Increased Risk of Coronary Heart Disease in Patients with Hip Fracture: A Nationwide Cohort Study
Running title: Hip Fracture and Coronary Heart Disease
Chun-Hao Tsai 1,2, Cheng-Li Lin 3,4, Horng-Chang Hsu 1,2, Wei-Sheng Chung 5,6,7* 1 Graduate Institute of Clinical Medicine, China Medical University, Taichung, Taiwan
2 Department of Orthopedics, China Medical University Hospital, Taichung, Taiwan
3 Management Office for Health Data, China Medical University Hospital, Taichung, Taiwan
4 College of Medicine, China Medical University, Taichung, Taiwan
5 Department of Internal Medicine, Taichung Hospital, Ministry of Health and Welfare, Taichung, Taiwan
6 Department of Health Services Administration, China Medical University, Taichung, Taiwan
7 Department of Healthcare Administration, Central Taiwan University of Science and Technology, Taichung, Taiwan
Correspondence to: *Wei-Sheng Chung, M.D., Ph.D., Department of Internal Medicine, Taichung Hospital, Ministry of Health and Welfare, Taichung, Taiwan; No. 199, Section 1, San-Min Road, Taichung City 40343, Taiwan Tel: 886-4-22294411. Fax: 886-4-22290020.
ABSTRACT
Aims: Bone and vasculature are modulated through numerous common pathways. However, data on the risk of coronary heart disease (CHD) after hip fracture are scarce. Therefore, we
investigated whether hip fracture increased the risk of CHD by conducting a large nationwide cohort study.
Methods: Using universal insurance claims data from 2000 to 2010, we identified a study cohort of 6013 participants newly diagnosed with hip fracture and a control cohort of 23 802 participants. Both cohorts were followed up to the end of 2011 to evaluate the risk of CHD. Results: The overall incidence of CHD was 1.69-fold higher in the hip fracture cohort than it was in the control cohort (29.2 vs. 17.1 per 1000 person-years) with an adjusted hazard ratio of 1.51 (95% confidence interval [CI], 1.39–1.65). Sex-, age-, and comorbidity-specific analysis showed a higher relative risk of CHD for both women and men, all age groups, those with and without comorbidities, and patients with hip fracture compared with the control cohort. The adjusted HR of
CHD was significantly higher in the first follow-up year (adjusted HR = 1.72, 95% CI = 1.45–2.04) than later on.
Conclusion: Hip fracture was independently associated with a subsequent risk of CHD. Keywords: hip fracture, coronary heart disease (CHD), cohort study
Introduction
Coronary heart disease (CHD) describes a spectrum of diseases ranging from coronary
atherosclerosis and myocardial infarction to pos-tinfarct heart failure, [1] and it continues to be a leading cause of morbidity and mortality among adults worldwide. [2–5]
The risk factors of CHD include high blood pressure, smoking, high cholesterol (TC), high LDL-C, low HDL-LDL-C, and diabetes. [6–8] With more knowledge about the risk factors, modification of lifestyle, modern pharmacology, and coronary intervention, the number of CHD-associated deaths has been steadily reduced in past decades. [9] However, as an increase in life expectancy has been observed worldwide, the occurrence of CHD and hip fracture has simultaneously increased. [10, 11] Hip fracture is a severe injury that causes major morbidity and mortality, particularly in elderly populations. [12–14] The total number of hip fractures worldwide has been estimated to be six million per year. [15]
The association between cardiovascular disease and hip fracture has attracted attention since 2009. [16, 17] Bone and vasculature are regulated by common pathophysiological mechanisms, and calcification of the vascular walls resembles the bone formation process in numerous ways. [18, 19] CHD is a well-known risk factor for hip fracture; however, only one previous study assessed the risk of acute myocardial infraction among patients who exhibited a hip fracture within a 10-year study period. [20] Long-term medication after hip fracture plays an additional role in the risk of CHD; therefore, we assessed the risk associated with various medications. This study investigated the frequency and risk of CHD after hip fracture using a nationwide
population-based cohort study. Methods
The study patients for this retrospective cohort study were obtained from the Longitudinal Health Insurance Database (LHID2000), a subset of the National Health Insurance Research Database (NHIRD). Taiwan’s National Health Insurance (NHI) program, launched in 1995, covers more than 99% of the population, which is currently 23 million (http://nhird.nhri.org.tw/en/index.htm). The NHIRD is a nationwide database of reimbursement claims data of the NHI program and is maintained by the National Health Research Institutes (NHRI). The LHID2000 includes the medical claims of 1 000 000 enrollees who were randomly selected from all enrollees. The LHID2000, which is accessible to researchers in Taiwan, is available from the NHRI (http://nhird.nhri.org.tw/date_01.html). The NHRI encrypts patients’ personal information for the protection of privacy, and provides researchers with anonymous identification numbers that relate to the relevant claims information. Diseases were identified according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). This study was approved by the Institutional Review Board of China Medical University (CMU-REC-101-012).
