1 Case Report
Early Rehabilitation of Temporomandibular Joint Ankylosis after Interpositional Arthroplasty
顳頜關節僵直病人於內置式關節整形術術後立即的復健治療
Yu-Liang Lai1, Li-Wei Chou1,2,3, Chen-Yi Wu1, Edward C Ko4, Yu-Chun Liu1,5, Mu-Jung Kao6,7
賴宇亮1, 周立偉1,2,3, 吳貞儀1, 柯政全4, 劉郁君1,5, 高木榮6,7
1
Department of Physical Medicine and Rehabilitation, China Medical University Hospital, Taichung, Taiwan, 2School of Chinese Medicine, College of Chinese Medicine, China Medical University, Taichung, Taiwan, 3Department of Physical Therapy, China Medical University, Taichung, Taiwan, 4Department of Oral and Maxillofacial Surgery, China Medical University Hospital, Taichung, Taiwan, 5Graduate Institute of Rehabilitation Counseling,
National Changhua University of Education, Changhua, Taiwan, 6Department of Physical Medicine and Rehabilitation, Taipei City Hospital, Taipei, Taiwan, 7Institute of Rehabilitation Science and Technology, Yang Ming University, Taipei, Taiwan.
1
中國醫藥大學附設醫院復健部, 2中國醫藥大學中醫學院中醫學系, 3中國醫藥大學物理
治療學系, 4中國醫藥大學附設醫院口腔顏面外科部, 5國立彰化師範大學復健諮商研究所,
6台北市立聯合醫院復健科,7國立陽明大學復健科技輔具研究所
Running title: Rehabilitation after Interpositional arthroplasty
Address: No. 105, Yu-sheng St., Shilin District, Taipei City 111, Taiwan, ROC. 台北市士林區雨聲街 105 號
TEL: 886-2-28389187 Fax: 886-2-28389513
3 Abstract
Early Rehabilitation of Temporomandibular Joint Ankylosis after Interpositional Arthroplasty
Spastic hypertonia, which is a component of upper motor neuron lesion, is not uncommon sequela after cerebrovascular accident (CVA). Though a satisfactory mouth opening in patient with temporomandibular joint ankylosis can be achieved by some surgery methods, the data of rehabilitation right after Lai's interpositional arthroplasty operation is still pending. We report a case of spastic hypertonia leading to severe trismus after brain stem stroke, successfully treated with early rehabilitation of temporomandibular joint ankylosis right after Lai's interpositional arthroplasty. The maximal dimension of mouth opening of 38mm was measured at the 6 months followed-up. Furthermore, the ankylosis disappeared after one year of follow-up. Early active rehabilitation achieved good functional outcome.
中文摘要 顳頜關節僵直病人於內置式關節整形術術後立即的復健治療 高張性痙攣是上運動神經元病變的一種表現,且是腦血管病變(或中風) 後常見的 後遺症。雖然透過一些已知的手術方法,可以使得顳頜關節僵直病人其張口程度獲得改 善,但是關於新的賴氏內置式關節整形術 (Lai's interpositional arthroplasty operation) 術 後立即的復健與成效研究資料尚仍缺如。我們報告一例腦幹中風後病患,因高張性痙攣 導致牙關緊閉,於賴氏內置式關節整形術術後立即的復健治療後,成功地治癒顳頜關節 僵直。在六個月的追蹤治療後,測量到 38 毫米的最大張口距離。 而且,於一年的追 蹤治療後,完全成功地治癒顳頜關節僵直。賴氏內置式關節整形術術後早期立即的復健 治療,在顳頜關節僵直治療上證實可以獲得良好的療效。 關鍵字: 復健,語言治療,中風,顳頜關節僵直
5 Introduction
Temporo-mandibular joint (TMJ) ankylosis is a common cause of acquired mandibular deformity due to spastic hypertonia. Spastic hypertonia is not uncommon sequela after cerebrovascular accident (CVA), which is a component of upper motor neuron lesion. Management of spastic hypertonia may involve the use of centrally acting agents, peripheral blockade, and ablative therapies [1]. The inability to open the mouth fully is the most serious threat to these individuals. Clinically TMJ ankylosis can lead to facial asymmetry, difficulties in mastication, speech impairment and poor oral hygiene [2]. Trismus in these patients can be managed by condylectomy or gap arthroplasty or by costochondral graft interposition [3]. Though a satisfactory mouth opening can be achieved with some surgery methods [4-6], the data of rehabilitation right after Lai's interpositional arthroplasty operation is still pending. Presented is a TMJ patient who demonstrated a favorable outcome and functional independence by early rehabilitation programs intervention right after the Lai's interpositional arthroplasty approach.
