http://oto.sagepub.com/
Otolaryngology -- Head and Neck Surgery
http://oto.sagepub.com/content/133/3/352
The online version of this article can be found at: DOI: 10.1016/j.otohns.2005.05.045
2005 133: 352 Otolaryngology -- Head and Neck Surgery
Pa-Chun Wang, Chul-Ho Jang, Yu-Hsiang Shu, Chih-Jaan Tai and Ko-Tsung Chu
Cost-Utility Analysis of Tympanomastoidectomy for Adults with Chronic Suppurative Otitis Media
Published by:
http://www.sagepublications.com On behalf of:
American Academy of Otolaryngology- Head and Neck Surgery
can be found at:
Otolaryngology -- Head and Neck Surgery
Additional services and information for
http://oto.sagepub.com/cgi/alerts Email Alerts: http://oto.sagepub.com/subscriptions Subscriptions: http://www.sagepub.com/journalsReprints.nav Reprints: http://www.sagepub.com/journalsPermissions.nav Permissions: What is This? - Sep 1, 2005 Version of Record >>
at NATIONAL CHIAO TUNG UNIV LIB on April 26, 2014
oto.sagepub.com
Downloaded from oto.sagepub.com at NATIONAL CHIAO TUNG UNIV LIB on April 26, 2014 Downloaded from
Cost– utility Analysis of Tympanomastoidectomy for
Adults with Chronic Suppurative Otitis Media
Pa-Chun Wang, MD, MSc, Chul-Ho Jang, MD, Yu-Hsiang Shu, BS,
Chih-Jaan Tai, MD, MSc, and Ko-Tsung Chu, MA, Taipei, Taiwan, Taichung,
Taiwan, Gwangju, South Korea, and Hsin-chu, Taiwan
OBJECTIVE: To undertake cost– utility analysis for tympano-mastoid surgery to analyze its cost-effectiveness in treating adult chronic suppurative otitis media (CSOM).
METHODS: Seventy-seven patients with CSOM were evalu-ated with the Chronic Ear Survey (CES) before and 1 year after tympanomastoid surgery. Direct health care cost data during the 1st year after operation were retrieved. The utility gain was defined as change in the CES total score. The cost– utility ratio (CUR) was defined as cost per utility gain. Patients were stratified by disease type into wet-ear and dry-ear groups.
RESULTS: The average total direct cost attributable to tympano-mastoid surgery is (in New Taiwan dollars [NT$]) 45,716.3 in the 1st postoperative year, and the average CUR is NT$ 1850.9. The lower CUR of NT$ 1280.9 for the wet-ear group is due to the greater utility gain (37.6⫾ 3.4 versus 24.4 ⫾ 6.8, P ⬍ 0.05) despite its higher cost (NT$ 48,163.2 versus NT$ 38,419.7, P⬍ 0.05).
CONCLUSIONS: Treating continuously or intermittently draining ears is more cost-effective, as compared with managing a quiescent infection, because of its favorable utility gain. © 2005 American Academy of Otolaryngology–Head and Neck Surgery Foundation, Inc. All rights reserved.
C
ost– utility analysis has emerged as a basic tool to assess the cost-effectiveness of health care practice. The cost, outcomes, and clinical process are incorporated into a decision-analytical model, and the expected cost–utility ratio (CUR) can be calculated. CUR provides a quan-tified assessment of medical interventions; unit of clinical effects from a particular medical intervention can be de-scribed in terms of benefit and cost. There has been height-ened awareness in recent years of the necessity for health care sectors to live within budgets. The climate in the shifting health care system toward a more managed envi-ronment has placed health care providers in a position to streamline resources and to provide quality care in the most cost-effective way. In terms of cost and health improvement trade-offs, it is essential to understand the relative values for medical and surgical interventions.1-3
Adult chronic suppurative otitis media (CSOM) is a major disease entity in otolaryngology practice. Thus, it is our intent to gather more scientific evidence for the estab-lishment of practice guidelines in surgical treatment of adult CSOM. The aims of this study are to evaluate the cost structure of tympanomastoid surgery, and to analyze the CURs for different CSOM disease groups.
