2015/May/13
Type of manuscript: Original article
Manuscript title: Chronic osteomyelitis correlates with increased risk of acute pancreatitis in a case-control study in Taiwan
Running head: chronic osteomyelitis and acute pancreatitis Authors' full names:
Shih-Wei Lai MD1,2 , Hsueh-Chou Lai DM and MS 3,4, Cheng-Li Lin MS 1,5, Kuan-Fu
Liao MD and MS 6,7, Chun-Hung Tseng MD 1,8
1College of Medicine, China Medical University and 2Department of Family
Medicine, China Medical University Hospital, Taichung, Taiwan
3College of Chinese Medicine, China Medical University and 4Division of
Hepato-gastroenterology, Department of Internal Medicine, China Medical University Hospital, Taichung, Taiwan.
5Management Office for Health Data, China Medical University Hospital, Taichung,
Taiwan
6Graduate Institute of Integrated Medicine, China Medical University and
7Department of Internal Medicine, Taichung Tzu Chi General Hospital, Taichung,
Taiwan
8Department of Neurology, China Medical University Hospital, Taichung, Taiwan
(The first two authors equally contributed to this study)
Corresponding author: Kuan-Fu Liao, Department of Internal Medicine, Taichung Tzu Chi General Hospital, No.66, Sec. 1, Fongsing Road, Tanzi District, Taichung City, 427, Taiwan
Phone: 886-4-2205-2121; Fax: 886-4-2203-3986 E-mail: kuanfuliaog@gmail.com
ABSTRACT
Objectives. The objective of this study was to examine the relationship between chronic osteomyelitis and acute pancreatitis in Taiwan. Methods. This was a population-based case-control study utilizing the database of the Taiwan National Health Insurance Program. We identified 7678 cases aged 20-84 with newly diagnosed acute pancreatitis during the period of 1998 to 2011. From the same database, 30712 subjects without diagnosis of acute pancreatitis were selected as controls. The cases and controls were matched with sex, age and index year of diagnosing acute pancreatitis. The odds ratio with 95% confidence interval of acute pancreatitis associated with chronic osteomyelitis was examined by the multivariable unconditional logistic regression analysis. Results. After adjustment for multiple confounders, the multivariable analysis showed that the adjusted odds ratio of acute pancreatitis was 1.93 for subjects with chronic osteomyelitis (95% confidence interval 1.01, 3.69), when compared with subjects without chronic osteomyelitis.
Conclusions. Chronic osteomyelitis correlates with increased risk of acute
pancreatitis. Patients with chronic osteomyelitis should be carefully monitored about the risk of acute pancreatitis.
INTRODUCTION
Acute pancreatitis is an acute inflammatory condition of the pancreas with variable clinical course that may range from mild, self-limiting to severe and life- threatening. Extensive evidence has revealed that many etiologic factors, including alcoholism, biliary stone, cardiovascular disease, diabetes mellitus, viral hepatitis and
hypertriglyceridemia, are associated with acute pancreatitis, but chronic osteomyelitis is not yet studied.
Chronic osteomyelitis is a chronically recurrent inflammatory condition of the bone which is mainly caused by bacteria. Chronic osteomyelitis is extremely difficult to treat because it has a high rate of relapse or therapeutic failure even after long-term antibiotic therapy and surgical debridement. Its long-term recurrence rate is about 20% to 30%. In addition to impact on the bone and bone marrow, there is growing body of evidence that chronic osteomyelitis is associated with other diseases, including diabetes mellitus, deep-vein thrombosis, coronary heart disease, epilepsy, depression and dementia, but acute pancreatitis is not yet studied.
Given that chronic osteomyelitis and acute pancreatitis are both inflammatory conditions, we make a rational hypothesis that bacterial surface antigens not only attack the bone, but also might attack the pancreas. Acute pancreatitis then develops. Therefore, we think there could be an association between chronic osteomyelitis and acute pancreatitis. From a view of clinical and public health implications, if an association substantially exists, patients with chronic osteomyelitis can be carefully monitored about the risk of acute pancreatitis. Since there is a lack of formal
epidemiological study about this issue, we therefore examine the relationship between chronic osteomyelitis and acute pancreatitis in a case-control study utilizing the database of the Taiwan National Health Insurance Program.