Case Report
A 60-year-old man is a patient of diabetes mellitus, hypertension under regular medicine control. He had been suffered poliomyelitis at childhood with right leg atrophy and contracture. About eight months prior to this hospitalization, an episode of brain stem infarct led to bilateral limbs weakness. He was then referred to our center for physical training due to bilateral limbs weakness and difficulties in both swallowing and communication. Physical examinations showed that the motor status of bilateral limbs were both Brunnstorm stage IV. The muscle powers of upper and lower limbs were about good and fair grade separately.
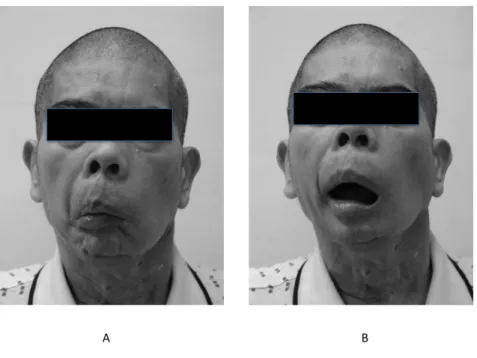
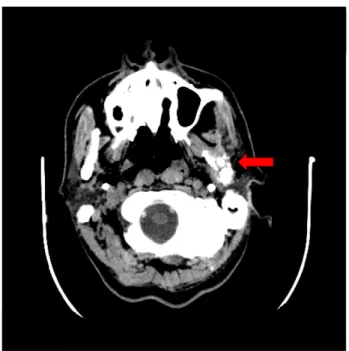
Severe trismus, however, was noted while transferring from intensive care unit to general ward, about 7 months prior to this hospitalization. Tracheostomy and naso-gastric tube implantation were performed for air way hygiene and feeding at ICU. At that time, no spasm of master, temporalis and scaclavicalmaster muscles was noted. The distance between his incisors was measured of 0 mm. The brain computer tomography (CT) image showed bony ankylosis of left side TMJ (Figure 1).
We arranged the electrodiagnostic study of bilateral master and pterygoid muscle as well to rule out the possible central problems. Flaccid dysarthria and dysphagia were initially impressed. During the period, he received simultaneously both facial sensation stimulation for poor light touch and sensation, and oral-facial muscle massage for muscle weakness.
Due to the poor muscle relaxation response (Figure 2-A), we arranged the Lai's interpositional TMJ arthroplasty with intraoral approach [4] under the Oral Maxillofacial surgery doctor’s suggestion. The Lai's arthroplasty started with intraoral incision placed over the buccal shelf. Then reflection of the soft tissue off the
7
mandibular ramus was done. Coronoidectomy was performed and arthroplasty was accomplished at the level of condylar neck. Finally the coronoid process was fixed with stainless steel wire and the wound was closed [4-6]. The interpositional material is his buccal fat pad.
After the operation, the rehabilitation programs of respiratory training (abdominal- breathing exercise, pushing exercise, and holding breath), the corking training to the side-hole tracheostoma set, speech therapy and swallowing training were performed.
Lai's interpositional TMJ arthroplasty increased the opening to 30mm (Figure 2-B), measured at the incisor edge, however, the oral-motor and swallowing evaluation showed few movement of oral-facial muscle with poor tongue motion. Furthermore, the poor cough ability with drooling, delayed in trigger pharyngeal phase, decreased pharyngeal wall contracture and laryngeal elevation were impressed. Therefore early mandibular movement was encouraged and speech therapy was initiated right after the surgery. Two days after operation, he could mildly open the mouth a little bit only. It was improved gradually with the speech therapy later. Successfully reached was the goal to open the mouth gradually.
Then he started the rehabilitation programs of respiratory training (abdominal- breathing exercise, pushing exercise, and holding breath) and the corking training to the side-hole tracheostoma set. We successfully remove the tracheostoma set and closed the hole at the twenty-seventh day post the operation. The programs of speech therapy and swallowing training including the Deep Pharyngeal Neuromuscular Stimulation (DPNS), tongue’s movement, stimulus of the vocastim-master muscles and oral muscle exercise were performed. Caregivers were asked also to stretched the TMI daily. The followed CT revealed bilateral normal zygomatic arch of temporomandibular joint without any
sign of recurrence just one month after operation (Figure 3).
Three months thereafter, he could speak in fluent sentences, spontaneously open his mouth and cough out sputum during the followed-up period though the percutaneous endoscopic gastrostomy (PEG) was performed due to his poor swallowing ability.