MATERIAL AND METHODS
Study Design
The study was conducted in a prospective, nonrandomized manner. Seventy-seven consecutive adult patients with From the Department of Otolaryngology, Cathay General Hospital, Fu
Jen Catholic University School of Medicine, Taipei, Taiwan (Dr Wang); Department of Public Health (Dr Wang) and Department of Otolaryngol-ogy (Dr Tai), China Medical University, Taichung, Taiwan; Department of Otolaryngology, Chonnam National University Medical School, Chonnam National University Hospital, Gwangju, South Korea (Dr Jang); Graduate School of Epidemiology, College of Public Health, National Taiwan Uni-versity, Taipei, Taiwan (Dr Shu); and Graduate Institute of Management of Technology, National Chiao Tung University, Hsin-Chu, Taiwan (Mr Chu).
Presented at the 2004 Annual Meeting of the American Academy of Otolaryngology –Head and Neck Surgery, New York, NY, September 19-22, 2004.
Reprint requests: Ko-Tsung Chu, MA, Graduate Institute of Manage-ment of Technology, National Chiao Tung University, PO Box HuKuo 5-35, Hsinchu, Taiwan.
E-mail address: ktc1009@must.edu.tw.
0194-5998/$30.00 © 2005 American Academy of Otolaryngology–Head and Neck Surgery Foundation, Inc. All rights reserved. doi:10.1016/j.otohns.2005.05.045
CSOM undergoing tympanomastoid surgery at the Cathay General Hospital were enrolled during a period from Janu-ary 2000 to December 2000. Informed consent to participate and institutional review board approval were obtained in advance. Patients were administered the validated Chinese-version Chronic Ear Survey (CES)4,5before and 1 year after surgery. Direct health care costs generated by tympanomas-toid surgery during the 1st year after operation were re-trieved from the hospital claim database.
Disease Classification
On the basis of clinical findings and otorrhea history, pa-tients were further stratified by disease type (wet-ear and dry-ear groups) using the classification system proposed by Nadol.6The wet-ear group was composed of patients with (1) chronic active otitis media without cholesteatoma (with granulation), (2) chronic active otitis media with cholestea-toma, and (3) chronic inactive otitis media with frequent reactivation. The dry-ear group was composed of patients with chronic inactive otitis media.
Surgery
Standard tympanoplasty with (n⫽ 58) or without mastoid-ectomy (n⫽ 19) were performed under general anesthesia on all patients. The tympanomastoid surgery is an inpatient service in our institute.
Medical Resource Utilization and Cost Calculation
Medical resource utilization information, including the length of stay, frequency of postoperative office visits, and duration of medication were retrospectively obtained from medical records. Records of revision operation within 1 year after the initial tympanomastoid surgery were also identified.
Cost data were retrieved from the hospital claim data-base. The up-front admission cost for each hospitalization was composed of physician fee, ward fee, nursing fee, laboratory fee, operation fee, anesthesia fee, inpatient dis-pensary service fee, and other miscellaneous fees (Table 1). Costs associated with the postoperative outpatient service, including antibiotics, physician fee, registration fee, ENT local treatment fee, and dispensary, also are listed inTable 1. The cumulative cost for tympanomastoid surgery is de-fined as a summation of admission cost, postoperative 1-year outpatient services cost, and readmission cost. The admission cost is adjusted with reoperation and inflation (5%) rates. The monetary unit is in 2000 New Taiwan dollars (NT$); the average exchange rate with US dollars was around 33.5:1 within that year. The formula for calcu-lating 1-year cumulative cost is as follows:
Cumulative cost⫽ admission cost
⫹ postoperative 1-year outpatient services cost ⫹ readmission cost (reoperative rate
⫻ admission cost ⫻ 1.05)
Utility Measure
Developed by the Massachusetts Eye and Ear Infirmary, the CES is a statistically validated chronic ear-specific outcomes measure.4It is a 13-item Likert scale survey that uses 3 sub-scales. The activity restriction (AR) subscale examines the impact of chronic otitis media on a patient’s daily life. The symptom subscale (SY) examines the presence of symptoms such as hearing impairment and drainage, whereas the medical resource utilization subscale (MR) reviews the use of medica-tions and office visits. The Chinese version CES (CCES) used in this study was previously validated, and its performance characteristics proved to be equivalent to the CES.5
Cost–Utility Ratio
The CUR is defined as the 1-year cumulative cost divided by the change in the CES total score. The formula for CUR is as follows:
Cost–utility ratio ⫽ 1-year cumulative cost
⫼ change in the CES total score.
