Kaohsiung J Med Sci April 2009 • Vol 25 • No 4 184
Despite the availability of a variety of therapeutic regimens for the treatment of patients with diabetes mellitus, glycemic control is still fundamental in dia-betes management. Better glycemic control decreases
the risk for the development of acute and chronic diabetic complications, and optimizes quality of life [1–3]. The patients’ behavioral changes and adher-ence to a glycemic control program are associated with their self-recognition of the disease state and their knowledge of diabetes, which can be enhanced by the implementation of a diabetes education plan [4–8]. In fact, patient education delivered by certified diabetes educators (CDEs) has become an important part of the diabetes treatment program in medical settings [9,10]. Nevertheless, the delivery of integrated care
Received: Nov 14, 2008 Accepted: Apr 13, 2009 Address correspondence and reprint requests to: Dr Shang-Jyh Hwang, Department of Medicine, Kaohsiung Medical University Hospital, 100 Tzyou 1stRoad, Kaohsiung 807, Taiwan. E-mail: sjhwang@kmu.edu.tw
A
DHERENCE TO A
D
IABETIC
C
ARE
P
LAN
P
ROVIDES
B
ETTER
G
LYCEMIC
C
ONTROL IN
A
MBULATORY
P
ATIENTS WITH
T
YPE
2 D
IABETES
Yi-Wen Chiu,1,6Jer-Ming Chang,1,6Li-Ing Lin,2Pi-Yu Chang,4Wan-Ching Lo,2Ling-Chu Wu,5
Tun-Chieh Chen,3and Shang-Jyh Hwang3,6
Departments of 1Medicine and 2Nursing, Kaohsiung Municipal Hsiao-Kang Hospital, Kaohsiung
Medical University; 3Department of Medicine, 4Center of Administration Management, and 5Department of Nursing, Kaohsiung Medical University Hospital, Kaohsiung Medical University; and
6Faculty of Renal Care, College of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan.
Tight control of blood sugar improves the outcomes for diabetic patients, but it can only be achieved by adhering to a well-organized care plan. To evaluate the effect of a diabetes care plan with reinforcement of glycemic control in diabetic patients, 98 ambulatory patients with type 2 diabetes who visited our diabetes clinic every 3–4 months and who completed four education courses given by certified diabetes educators within 3 months after the first visit, were defined as the Intervention group. A total of 82 patients fulfilling the inclusion criteria for the Intervention group but who missed at least half of the diabetes education sessions were selected as controls. Both groups had comparable mean hemoglobin A1c (HbA1c) levels at baseline, which decreased significantly at 3 months and were maintained at approximately constant levels at intervals for up to 1 year. The HbA1c decrement in the Intervention group was significantly greater than that in the Control group over the 1-year follow-up period (HbA1c change: −2.5 ± 1.8% vs. −1.1 ± 1.7%,
p< 0.01). The maximal HbA1c decrement occurred during the first 3 months, and accounted for
95.6% and 94.6% of the total HbA1c decrements in the Intervention and Control groups, respec-tively. In the multiple regression model, after adjustment for age, body mass index, and duration of diabetes, the Intervention group may still have a 12.6% improvement in HbA1c from their original value to the end of 1 year treatment compared with the Control group (p< 0.05). Diabetes care, with reinforcement from certified diabetes educators, significantly improved and main-tained the effects on glycemic control in ambulatory patients with type 2 diabetes.
Key Words:diabetes, diabetes care, glycemic control (Kaohsiung J Med Sci 2009;25:184–92)
by diabetes specialists, nurses and dietitians, with rein-forcement of drug adherence, self-glucose monitor-ing and dietary control, also significantly contributes to the management of diabetic patients and should not be neglected [11–15].