Sampled Participants
Using the LHID2000, we selected patients aged 20 years and older with newly diagnosed hip fracture (ICD-9-CM 820) from 2000 to 2010 as the hip fracture cohort (HF cohort). The first hospitalization of hip fracture was used as the index date. Patients with a history of CHD (ICD-9-CM 410–414) recorded before the index date, a diagnosis of pathological fracture (ICD-9-CM 733.1), fractures from transport-related accidents (E800–E848), or incomplete demographic information, and those younger than 20 years were excluded. The control cohort comprised patients in the LHID2000 without records of hip fracture. We selected 4 times the number of patients in the HF cohort for the control cohort and frequency matched the 2 cohorts by age (in 5-year bands), sex, and index year. The same exclusion criteria were applied to the control patients.
All subjects were followed from the index date until the date that the CHD occurred. Those without occurrence of CHD were followed until the date of withdrawal from the program or the end of December 31, 2011.
Comorbidities
We obtained baseline comorbidities including diabetes CM code 250), hypertension (ICD-9-CM codes 401–405), hyperlipidemia (ICD-9-CM code 272), osteoporosis (ICD-9-CM code 733.0), stroke (ICD-9-CM codes 430-438), obesity (ICD-9-CM code 278), heart failure (ICD-9-CM code 428), alcoholism (ICD-9-CM codes 291, 303, 305.00, 305.01, 305.02, 305.03, 790.3, and V11.3), and chronic obstructive pulmonary disease (COPD) (ICD-9-CM codes 491, 492, 496).
Statistical Analysis
We calculated the proportions for the category variable to describe the distribution, and standard deviation (SD) for the continuous variable between the 2 cohorts. Chi-square and t tests were used to test the differences between the 2 cohorts. We used the Kaplan–Meier method to estimate the cumulative CHD incidence curves for the HF and control cohorts, and tested the difference between the two curves with the log-rank test. Incidence densities (1000 person-years) of CHD by sex-, age-, comorbidity-, and follow-up-years-specific were estimated. Univariable and multivariable Cox proportional hazards regression models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for CHD in patients with hip fracture in relation to the control cohort. Baseline characteristic variables such as sex, age, and comorbidities were included in the multivariate model for adjustment. The comorbidities in the multivariable model, including diabetes, hypertension, hyperlipidemia, COPD, stroke, and heart failure, were considerable Further data analysis was performed to evaluate the interaction pattern among diabetes, hypertension, hyperlipidemia, COPD, stroke, and heart failure on the risk of CHD. Statistical analyses and data management were performed with SAS 9.3 (SAS Institute, Inc., Cary, NC, USA). The statistical significance level was set at P < .05.
