Hypoalbuminemia in drug-free patients with major depressive
disorder compared with a dietary matched control group:
a clinical meaning beyond malnutrition
Shih-Yi Huang
a, Chih-Chiang Chiu
a,b, Winston W. Shen
c, Hui-Chih Chang
d,
Po-Lun Wu
e, Kuan-Pin Su
e,*
a
Graduate Institute of Nutrition and Health Sciences, Taipei Medical University, Taiwan
b
Laboratory of Biological Psychiatry, Taipei City Psychiatric Center, Taiwan
c
Department of Psychiatry, Taipei Medical University-Wan Fang Medical Center, Taiwan
d
School of Health Care Administration, Taipei Medical University, Taiwan
e
Department of General Psychiatry, China Medical University Hospital, No. 2, Yuh-Der Road, Taichung 404, Taiwan Received 5 May 2004; received in revised form 27 October 2004; accepted 27 October 2004
Abstract
Serum albumin (sALB) is routinely determined in blood tests and is an excellent predictor of risk for many medical illnesses. Hypoalbuminemia has been sporadically reported in patients with psychiatric disorders, such as major depressive disorder and schizophrenia. We compared sALB levels between 19 drug-free patients of major depressive disorder with a control group of matching diets. We conducted this study by controlling the nutrition factor by assessing patient’s diets, as well as other possible confounding factors such as sex, age, body mass index (BMI), liver function, and exercise, while focusing on hypoalbuminemia in patients with major depressive disorder. There is no difference in age, gender distribution, and dietary frequency on protein and albumin intake between the patient and control group. The sALB levels of the group with major depressive disorder were significantly reduced ( p=0.049). The severity of depression is negatively correlated to the sALB level (r= 0.46, p=0.04). Hypoalbuminemia has clinical meanings on severity of depression and is independent of malnutrition. However, our results can only be seen as very preliminary and should be confirmed by larger studies.
D 2004 Elsevier B.V. and ECNP. All rights reserved.
Keywords: Hypoalbuminemia; Major depressive disorder; Drug-free patients
1. Introduction
Serum albumin (sALB) is routinely determined in blood tests and is an excellent predictor of risk or prognosis in different clinical settings. In Blackburn’s classic study, sALB was reported to have important prognostic value in hospitalized patients (Harvey et al., 1981).Herrmann et al.
(1992)recorded sALB concentrations from 15,511 patients
with either medical or surgical diseases, and found that
patients with hypoalbuminaemia had higher mortality, longer hospital stay, and were more likely to be readmitted after discharge. Interestingly, sALB has also been found to be a prognostic factor in healthy population.Phillips et al. (1989)
followed 7736 healthy individuals for 9 years, and found that sALB levels below 4 g/dL was an independent prognostic factor for all kinds of deaths, increasing its risk by sixfold.
Hypoalbuminaemia has been sporadically reported in patients with psychiatric disorders. Serum albumin is significantly lower in patients with major depressive
disorder than in healthy volunteers (Maes et al., 1999;
Van Hunsel et al., 1996; Gendall et al., 1999a). Male
patients with schizophrenia had significantly lower levels of
0924-977X/$ - see front matterD 2004 Elsevier B.V. and ECNP. All rights reserved. doi:10.1016/j.euroneuro.2004.10.003
* Corresponding author. Tel.: +886 4 22062121x5076; fax: +886 4 22361230.
E-mail address: cobol@www.cmuh.org.tw (K.-P. Su).
European Neuropsychopharmacology 15 (2005) 227 – 230
plasma albumin compared to age- and sex-matched healthy volunteers (Yao et al., 2000). Due to the retrospective nature of this analysis and the lack of dietary assessment, it is difficult to interpret these findings.
Does hypoalbuminaemia merely result from malnutri-tion, which is the common consequence for physical and mental disorders? The natural association between hypo-albuminaemia and malnutrition apparently gives an over-simplified answer to the complex question of causality. For example, sALB remains unchanged in patients with anorexia nervosa, the extreme form of malnutrition (Smith et al., 1996). Furthermore, nutritional support often fails to
improve sALB levels (Gray and Meguid, 1990). We
hypothesize that hypoalbuminaemia has further clinical meanings beyond malnutrition. Therefore, we conducted this study by controlling the nutrition factor through food diaries that the patients fill out, as well as other possible confounding factors such as sex, age, BMI, and exercise, while focusing on hypoalbuminaemia in patients with major depressive disorder.
2. Methods
Participating subjects were outpatients with age ranging from 18 to 60 years, who were referred by the University-affiliated Hospital. Those who enrolled in the study met the following criteria: (1) diagnosis of DSM-IV for major depressive disorder, (2) ratings of 17 or greater on the 21-item Hamilton Rating Scale for Depression (HRSD), (3) physically healthy on the comprehensive evaluations from medical history, physical examination and laboratory tests, (4) free from any medication for at least 4 weeks, and (5) comprehend the full explanation of the study and give written informed consent.
