Brief communication
Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality
Index (CPSQI) in primary insomnia and control subjects
Pei-Shan Tsai, Shu-Yi Wang, Mei-Yeh Wang, Chein-Tien Su, Tsung-Tsair Yang, Chun-Jen Huang & Su-Chen Fang
College of Nursing, Taipei Medical University, Taipei 110, Taiwan (E-mail: ptsai@tmu.edu.tw)
Accepted in revised form 21 March 2005
Abstract
In order to effectively study the population experiencing insomnia, it is important to identify reliable and valid tools to measure sleep that can be administered in the home setting. The purpose of this study was to assess psychometric properties for the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in community-dwelling adults with primary insomnia. The CPSQI had an overall reliability coefficient of 0.82–0.83 for all subjects. ‘Subjective sleep quality’ was the component most highly correlated with the global score. Overall, the CPSQI showed acceptable test–retest reliability over a 14- to 21-day interval with a coefficient of 0.85 for all subjects and 0.77 for primary insomniacs. The two contrasting groups had significantly different global and component scores. A CPSQI of greater than 5 yielded a sensitivity and specificity of 98 and 55% in primary insomniacs vs. controls. A CPSQI of greater than 6 resulted in a sensitivity and specificity of 90 and 67%. Results suggest that the CPSQI is a psychometrically sound measure of sleep quality and disturbance for patients with primary insomnia. It may not be an effective screening tool because of its low specificity, but it can be a sensitive, reliable, and valid outcome assessment tool for use in community-based studies of primary insomnia
Key words: Pittsburgh Sleep Quality Index, Primary insomnia, Psychometric properties
Introduction
Insomnia is a common psychological health problem in the general population. It is a hetero-geneous complaint reflecting reduced quality, duration, or efficiency of sleep [1]. A national telephone survey conducted by the National Sleep Foundation in conjunction with the Gallup Organization found that about 25% of Americans reported occasional insomnia while 9% reported having sleep difficulty on a regular basis [2]. A study that assessed 5078 married women aged 20–59 in an urban community of northern Taiwan found that the prevalence rates of difficulty initi-ating sleep, difficulty maintaining sleep, and early morning awakening were 29.5, 38.17, and 26.02% [3], suggesting that a large proportion of people
living in Taiwan are similarly experiencing some types of sleep problem.
Insomnia can negatively impact individuals’ physical and social performance, as well as quality of life. The association between quality of life impairments and insomnia has been well docu-mented in the literature [4, 5]. Chronic insomnia necessitates treatment in the majority of cases, but it is often under-treated. Because the effectiveness of hypnotic medications in long-term use has been controversial, non-pharmacological therapy could be an effective treatment alternative for persistent insomnia [6, 7]. For primary insomnia in particu-lar, multifaceted cognitive-behavioral therapy (CBT) has been developed to counteract the cog-nitive and/or behavioral mechanism of insomnia. Despite the fact that a sizable portion of the
population is experiencing insomnia, effective community-based CBT programs are currently lacking. In order to effectively study the popula-tion experiencing insomnia, it is important to identify a reliable and valid tool to measure sleep that can be administered in the home setting. Subjective sleep quality can be a useful outcome measure for community-based randomized con-trolled trials of the effect of CBT on sleep. Researchers have traditionally utilized subjective assessment of sleep quality and disturbances in sleep research. The Pittsburgh Sleep Quality Index (PSQI) is a self-report questionnaire that assesses multiple dimensions of sleep over a 1-month time period [8, 9]. Nineteen individual items generate seven ‘component’ scores: subjective sleep quality, sleep latency, sleep duration, habitual sleep effi-ciency, sleep disturbances, use of sleeping medi-cation, and daytime dysfunction. The sum of the seven component scores yields one global score of subjective sleep quality (range 0–21); higher scores represent poorer subjective sleep quality.
PSQI has been used extensively in a variety of clinical populations. However, only limited pub-lished psychometric information for the PSQI is available. The original authors have established acceptable internal consistency, test–retest reli-ability, sensitivity, and specificity in depressed, sleep-disorder patients, and healthy subjects [8]. Apart from the original article, other studies have evaluated the psychometric properties of the PSQI and reported acceptable internal consistency [10], test–retest reliability [11], construct validity [10], and criterion-related validity [11] in several clinical populations including bone marrow transplant patients (n¼ 155), renal transplant patients (n¼ 56), women with breast cancer (n ¼ 102), women with benign breast problems (n¼ 102) [10], and individuals with primary insomnia (n¼ 80) [11]. Unfortunately, published psychometric data on the use of the PSQI in community-dwelling adults with primary insomnia has been limited.