Results
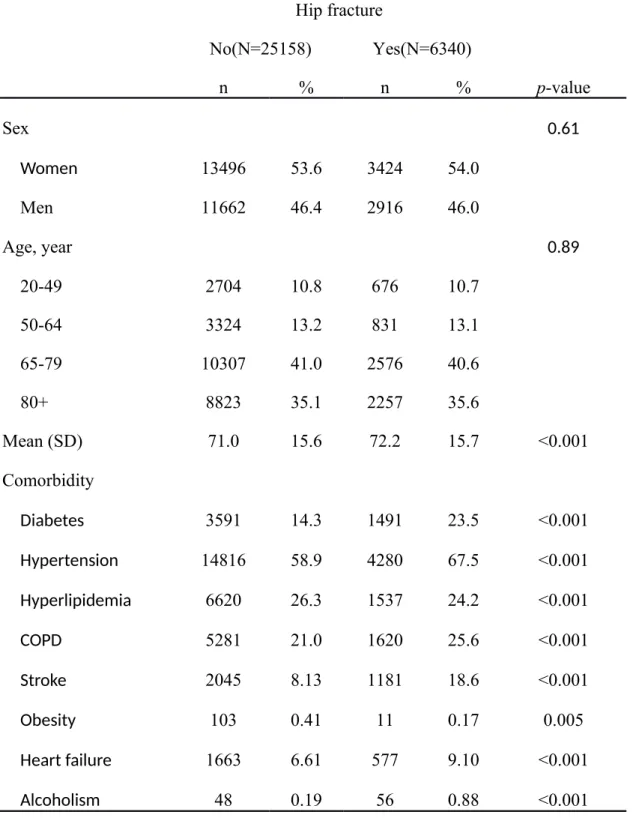
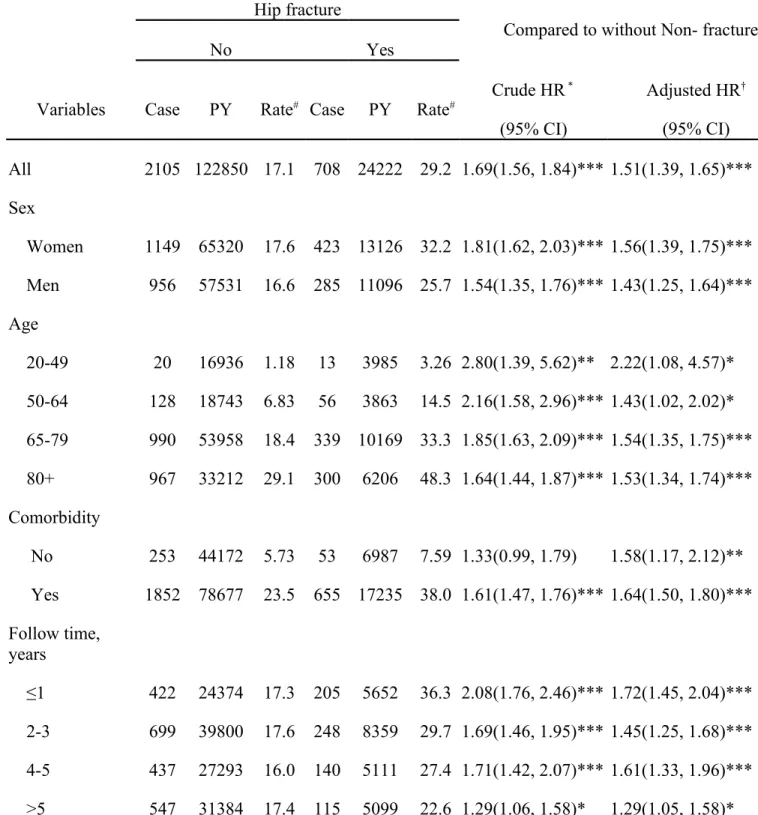
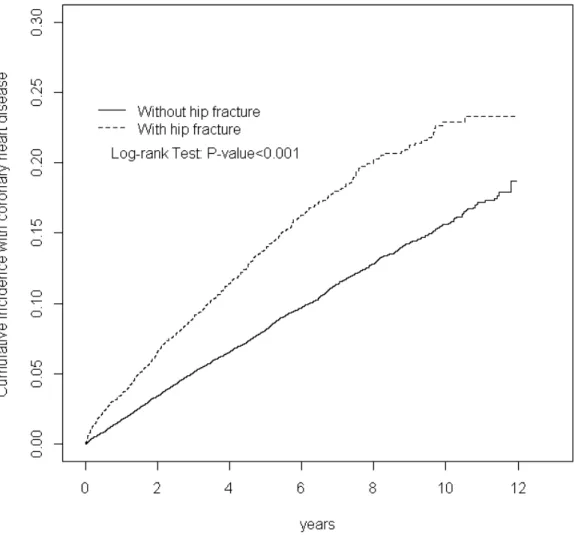
In this study, we established an HF cohort with 6340 patients and a control cohort with 25 158 patients at a highly similar sex ratio (54.0% female) and more than 65 years of age (approximately 51%; Table 1). The mean ages in the HF and control cohorts were 72.2 (SD = 15.7) and 71.0 (SD = 15.6) years, respectively. The prevalence of comorbidities in patients of the HF cohort was higher than it was in patients of the control cohort; comorbidities included diabetes, hypertension, hyperlipidemia, osteoporosis, stroke, obesity, heart failure, alcoholism, and COPD (all P < .05). The mean follow-up was 3.82 years for the HF cohort and 4.88 years for the control cohort, respectively. Figure 1 shows that the HF cohort exhibited a higher incidence of CHD than the control cohort, and the difference was significant for CHD between the 2 cohorts (log-rank test P < .001). The CHD incidence in the HF cohort was 29.2 per 1000 person-years, 1.69-fold higher than that in the control cohort (Table 2). After adjusting for confounding factors, patients in the HF cohort exhibited a risk of developing CHD 1.51-fold higher than that of those in the control cohort (adjusted HR = 1.51, 95% CI = 1.39–1.65). The incidence of CHD was higher in women than in men