Study design and study population
This was a population-based case-control study using the database of the Taiwan National Health Insurance Program. In a brief, this insurance program began in March 1, 1995, which has included about 99% of 23 million citizens living in Taiwan. The details of the program have been well recorded in previous high-quality studies. This study was approved by the Ethics Review Board of China Medical University and Hospital in Taiwan (CMU-REC-101-012).
Participant selection
Based on diagnostic codes of the International Classification of Diseases (ICD) 9th Revision, we selected subjects with newly diagnosed acute pancreatitis as cases during the period of 1998 to2011 (ICD-9 code 577.0), who were aged 20-84 years at the date of diagnosing acute pancreatitis. The index date for each case was defined as the date of diagnosing acute pancreatitis. For each acute pancreatitis case, we
randomly selected 4 subjects without acute pancreatitis as controls from the same database, frequency matched with sex, age (per 5 years) and the index year of
diagnosing acute pancreatitis. Subjects with prior history of acute osteomyelitis (ICD-9 code 730.0), chronic pancreatitis (ICD-(ICD-9 code 577.1) or pancreatic cancer (ICD-(ICD-9 code 157) before the date of diagnosing acute pancreatitis were excluded from this study.
Potential confounders
Comorbidities before the date of diagnosing acute pancreatitis were included as follows: chronic osteomyelitis (ICD-9 code 730.1), alcohol-related disease (ICD-9 codes 291, 303, 305.00, 305.01, 305.02, 305.03, 790.3 and V11.3), biliary stone (ICD-9 code 574), cardiovascular disease including coronary artery disease, heart failure, cerebrovascular disease and peripheral atherosclerosis (ICD-9 codes 410–414, 428, 430–438 and 440–448), chronic kidney disease (ICD-9 codes 585–586 and
588.8–588.9), chronic obstructive pulmonary disease (ICD-9 codes 491, 492, 493 and 496), diabetes mellitus (ICD-9 code 250), hepatitis B (ICD-9 codes V02.61, 070.20, 070.22, 070.30 and 070.32), hepatitis C (ICD-9 codes V02.62, 070.41, 070.44, 070.51 and 070.54), hyperparathyroidism (ICD-9 code 252.0) and hypertriglyceridemia (ICD-9 codes 272.1, 272.2 and 272.4). According to ICD-9 codes, the diagnosis accuracy of these comorbidities has been recorded in previous studies.
Statistical Analysis
We used the Chi-square test and the t test to compare the differences for distribution of demographic information and comorbidities between the case group and the control group. Only factors found to be significant in the univariable unconditional logistic regression model were further included in the multivariable unconditional logistic regression model to estimate the odds ratio (OR) and 95% confidence interval (CI) for acute pancreatitis associated with chronic osteomyelitis and other comorbidities. The probability value < 0.05 was considered statistically significant (SAS software version 9.1, SAS Institute Inc., Cary, North Carolina, USA).