Statistical Analysis
Fisher’s exact test was used to compare recurrence rates between disease groups. Mann-Whitney U tests were used to compare the medical resource utilization, costs, utility gains, and CURs between different CSOM groups. All data were stored in an Access 7.0 database (Microsoft, Seattle, WA). Analyses were conducted by using the SAS software package (SAS Institute, Cary, NC). Continuous data are presented as mean⫾ standard deviation.
Table 1
Unit cost for the surgical treatment of CSOM
Cost structure Unit cost (NTD$) Admission service item
Physician fee 243/day Ward fee 512/day Nursing fee 613/day
Lab fee 1,218/admission Pathology exam fee 1,714/specimen Image fee 200/admission Tympanoplasty 12,000/admission Tympanomastoidectomy 15,000/admission Anesthesia (⬍2 h) fee 3850/operation Anesthesia (2–4 h) fee 880/30 min Anesthesia (⬎4 h) fee 1100/30 min Inpatient dispensary fee 84/day Intravenous fluid fee 75/day Local treatment fee 280/day Material fee 85/admission Outpatient service item
Antibiotics 50/wk Ear drop 150/bottle Physician fee 213/visit Registration fee 150/visit ENT local treatment fee 120/visit
353 Wang et al Cost-utility Analysis of Tympanomastoidectomy for . . .
at NATIONAL CHIAO TUNG UNIV LIB on April 26, 2014
oto.sagepub.com
RESULTS
Patient Characteristics
The study population comprises 77 patients (male-female ratio, 20:57; mean age, 43.2⫾ 12.6 years). The distributions of systemic comorbid diseases are as follows: 2 with hy-pertension (2.6%), 2 with diabetes (2.6%), and 10 with nasal allergy (13.0%). The distribution of disease category is as follows: wet-ear group, 58 (75.3%, including 7 with cho-lesteatoma, 8 with granulation, and 43 with frequent reac-tivation), and dry-ear group, 19 (24.7%, including 3 with retraction pocket, 11 with perforation, 2 with ossicular re-sorption, and 3 with adhesive otitis media).6
Medical Resource Utilization
The surgeries all went smoothly; no adverse events were reported in this group of patients.
The mean operation time (including the induction and resuscitation time) is 158.0 ⫾ 51.9 minutes. There is a significant difference in operation time between the 2 dis-ease groups (P⬍ 0.05). Patients in the wet-ear group tend to have longer operation times.
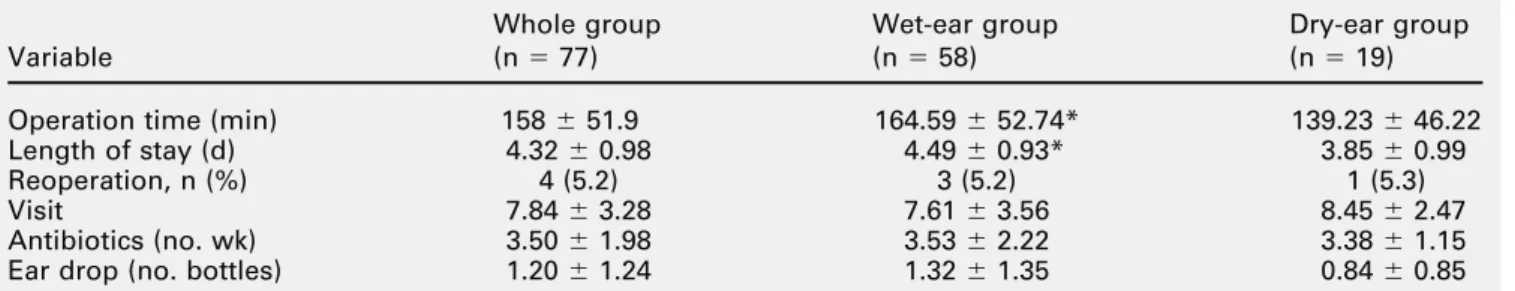
The average length of stay for this population is 4.32⫾ 0.97 days. The medical resources utilization within the 1-year period after tympanomastoid surgery is as follows: number of visits, 7.84⫾ 3.28; antibiotics use, 3.50 ⫾ 1.98 weeks; ear drops, 1.20⫾ 1.24 bottles. Except for length of stay (P⬍ 0.05), there is no significant difference in medical utilization within 1 year after tympanomastoid surgery be-tween different disease groups (P⬎ 0.05;Table 2). Patients in the wet-ear group tend to stay longer in the hospital (4.48 ⫾ 0.93 versus 3.84 ⫾ 0.98, P ⬍ 0.05); but the postoperative visit number and medication use (both antibiotics and ear drop) are similar in both groups.