We developed the Chinese version of the Pitts-burgh Sleep Quality Index (CPSQI) after obtain-ing permission from the original authors of the PSQI. The purpose of this study was to establish sensitivity, specificity, internal consistency, test– retest reliability, and construct validity data for the CPSQI in community-dwelling adults with primary insomnia.
Methods Participants
Participants were recruited from two study sites, a general practitioner clinic and a psychiatric clinic. Two physicians (a general practitioner and a psy-chiatrist) who participated in this study performed the screening of individuals’ eligibility for partici-pation in the study. The diagnostic criteria for primary insomnia were based on the fourth edition of the Diagnosis and Statistical Manual of Mental Disorders (DSM-IV) [12]. The 12-item Chinese Health Questionnaire (CHQ-12) [13] was used as a screening tool to identify potential participants who might be experiencing mental disorders. A CHQ-12 score of four was used as the cutoff value. The Mini International Neuropsychiatric Inter-view (MINI) [14]-Taiwan version 2.0.0 [15] was used to identify positive cases for any lifetime psychiatric disorder. After a thorough medical examination to rule out any psychiatric or somatic disorder underlying sleep disturbances, those who met the DSM-IV diagnostic criteria for primary insomnia were referred to as primary insomniacs; those who did not meet the DSM-IV diagnostic criteria for primary insomnia were referred to as healthy controls. A total of 244 potential partici-pants were referred to participate in the study, including 87 participants with primary insomnia and 157 healthy controls.
Translation of the PSQI
The PSQI was first translated into Mandarin Chinese (CPSQI) by a bilingual researcher from the research team (Wang SY). An independent bilingual researcher from the research team (Wang MY) then back-translated the first version of the CPSQI into English for content comparison. The first author (Tsai PS) who is also proficient in both English and Mandarin Chinese compared the content of each item in this back translated version with its corresponding item in the original English version. Consequently, some items in the first CPSQI were modified to better correspond to the meaning of the original item in PSQI. A lay panel was then asked to assess the comprehensibility of CPSQI, highlight errors, and suggest translation alternatives. The three research team members
then met to finalize the CPSQI based on the sug-gestions from the lay panel. The content of the final CPSQI was further verified by back translation procedure until both translated and back-translated versions were considered com-pletely interchangeable, conceptually and linguis-tically.
Instruments
Chinese Health Questionnaire-12
The 12-item CHQ-12 is a psychiatric screening instrument, which was developed by discriminant function analysis on the 30-item CHQ which is a Chinese translation of the General Health Ques-tionnaire originally developed by Goldberg with addition of several culturally-relevant items [13]. Each item specifically asks the respondent to rate their health status during the past weeks in four categories: ‘not at all’, ‘ no more than usual’, ‘more than usual’, and ‘a lot more than usual’. The possible scores for the CHQ-12 range from 0 to 12. The Cronbach’s a coefficients were 0.84 for the community sample (n¼ 1023) and 0.83 for the hospital sample (n¼ 386) [16].
7-Day Daily Sleep Log
The 7-day Daily Sleep Log is a sleep diary that collects information on total time spent in bed (TTSIB), sleep onset latency (SOL), total sleep time (TST), and frequency of awakenings. Sleep efficiency (SE) can be calculated using the formula: SE¼ TST/TTSIB. Participants were asked to fill out the sleep log as soon as they get out of the bed each morning for a consecutive 7-day period. Questions in the 7-day Daily Sleep Log include: 1. Last night, I went to bed at: (clock time) 2. Last night, I fell asleep in: (minutes)
3. I got out of bed this morning at: (clock time) 4. Last night I slept a total of: (hours and minutes) 5. I woke up during the night: (times)
Epworth Sleepiness Scale-Chinese version (CESS) The Epworth Sleepiness Scale (ESS) is a widely used scale that evaluates degree of somnolence. The Chinese version of the ESS (CESS) was translated and validated by Chen and colleagues [17]. The scale showed acceptable internal consis-tency (Cronbach a¼ 0.81, n ¼ 359) and accept-able test–retest reliability (Spearman’s q¼ 0.74,
n¼ 30) in individuals experienced symptoms of sleep-disordered breathing.