To clarify whether an integrated care plan, includ-ing diabetes education, does have benefits in terms of the outcomes of glycemic control, however, remains a challenge because of the coexistence of many other factors, e.g. the demographic and physiological char-acteristics of patients, teaching methods used, types of antidiabetic medication, and the presence of com-plications. Randomized control trials (RCTs) designed by specialists from multiple disciplines and that incor-porate the dedication of patients, healthcare providers and institution facilities are highly recommended as the most reliable study design to address this issue [16]. However, meta-analysis of the results of several RCTs revealed that patient education exerted only a modest effect on the glycemic control of diabetic patients [17–19]. Furthermore, the effect of an educa-tion plan on glycemic control reportedly declined over the diabetes disease course [18], unless self-management was enhanced by reinforcement of the education plan [20].
Thus, although diabetes education has an tant role in managing diabetic patients, the impor-tance of diabetes education has been overemphasized. However, the patient adherence to the care plan is often overlooked. The purpose of the present study was to determine whether adherence to a new dia-betes care plan implemented at a regional hospital was effective in enhancing the glycemic control of ambulatory patients with type 2 diabetes.
M
ATERIALS ANDM
ETHODSThis study was conducted at a 464-bed regional hos-pital of Kaohsiung City in southern Taiwan between January 2000 and June 2001. Ambulatory patients with diabetes were put under the care of a diabetes team, which was composed of diabetes specialists, nurses and dietitians of CDEs. We recruited 98 ambu-latory patients with diabetes as the Intervention group according to the following inclusion criteria: (1) patients with type 2 diabetes who were diagnosed and treated by diabetes specialists at the diabetes clinic at our hospital; (2) patients with clear consciousness,
capable of verbal comprehension and communica-tion, and independent in terms of self care; and (3) patients able to return for regular follow-up at the diabetes clinic every 3–4 months and take four dia-betes education courses within 3 months after their initial visit. To study the effectiveness of diabetes education on glycemic control, another 82 diabetic patients, who were regularly treated at out-patient clinics, were selected retrospectively by chart review, and fulfilled the inclusion criteria described above, except that they had taken only one or two diabetes education courses over 3 months, were included as the Control group.
The introduction of diabetes mellitus and diabetes-related complications, exercise, antidiabetic medica-tion, dietary principles for control of blood glucose, and social and psychological support, for example, were all included in the education course. Two nurses, who were qualified CDEs, were responsible for the imple-mentation of this education program. The patients referred to the CDEs from the diabetes specialists were first evaluated by the CDEs, and then received a 30–45-minute one-to-one instruction from the CDEs according to the disease status and needs of the patient. The CDEs then arranged subsequent inter-views in which education courses would be given four times within 3 months after the first visit. In addition, the patients were able to ask the CDEs questions regarding their experiences and to obtain answers in the subsequent follow-up periods until the end of study. In terms of diabetes treatment, most of the patients took oral hypoglycemic agents for blood glucose control, and insulin was used by only two patients. Basic demographic and physical char-acteristics of the patients, presence of complications and laboratory tests were investigated and collected at baseline and every 3–4 months for 1 year. Blood hemoglobin A1c (HbA1c) was measured with an immunoassay, using a monoclonal antibody against the conjugated site of glucose and six amino acids on the N-terminal of hemoglobin β chain. The extent of the reaction was determined using an automatic chemistry analyzer (COBAS INTEGRA 700; Roche Diagnostics, Indianapolis, IN, USA).
Data processing, statistical analyses and graph drawing were conducted using SPSS 11.0 (SPSS Inc., Chicago, IL, USA) and Prism 4.0 (GraphPad Software Inc., San Diego, CA, USA). For the descriptive statistics for demographic and other characteristics of patients
in different groups, the continuous variables are expressed as mean± standard deviation, and categor-ical variables are expressed as frequencies or percent-ages. One-way repeated-measures analysis of variance was used to determine the differences in HbA1c lev-els within each group and between groups at various time points. Values were compared between groups using Student’s t test. Multiple regression analyses were carried out to determine the effects of age, sex, body mass index (BMI), duration of diabetes, group, and duration of diabetes× group on the magnitude of HbA1c improvement. The magnitude of HbA1c im-provement was defined as the difference between the HbA1c level at a particular time point and the base-line level to the basebase-line level, and is expressed as a
percentage. A p value less than 0.05 was considered to be statistically significant.