The recurrence rate within 1 year after tympanomastoid surgery is 5.2%. A total of 4 revision surgeries are identi-fied. The reoperation rates are 3 (5.2%) for the wet-ear group and 1 (5.3%) for the dry-ear group. There is no significant difference in recurrence rates between the dis-ease groups (P⬎ 0.05).
One-Year Cumulative Cost
The operation (NT$ 19,447.1) and anesthesia (NT$ 6906.1) fees comprise 55% and 19% of the up-front admission cost (NT$ 35,691.94), respectively. The inpatient medication, laboratory, and physician fees comprise 5%, 4%, and 3% of the up-front admission cost, respectively. The ward fee is 9% of the up-front admission cost, based on an average of 4.3 days’ stay in the hospital. The admission cost structure analysis is shown inFigure 1.
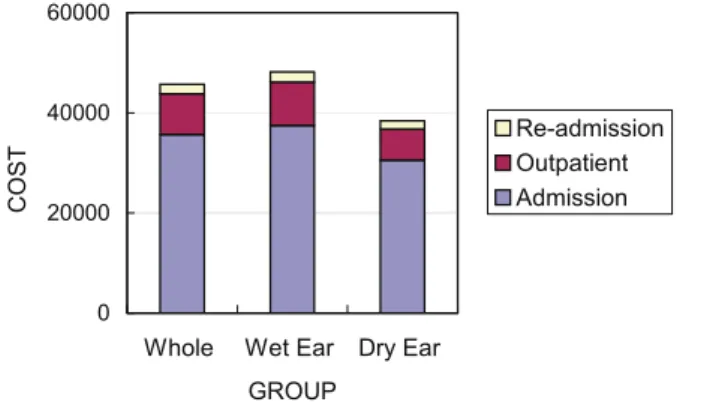
The average cumulative cost within a 1-year period after tympanomastoid surgery is NT$ 45,716.3. The components of tympanomastoid surgery cost structure are as follows: admission cost, NT$ 35,691.9 (78.07%); outpatient services cost, NT$ 8112.7 (17.75%); and readmission cost, NT$ 1911.7 (4.18%). The cumulative costs for different disease groups are listed inFigure 2.
Utility Gain
The average utility gain is 24.7⫾ 3.0 in the change of the CES total scores. The utility gains for different disease groups are as follows: wet-ear group, 37.6 ⫾ 3.4; and dry-ear group, 24.4 ⫾ 2.2 (Fig 3). There are significant differences in the changes of the CES total scores between disease groups (P⬍ 0.05).
Cost–Utility Ratio
The average CUR ($NT/utility gain) is 1850.9 New Taiwan dollars per utility gain, and the CURs for different disease groups are as follows: wet-ear group, NT$ 1280.9; and
Figure 1 Cost structure for the surgical treatment of CSOM.
Table 2
1-year medical resource utilization
Variable Whole group (n⫽ 77) Wet-ear group (n⫽ 58) Dry-ear group (n⫽ 19) Operation time (min) 158⫾ 51.9 164.59⫾ 52.74* 139.23⫾ 46.22 Length of stay (d) 4.32⫾ 0.98 4.49⫾ 0.93* 3.85⫾ 0.99 Reoperation, n (%) 4 (5.2) 3 (5.2) 1 (5.3) Visit 7.84⫾ 3.28 7.61⫾ 3.56 8.45⫾ 2.47 Antibiotics (no. wk) 3.50⫾ 1.98 3.53⫾ 2.22 3.38⫾ 1.15 Ear drop (no. bottles) 1.20⫾ 1.24 1.32⫾ 1.35 0.84⫾ 0.85
*Mann-Whitney U test, comparison between wet-ear and dry-ear group, P⬍ 0.05. Continuous data are presented as mean⫾ standard deviation.
dry-ear group, NT$ 1574.6 (Fig 4). There is a significant difference in the CUR between disease groups (P ⫽ 0.0001).
Sensitivity Test
In general, shortening length of stay by 1 day (discounting the sum of NT$ 1807 from daily physician, ward, nursing, dispensary, intravenous fluid, and local treatment charges;
Table 1) will reduce average CUR by NT$ 73.1 for the whole group. Improving the reoperation rate by 1% (dis-counting readmission cost by NT$ 374.7) will reduce aver-age CUR by NT$ 15.1.