Stanford Sleepiness Scale
The Stanford Sleepiness Scale (SSS) is an instru-ment that measures daytime sleepiness [18]. The SSS consists of seven statements from which the respondent chooses to report his or her symptoms and feelings at the moment. Responses range from alert, wide awake, functioning with no problems to extremely drowsy, very tired, almost asleep. The possible scores range from 1 to 7; the greater the score the more severe the degree of sleepiness. The translation of SSS into the Chinese version fol-lowed the standard translation–back translation procedure.
Sleep Quality Visual Analogue Scale
The Sleep Quality Visual Analogue Scale (SQ-VAS) assesses an individual’s subjective feelings of overall sleep quality with a possible score ranging from 0 to 10; the greater the SQ-VAS score the better the sleep quality. The SQ-VAS contains a 10-cm line with numerals ‘0’ on one side and ‘10’ on the other, indicating ‘very poor’ sleep quality and ‘very good’ sleep quality, respectively. Partic-ipants were given an example of how to respond and asked to draw a vertical line to indicate their subjective sleep quality.
Study procedure
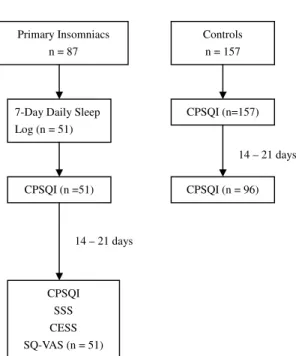
The study protocol is diagrammatically illustrated in Figure 1. All participants gave informed con-sent and filled out the CHQ. Demographic data (age, sex, education, and marital status) and information on lifestyle habits (alcohol consump-tion, smoking habit, and use of hypnotics) were also collected. All participants received the CPSQI twice over a test–retest interval of 14–21 days. Primary insomniacs filled out daily sleep logs over a period of 7 days before they received the CPSQI. On the second testing of the CPSQI, primary insomniacs also completed the SSS, the CESS, and the SQ-VAS. Questionnaires were completed at home and returned by mail in pre-stamped envel-oped. Of 87 primary insomniacs, 51 returned the completed questionnaires (sleep log, first CPSQI, second CPSQI, SSS, CESS, and SQ-VAS). All control subjects completed the first CPSQI but
only 96 controls returned the second CPSQI. The overall participation rate was 59.9% for the insomnia group and 61% for the control group. Statistical analyses
Differences in demographic data and lifestyle habits between the two contrasting groups were tested using the t-test (continuous variables) and the Mann–Whitney test (categorical variables).
Internal consistency was examined by comput-ing the reliability coefficient (Cronbach’s a). The criterion level for coefficient alpha was set at 0.70 or above. Pearson correlations between compo-nent scores and the global score were also calcu-lated to determine the internal homogeneity of the CQSPI. Each component score was treated as one item. The item-to-item correlation was performed to examine the contribution of each item and to examine any redundancy. Interitem correlations of between 0.30 and 0.70 were acceptable. Correla-tions above 0.70 suggest redundancy. Test–retest reliability was examined by Pearson correlations between the initial and retest component and global scores. The higher the test–retest reliability
coefficients, the more stable the scale is assumed to be, with 0.71 and over termed ‘substantial’ and 0.50–0.70 ‘moderate’.
Validity testing was performed by comparing scores on the instrument between contrasting groups (i.e., insomniacs vs. controls). In addition, the correlations between other subjective measures of sleep and selected component scores were also calculated.