R
ESULTSThe patient characteristics and the levels of HbA1c are shown in the Table. There were no significant differences between the Intervention and Control groups in terms of age, sex ratio, marital status, edu-cational level, family history of diabetes, body height, body weight, BMI, smoking, and frequency of follow up. Although the Control group had a longer dura-tion of diabetes (8.8± 6.7 vs. 5.3 ± 5.7 years, p < 0.05), the HbA1c levels at baseline were not significantly
Table.Characteristics of the Intervention and Control groups*†
Intervention group (n= 98) Control group (n= 82)
Age (yr) 57.5± 11.3 58.9± 11.0
Male 46.0 51.8
Married 98.0 100
Family history of diabetes 48.0 53.0
Body height (cm) 160.0± 7.7 159.6± 7.5
Body weight (kg) 65.0± 10.3 66.2± 11.4
Body mass index (kg/m2) 25.2± 3.3 25.8± 3.4 Education level
Below primary school 32.0 44.6
Primary and junior school 38.0 22.9
Above junior school 30.0 32.5
Smoking 24.0 21.7
Outpatient clinic visits
> 12 times 64.0 53.0
9–12 times 25.0 26.5
< 9 times 11.0 20.5
Duration of diabetes (yr)‡ 5.3± 5.7 8.8± 6.7 Diabetes-related complications Neuropathy 35.0 38.6 Cardiovascular diseases‡ 6.0 15.7 Retinopathy 33.0 44.6 Nephropathy‡ 14.0 31.3 Laboratory data
Hemoglobin A1c at baseline (%) 9.4± 1.8 9.2± 1.5 *Data presented as mean± standard deviation or %; †statistical comparisons using Student’s t test or χ2test; ‡significant differences between the Intervention and Control groups (p< 0.05).
different between groups (Control group vs. Inter-vention group: 9.2± 1.5% vs. 9.4 ± 1.8%, p > 0.05), and there was no correlation between the duration of diabetes and the baseline HbA1c levels (r= −0.045,
p> 0.05; Pearson’s correlation). The percentage of
patients with complications, including cardiovascu-lar diseases or nephropathy, was higher in the Control group. However, the HbA1c levels in patients with or without each complication were not different.
Despite the comparable HbA1c levels at baseline in the two groups (Table), the HbA1c levels at 3 months, 6 months, 9 months and 12 months were lower in the Intervention group than in the Control group (Figure 1). The repeated-measures analysis of variance re-vealed that the differences in HbA1c levels at these
time points within each group and between both groups were statistically significant. The HbA1c level in the Intervention group was significantly lower than that in the Control group at 12 months (HbA1c: 6.9± 1.2% vs. 7.9 ± 1.8%, p < 0.01; Figure 1A), and the HbA1c decrement at 12 months in the Intervention group was significantly greater than that in the Control group (⌬HbA1c: −2.5 ± 1.8% vs. −1.1 ± 1.7%, p < 0.01; decrement: 26.7% vs. 12.5%; Figure 1B). The maximal HbA1c decrement occurred during the first 3 months, and accounted for 95.6% and 94.6% of the total HbA1c decrements in the Intervention and Control groups, respectively (Figure 1B).
