Spine
Posterior epidural migration of lumbar disk fragments:
report of two cases and review of the literature
Abad Cherif El Asri, MD
⁎
, Okacha Naama, MD, Ali Akhaddar, MD, Miloudi Gazzaz, MD,
Adil Belhachmi, MD, Brahim El Mostarchid, MD, Mohamed Boucetta, MD
Department of Neurosurgery, Mohamed V Military Hospital, Hay Riyad 10106, Rabat, MoroccoReceived 17 April 2007; accepted 11 June 2007
Abstract Background: Posterior epidural migration of an extruded disk fragment is rare, and posterior migration of the free fragments causing cauda equina syndrome is exceptionally rare. The disk frag-ment must transgress through numerous anatomical restraints including the nerve roots in such cases. Methods: Two cases of migration of the sequestrated disk into the posterior epidural space are presented. The first patient complained, over the course of 1 month, of paresthesias and weakness of the lower limbs, with urinary retention. However, in the other case, there was steppage gait and strength score of 3/5 on dorsiflexion of left foot, without bladder or bowel disturbance.
Results: Lumbar CT scan with sagittal reconstruction showed a posterior epidural mass, which was isodense to the disk. The preoperative differential diagnosis included epidural abscess, hematoma, and neoplasm. An urgent decompressive lumbar laminectomy was performed. At surgery, the lesion proved to be a massive extruded disk fragment.
Conclusion: Diagnosis of posterior epidural migration of the sequestrated disks may be difficult. It may present with subtle clinical features. Magnetic resonance images may mimic those of other more common posterior epidural lesions. Early surgery should be the first choice to prevent severe neurologic deficits. © 2008 Elsevier Inc. All rights reserved.
Keywords: Posterior epidural disk fragment; Cauda equina syndrome; Magnetic resonance imaging
1. Introduction
Some degree of disk fragment migration occurs in 35% to 72% of lumbar disk herniations [1,6,13]. Posterior epidural migration is an interesting but rare path taken by a prolapsed intervertebral disk fragment[7]. We report 2 such cases and review the literature on the posterior migration of the sequestrated disk fragments (Table 1).
2. Case 1
A 42-year-old man presented with 3 years' history of intermittent lumbago. Since 1 month ago, he experienced a
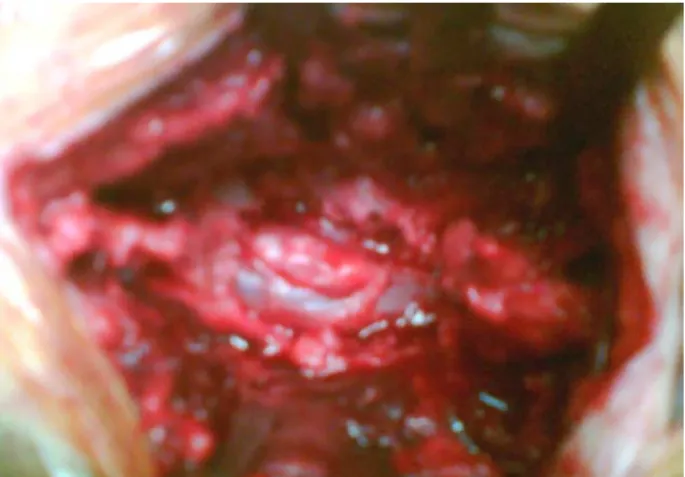
progressive left-sided radiculopathy. There were no bladder or bowel symptoms. Clinical examination revealed steppage gait and a strength score of 3/5 on dorsiflexion of left foot, with hypoesthesia of lateral side of the left limb. There was some ill-defined tenderness on palpation of the lower lumbosacral spine. Plain radiographs of the lumbar sacral spine were essentially normal. Lumbar CT scan with sagittal reconstruction showed extensive lateral disk herniation at L5-S1, with an isodense mass level located in the posterior epidural space on the left side (Fig. 1).