Sensitivity was calculated as the percentage of cases (i.e., primary insomniacs) correctly classified by the cutoff value. Specificity was calculated as the percentage of non-cases (controls) correctly classi-fied by the cutoff value. Sensitivity of 90% or above and specificity of 90% or above were preferred. Results
Group comparison
The t-test and Mann–Whitney test revealed that the two contrasting groups differed significantly in age (41 ± 10 for insomniacs and 37 ± 14 for controls, p¼ 0.01), educational levels (p ¼ 0.007), marital status (p¼ 0.017), and the use of hypnot-ics (p < 0.001) whereas no differences were ob-served for sex (p¼ 0.314), alcohol intake (p¼ 0.628), and smoking habits (p ¼ 0.137). Internal consistency
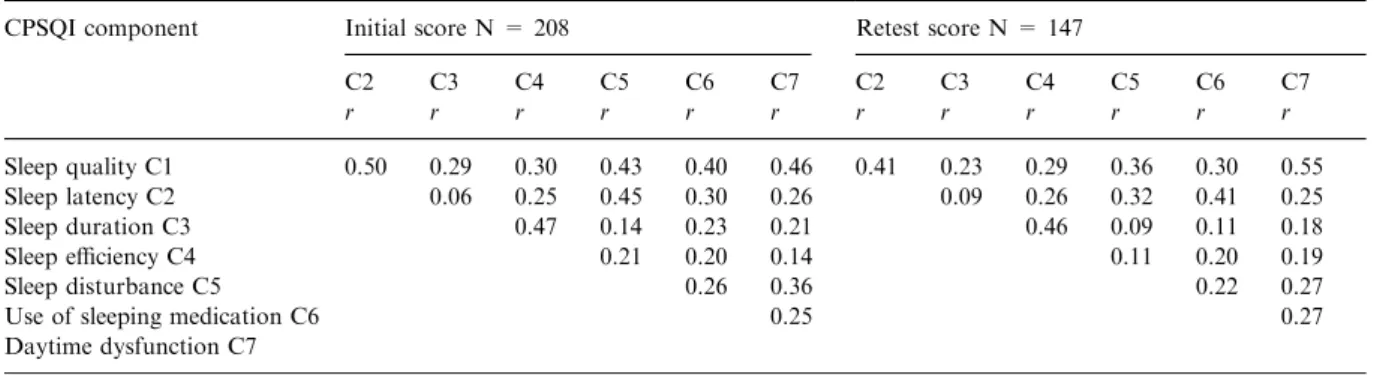
In all subjects, Cronbach’s a was 0.83 for the first testing (n¼ 208) and 0.82 for the second testing (n¼ 147) of the CPSQI. In primary insomniacs, Cronbach’s a was 0.72 for the first testing (n¼ 51) and 0.71 for the second testing (n¼ 51) of the CPSQI. To assess the homogeneity of the instru-ment, Pearson correlations between CPSQI global and components scores were calculated. On the first testing, the global-component correlation coefficients ranged from 0.59 to 0.75 with a mean of 0.71 (see Table 1). Similarly, for the second testing of the CPSQI the correlation coefficients between component scores and the global score ranged from 0.50 to 0.72 (see Table 1). Item-to-item correlation coefficients were calculated for all subjects and the correlations ranged from 0.06 (C2 and C3) to 0.50 (C1 and C2) for the first testing (see Table 2). Item-to-item analysis generated similar results for the second testing.
Primary Insomniacs n = 87
Controls n = 157
7-Day Daily Sleep Log (n = 51) CPSQI (n =51) CPSQI (n=157) CPSQI (n = 96) CPSQI SSS CESS SQ-VAS (n = 51) 14 – 21 days 14 – 21 days
Figure 1. Diagram of the study protocol. CPSQI: The Chinese version of Pittsburgh Sleep Quality Index; SSS: Stanford Sleepiness Scale; CESS: The Chinese version of Epworth Sleepiness Scale; SQ-VAS: Sleep Quality Visual Analogue Scale.