Exclusion criteria for patients were: (1) a recent or past history of other axis-I diagnoses besides major depressive disorder, including psychotic disorders; organic mental disorders; impulse control disorders; substance use disorder or substance abuse (in the last 6 months prior to the study); primary anxiety disorders, including post-traumatic stress disorder and panic disorder; and bipolar disorders; (2) axis-II diagnoses, i.e. borderline and antisocial personality disorder; (3) a notable medical comorbidity, known or suspected pregnancy; and (4) acute suicidal ideation and attempt were noted that close monitoring such as hospital-ization is necessary. This research proceeded after obtaining approval from the human subject committee of Taipei Medical University-Wan Fang Medical Center.
After obtaining written informed consent, the patients and controls provided blood samples between the hours of 0830 and 0930 following an overnight fasting. Serum albumin levels were determined in the clinical biochemistry labora-tory of Medical University Hospital. The well-trained interviewers with good inter-rater validity then collected frequency records, 24-h dietary recalls and 3-consecutive day
food diaries. Each subject completed dietary assessments consisting of 24-h dietary recall and 3-consecutive day food diaries that consist of 2 weekdays and 1 day in the weekend. The food frequency questionnaire has been validated for many nutrients. Usual dietary intake was assessed by a modified, semi-quantitative, 86-item food frequency
ques-tionnaire (Rimm et al., 1992). The questionnaire was
completed during the visit. The questionnaire instructed subjects to note the frequency of consumption of individual foods, with the assumption of a standard portion size, which is provided on the questionnaire for guidance. The ques-tionnaire included questions about the patient’s history in relation to smoking, drinking, exercise and use of dietary supplements (such as vitamin, mineral and herbal products). Dietary data were collected and analyzed with the Nutrition Data System software; nutrient analysis was conducted with the Academia Sinica Database (Version 1.01, Academia Sinica, 1994, Taiwan).
Food diaries consisted of a listing of each item consumed, with information on the location where the food was consumed, and the frequency of consumption. A maximum of seven potential eating occasions were identified per day (three meals and two snacks). For foods consumed in the home, patients provided detailed information on the prepa-ration method, including individual ingredients for home made dishes, as well as identifying those who consumed the food. For foods consumed outside the home, patients gave a detailed description of the location. To reduce the burden for those who completed diaries for the entire household, amounts of foods consumed were not recorded. Instead, an average weight (grams) of a given food item was calculated per eating occasion for a person of that age and gender based on data from the 1993–1996 Nutrition and Health Survey in Taiwan (NAHSIT). For foods prepared at home, information on ingredients and preparation methods was applied to standard recipes, and the amounts consumed were computed as percentages of the final dish.
Data were analyzed by the Statistical Package for Social Sciences, Version 9.0 (SPSS, Chicago, USA). The Mann– Whitney test compared serum albumin levels, age, BMI, exercise, and frequency of protein intake in 24-h dietary recall and 3-consecutive day food diaries between depressed patients and controls. Among patients with major depressive disorder, Pearson’s correlations were used to examine the relationship of continuous variables of the clinical features of HRSD to each sALB.
3. Results
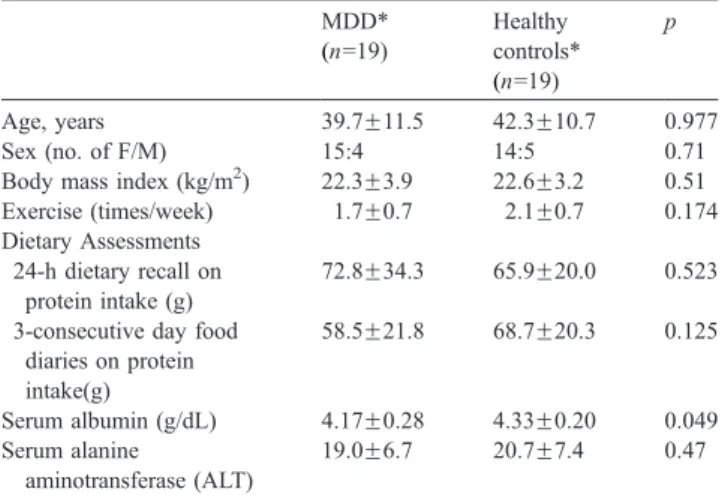
The participating subjects included 19 (4 male and 15 female) depressive patients with a mean age of 39.7F11.5 (S.D.) years, and 19 (5 male and 14 female) healthy controls with mean age of 42.3F10.7 (S.D.) years. The body mass index in patients and controls were 22.3F3.9 (S.D.) and 22.6F3.2 (S.D.), respectively.Table 1showed no statistical
S.-Y. Huang et al. / European Neuropsychopharmacology 15 (2005) 227–230 228
differences in sex, age, body mass index (BMI), serum alanine aminotransferase (ALT) level, and frequency of protein intake between the patient and control group. In depressive patients, the age of onset was 31.6F12.0 (S.D.) years with duration of index episode being 24.6F15.8 (S.D.) weeks. Numbers of depressive episodes were 3.0F3.3 (S.D.). Further, the mean score on the 21-item Hamilton Rating Scale for Depression (HRSD) in patient group at the time of blood sampling for the study was 21.8F4.3 (S.D.), ranging from 17 to 35.