in both cohorts. The sex-specific relative risk of CHD in the HF and control cohorts was significant for both women (adjusted HR = 1.56, 95% CI = 1.39–1.75) and men (adjusted HR = 1.43, 95% CI = 1.25–1.64). The CHD incidence increased with age in both cohorts. However, the age-specific relative risk in the HF and control cohorts was higher for patients aged 20–49 (adjusted HR = 2.22; 95% CI = 1.08–4.57). The subsequent CHD risk in the HF cohort was considerably higher than that in the control cohort when both cohorts were without comorbidity (adjusted HR = 1.58, 95% CI = 1.17–
2.12), and with comorbidity (adjusted HR = 1.64, 95% CI = 1.50–1.80). The highest risk in patients with hip fracture was in the follow-up duration ≤ 1 year (adjusted HR = 1.72; 95% CI = 1.45–2.04), but the risk in patients with over 5 years of follow-up was still significantly higher (adjusted HR = 1.29; 95% CI = 1.05–1.58).
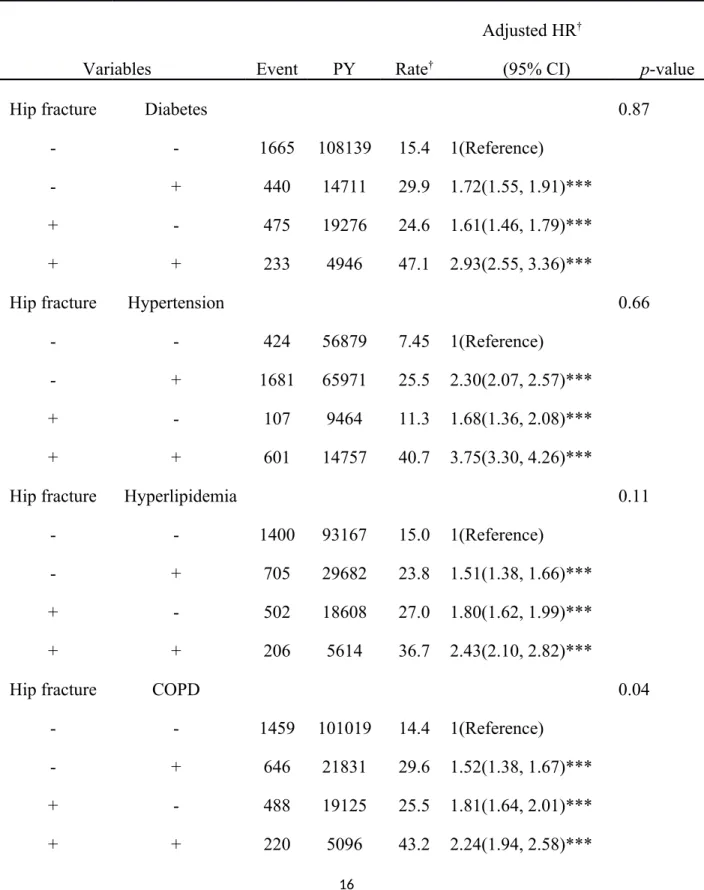
Table 3 shows the joint effects of hip fracture and comorbidities on the risk of CHD. Coexistence with diabetes (adjusted HR = 2.93, 95% CI = 2.55, 3.36), hypertension (adjusted HR = 3.75, 95% CI = 3.30, 4.26), hyperlipidemia (adjusted HR = 2.43, 95% CI = 2.10, 2.82), COPD (adjusted HR = 2.24, 95%, CI = 1.94, 2.58), stroke and heart failure (adjusted HR = 3.98, 95% CI = 3.30-4.80) enhanced the risk of CHD in patients with HF.