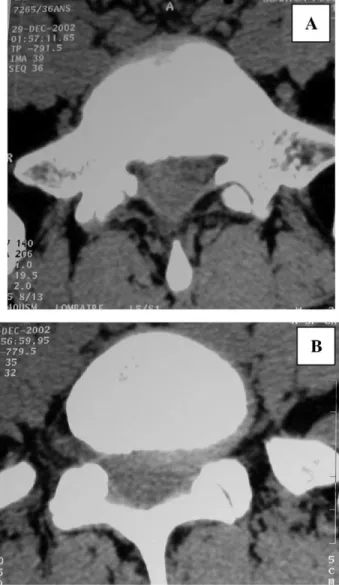
An L5 laminectomy was performed. After removal of the ligamentum flavum, the extruded disk fragment embedded in fibrous epidural tissue was readily visible posterior and lateral to the thecal sac. The fragment clearly compressed and was adherent to the thecal sac. It was dorsal to the S1 nerve root from the axilla (Fig. 2). The fragment was removed. The L5-S1 interspace was explored on the left side. Rupture at the posterior longitudinal ligament (PLL) was
Available online at www.sciencedirect.com
Surgical Neurology 70 (2008) 668–671
www.surgicalneurology-online.com
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging.
⁎ Corresponding author. Tel.: +212 612 47544. E-mail address:abad20031@hotmail.com(A.C. El Asri).
0090-3019/$– see front matter © 2008 Elsevier Inc. All rights reserved. doi:10.1016/j.surneu.2007.06.034
detected, and an L5-S1 diskectomy was performed. Inspec-tion of the dura showed no dural rent. Histopathology confirmed the posterior epidural fragments to be the intervertebral disk. The patient was completely relieved of his leg pain, with persistence of discrete dorsiflexion deficit on left foot, when he was seen in the outpatient clinic tow months later.
3. Case 2
A 36-year-old man developed, after lifting a heavy load, intermittent acute lumbago. The pain radiated down to the lateral side of bilateral leg. In the course of 1 month, he complained of paresthesias and weakness of the lower limbs and urinary retention. Physical examination revealed a strength score of 2/5 on dorsiflexion of left and right feet. Reflexes were decreased at the knee and absent at the ankle with anesthesia on saddle.
Plain radiograph films of the lumbar spine showed collapse of the L5-S1 intervertebral disk. Lumbar spine CT scan demonstrated a mass that was located posteriorly and laterally to the left aspect of the dural sac at L5-S1. The lesion was isodense to the lumbar disk, and there was continuity of the fragment with the L5-S1 disk space, which presented extensive lateral disk herniation (Fig. 3).
An urgent decompressive lumbar L5 laminectomy was performed. After removal of the ligamentum flavum, the extruded disk fragment was readily visible posterior and lateral to the thecal sac. The extirpated tissue had a yellowish appearance and a fibrotic consistency, with
Table 1
Summary of reported cases of posterior epidural migration of lumbar disk fragments
Author/s, year (reference) No. of cases Level of herniation Clinical symptoms Lichtor[8], 1989 1 L2-L3 Radicular Lutz[9], 1990 1 L4-L5 Radicular
Sekerci et al[14], 1992 1 L3-L4 Cauda equina syndrome Sakas et al[11], 1995 1 L4-L5 Radicular
Bonaroti and Welch[1], 1998
1 L2-L3 Cauda equina syndrome Saruhashi et al[12], 1999 1 L5-S1 Radicular
Robe et al[10], 1999 2 L3-L4 Radicular L3-L4 Radicular
Dosoglu et al[3], 2001 1 L3-L4 Cauda equina syndrome Eysel and Herbsthofer[5],
2001
3 L3-L4 Cauda equina syndrome L4-L5 Radicular
L3-L4 Acute lumbago Kuzeyli et al[6], 2003 3 L4-L5 Acute lumbago
L1-L2 Cauda equina syndrome L2-L3 Cauda equina syndrome Lakshmanan et al[7],
2006
2 L4-L5 Radicular L4-L5 Radicular
Tatli et al[15], 2005 2 L3-L4 Cauda equina syndrome L5-S1 Cauda equina syndrome Chen et al[2], 2006 1 L2-L3 Radicular
Present case 2 L4-L5 Cauda equina syndrome L4-L5 Radicular
Fig. 1. Lumbar CT scan in the first case. A: Disk material appears posterior to dural sac and isodense to the intervertebral disk. B: Sagittal reconstruction showed collapse of the L5-S1 intervertebral disk and posterior isodense mass.