RESULTS
Characteristics of the study population
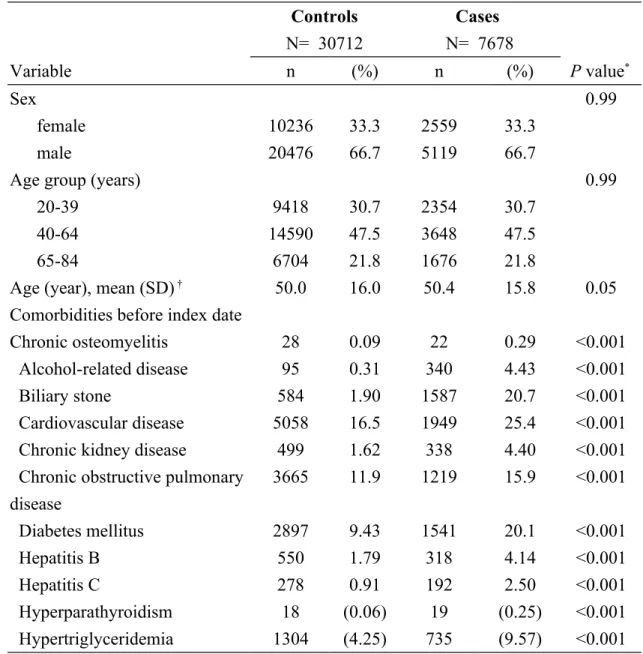
There were 7678 subjects with acute pancreatitis as cases and 30712 subjects without acute pancreatitis as controls. Cases and controls had similar distributions of sex and age. Table 1 shows the case group had higher proportions of chronic osteomyelitis, alcohol-related disease, biliary stone, cardiovascular disease, chronic kidney disease, chronic obstructive pulmonary disease, diabetes mellitus, hepatitis B, hepatitis C, hyperparathyroidism and hypertriglyceridemia than the control group (P <0.001 for Chi-square test).
Association between acute pancreatitis and comorbidities
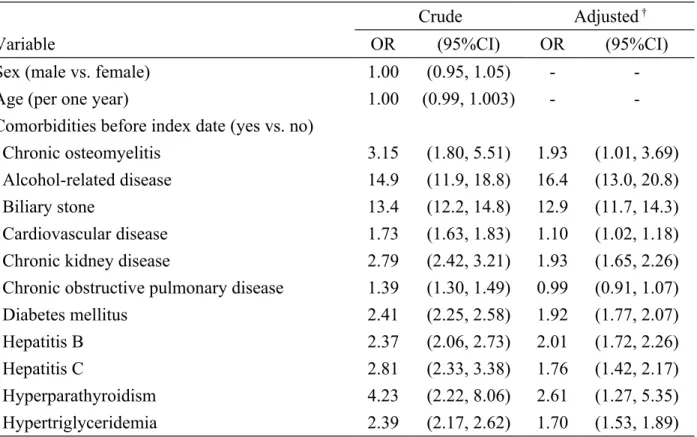
univariable analysis, the multivariable analysis showed that the adjusted odds ratio of acute pancreatitis was 1.93 for subjects with chronic osteomyelitis (95% confidence interval 1.01, 3.69), when compared with subjects without chronic osteomyelitis (Table 2). In addition, alcohol-related disease, biliary stone, cardiovascular disease, chronic kidney disease, diabetes mellitus, hepatitis B, hepatitis C,
hyperparathyroidism and hypertriglyceridemia were other factors significantly related to acute pancreatitis.
DISCUSSION
In this population-based case-control study, we observed that patients with chronic osteomyelitis were associated with increased odds of acute pancreatitis, as compared with patients without chronic osteomyelitis (adjusted OR 1.93). In addition, alcohol-related disease and biliary stone seem to be significantly associated with acute pancreatitis (Table 2). In order to test whether the confounding effect of alcohol-related disease or biliary stone exits, we made a further analysis. When compared with patients without chronic osteomyelitis and without alcohol-related disease and biliary stone, the adjusted odds ratio of acute pancreatitis was 2.44 among those with chronic osteomyelitis and without alcohol-related disease and biliary stone (95% confidence interval 1.26, 4.73, Table not shown). This indicates that the increased risk of acute pancreatitis associated with chronic osteomyelitis seems to be not
confounded by related disease and biliary stone. Even in absence of alcohol-related disease and biliary stone, chronic osteomyelitis alone still has an effect on risk of acute pancreatitis. Since chronic osteomyelitis is a chronically recurrent inflammatory condition needing long-term treatment and the overall incidence remains high worldwide, our findings would be important to dedicate some attention
on this issue in a worldwide perspective.