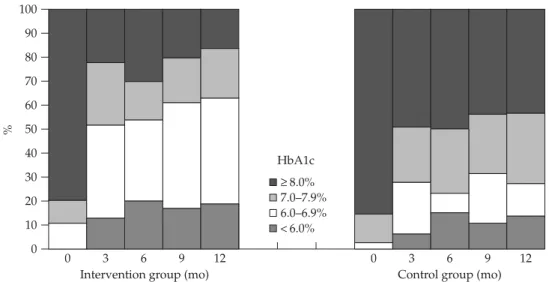
Figure 2 shows the change in percentage in each HbA1c category. In both groups, the percentages shifted toward lower HbA1c categories at 3 months, and the effect persisted for the duration of the study. However, such a shift indicative of improved glycemic control was more pronounced in the Intervention group. To determine whether the decrement in HbA1c was more pronounced during the first 3 months, the differences in HbA1c between 3 months and baseline were plotted against the baseline values in both groups (Figure 3). This showed that higher absolute values of HbA1c at baseline were associated with greater HbA1c decrements at 3 months. This phenomenon was more pronounced in the Intervention group than in the Control group, as shown in Figure 3.
To identify the factors associated with the improve-ment in HbA1c during the study period, a multiple regression model with independent variables was tested. The parameters associated with the magni-tude of HbA1c improvement can be represented in a regression equation:
Magnitude of HbA1c improvement= −28.435 + (12.556 × Intervention group) + (0.954 × BMI) + (0.336 × age) − (0.504 × diabetes duration) This equation revealed that the Intervention group may have a 12.6% improvement in HbA1c from the original value to that at 1 year compared with the Control group (p< 0.05). However, the effect on the im-provement of HbA1c was only 0.34% for age, 0.95% for BMI, and decreased by 0.50% for diabetes dura-tion (all p< 0.05). This model had an R2of 0.198 and an
adjusted R2of 0.179, which means that about 19.8% of the variation in the improvement of HbA1c could be explained by this model.
* * † 10 9 8 7 6 HbA1c (%) Intv. G. Cont. G. p n n 98 82 ns 81 67 < 0.01 77 66 < 0.01 98 78 < 0.01 98 75 < 0.01 Baseline 3 Months 6 9 12
Intervention group Control group
Months 0.5 0.0 −0.5 −1.0 −1.5 −2.0 −2.5 * 0–3 3–6 6–9 9–12 0–12 −3.0 Δ HbA1c (%) * Intervention group Control group
Figure 1. (A) Hemoglobin A1c (HbA1c) levels (mean± standard
error of the mean) in the Intervention group (n= 98) and Control group (n= 82) at baseline and at time intervals of 3 months. Significant differences are noted in the improvement of HbA1c within each group (*p< 0.05) and between groups (†p< 0.05) by
repeated-measures analysis of variance. The differences between the two groups are demonstrated to be significant at all time points, except for at baseline, by Student’s t test (p< 0.01). (B) The mag-nitude of HbA1c decrement at different intervals during the 1-year study period in the Intervention group and Control group. Statistically significant differences can be seen between groups at 3 months and for the total decrement (Student’s unpaired t test; *p< 0.01). The HbA1c decrements are greatest at 3 months, and were responsible for 95.6% and 94.6% of the total HbA1c decre-ments in the Intervention and Control groups, respectively.
HbA1c ≥ 8.0% 7.0–7.9% 6.0–6.9% < 6.0% 100 90 80 70 60 50 40 30 20 10 0 % 0 3 6 9 12
Intervention group (mo)
0 3 6 9 12
Control group (mo)
Figure 2.The percentage of patients in each hemoglobin A1c (HbA1c) category at different time intervals during the 1-year study
period in the: (A) Intervention group (n= 98); and (B) Control group (n = 82). A greater proportion of patients shift towards the lower HbA1c categories at 3 months compared with at baseline, and persist up to 1 year. This shift in HbA1c levels is more pronounced in the Intervention group.
D
ISCUSSIONAlthough there is some discrepancy in the results, several studies have revealed the beneficial effect of integrated care and diabetes education on glycemic control [4,5,21], based on whether a patient education program becomes an integral part of diabetes man-agement. In the present study, the HbA1c level of patients who received a recently introduced diabetes education plan decreased from 9.4± 1.8% at baseline
to 6.9± 1.2% at 12 months, corresponding to a decre-ment of 26.7%, compared with a 12.5% decredecre-ment in the Control group. The significant difference in HbA1c change between the two groups demonstrates the ben-eficial effect of the care plan. This finding was further confirmed by the results of multiple regression analy-sis, in which the group factor accounted for a 12.6% reduction in the HbA1c level in the Intervention group.