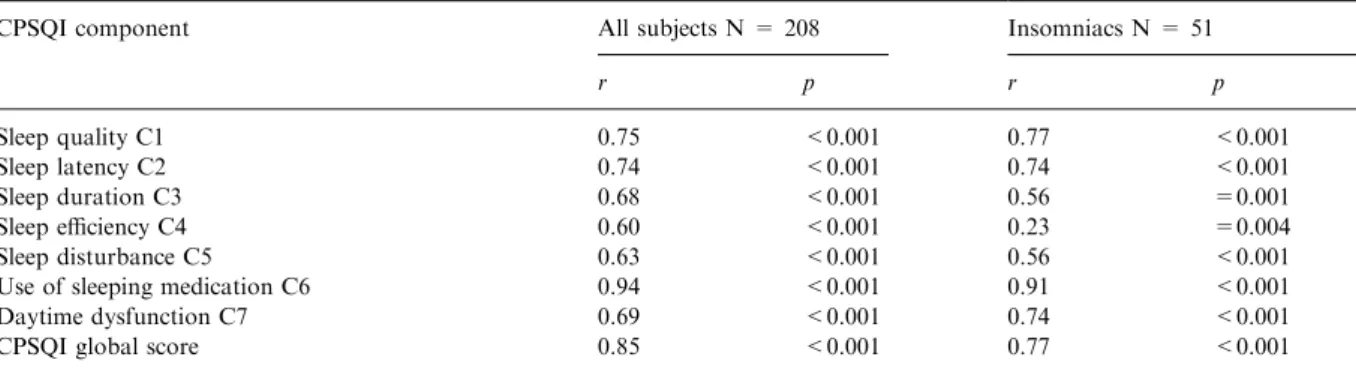
Test–retest reliability
In all subjects, the CPSQI global score had a test– retest reliability of 0.85 (p < 0.001). In primary insomniacs, the test–retest reliability for the CPSQI global score was 0.77 (p < 0.001). The test–retest reliability for each CPSQI component score (C1–C7) was also calculated for all subjects and for the primary insomnia group (see Table 3). In all subjects, all the initial component scores correlated well with the retest component scores. In primary insomniacs, the CPSQI test–retest correlation coefficients were moderate to sub-stantial (0.56–0.91) for the subscores with an exception of the subscore ‘habitual sleep efficiency’ (C4) which was low (r¼ 0.23).
Validity
The component and global scores of the CPSQI were compared between the two contrasting groups (see Table 4). There were statistically sig-nificant differences in all component scores (C1–
C7) and in the global score between the insomnia group (n¼ 51) and the control group (n ¼ 157) in both the initial and the retest CPSQI. The mean CPSQI global score was 10.58 for the insomnia group and 5.63 for the control group (p < 0.001). Similar results were replicated by the second test-ing of the CPSQI with the mean global score of 10.20 for the insomnia and 5.73 for the control group (p < 0.001).
In primary insomniacs, the CPSQI global score significantly correlated with SQ-VAS (r¼)0.30, p¼ 0.043). In addition, the CPSQI significantly correlated with SOL (r¼ 0.30, p ¼ 0.041) and SE (r¼)0.37, p ¼ 0.019) derived from the sleep diary. On the contrast, the correlations between the CPSQI global score and CESS and that between the CPSQI global score and SSS were non-significant.
Correlations between other subjective measures of sleep and selected CPSQI component scores were also calculated for the insomnia group. The C1 (sleep quality) score inversely and significantly correlated with the SQ-VAS (r¼)0.54, p < 0.001) (see Figure 2). Several component
Table 1. Correlations between the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) global and component scores
CPSQI component Initial score N = 208 Retest score N = 147
r p r p Sleep quality C1 0.75 <0.001 0.72 <0.001 Sleep latency C2 0.65 <0.001 0.67 <0.001 Sleep duration C3 0.58 <0.001 0.52 <0.001 Sleep efficiency C4 0.61 <0.001 0.60 <0.001 Sleep disturbance C5 0.59 <0.001 0.50 <0.001
Use of sleeping medication C6 0.60 <0.001 0.61 <0.001
Daytime dysfunction C7 0.60 <0.001 0.63 <0.001
Table 2. Item-to-item correlations for the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI)
CPSQI component Initial score N = 208 Retest score N = 147
C2 C3 C4 C5 C6 C7 C2 C3 C4 C5 C6 C7 r r r r r r r r r r r r Sleep quality C1 0.50 0.29 0.30 0.43 0.40 0.46 0.41 0.23 0.29 0.36 0.30 0.55 Sleep latency C2 0.06 0.25 0.45 0.30 0.26 0.09 0.26 0.32 0.41 0.25 Sleep duration C3 0.47 0.14 0.23 0.21 0.46 0.09 0.11 0.18 Sleep efficiency C4 0.21 0.20 0.14 0.11 0.20 0.19 Sleep disturbance C5 0.26 0.36 0.22 0.27
Use of sleeping medication C6 0.25 0.27
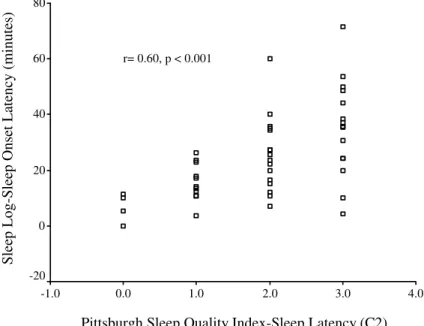
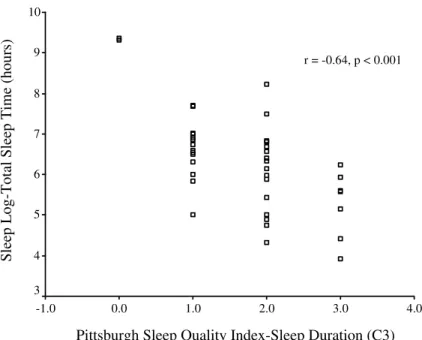
scores (i.e., C2, C3, and C4) significantly corre-lated to several sleep parameters derived from the 7-day Daily Sleep Log, including SOL, TST, and SE. The C2 (sleep latency) score significantly cor-related to the SOL (r¼ 0.60, p < 0.001) derived from the 7-day Daily Sleep Log (see Figure 3). The C3 (sleep duration) score inversely correlated with TST (r¼)0.64, p < 0.001) (see Figure 4). The C4 (habitual sleep efficient) inversely correlated with SE (r¼)0.36, p ¼ 0.021). The C7 score, which is an estimate of the daytime functioning, failed to exhibit significant correlations with other measures of daytime sleepiness used in this study, namely SSS and CESS.