Because no other similar study was reported, our study provides the first
epidemiological report about this association. Since the role of chronic osteomyelitis associated with acute pancreatitis remains poorly understood, the relevant studies were reviewed to explain this association. First, it may be an inflammatory theory. Chronic osteomyelitis is a chronically recurrent inflammatory condition of the bone which is mainly caused by bacteria. Bacterial surface antigens not only attack the bone, but also might attack the pancreas. Therefore, the endogenous immune defense systems of the host, including cytokines, would be activated. Acute inflammation of the pancreas might be induced by the interaction of bacterial surface antigens with endogenous immunity. Second, it may be a drug-related theory. Many drugs are found to potentially cause acute pancreatitis. To date, multiple drugs are listed in the World Health Organization (WHO) database suspected to be associated with acute pancreatitis. Long-term antibiotic therapy is always needed to treat chronic
osteomyelitis. During treatment period, one key drug could potentially induce acute pancreatitis, but it seems to be relatively difficult to find the key drug in this
observational study. Moreover, a high index of suspicion of drug-related acute pancreatitis is needed among patients with chronic osteomyelitis during receiving antibiotic therapy.
When interpreting our results, some limitations should be taken into consideration. First, although other traditional risk factors including alcoholism, biliary stone, hypertriglyceridemia and type 2 diabetes mellitus, were found to be associated with acute pancreatitis in Taiwan, whether chronic osteomyelitis is another risk factor for acute pancreatitis could not be determined in a case-control study. Similarly, whether patients with chronic osteomyelitis had other unfound factors related to acute
pancreatitis could not be clarified in this study. Second, the exact invading microorganism type of chronic osteomyelitis was not recorded due to the natural limitation of this database. Whether the microorganism type is associated with acute pancreatitis remains inconclusive. If bacteria play a role in the etiology of both conditions, recent exciting discoveries may be helpful in that antibacterial bioactive glass has been used in treatment of chronic osteomyelitis with good primary results. If it works, this rare association may diminish in the future. Third, one study showed that approximately 2% of acute pancreatitis cases might be related to the procedure of iatrogenic endoscopic retrograde cholangiopancreatography (ERCP). Due to the natural limitation of this database, whether patients studied were admitted for undergoing therapeutic ERCP due to biliary-related cause or were admitted due to other causes but complicated by iatrogenic ERCP can not be completely
differentiated. Therefore, whether ERCP is a cause or an effect for acute pancreatitis can not be discerned in this study. That is why ERCP were not included for analysis.
Some strengths of this paper should be discussed. Although this observational study can not analyze the drugs that may have caused the episode of acute pancreatitis, there is a lack of formal epidemiological study about this issue and this study provides the first epidemiological report about this association. It has a large sample size to increase its statistical power. The methods, results and discussion are relatively appropriate. It really provides the undated evidence for this issue.
In conclusion, chronic osteomyelitis correlates with increased risk of acute
pancreatitis. Patients with chronic osteomyelitis should be carefully monitored about the risk of acute pancreatitis, particularly in those receiving antibiotic therapy. Further studies are required to assess the potential mechanism.
Acknowledgement
This study is supported in part by Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence (MOHW104-TDU-B-212-113002), China Medical University Hospital, Academia Sinica Taiwan Biobank, Stroke Biosignature Project (BM104010092), NRPB Stroke Clinical Trial Consortium (MOST 103-2325-B-039 -006), Tseng-Lien Lin Foundation in Taichung in Taiwan, Taiwan Brain Disease Foundation in Taipei in Taiwan, and Katsuzo and Kiyo Aoshima Memorial Funds in Japan. These funding agencies did not influence the study design, data collection and analysis, decision to publish, or preparation of the manuscript. Specific author contributions
Shih-Wei Lai substantially contributed to the conception of this article. He planned and conducted this study. He initiated the draft of the article and critically revised the article.
Hsueh-Chou Lai, Cheng-Li Lin and Chun-Hung Tseng conducted the data analysis and critically revised the article.
Kuan-Fu Liao planned and conducted this study. He participated in the data interpretation and also critically revised the article.
Conflict of Interest Statement
REFERENCES
[1] Kahl S, Mayer JM. Update on experimental acute pancreatitis. Minerva Gastroenterol Dietol. 2012;58:355-63.