9 Discussions
TMJ ankylosis is a pathological condition which generally follows the damage to the joint, of a traumatic or infective nature. Trauma, rheumatoid arthritis, irradiation, soft tissue and bone tumors are some other causes [7]. The symptoms of ankylosis are progressive trismus and mandibular deformity with retrognathia and lateral displacement of the chin. Inability to fully open the mouth can compromise the adequate calorie intake, speech rehabilitation and oral hygiene care.
Trismus in these patients can be managed by condylectomy or gap arthroplasty or by constochondral graft interposition. In surgical treatment of TMJ ankylosis, the main goals are resection of ankylosed bone, restoration of function and prevention of recurrence [8]. Ostectomy alone gives rise to a gap between the articular cavity and the mandibular ramus, which shortens the mandibular ramus and leads to the possible pseudo-articulation regeneration. It seems, however, to increase the risk of recurrence [9]. The long-term physiotherapy is critical and necessary to acquire satisfactory results but the operation. The physical therapy greatly contributes to improved function of the secondary TMJ, particularly after trauma [10]. This case report stands for the result as well.
Since the condylar regeneration is well controlled by good oral function, the lateral pterygoid muscle is a key element. The better functional outcome of TMJ without any ankylosis depends on the quality of early active rehabilitation directly [11].
So far limited experience of physiotherapy intervention post operation by intraoral approach was reported. This case report, however, presented the patient with ankylosis could fully open and reach his mouth to 38 mm spontaneously after 6 months of physiotherapy. Successfully confirmed are the good functional recovery of the joint and
the restored vertical dimension of the mandibular ramus by clinical and instrumental tests.
In conclusion, we corrected the trismus in a patient with TMJ dyskinesia after the brain stem stroke and he can spontaneously open and close the mouth. Furthermore, he can speak fluently after rehabilitation. The improved outcome with the independent oral function was required. Patient was treated with the operation of oronoidectomy and interpositional arhtroplasty. The intensive and aggressive physiotherapy right after the operation is essential to maintain optimal muscle length over time while persuing the goal of the improved range of motion and preventing relapse.
11 References
1. Vivek K, Albert CC, Michael E, et al. Severe trismus as a complication of cerebrovascular accident: A case report. Arch Phys Med Rehabil. 2005; 86: 594-95
2. Zins JE, Smith JD, James DR. Surgical correction of temporomandibular joint ankylosis. Clin. Plast. Surg. 1989; 16: 725-32
3. Politis C, Fossion E, Bossuyt M. The use of costochondral grafts in arthroplasty of the temporomandibular joint. J Craniomaxillofac Surg. 1987; 15: 345-54
4. Ko E, Chen M, Huang E, et al. Lai’s arthroplasty for TMJ ankylosis with intraoral approach. Int J Oral Maxillofac Surg. 2005; 34: supp (1): 1
5. Ko E, Hsu M, Huang E, et al. Intraoral approach arthroplasty of Temporomandibular joint. Taiwan J Oral Maxillofac Surg . 2001; 12(2): 100-10 6. E. C. Ko, M. Y. Chen, M. Hsu1, et al. Intraoral approach for arthroplasty for
correction of TMJ ankylosis. Int J Oral Maxillofac Surg. 2009; 8: 1256–62 7. Jacobs JS, Bessette R: Temporomandibular joint deformities, in Smith JW, Aston
SJ , Grabb and Smith's Plastic Surgery (4th ed). Boston: Little Brown & Commpany, 1991; 247-70
8. Karaca C, Barutcu A, Baytekin C, et al. Modifications of the inverted T-shaped silicone implant for treatment of temporomandibular joint ankylosis. J Craniomaxillofac Surg. 2004; 32: 243-6
9. Manganello-Souza LC, Mariani PB. Temporomandibular joint ankylosis: report of 14 cases. Int J Oral Maxillofac Surg. 2003; 32: 24-9
in children. Acta Chir Plast. 1998; 40: 97-104
11. Lemiere E, Sicre A, Vereecke F, et al. Our physiotherapy treatment of articular fractures of the mandibular condyle. Rev Stomatol Chir Maxillofac. 2003; 104: 104-6
13 Figures legends:
Figure 1. Pre-operation CT image: The brain computer tomography (CT) image showed bony ankylosis (arrow) of left side TMJ
Figure 2. A. The patient could not open his mouth spontaneously before operation. B. The increasing mouth opening was achieved gradually after operation.
15
Figure 3. Post-operation CT image: The followed CT revealed bilateral normal zygomatic arch of temporomandibular joint without evidence of recurrence one (arrow) month after operation