RCTs are considered the most reliable study design to address the effect of diabetes education on glycemic control [16]. Meanwhile, meta-analysis of the results of several RCTs has been well addressed [17–19]. However, we were confined to a case-control study because of the complexity in conducting an RCT in this setting. This study was originally part of a pilot study of a nation-wide program of diabetes educa-tion and clinical pathways. It was not designed as an RCT, and the main objective was to establish better care of patients with diabetes through integrated care, including the education plan. Nevertheless, this care plan with its emphasis on diabetes education and professional management led to positive outcomes in terms of glycemic control.
In addition to the reports describing the varied levels of success achieved by programs in promoting glycemic control [17–19], Jiang et al [22] reported that a diabetes education program improved the short-term glycemic control in Taiwanese patients, and determined that the intensity of diabetes education
Figure 3.Correlation between hemoglobin A1c (HbA1c) level at
baseline and HbA1c decrement at 3 months in the Intervention (n= 81) and Control (n = 67) groups. This shows that absolute values for HbA1c at baseline were associated with greater decre-ments in HbA1c at 3 months. This phenomenon, as shown by regression lines, was more pronounced in the Intervention group (solid lines) than in the Control group (dash lines).
4 3 2 1 0 −1 −2 −3 −4 −5 −6 −7 −8 Δ HbA1c, 3 mo – 0 mo (%) 6 7 8 9 10 11 12 13 14 15 16
HbA1c at zero time, %
Intervention group y =−0.8418x + 5.673 Control group y =−0.7760x + 5.902
was the only significant variable associated with the decrease in fasting blood glucose. Keers et al [23] showed that their Multidisciplinary Intensive Edu-cation Programme improved glycemic control and quality of life in diabetes patients with prolonged self-management difficulties. Recently, Tien at al [24] demonstrated the effectiveness of a comprehensive diabetes care program in lowering the HbA1c levels. They found that male patients with a shorter dura-tion of diabetes history and higher baseline levels of HbA1c were more likely to achieve better glycemic control [24]. However, the magnitude of the HbA1c decrement of up to 26.7% in the present study is higher than that achieved in these three reports. In Jiang et al’s study, the HbA1c decrement was 3.2% and 7.4% in patients receiving basic and advanced education programs, respectively, after 4 months of care [22]. Meanwhile, in Keers et al’s study, the HbA1c decrement was 5.1% at 3 months after the Multi-disciplinary Intensive Education Programme [23]. Finally, in Tien et al’s study, the HbA1c decrement was only 2.6% at 3 months [24]. Differences in patient selection and patient characteristics might be respon-sible for these differences.
In this study, we found that patients with higher baseline HbA1c had larger HbA1c decrements, which was also observed in another study [23]. Our patients were not restricted to those with relatively high HbA1c levels, as shown in Figure 3, and only 19.6% of patients in the Intervention group and 14.6% in the Control group had an HbA1c level less than 8.0%. This means that our patients had relative high glycemic status, which might explain why the magnitude in HbA1c improvement was greater in our study. Furthermore, a large proportion of our patients were newly diag-nosed, newly referred and new receivers of diabetes education (94%), meaning that they might display better compliance compared with later stage diabetic patients. Newly diagnosed patients with diabetes have been shown to display better responses to med-ication and the education plan from different aspects, and thus generally have better glycemic control [25]. This might, at least partially, be because they have more interest and motive for complying with med-ication and dietary control in their daily living.