Discussion
The results of the current study indicated that, after adjustment for potential confounding factors, patients with hip fracture exhibited a risk of developing CHD that was 1.51-fold higher than that of patients in the control cohort. This finding is consistent with those of previous studies. [20] However, a study by Chiang [20] focused only on the increased risk of acute myocardial infarctionafter hip fracture and separate coronary heart disorder as a risk factor. Our study demonstrated that the risk of CHD persisted during follow-up periods of over 12 years.
The causality mediating CHD occurrence among patients with hip fracture requires further study. Numerous factors may be involved in the association of hip fracture and CHD, such as chronic inflammation, lipid metabolism, oxidative stress, and regulatory hormones. [19, 21] The formation of atherosclerosis mainly results from maturation of macrophages in the vessel wall with subsequent ingestion of lipid to form an atherosclerotic plaque. The presence of
proinflammatory endothelial cells with resident macrophages drives alterations in vascular smooth muscle cells, which leads to the development of a bone phenotype.[22–24] According to a genetic explanation, the association between hip fracture and CHD involves not only telomere length but also specific genes involved in cellular mechanisms shared by the vasculature and bone. [25, 26] Matrix proteins supporting bones, vessel walls, and the myocardium might be particularly relevant. Decreased physical activity, psychological distress, and pain are common after hip fracture. [27] Disruption or deterioration of preexisting cardiovascular risk could be
triggered in such circumstances.
The high risk observed for the presence of hip fracture and comorbid medical disorders might reflect a synergistic effect between these risk factors. The higher risk in patients of a younger age may be attributable to the genetic factor. [25, 26] In the current study, the risk of CHD after hip fracture was prominent among young patients, females, and those with COPD and stroke. Typically, the main risk factor for CHD is male sex. Women exhibit a high risk of CHD, consistent with previous studies in which a high risk of acute myocardial infarction after hip fracture was observed. The relationship between sex and CHD risk remains controversial. [28, 29]
Our study revealed that the highest risk of CHD was within the first year after hip fracture, and the risk remained high in the following years. Our findings indicate that not only short term prophylaxis for cardiovascular events in primary care after hip fracture should be ensured, but also long-term life-style changes should be considered.
The strength of our study lies in the use of a population-based data set comprising a high number of subjects. The current cohort study confirms that hip fracture is associated with an increased risk of CHD. However, several limitations must be considered when interpreting these findings. First, because a claims database was used, we were unable to investigate the effects of risk factors such as body mass index, dietary habits, exercise capacity, and smoking in the regression model, which potentially compromises our findings. In addition, because nutritional supplements are not covered by the NHI program in Taiwan, information on vitamin D and calcium supplements is lacking. We could not adjust our estimates for severity of CHD and comorbidity. Bisphosphonate is widely used in the treatment of osteoporosis and after hip fracture. The current study adjusted for the risk between bisphosphonates and CHD. Although bisphosphate use was not related to the risk of CHD in our study, the cardiovascular safety of
bisphosphonates for the treatment of osteoporosis remains a concern [30–33]. Further study of dosage and course of various bisphosphonates as well as the risk of CHD after hip fracture and surgery is warranted.
In conclusion, hip fracture was independently associated with an increased risk of developing CHD. In addition, the risk of CHD after hip fracture was more prominent in younger patients, women, and patients with more cardiovascular comorbidities. We suggest that physicians be proactive in preventing CHD because of the subsequently higher risk of CHD among patients with hip fracture. Controlling cardiovascular risks, early mobilization, lipid control medication, and life-style adjustment play crucial roles in decreasing the risk of CHD after hip fracture.