Fig. 2. Preoperative view of the dural sac after L5 laminectomy showed extracted disk fragment with yellowish appearance and attachment to the posterior dural sac.
669 A.C. El Asri et al. / Surgical Neurology 70 (2008) 668–671
attachment to the dura. It was dorsal to the L5 nerve root and had continuity through the axilla of the S1 nerve root component anteriorly. The L5-S1 interspace was explored on the left side. A rent in the PLL was observed, and an L5-S1 diskectomy was performed. Inspection of the dura showed no dural rent. The pathologic examination con-firmed that the specimen was an intervertebral disk. Postoperatively, his lower extremity weakness gradually recovered over a period of 1 year. His symptom of urinary retention required intermittent self-catheterization.
4. Discussion
Sequestered disk fragments account for 28.6% of all disk herniations[6]. It most often migrates in the anterior epidural space. Rostral, caudal, and lateral migration are the most clinically important modes of this migration [1,4,6,13]. Occasionally, sequestered disk fragments may migrate to the
posterior epidural space of the dural sac[1-12,14,15]. This condition is rare, and posterior migration of the free fragments causing cauda equina syndrome is exceptionally rare [1,3,5-7,14,15]. Disk fragment migration patterns are generally limited by the attachments of the PLL and its associated “midline septum” and “peridural” or “lateral membrane” and the nerve root itself[1-3,6,7,13]. A problem with any one of these barriers may facilitate posterior migration of disk fragments, which may be greater when the angle formed by the nerve root and the dural sac is obtuse at the site where the root exits and when the disk space is cranial or caudal to the intervertebral foramen. In this condition, the nerve root is not in its supportive position as a potential key anatomical barrier to posterior migration of disk material[6].
Most symptomatic lumbar disk herniations are noted to be in a lateral position, with resultant nerve root irritation. The posterior migration of the disk may be expected to present clinically with isolated acute or chronic lumbago to significant neurologic symptoms, and to the extent of presenting as cauda equina compression [1]. In the first observation, the patient had a history of intermittent lumbago, and preoperatively, the fragment was embedded by fibrosis tissue. This suggests that the fragment had already migrated, and this was decompensated by disk herniation in the same level to the epidural posterior fragment or in the cranial or rostral interspace. However, this posterior migration of the disk can be alarming, such as in the second observation and in most cases reported in literature, when the clinical condition is serious and acute [1-12,14,15].
Definite diagnosis of posteriorly located disk fragments is difficult because the radiologic images of disk fragments may mimic those of other more common posterior epidural lesions. Magnetic resonance imaging, with gadolinium administration, is considered the method of choice for diagnosis by most authors [2]; this was not used for diagnosis in our patients, who were explored by simple CT scan. However, in the literature, MRI of sequestrated disk fragments is well distinguished. It show fragments as a posterior epidural mass compressing the dural sac; usually, they are hypointense on T1-weighted images, and 80% are hyperintense on T2-weighted images[2,6,13]. The epidural fat is vascular; the presence of a fragment in this space will induce an inflammatory response with granulation tissue and neovascularization around the extruded tissue, causing a ring enhancement with gadolinium in the MRI scan[7]. This may aid in the preoperative diagnosis of such rare disk migration into the posterior epidural space. This enhancement can make differential diagnosis to other common epidural lesions such as neoplasia, abscess, and hematoma [1-12,14,15]. Rare lesions, such as synovial cyst from the facet joint, pigmented villonodular synovitis, or hypertrophic ligamen-tum flavum, may be evocated[7]. Saruhashi et al[12]have reported a disk fragment located at the dorsal epidural space and extending to the interspace foramen, which simulated a
Fig. 3. Lumbar CT scan in the second case showed left lateral herniated disk at L5-S1 (A) and posteriorly located mass, which appears isodense to the intervertebral disk (B).
dumbbell tumor. However, extradural fibrosis is a well-recognized finding in cases of acute lumbar disk herniation and is considered to be an important indicator of possible disk fragment sequestration[6].