In addition, the majority of the HbA1c decrement was achieved during the first 3 months of the inte-grated care plan, which contributed 95.6% of the total HbA1c decrement over the year. This means that the
effect of diabetes care on the improvement of glycemic control was most pronounced during the initial phase of the intervention program, during which the dia-betes education was delivered. This result is consis-tent with that in other studies [26,27]. Some studies have demonstrated that a more intensive education and care program might be required to achieve fur-ther reduction in HbA1c levels [20]. Nevertheless, maintaining the beneficial effect of diabetes educa-tion on glycemic control is already a real challenge [28]. A gradual deterioration in glycemic control has been observed with prolongation of diabetes [8], which can be attributed to factors such as increased insulin resistance or decreased insulin secretion, lack of response to antidiabetic medication, loss of patient compliance, or fatigue on the part of the care facility. Therefore, the absence of further improvements in glycemic control in the subsequent 9 months might not reflect the ineffectiveness of the integrated care plan during that period of time but rather its remark-able work in maintaining the effect on glycemic control in consideration of persistent significant differences in absolute HbA1c levels between the Intervention and Control groups.
Limitations in the study design and interpretation of the results should be carefully considered. Because this was a retrospective study, selection bias in terms of the study population could exist, although this was minimized as much as possible. The Control group had relatively longer duration of diabetes, and more diabetic complications. These might hinder the im-provements in glycemic control [29], although nei-ther had an effect on the differences in HbA1c levels between the groups in this study. Nevertheless, the control patients were regularly followed-up. They received treatment and their HbA1c was measured in the same manner as the Intervention group; the only difference was that the subjects in the Control group participated in none, one or two diabetes education sessions. The reasons for subject non-participation in the courses were diverse. Some were followed-up at night clinics, and others were unable to attend because of personal or family reasons. By the very fact of attending follow-up regularly, these subjects in the Control group could be regarded as a group of patients who have better compliance with medication and dietary control compared with those who miss their follow-up consultations. This might explain why there was some improvement in their HbA1c levels
during the study, albeit less than that in the Inter-vention group [20].
The present study revealed that ambulatory patients with type 2 diabetes who received an inte-grated care plan, delivered by diabetes specialists and CDEs, had better glycemic control over a 1-year follow-up period. This effect was most pronounced during the first 3 months; this period saw the major-ity of the HbA1c decrement. Whether patients received a diabetes care plan or not was the major determinant for the improvement in glycemic control. Therefore, a diabetes care plan implemented with a reinforcement approach can provide better short-term improve-ments and maintenance of glycemic control in ambu-latory patients with type 2 diabetes.
A
CKNOWLEDGMENTSThe authors would like to express their appreciation to Yi-Hsin Yang, PhD, Associate Professor of the Graduate Institute of Oral Health Science, College of Oral Medicine, Kaohsiung Medical University, for statistical advice.
R
EFERENCES1. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term compli-cations in insulin-dependent diabetes mellitus. N Engl J Med 1993;3299:977–86.
2. Ohkubo Y, Kishikawa H, Araki E, et al. Intensive insulin therapy prevents the progression of diabetic microvascu-lar complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study. Diabetes Res Clin Pract 1995;28:103–17. 3. UK Prospective Diabetes Study (UKPDS) Group. Effect
of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 1998;352:854–65.
4. Rubin RR, Peyrot M, Saudek CD. Effect of diabetes education on self-care, metabolic control, and emotional well-being. Diabetes Care 1989;12:673–9.
5. Raji A, Gomes H, Beard JO, et al. A randomized trial comparing intensive and passive education in patients with diabetes mellitus. Arch Intern Med 2002;162: 1301–4.
6. Panja S, Starr B, Colleran KM. Patient knowledge improves glycemic control: is it time to go back to the classroom? J Invest Med 2005;53:264–6.
7. Heisler M, Piette JD, Spencer M, et al. The relationship between knowledge of recent HbA1c values and dia-betes care understanding and self-management. Diadia-betes Care 2005;28:816–22.
8. Goudswaard AN, Stolk RP, Zuithoff NP, et al. Long-term effects of self-management education for patients with Type 2 diabetes taking maximal oral hypogly-caemic therapy: a randomized trial in primary care. Diabetic Med 2004;1:17:491–6.