References
1. Taylor DA, Robertson MJ (2009) The basics of cell therapy to treat cardiovascular disease: one cell does not fit all. Rev Esp Cardiol 62:1032-1044 2. McGovern PG, Pankow JS, Shahar E, Doliszny KM, Folsom AR, Blackburn H, Luepker RV (1996) Recent trends in acute coronary heart disease--mortality,
morbidity, medical care, and risk factors. The Minnesota Heart Survey Investigators. N Engl J Med 334:884-890
3. McGovern PG, Jacobs DR, Jr., Shahar E, Arnett DK, Folsom AR, Blackburn H, Luepker RV (2001) Trends in acute coronary heart disease mortality, morbidity, and medical care from 1985 through 1997: the Minnesota heart survey. Circulation 104:19-24
4. Roger VL (2007) Epidemiology of myocardial infarction. Med Clin North Am 91:537-552; ix
5. Go AS, Mozaffarian D, Roger VL, et al. (2013) Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation 127:e6-e245
6. Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR (1977) Diabetes, blood lipids, and the role of obesity in coronary heart disease risk for women. The Framingham study. Ann Intern Med 87:393-397
7. Gordon T, Kannel WB (1982) Multiple risk functions for predicting coronary heart disease: the concept, accuracy, and application. Am Heart J 103:1031-1039 8. Anthony D, George P, Eaton CB (2014) Cardiac risk factors: environmental, sociodemographic, and behavioral cardiovascular risk factors. FP Essent 421:16-20 9. Levy LB (2013) Dietary strategies, policy and cardiovascular disease risk reduction in England. Proc Nutr Soc 72:386-389
10. Gerber Y, Jacobsen SJ, Frye RL, Weston SA, Killian JM, Roger VL (2006) Secular trends in deaths from cardiovascular diseases: a 25-year community study. Circulation 113:2285-2292
11. Alves SM, Castiglione D, Oliveira CM, de Sousa B, Pina MF (2014) Age-period-cohort effects in the incidence of hip fractures: political and economic events are coincident with changes in risk. Osteoporos Int 25:711-720
12. Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359:1761-1767
13. Fisher AA, Davis MW, Rubenach SE, Sivakumaran S, Smith PN, Budge MM (2006) Outcomes for older patients with hip fractures: the impact of orthopedic and geriatric medicine cocare. J orthop trauma 20:172-178; discussion 179-180
14. Bentler SE, Liu L, Obrizan M, et al. (2009) The aftermath of hip fracture: discharge placement, functional status change, and mortality. American journal of epidemiology 170:1290-1299
15. Kannus P, Parkkari J, Sievanen H, Heinonen A, Vuori I, Jarvinen M (1996) Epidemiology of hip fractures. Bone 18:57S-63S
16. Sennerby U, Melhus H, Gedeborg R, Byberg L, Garmo H, Ahlbom A, Pedersen NL, Michaelsson K (2009) Cardiovascular diseases and risk of hip fracture. JAMA : the journal of the American Medical Association 302:1666-1673
17. Batsis JA, Huddleston JM, Melton LJt, Huddleston PM, Lopez-Jimenez F, Larson DR, Gullerud RE, McMahon MM (2009) Body mass index and risk of adverse cardiac events in elderly patients with hip fracture: a population-based study. Journal of the American Geriatrics Society 57:419-426
18. McFarlane SI (2006) Bone metabolism and the cardiometabolic syndrome: pathophysiologic insights. Journal of the cardiometabolic syndrome 1:53-57 19. McFarlane SI, Muniyappa R, Shin JJ, Bahtiyar G, Sowers JR (2004)
