34918 20.2 242 11524 21.0 1.04(0.92, 1.17) 1.15(1.07, 1.24) Coronary artery disease Without comorbidity 1750 387766 4.51 443 92123 4.81 1.07(1.01, 1.12) 1(Reference) With comorbidity 1923 81234 23.7 614 24647 24.9 1.05(0.97, 1.14) 2.90(2.73, 3.08) Diabetes No 3069 443568 6.92 832 108721 7.65 1.11(1.06, 1.16) 1(Reference) Yes 604 25431 23.8 225 8050 28.0 1.18(1.03, 1.35) 1.21(1.12, 1.32) Hypertension No 2139 412443 5.19 597 100629 5.93 1.14(1.09, 1.20) 1(Reference) Yes 1534 56557 27.1 460 16142 28.5 1.05(0.96, 1.16) 2.16(2.02, 2.32) Hyperlipidemia No 2890 434716 6.65 788 105439 7.47 1.12(1.07, 1.18) 1(Reference) Yes 783 34284 22.8 269 11331 23.7 1.04(0.92, 1.17) 1.50(1.39, 1.62) PY, person-years
aRate, incidence rate per 1,000 person-years bIRR, incidence rate ratio
Table 4. Trends of cardiovascular event risks by stratified follow-up years
Non-herpes zosterCohort herpes zoster Cohort Follow time,
years Event PY Ratea Event PY Ratea IRRb(95% CI)
Adjusted HR (95% CI) Arrhythmia ≤ 2 years 2039 151741 13.4 627 37782 16.6 1.24(1.18, 1.29) 1.22(1.12, 1.34) 2-5 1738 176659 9.84 511 43892 11.6 1.18(1.13, 1.24) 1.16(1.05, 1.29) 5-8 992 96065 10.3 266 23858 11.1 1.08(1.01, 1.15) 1.06(0.93, 1.22) > 8 445 37347 11.9 114 9175 12.4 1.04(0.95, 1.14) 1.03(0.84, 1.26) Coronary artery disease ≤ 2 years 1297 152615 8.50 388 38028 10.2 1.20(1.14, 1.26) 1.14(1.02, 1.28) 2-5 1383 178780 7.74 412 44493 9.25 1.20(1.14, 1.26) 1.15(1.03, 1.28) 5-8 739 98178 7.53 194 24480 7.92 1.05(0.99, 1.12) 1.01(0.86, 1.18) > 8 254 39427 6.44 63 9769 6.45 1.00(0.91, 1.10) 0.98(0.74, 1.29) PY, person-years
aRate, incidence rate per 1,000 person-years bIRR, incidence rate ratio
Supplemental Table 1. Incidence, incidence rate ratio and hazard ratio of coronary artery disease and stroke in herpes zoster cohort compared with non-herpes zoster cohort for those with arrhythmia
Non-herpes zostercohort herpes zoster cohort
Outcome Event PY Ratea Event PY Ratea IRRb(95% CI) Adjusted HR
(95% CI) Coronary artery disease 1178 18138 64.9 351 5067 69.3 1.05(0.92, 1.20) 1.08(0.96, 1.22) Without comorbidity 584 25102 23.3 156 6967 22.4 0.96(0.81, 1.14) 1.02(0.86, 1.22) With comorbidity 594 10523 56.5 195 3129 62.3 1.10(0.91, 1.34) 1.11(0.95, 1.31) Stroke 516 39790 13.0 125 11616 10.8 0.83(0.71, 0.97) 0.90(0.74, 1.09) Without comorbidity 229 27157 8.43 55 7627 7.21 0.86(0.70, 1.05) 0.97(0.72, 1.30) With comorbidity 287 12632 22.7 70 3988 17.6 0.77(0.61, 0.98) 0.83(0.64, 1.08) PY, person-years
aRate, incidence rate per 1,000 person-years bIRR, incidence rate ratio