[2] Mishra A, Saigal S, Gupta R, Sarin SK. Acute pancreatitis associated with viral hepatitis: a report of six cases with review of literature. Am J Gastroenterol.
1999;94:2292-5.
[3] Spicak J. Etiological factors of acute pancreatitis. Vnitr Lek. 2002;48:829-41. [4] Lai SW, Muo CH, Liao KF, Sung FC, Chen PC. Risk of acute pancreatitis in type 2 diabetes and risk reduction on anti-diabetic drugs: a population-based cohort study in Taiwan. Am J Gastroenterol. 2011;106:1697-704.
[5] Bexelius TS, Ljung R, Mattsson F, Lagergren J. Cardiovascular disease and risk of acute pancreatitis in a population-based study. Pancreas. 2013;42:1011-5.
[6] Ewald N. Hypertriglyceridemia-induced acute pancreatitis. Clinical Lipidology. 2013;8:587-94.
[7] Hogan A, Heppert VG, Suda AJ. Osteomyelitis. Arch Orthop Trauma Surg. 2013;133:1183-96.
[8] Conterno LO, Turchi MD. Antibiotics for treating chronic osteomyelitis in adults. Cochrane Database Syst Rev. 2013;9:CD004439.
[9] Spellberg B, Lipsky BA. Systemic antibiotic therapy for chronic osteomyelitis in adults. Clin Infect Dis. 2012;54:393-407.
[10] Bhattacharya R, Kundu B, Nandi SK, Basu D. Systematic approach to treat chronic osteomyelitis through localized drug delivery system: bench to bed side. Mater Sci Eng C Mater Biol Appl. 2013;33:3986-93.
[11] Lin SY, Lin CL, Tseng CH, Wang IK, Wang SM, Huang CC, et al. The association between chronic osteomyelitis and increased risk of diabetes mellitus: a population-based cohort study. Eur J Clin Microbiol Infect Dis. 2014;33:1647-52. [12] Lin TY, Chen YG, Huang WY, Lin CL, Peng CL, Sung FC, et al. Association between chronic osteomyelitis and deep-vein thrombosis. Analysis of a nationwide population-based registry. Thromb Haemost. 2014;112:573-9.
[13] Hsiao LC, Muo CH, Chen YC, Chou CY, Tseng CH, Chang KC. Increased risk of coronary heart disease in patients with chronic osteomyelitis: a population-based study in a cohort of 23 million. Heart. 2014;100:1450-4.
[14] Tseng CH, Huang WS, Muo CH, Kao CH. Increased risk of epilepsy among patients diagnosed with chronic osteomyelitis. Epilepsy Res. 2014;108:1427-34. [15] Tseng CH, Huang WS, Muo CH, Chang YJ, Kao CH. Increased depression risk
among patients with chronic osteomyelitis. J Psychosom Res. 2014;77:535-40. [16] Tseng CH, Huang WS, Muo CH, Kao CH. Increased risk of dementia among chronic osteomyelitis patients. Eur J Clin Microbiol Infect Dis. 2015;34:153-9. [17] Database NHIR. Taiwan. http://nhird.nhri.org.tw/en/Backgroundhtml. [cited in 2015 January].
[18] Lai SW, Liao KF, Liao CC, Muo CH, Liu CS, Sung FC. Polypharmacy correlates with increased risk for hip fracture in the elderly: a population-based study. Medicine (Baltimore). 2010;89:295-9.
[19] Liao KF, Lai SW, Li CI, Chen WC. Diabetes mellitus correlates with increased risk of pancreatic cancer: a population-based cohort study in Taiwan. J Gastroenterol Hepatol. 2012;27:709-13.
[20] Lai SW, Lin CL, Liao KF, Lin CY. Amiodarone use and risk of acute
pancreatitis: A population-based case-control study. Heart Rhythm. 2015;12:163-6. [21] Ciampolini J, Harding KG. Pathophysiology of chronic bacterial osteomyelitis. Why do antibiotics fail so often? Postgrad Med J. 2000;76:479-83.