Sensitivity and specificity testing
The CPSQI global score could sensitively identify subjects with poor sleep conditions. The sensitivity
of the CPSQI was 98% using a cutoff value of 5 to discriminate poor from good sleepers whereas the sensitivity was 90% using a cutoff value of 6. In terms of specificity, a cutoff value of 5 could cor-rectly categorize good sleepers with a specificity of 55% and a cutoff value of 6 could correctly cate-gorize good sleeps with a specificity of 67%.
Discussion
The results demonstrated that the seven compo-nents of the CPSQI had an overall reliability coefficient of 0.82–0.83 for all subjects, indicating a high degree of internal consistency. The reliability data was comparable to the data in 150 subjects (51 healthy controls, 34 depressed patients, 62 sleep-disordered patients) reported by the original authors [8]. In terms of internal homogeneity, the
Table 4. Comparisons of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) between primary insomnia and control subjectsa
CPSQI component score Initial score Retest score
Insomniacs N = 51 Controls N = 157 p Insomniacs N = 51 Controls N = 96 p Sleep quality C1 2.00 ± 0.66 1.14 ± 0.62 <0.001 1.98 ± 0.71 1.20 ± 0.69 <0.001 Sleep latency C2 1.85 ± 1.04 0.96 ± 0.83 <0.001 1.92 ± 0.94 0.95 ± 0.78 <0.001 Sleep duration C3 1.80 ± 0.92 1.22 ± 0.91 <0.001 1.71 ± 0.81 1.28 ± 0.88 =0.005 Sleep efficiency C4 0.82 ± 1.05 0.42 ± 0.81 =0.005 0.75 ± 0.91 0.40 ± 0.77 =0.016 Sleep disturbance C5 1.52 ± 0.54 1.04 ± 0.50 <0.001 1.37 ± 0.56 0.98 ± 0.51 <0.001 Use of sleeping medication C6 1.16 ± 1.30 0.03 ± 0.18 <0.001 1.20 ± 1.36 0.06 ± 0.24 <0.001 Daytime dysfunction C7 1.39 ± 0.83 0.83 ± 0.81 <0.001 1.29 ± 0.76 0.88 ± 0.80 =0.002 CPSQI Global score 10.58 ± 3.36 5.63 ± 2.71 <0.001 10.20 ± 3.20 5.73 ± 2.63 <0.001
aComparisons by t-test. Values are expressed as mean score ±S.D.
Table 3. Correlation Coefficients for test–retest reliability in all subjects and in patients with insomniacs
CPSQI component All subjects N = 208 Insomniacs N = 51
r p r p Sleep quality C1 0.75 <0.001 0.77 <0.001 Sleep latency C2 0.74 <0.001 0.74 <0.001 Sleep duration C3 0.68 <0.001 0.56 =0.001 Sleep efficiency C4 0.60 <0.001 0.23 =0.004 Sleep disturbance C5 0.63 <0.001 0.56 <0.001
Use of sleeping medication C6 0.94 <0.001 0.91 <0.001
Daytime dysfunction C7 0.69 <0.001 0.74 <0.001
CPSQI global score 0.85 <0.001 0.77 <0.001
global-component scores correlations were mod-erate, suggesting acceptable internal homogeneity of the CPSQI. Overall, ‘subjective sleep quality’ was the component most highly correlated with the global score whereas ‘sleep duration’ and ‘sleep
disturbance’ correlated less satisfactorily with the global score, indicating that the global score re-flects sleep quality to a greater degree than other components. These data are interesting because we also found that ‘subjective sleep quality’ as a
Figure 2. Bivariate correlation between CPSQI-subjective sleep quality and visual analogue scale-sleep quality.