Table 1 also shows that sALB levels in patients with
major depressive disorder (4.17F0.28 g/dL) were signifi-cantly lower ( p=0.049) than those of the control group
(4.33F0.20 g/dL). Fig. 1 shows that the severity of
depression is negatively correlated to the level of sALB (r= 0.46, p=0.04) in patients with major depressive disorder. We also examined possible influences of clinical variables on the differences of sALB levels, including age, exercise, BMI, and protein intake. Serum albumin levels in patients with major depressive disorder were not found to correlate to any aforementioned clinical variables.
4. Discussion
Hypoalbuminaemia has been reported more in patients with major depressive disorder than in normal volunteers (Maes et al., 1999; Van Hunsel et al., 1996; Gendall et al., 1999b). Due to the retrospective nature of their analysis and the lack of dietary assessment, it is difficult to interpret those findings. To the best of our knowledge, this is the first diet-controlled study focusing on the sALB levels in patients with major depressive disorder. The main finding of this study is that sALB levels are significantly lower in patients with major depressive disorder than in normal volunteers.
Furthermore, the decrease of sALB levels correlates to the severity of depressive symptoms rated by HRSD. Hypo-albuminaemia seems to have an important clinical meaning beyond malnutrition in major depressive disorder.
In general, hypoalbuminaemia is a multifactorial process involving several processes, such as protein intake, albumin synthesis, breakdown, and leakage to the extravascular space. In this study, protein intake between patients and the control group were the same. Reduced albumin synthesis may be an important additional reason of low serum albumin concentration, since albumin is exclusively synthe-sized in the liver. We measured serum alanine amino-transferase (ALT) levels and found that there is no difference between patient and control groups (Table 1).
Under inflammatory conditions, the transcapillary escape rate (TER) of albumin may increase by several folds (Ballmer et al., 1994; Fleck et al., 1985). The inflammatory response could be an important factor causing albumin leakage. Possible direct or indirect mediators affecting TER of albumin were identified as interleukin-2, interferon-a,
and interleukin-6 (Ballmer, 2001). Interestingly, major
depressive disorder has been reported to be associated with systemic immune activation and inflammatory response
markers (Maes et al., 1995b). The complex relations
between HPA axis hyperactivity and systemic stimulation of the immune system may be part of the pathophysiology
and pathogeneses of depression (Maes et al., 1994). The
hypothesis is that an increased production of interleukins (IL-6, IL-2, IL-1h) in severe depression is the underlying mechanism for several aspects of the immune and acute
phase response (Maes et al., 1995a,b). The decrease of
sALB in patients with major depressive disorder in our study may be the result of systemic immune activation. Further studies connecting the relationship of the decrease of sALB levels and the increase of immune function in patients with major depressive disorder are needed.
Table 1
Demographic, clinical characteristics, two dietary assessments, and serum albumin levels of patients of major depressive disorder (MDD) and healthy controls MDD* (n=19) Healthy controls* (n=19) p Age, years 39.7F11.5 42.3F10.7 0.977 Sex (no. of F/M) 15:4 14:5 0.71 Body mass index (kg/m2) 22.3F3.9 22.6F3.2 0.51
Exercise (times/week) 1.7F0.7 2.1F0.7 0.174 Dietary Assessments
24-h dietary recall on protein intake (g)
72.8F34.3 65.9F20.0 0.523
3-consecutive day food diaries on protein intake(g) 58.5F21.8 68.7F20.3 0.125 Serum albumin (g/dL) 4.17F0.28 4.33F0.20 0.049 Serum alanine aminotransferase (ALT) 19.0F6.7 20.7F7.4 0.47
* MeanFS.D. were listed unless otherwise specified. Differences were compared by the Mann–Whitney test. Difference was considered statisti-cally significant if a P-value was equal to or smaller than 0.05.
Fig. 1. The severity of depression rated by Hamilton Rating Scale for Depression (HRSD) is negatively correlated (Pearson’s correlations test, r= 0.46, p=0.04) to the level of serum albumin (sALB) in patients with major depressive disorder.