DISCUSSION
Cost-effectiveness analysis (CEA) is a method for evaluat-ing the outcomes and costs of interventions designed to improve health. The results are usually summarized in CURs that demonstrate the cost of achieving a unit of health effect for diverse types of patients or for variations of intervention. In a CUR, changes in health caused by an intervention can be captured in the denominator; and changes in resource use, valued in monetary terms, are captured in the numerator. The central function of CEA is to
show the relative values of alternative interventions for improving health. Information provided by CEA can help decision makers in a variety of settings to prioritize their constrained medical resources.1-3
The average total direct cost attributable to CSOM in the 1-year period after tympanomastoid surgery is NT $45,716.3, or US$ 1364.6 (2000⬃2001 average exchange rate, 33.5 NT$ to 1 US$); the majority of that cost stems from the up-front operation-related fees (operation, 43.0%; anesthesia, 15.1%). Treating wet-ear group patients is more expensive; the 1-time admission cost is 23% higher in the wet-ear group (NT$ 37,490.0) than that of NT$ 30,574.4 in the dry-ear group. Our data demonstrate that the upfront cost is sensitive to the change of operation cost, anesthesia time, and length of stay in the hospital. For example, the variance in cost-effectiveness regarding length of stay for the whole group shows that the reduction of hospitalization by 1 day will reduce the CUR value by 3.9% accordingly. The aftercare expenses during the 1st year after tympa-nomastoid surgery comprise 17.7% (16.07% for the dry-ear group and 17.9% for the wet-ear group) of the total 1-year cumulative cost. The 1-year postoperative outpatient ser-vices cost is nearly 40% higher in the wet-ear group (NT$ 8665.2 versus NT$ 6176.2); the difference of NT$ 2489 may partly attribute to the significant difference in cumula-tive cost between 2 disease groups. Data from previous CEA research on the endoscopic sinus surgery demon-strated that the after-care expenses were case sensitive and might amount to one fourth of the total cumulative cost.7 Our data in this study prove that outpatient medical resource utilization during the 1st postoperative year is also a major determinant of cumulative costs after chronic ear surgery.
A conservative, short-term estimation on rate of recur-rence or failure for the chronic ear surgery is around 5% in this study. Merchant et al8reported a 95% so-called dry-ear rate with a minimum of 12 months’ follow-up after chronic ear surgery. A review of the otologic literature indicates that the incidence of dry ears in various large clinical series ranges between 70% and 95%9-15; greater differences be-tween wet-ear and dry-ear groups in recurrence rates might be observed over time. However, the readmission cost plays a relatively minor role by comprising only 4.18% of the total cumulative cost. Sensitivity simulation shows that the
Figure 2 One-year cumulative cost for surgical treatment of CSOM.
Figure 3 One-year utility gain after tympanomastoid surgery.
Figure 4 Cost– utility ratio for surgical treatment of CSOM.
355 Wang et al Cost-utility Analysis of Tympanomastoidectomy for . . .
at NATIONAL CHIAO TUNG UNIV LIB on April 26, 2014
oto.sagepub.com
reduction of revision rate by 1% will barely reduce the CUR value by 0.8% accordingly.
Theoretically, healthcare effectiveness can be measured in terms of quality-of-life-years (QALYs); use of interval-scaled, patient-perceived health status to serve as a utility measure also is an acceptable alternative. As an adjunct to objective clinical findings, the CES we used in this study is a well-established subjective outcome measure in reporting tympanomastoid surgery results.16-18 The change in the CES total score of 24.7 ⫾ 3.0 points for the whole popu-lation is suggestive of a meaningful enhancement in their ear-related quality of life. We found that the effects of surgery are particularly remarkable for patients with drain-ing ears. The significantly superior improvements of all CES subscores (AR, SY, MR) are observed in the wet-ear group.
The average CUR indicates that the average cost is around $1850 New Taiwan dollars, or $55.2 US dollars to gain 1 unit of ear-specific quality-of-life. The CUR is a product of sophisticated multifactorial effect; even though the 1-year cumulative cost for the wet-ear group of NT$ 48,163.2 is 25% higher than that of the dry-ear group (NT$ 38,419.7), the favorable CUR for wet-ear group is caused by its preferred utility gain (54% greater than that of dry-ear group). Our data support that treating continuous or inter-mittent chronic draining ear is most cost-effective because of their favorable utility gain and relatively reasonable cost. However, the efficacy of surgery for dry chronic otitis media should not be discouraged by these cost utility data; patients in the dry-ear group still proved to benefit from surgery by showing significant improvement in their quality of life (Fig 3).