Pittsburgh Sleep Quality Index-Sleep Latency (C2)
4.0 3.0 2.0 1.0 0.0 -1.0
Sleep Log-Sleep Onset Latency (minutes)
80 60 40 20 0 -20 r= 0.60, p < 0.001
single-item component and the CPSQI global score significantly correlated with the measure-ment of sleep quality by VAS. Item-to-item cor-relations were low, suggesting that there were few redundancies in the seven components of the scale. Previously researchers have reported substantial test–retest reliability for the PSQI global score over a 2-day interval (r¼ 0.90) and over a mean interval of 45 days (r¼ 0.86) in patients with pri-mary insomnia [11]. Short-interval test–retest reli-ability for all seven components was high but two components (‘subjective sleep quality’ and ‘sleep disturbance’) had very low long-interval test–retest reliability in Backhaus’ study [11]. In this study, the CPSQI global score showed substantial test– retest reliability over a 14–21-day interval with a correlation coefficient of 0.85 for all subjects and 0.77 for primary insomniacs. The test–retest reli-ability of the CPSQI subscores (component scores) in primary insomniacs were moderate to sub-stantial with an exception of the subscore ‘habitual sleep efficiency’ which was very low. This finding pinpoints the variability of ‘sleep efficiency’ as a sleep parameter across time. The fact that ‘sleep efficiency’ is a calculated parameter determined by three other aspects of sleep, namely, total time spent in bed, sleep onset latency, and wake time
after sleep onset can explain the observation that ‘sleep efficiency’ is unstable across time.
Using a contrasting groups approach, we found good construct validity for the CPSQI. The CPSQI global score and subscores could differentiate be-tween primary insomniacs and normal controls as these scores were significantly different between the two contrasting groups. In terms of external validity, the CPSQI global score significantly cor-related with the sleep quality VAS and some sleep parameters (i.e., SOL and SE) derived from the sleep diary in primary insomniacs. However, the strength of these correlations was small. The validity of the scale was further supported by the results that subjective sleep quality, sleep latency, sleep duration, and habitual sleep efficiency sub-scores significantly correlated to corresponding measures obtained by or derived from other instruments.
With regard to the relationship of the CPSQI and measures of daytime sleepiness in primary insomnia patients, validity analyses revealed that neither did SSS nor did CESS significantly cor-relate with the CPSQI global score. This finding is of particular interest because it challenges the notion that primary insomnia patients generally experience excessive daytime sleepiness [19, 20]. Pittsburgh Sleep Quality Index-Sleep Duration (C3)
4.0 3.0 2.0 1.0 0.0 -1.0 Sleep L og-T o tal Sleep T ime (hour s) 10 9 8 7 6 5 4 3 r = -0.64, p < 0.001
Interestingly enough neither did SSS nor did CESS correlate to the daytime dysfunction subscore.
A CPSQI global score of greater than 5 yielded a sensitivity of 98% and a specificity of 55% as a marker for poor sleep in primary insomniacs vs. controls. A CPSQI global score of greater than 6 resulted in a sensitivity of 90% and a specificity of 67%. The diagnostic sensitivity of the CPSQI is very high. However, it has a poor specificity, with 52–70 out of 175 healthy controls were falsely categorized as ‘poor sleepers’. The result of a good diagnostic sensitivity for primary insomniacs in comparison to healthy controls is comparable to those reported by others [11, 21], but the specificity is significantly lower. Similar to our study, the diagnosis of primary insomnia was based on the DSM-IV criteria in Backnahs’ and Doi’s studies [11, 21]. It could be that we employed a stricter procedure for diagnosing primary insomnia and a large proportion of poor sleepers were conse-quently wrongly categorized. Alternatively, our version of the PSQI may be in fact not specific enough as a tool to differentiate healthy controls from primary insomniacs.