Osteoporosis and cardiovascular disease: brittle bones and boned arteries, is there a link? Endocrine 23:1-10
20. Chiang CH, Liu CJ, Chen PJ, et al. (2013) Hip fracture and risk of acute myocardial infarction: a nationwide study. J Bone Miner Res 28:404-411
21. Theill LE, Boyle WJ, Penninger JM (2002) RANK-L and RANK: T cells, bone loss, and mammalian evolution. Annu Rev Immunol 20:795-823
22. Eastell R, Newman C, Crossman DC (2010) Cardiovascular disease and bone. Archives of Biochemistry and Biophysics 503:78-83
23. Baldini V, Mastropasqua M, Francucci CM, D'Erasmo E (2005) Cardiovascular disease and osteoporosis. J Endocrinol Invest 28:69-72
24. Hofbauer LC, Brueck CC, Shanahan CM, Schoppet M, Dobnig H (2007)
Vascular calcification and osteoporosis--from clinical observation towards molecular understanding. Osteoporos Int 18:251-259
25. Wong LS, de Boer RA, Samani NJ, van Veldhuisen DJ, van der Harst P (2008) Telomere biology in heart failure. Eur J Heart Fail 10:1049-1056
26. Valdes AM, Richards JB, Gardner JP, Swaminathan R, Kimura M, Xiaobin L, Aviv A, Spector TD (2007) Telomere length in leukocytes correlates with bone mineral density and is shorter in women with osteoporosis. Osteoporos Int 18:1203-1210
27. Dharmarajan TS, Banik P (2006) Hip fracture. Risk factors, preoperative assessment, and postoperative management. Postgraduate medicine 119:31-38
28. Seshadri S, Beiser A, Kelly-Hayes M, Kase CS, Au R, Kannel WB, Wolf PA (2006) The lifetime risk of stroke: estimates from the Framingham Study. Stroke; a journal of cerebral circulation 37:345-350
29. Rosamond W, Flegal K, Friday G, et al. (2007) Heart disease and stroke statistics--2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 115:e69-171
30. John Camm A (2010) Review of the cardiovascular safety of zoledronic acid and other bisphosphonates for the treatment of osteoporosis. Clin Ther 32:426-436
31. Black DM, Reid IR, Boonen S, et al. (2012) The effect of 3 versus 6 years of zoledronic acid treatment of osteoporosis: a randomized extension to the HORIZON-Pivotal Fracture Trial (PFT). J Bone Miner Res 27:243-254
32. Sharma A, Chatterjee S, Arbab-Zadeh A, Goyal S, Lichstein E, Ghosh J, Aikat S (2013) Risk of serious atrial fibrillation and stroke with use of bisphosphonates: evidence from a meta-analysis. Chest 144:1311-1322
33. Huang WF, Tsai YW, Wen YW, Hsiao FY, Kuo KN, Tsai CR (2010) Osteoporosis treatment and atrial fibrillation: alendronate versus raloxifene. Menopause 17:57-63
Table 1. Comparison of demographics and comorbidity between patients with hip fracture and control patients
Hip fracture No(N=25158) Yes(N=6340) n % n % p-value Sex 0.61 Women 13496 53.6 3424 54.0 Men 11662 46.4 2916 46.0 Age, year 0.89 20-49 2704 10.8 676 10.7 50-64 3324 13.2 831 13.1 65-79 10307 41.0 2576 40.6 80+ 8823 35.1 2257 35.6 Mean (SD) 71.0 15.6 72.2 15.7 <0.001 Comorbidity Diabetes 3591 14.3 1491 23.5 <0.001 Hypertension 14816 58.9 4280 67.5 <0.001 Hyperlipidemia 6620 26.3 1537 24.2 <0.001 COPD 5281 21.0 1620 25.6 <0.001 Stroke 2045 8.13 1181 18.6 <0.001 Obesity 103 0.41 11 0.17 0.005 Heart failure 1663 6.61 577 9.10 <0.001 Alcoholism 48 0.19 56 0.88 <0.001