As in our patients, lumbar CT scan with sagittal reconstruction can show some direct or indirect sign of this rarity; the fragment appears to have the same density as the intervertebral disk, which was collapsed, and the presumed disk space of origin could not be identified on preoperative imaging. The finding on CT scan is inconclusive because of its limitation in recognizing the extradural migrated fragment as a mass compressing the dural sac[2]. Interestingly, it may be useful in emergency, but with less sensibility and specificity than MRI.
Treatment consisted of removal of the extracted fragment through hemi- or complete laminectomy. Early surgery should be the first choice to prevent severe neurologic deficits such as cauda equina syndrome[6,7].
References
[1] Bonaroti EA, Welch WC. Posterior epidural migration of an extruded lumbar disc fragment causing cauda equina syndrome. Spine 1998;23: 378-81.
[2] Chen CY, Chuang YL, Yao MS, Chiu WT, Chen CL, Chan WP. Posterior epidural migration of sequestrated lumbar disk fragment: MR imaging findings. AJNR Am J Neuroradiol 2006;27(7):1592-4. [3] Dosoglu M, Is M, Gezen F, Ziyal MI. Posterior epidural migration
of a lumbar disc fragment causing cauda equina syndrome: case report and review of the relevant literature. Eur Spine J 2001;10(4): 348-51.
[4] Ebeling U, Reulen HJ. Are there typical localisations of lumbar disc herniations? A prospective study. Acta Neurochir 1992;117: 143-8.
[5] Eysel P, Herbsthofer B. Dorsal compression of the epidural cord due to the free sequestral lumbar prolapse: diagnostic problems in magnetic resonance imaging and computed tomography. Arch Orthop Trauma Surg 2001;121:238-40.
[6] Kuzeyli K, Akýr E, Usul H, Baykal S, Yazar U, Karaarslan G, Arslan E, Peksoylu B. Posterior epidural migration of lumbar disc fragments: report of three cases. Spine 2003;28:64-7.
[7] Lakshmanan P, Ahuja S, Lyons K, Howes J, Davies PR. Sequestrated lumbar intervertebral disc in the posterior epidural space: a report on two cases and review of the literature. Spine J 2006;6:583-6. [8] Lichtor T. Posterior epidural migration of extruded lumbar disk.
Surg Neurol 1989;32:311-2.
[9] Lutz JD. CT myelography of a fragment of a lumbar disk seques-trated posterior to the thecal sac. AJNR Am J Neuroradiol 1990;11: 610-1.
[10] Robe P, Didier M, Jacques L, Achille S. Posterior epidural migration of sequestrated lumbar disc fragments. J Neurosurg (Spine 2) 1999;90: 264-6.
[11] Sakas DE, Farrell MA, Young S, Toland J. Posterior thecal lumbar disc herniation mimicking synovial cyst. Neuroradiology 1995;37:192-4. [12] Saruhashi Y, Omura K, Miyamoto K, Katsuura A, Hukuda S.
A migrated lumbar disc herniation simulating a dumbbell tumor. J Spinal Disord 1999;12:307-9.
[13] Schellinger D, Manz H, Vidu B. Disk fragment migration. Radiology 1990;175:831-6.
[14] Sekerci Z, Ildan F, Yuksel M, Gul B, Kilic C. Cauda equina compression due to posterior epidural migration of extruded lumbar disc. Neurosurg Rev 1992;15:311-3.
[15] Tatli M, Guzel A, Ceviz A, Karadag O. Posterior epidural migration of sequestered lumbar disc fragment causing cauda equina syndrome. Br J Neurosurg 2005;19:257-9.
Commentary
Posterior migration of a lumbar herniated disk fragment is rare, as the authors of this article point out. The exact mechanism whereby such a migration occurs is unclear, however, and the authors do not resolve this conundrum. Nevertheless, the report serves to remind the spine surgeon that when hoofbeats are heard, occasionally, one must think of zebras, even when out of Africa.
Ron Pawl, MD Department of Neurosurgery University of Illinois, Chicago Lake Forest Hospital Chicago, IL 60045, USA
671 A.C. El Asri et al. / Surgical Neurology 70 (2008) 668–671