This study has followed the consensus in reporting CEA results.1-3However, because the actual direct costs of tym-panomastoid surgery are difficult to obtain, readers are re-minded that the cost calculations in this study are based on hospital bills (claim data); the price variation and intangible opportunity costs are not taken into consideration. Also, the cost– utility methodology can be limited by the assumptions underlying its model, and the exploration of this study might be restricted by the relatively small cohort data from a single institution.
CONCLUSION
CSOM is one of the most common surgical disease entities in otolaryngology practice. The cost– utility data generated from this study provide more scientific evidence for the establishment of tympanomastoid surgery practice guide-lines. We find that treating continuous or intermittent
drain-ing ear is more cost-effective, as compared with managdrain-ing a quiescent infection, because of its favorable utility gain. Disease subclassification and outcomes data are key infor-mation needed for a cost-effective approach to tympano-mastoid surgery.
REFERENCES
1. Russell LB, Gold MR, Siegel JE, et al. The role of cost-effectiveness analysis in health and medicine. JAMA 1996;276:1172–7. (Grade D). 2. Weinstein MC, Siegel JE, Gold MR, et al. Recommendations of the panel on cost-effectiveness in health and medicine. JAMA 1996;276: 1253– 8. (Grade D).
3. Siegel JE, Weinstein MC, Russell LB, et al. Recommendations for reporting cost-effectiveness analysis. JAMA 1996;276:1339 – 41. (Grade D).
4. Wang PC, Nadol Jr, JB Merchant SN, et al. Validation of outcomes survey for adults with chronic suppurative otitis media. Ann Otol Rhinol Laryngol 2000;109:249 –54. (Grade B).
5. Wang PC, Chu CC, Liang SC, et al. Validation assessment of the Chinese version Chronic Ear Survey: a comparison between data from English and Chinese versions. Ann Otol Rhinol Laryngol 2003;112: 85–90. (Grade B).
6. Nadol Jr. JB Chronic otitis media. In: Nadol JB Jr, McKenna MJ, editors. Surgery of the ear and temporal bone, 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2004. p. 199 –218 (Grade D). 7. Wang PC, Chu CC, Liang SC, et al. Cost-utility analysis for
endo-scopic sinus surgery. Otolaryngol Head Neck Surg 2004;130:31– 8. (Grade B).
8. Merchant SN, Wang PC, Jang CH, et al. Efficacy of tympanomastoid surgery for control of infection in active chronic otitis media. Laryn-goscope 1997;107:872–7. (Grade B).
9. Nadol Jr. JB Causes of failure of mastoidectomy for chronic otitis media. Laryngoscope 1985;95:410 –3. (Grade B).
10. Cody DTR, McDonald TJ. Mastoidectomy for acquired cholesteatoma: follow-up to 20 years. Laryngoscope 1984;94:1027–30. (Grade B). 11. Vartiainen E, Nuutinen J. Long-term results of surgical treatment in
different cholesteatoma types. Am J Otol 1993;14:507–11. (Grade B). 12. Jackson CG, Glasscock ME, Nissen AJ, et al. Open mastoid proce-dures: contemporary indications and surgical technique. Laryngoscope 1985;95:1037– 43. (Grade B).
13. Paparella MM, Kim CS. Mastoidectomy update. Laryngoscope 1977; 87:1977– 88. (Grade B).
14. Sheehy JL, Brackmann DE, Graham MD. Cholesteatoma surgery: residual and recurrent disease. A review of 1,024 cases. Ann Otol 1977;86:451– 62. (Grade B).
15. Lee K, Schuknecht HF. Results of tympanoplasty and mastoidectomy at the Massachusetts Eye and Ear Infirmary. Laryngoscope 1971;81: 529 – 43. (Grade B).
16. Wang PC, Tai CJ, Shu YH, et al. Quality of life investigation for patients with chronic otitis media. J Taiwan Otolaryngol Soc 2001;36: 360 –70. (Grade B).
17. Yen MS, Wang PC, Shu YH, et al. Quality of life improvement following chronic ear surgery. J Taiwan Otolaryngol Soc 2002;37: 424 –30. (Grade B).
18. Nadol Jr, JB Staecker H, Gliklich RE. Outcomes assessment for chronic otitis media: the Chronic Ear Survey. Laryngoscope 2000;110: 32–5. (Grade B).