The other important finding in our study is that the decrease of sALB levels correlates to the severity of depressive symptoms rated by HRSD. The search for biological markers of depression has been motivated by the need to facilitate the ease and accuracy of diagnosis and prediction of the prognosis. Serum albumin is routinely determined in blood tests and easily determined without the use of sophisticated equipment.
The result of this study should be carefully interpreted because the sample size is small and it shows only borderline statistical significance in the differences in sALB levels between groups and the correlation between sALB and HRSD scores. Furthermore, if the outlier patient with sALB level of 3.7 g/dL and HRSD score of 35 was excluded, there would not be statistical significance. Our results can only be seen as very preliminary and should be confirmed by larger studies.
Acknowledgements
The work was supported by the following grants, NSC 93-2320-B-039-001 and NSC90-2320-B-038-057 from the National Science Council and CMU93-M-24 and DMR-92-017 from China Medical University Hospital in Taiwan.
References
Ballmer, P.E., 2001. Causes and mechanisms of hypoalbuminaemia. Clin. Nutr. 20 (3), 271 – 273.
Ballmer, P.E., Ochsenbein, A.F., Schutz-Hofmann, S., 1994. Transcapillary escape rate of albumin positively correlates with plasma albumin concentration in acute but not in chronic inflammatory disease. Metabolism 43 (6), 697 – 705.
Fleck, A., Raines, G., Hawker, F., Trotter, J., Wallace, P.I., Ledingham, I.M., Calman, K.C., 1985. Increased vascular permeability: a major cause of hypoalbuminaemia in disease and injury. Lancet 1 (8432), 781 – 784.
Gendall, K.A., Bulik, C.M., Joyce, P.R., 1999a. Visceral protein and hematological status of women with bulimia nervosa and depressed controls. Physiol. Behav. 66 (1), 159 – 163.
Gendall, K.A., Bulik, C.M., Joyce, P.R., 1999b. Visceral protein and hematological status of women with bulimia nervosa and depressed controls. Physiol. Behav. 66 (1), 159 – 163.
Gray, G.E., Meguid, M.M., 1990. Can total parenteral nutrition reverse hypoalbuminemia in oncology patients? Nutrition 6 (3), 225 – 228. Harvey, K.B., Moldawer, L.L., Bistrian, B.R., Blackburn, G.L., 1981.
Biological measures for the formulation of a hospital prognostic index. Am. J. Clin. Nutr. 34 (10), 2013 – 2022.
Herrmann, F.R., Safran, C., Levkoff, S.E., Minaker, K.L., 1992. Serum albumin level on admission as a predictor of death, length of stay, and readmission. Arch. Intern. Med. 152 (1), 125 – 130.
Maes, M., Meltzer, H.Y., Stevens, W., Cosyns, P., Blockx, P., 1994. Multiple reciprocal relationships between in vivo cellular immunity and hypothalamic–pituitary–adrenal axis in depression. Psychol. Med. 24 (1), 167 – 177.
Maes, M., Meltzer, H.Y., Bosmans, E., Bergmans, R., Vandoolaeghe, E., Ranjan, R., Desnyder, R., 1995a. Increased plasma concentrations of interleukin-6, soluble interleukin-6, soluble interleukin-2 and transferrin receptor in major depression. J. Affect. Disord. 34 (4), 301 – 309. Maes, M., Smith, R., Scharpe, S., 1995b. The monocyte–T-lymphocyte
hypothesis of major depression. Psychoneuroendocrinology 20 (2), 111 – 116.
Maes, M., De Vos, N., Demedts, P., Wauters, A., Neels, H., 1999. Lower serum zinc in major depression in relation to changes in serum acute phase proteins. J. Affect. Disord. 56 (2–3), 189 – 194.
Phillips, A., Shaper, A.G., Whincup, P.H., 1989. Association between serum albumin and mortality from cardiovascular disease, cancer, and other causes. Lancet 2 (8677), 1434 – 1436.
Rimm, E.B., Giovannucci, E.L., Stampfer, M.J., Colditz, G.A., Litin, L.B., Willett, W.C., 1992. Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am. J. Epidemiol. 135 (10), 1114 – 1126. Smith, G., Robinson, P.H., Fleck, A., 1996. Serum albumin distribution in
early treated anorexia nervosa. Nutrition 12 (10), 677 – 684.
Van Hunsel, F., Wauters, A., Vandoolaeghe, E., Neels, H., Demedts, P., Maes, M., 1996. Lower total serum protein, albumin, and beta- and gamma-globulin in major and treatment-resistant depression: effects of antidepressant treatments. Psychiatry Res. 65 (3), 159 – 169.
Yao, J.K., Reddy, R., Van Kammen, D.P., 2000. Abnormal age-related changes of plasma antioxidant proteins in schizophrenia. Psychiatry Res. 97 (2–3), 137 – 151.
S.-Y. Huang et al. / European Neuropsychopharmacology 15 (2005) 227–230 230