Chi-square test; †T-test;
Table 2. Incidence and adjusted HRs of CHD stratified by sex, age, and comorbidity; comparing patients with hip fracture and patients without hip fracture
Hip fracture
Compared to without Non- fracture
No Yes
Variables Case PY Rate# Case PY Rate# Crude HR
* (95% CI) Adjusted HR† (95% CI) All 2105 122850 17.1 708 24222 29.2 1.69(1.56, 1.84)*** 1.51(1.39, 1.65)*** Sex Women 1149 65320 17.6 423 13126 32.2 1.81(1.62, 2.03)*** 1.56(1.39, 1.75)*** Men 956 57531 16.6 285 11096 25.7 1.54(1.35, 1.76)*** 1.43(1.25, 1.64)*** Age 20-49 20 16936 1.18 13 3985 3.26 2.80(1.39, 5.62)** 2.22(1.08, 4.57)* 50-64 128 18743 6.83 56 3863 14.5 2.16(1.58, 2.96)*** 1.43(1.02, 2.02)* 65-79 990 53958 18.4 339 10169 33.3 1.85(1.63, 2.09)*** 1.54(1.35, 1.75)*** 80+ 967 33212 29.1 300 6206 48.3 1.64(1.44, 1.87)*** 1.53(1.34, 1.74)*** Comorbidity No 253 44172 5.73 53 6987 7.59 1.33(0.99, 1.79) 1.58(1.17, 2.12)** Yes 1852 78677 23.5 655 17235 38.0 1.61(1.47, 1.76)*** 1.64(1.50, 1.80)*** Follow time, years ≤1 422 24374 17.3 205 5652 36.3 2.08(1.76, 2.46)*** 1.72(1.45, 2.04)*** 2-3 699 39800 17.6 248 8359 29.7 1.69(1.46, 1.95)*** 1.45(1.25, 1.68)*** 4-5 437 27293 16.0 140 5111 27.4 1.71(1.42, 2.07)*** 1.61(1.33, 1.96)*** >5 547 31384 17.4 115 5099 22.6 1.29(1.06, 1.58)* 1.29(1.05, 1.58)*
Adjusted HR† : multivariable analysis including age, sex, co-morbidities of diabetes, hypertension, hyperlipidemia, osteoporosis, CAD, and heart failure; *p<0.05, **p<0.01, ***p<0.001
Comorbidity‡: Only to have one of comorbidities (including diabetes, hypertension,
hyperlipidemia, osteoporosis, stroke, obesity, heart failure, and alcoholism) classified as the comorbidity group
Table 3. HRs measured using Cox proportional model for the patients with hip fracture - associated with CHD combined effect of comorbidity
Adjusted HR†
Variables Event PY Rate† (95% CI) p-value
Hip fracture Diabetes 0.87
- - 1665 108139 15.4 1(Reference)
- + 440 14711 29.9 1.72(1.55, 1.91)***
+ - 475 19276 24.6 1.61(1.46, 1.79)***
+ + 233 4946 47.1 2.93(2.55, 3.36)***
Hip fracture Hypertension 0.66
- - 424 56879 7.45 1(Reference)
- + 1681 65971 25.5 2.30(2.07, 2.57)***
+ - 107 9464 11.3 1.68(1.36, 2.08)***
+ + 601 14757 40.7 3.75(3.30, 4.26)***
Hip fracture Hyperlipidemia 0.11
- - 1400 93167 15.0 1(Reference)
- + 705 29682 23.8 1.51(1.38, 1.66)***
+ - 502 18608 27.0 1.80(1.62, 1.99)***
+ + 206 5614 36.7 2.43(2.10, 2.82)***
Hip fracture COPD 0.04
- - 1459 101019 14.4 1(Reference)
- + 646 21831 29.6 1.52(1.38, 1.67)***
+ - 488 19125 25.5 1.81(1.64, 2.01)***
Hip fracture Stroke 0.008
- - 1822 115942 15.7 1(Reference)
- + 283 6908 41.0 1.91(1.68, 2.16)***
+ - 527 20606 25.6 1.66(1.51, 1.83)***
+ + 181 3616 50.1 2.74(2.35, 3.19)***
Hip fracture Heart failure 0.21
- - 1772 116854 15.2 1(Reference)
- + 333 5996 55.5 2.60(2.31, 2.92)***
+ - 588 22760 25.8 1.73(1.58, 1.91)***
+ + 120 1462 82.1 3.98(3.30, 4.80)***
N, sample size; n, events of coronary heart disease; Rate†, incidence rate, per 1,000 person-years; Adjusted HR† : multivariable analysis including age and gender;
*P<.05, **P<.01, ***P<.001 §P-value for interaction
Figure 1. Cumulative incidence of CHD for patients with (dashed line) and without (solid line) hip fracture