9. Mensing C, Boucher J, Cypress M, et al. National stan-dards for diabetes self-management education. Diabetes Care 2006;29(Suppl 1):S78–85.
10. American Diabetes Association. Third-party reimburse-ment for diabetes care, self-managereimburse-ment education, and supplies. Diabetes Care 2006;29(Suppl 1):S68–9.
11. Day JL, Metcalfe J, Johnson P. Benefits provided by an integrated education and clinical diabetes centre: a follow-up study. Diabetic Med 1992;9:855–9.
12. Integrated care for diabetes: clinical, psychosocial, and economic evaluation. Diabetes Integrated Care Eval-uation Team. Br Med J 1994;308:1208–12.
13. Abourizk NN, O’Connor PJ, Crabtree BF, et al. An out-patient model of integrated diabetes treatment and education: functional, metabolic, and knowledge out-comes. Diabetes Educ 1994;20:416–21.
14. van den Arend IJ, Stolk RP, Rutten GE, et al. Education integrated into structured general practice care for type 2 diabetic patients results in sustained improve-ment of disease knowledge and self-care. Diabetic Med 2000;17:190–7.
15. Larsen DL, Cannon W, Towner S. Longitudinal assess-ment of a diabetes care manageassess-ment system in an inte-grated health network. J Manag Care Pharm 2003;9: 552–8.
16. Wheeler ML, Wylie-Rosett J, Pichert JW. Diabetes education research. Diabetes Care 2001;24:421–2.
17. Norris SL, Lau J, Smith SJ, et al. Self-management edu-cation for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care 2002;25: 1159–71.
18. Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a sys-tematic review of randomized controlled trials. Diabetes Care 2001;24:561–87.
19. Gary TL, Genkinger JM, Guallar E, et al. Meta-analysis of randomized educational and behavioral interven-tions in type 2 diabetes. Diabetes Educ 2003;29:488–501. 20. Rhee MK, Slocum W, Ziemer DC, et al. Patient
adher-ence improves glycemic control. Diabetes Educ 2005;31: 240–50.
21. Johnson JA, Eurich DT, Toth EL, et al. Generalizability and persistence of a multifaceted intervention for im-proving quality of care for rural patients with type 2 diabetes. Diabetes Care 2005;28:783–8.
22. Jiang YD, Chuang LM, Wu HP, et al. Assessment of the function and effect of diabetes education programs in Taiwan. Diabetes Res Clin Pract 1999;46:77–82.
23. Keers JC, Bouma J, Links TP, et al. One-year follow-up effects of diabetes rehabilitation for patients with pro-longed self-management difficulties. Patient Educ Couns 2006;60:16–23.
24. Tien KJ, Hung HC, Hsaio JY, et al. Effectiveness of com-prehensive diabetes care program in Taiwanese with type diabetes. Diabetes Res Clin Pract 2008;79:276–83. 25. Tilly KF, Belton AB, McLachlan JF. Continuous
moni-toring of health status outcomes: experience with a diabetes education program. Diabetes Educ 1995;21: 413–9.
26. Jenhani M, Gaha K, Nabouli R, et al. Effectiveness of patient education on glycemic control in insulin treated
patients in general practice. Diabetes Metab 2005;31: 376–81.
27. Rothman RL, Malone R, Bryant B, et al. A randomized trial of a primary care-based disease management pro-gram to improve cardiovascular risk factors and gly-cated hemoglobin levels in patients with diabetes. Am J Med 2005;118:276–84.
28. Saaddine JB, Engelgau MM, Beckles GL, et al. A dia-betes report card for the United States: quality of care in the 1990s. Ann Intern Med 2002;136:565–74.
29. Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. JAMA 2002; 288:475–82.
收文日期:97 年 11 月 14 日 接受刊載:98 年 4 月 13 日 通訊作者:黃尚志醫師 高雄醫學大學附設醫院內科 高雄市 807 三民區自由一路 100 號