One might argue that the respondents of this study might be unrepresentative of the population at large since the non-participation rate was high. Readers should, therefore, exercise caution when drawing any inferences from this study.
Conclusions
This study examined the psychometric properties of the CPSQI in a group of community-dwelling adults with primary insomnia or without. Results suggest that the CPSQI is a psychometrically sound measure of sleep quality and disturbance for community-dwelling adults and can be successfully self-administered to patients with primary insom-nia in community-based research. The overall scale better reflects sleep quality than other aspects of sleep. The CPSQI may not be an effective screen-ing tool for identifyscreen-ing subjects with primary insomnia because it has a low specificity. However, it can be a sensitive, reliable, and valid outcome measurement tool for use with community-based studies in primary insomnia.
References
1. Espie CA. Insomnia: Conceptual issues in the development, persistence, and treatment of sleep disorder in adults. Annu Rev Psychol 2002; 53: 215–243.
2. Ancoli-Israel S, Roth T. Characteristics of insomnia in the United States: Results of the 1991 National Sleep Foun-dation Survey. I. Sleep 1999; 22 (Suppl 2): S347–S353. 3. Li CY, Chen PC, Sung FC, Lin RS. Residential exposure to
power frequency magnetic field and sleep disorders among women in an urban community of northern Taiwan. Sleep 2002; 25: 428–432.
4. Zammit GK, Weiner J, Damato N, Sillup GP, McMillan CA. Quality of life in people with insomnia. Sleep 1999; 22 (Suppl 2): S379–85.
5. Leger D, Scheuermaier K, Philip P, Paillard M, Guille-minault C. SF-36: Evaluation of quality of life in severe and mild insomniacs compared with good sleepers. Psychosom Med 2001; 63: 49–55.
6 Morin CM, Hauri PJ, Espie CA, Spielman AJ, Buysse DJ, Bootzin RR. Nonpharmacologic treatment of chronic insomnia. An American Academy of Sleep Medicine review. Sleep 1999; 22: 1134–1156.
7. Smith MT, Perlis ML, Park A, et al. Comparative meta-analysis of pharmacotherapy and behavior therapy for persistent insomnia. Am J Psychiatry 2002; 159: 5–11. 8. Buysse DJ, Reynolds CF, III, Monk TH, Berman SR,
Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res 1989; 28: 193–213.
9. Buysse DJ, Reynolds CF, III, Monk TH, Hoch CC, Yeager AL, Kupfer DJ. Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI). Sleep 1991; 14: 331–338.
10. Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res 1998; 45: 5–13.
11. Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test–retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res 2002; 53: 737–740.
12. American Psychology Association. Diagnosis and Statisti-cal Manual of Mental Disorders, 4th edn. Washington, D. C.: American Psychiatric Association, 1994: 551–607. 13. Cheng TA, Williams P. The design and development of a
screening questionnaire (CHQ) for use in community studies of mental disorders in Taiwan. Psychol Med 1986; 16: 415–422.
14. Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998; 59 (Suppl 20): 22–33.
15. Taiwanese Society of Psychiatry, The Mini International Neuropsychiatric Interview (MINI) Taiwan version 2.0.0, Taipei, Taiwan: Taiwanese Society of Psychiatry, 2001. 16. Cheng TA, Wu JT, Chong MY, Williams P. Internal
con-sistency and factor structure of the Chinese Health Ques-tionnaire. Acta Psychiatr Scand 1990; 82: 304–308.
17. Chen NH, Johns MW, Li HY, et al. Validation of a Chi-nese version of the Epworth sleepiness scale. Qual Life Res 2002; 11: 817–821.
18. Hoddes E, Zarcone V, Smythe H, Phillips R, Dement WC. Quantification of sleepiness: A new approach. Psycho-physiology 1973; 10: 431–436.
19. Rosenthal LD, Meixner RM. Psychological status and levels of sleepiness-alertness among patients with insomnia. CNS Spectr 2003; 8: 114–118.
20. Roth T, Roehrs T. Insomnia: Epidemiology, characteris-tics, and consequences. Clin Cornerstone 2003; 5: 5–15.
21. Doi Y, Minowa M, Uchiyama M, et al. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res 2000; 97: 165–172.
Address for correspondence: Pei-Shan Tsai, College of Nursing, Taipei Medical University, 250 Wu Hsing Street, Taipei 110, Taiwan