[22] Nitsche C, Maertin S, Scheiber J, Ritter CA, Lerch MM, Mayerle J. Drug-induced pancreatitis. Curr Gastroenterol Rep. 2012;14:131-8.
[23] Chang MC, Su CH, Sun MS, Huang SC, Chiu CT, Chen MC, et al. Etiology of acute pancreatitis--a multi-center study in Taiwan. Hepatogastroenterology.
2003;50:1655-7.
[24] Chen CH, Dai CY, Hou NJ, Chen SC, Chuang WL, Yu ML. Etiology, severity and recurrence of acute pancreatitis in southern taiwan. J Formos Med Assoc. 2006;105:550-5.
[25] Drago L, Romano D, De Vecchi E, Vassena C, Logoluso N, Mattina R, et al. Bioactive glass BAG-S53P4 for the adjunctive treatment of chronic osteomyelitis of the long bones: an in vitro and prospective clinical study. BMC Infect Dis.
2013;13:584.
[26] Romano CL, Logoluso N, Meani E, Romano D, De Vecchi E, Vassena C, et al. A comparative study of the use of bioactive glass S53P4 and antibiotic-loaded calcium-based bone substitutes in the treatment of chronic osteomyelitis: a retrospective comparative study. Bone Joint J. 2014;96-B:845-50.
[27] Bugdaci MS, Oztekin E, Kara E, Koker I, Tufan A. Prognostic value of increased B type natriuretic peptide in cases with acute pancreatitis. Eur J Intern Med.
2012;23:e97-e100.
[28] Lai SW, Liao KF, Lin CL, Chen PC. Pyogenic liver abscess correlates with increased risk of acute pancreatitis: a population-based cohort study. J Epidemiol. 2015;25:246-53.
Table 1. Descriptive characteristics of cases with acute pancreatitis and controls Controls N= 30712 Cases N= 7678 Variable n (%) n (%) P value* Sex 0.99 female 10236 33.3 2559 33.3 male 20476 66.7 5119 66.7
Age group (years) 0.99
20-39 9418 30.7 2354 30.7
40-64 14590 47.5 3648 47.5
65-84 6704 21.8 1676 21.8
Age (year), mean (SD) † 50.0 16.0 50.4 15.8 0.05
Comorbidities before index date
Chronic osteomyelitis 28 0.09 22 0.29 <0.001
Alcohol-related disease 95 0.31 340 4.43 <0.001
Biliary stone 584 1.90 1587 20.7 <0.001
Cardiovascular disease 5058 16.5 1949 25.4 <0.001
Chronic kidney disease 499 1.62 338 4.40 <0.001
Chronic obstructive pulmonary disease 3665 11.9 1219 15.9 <0.001 Diabetes mellitus 2897 9.43 1541 20.1 <0.001 Hepatitis B 550 1.79 318 4.14 <0.001 Hepatitis C 278 0.91 192 2.50 <0.001 Hyperparathyroidism 18 (0.06) 19 (0.25) <0.001 Hypertriglyceridemia 1304 (4.25) 735 (9.57) <0.001 Data are presented as the number of subjects in each group, with percentages given in parentheses.
Table 2. Crude and adjustedodds ratio and 95% confidence interval of acute pancreatitis associated with chronic osteomyelitis and other comorbidities
Crude Adjusted †
Variable OR (95%CI) OR (95%CI)
Sex (male vs. female) 1.00 (0.95, 1.05) -
-Age (per one year) 1.00 (0.99, 1.003) -
-Comorbidities before index date (yes vs. no)
Chronic osteomyelitis 3.15 (1.80, 5.51) 1.93 (1.01, 3.69)
Alcohol-related disease 14.9 (11.9, 18.8) 16.4 (13.0, 20.8)
Biliary stone 13.4 (12.2, 14.8) 12.9 (11.7, 14.3)
Cardiovascular disease 1.73 (1.63, 1.83) 1.10 (1.02, 1.18)
Chronic kidney disease 2.79 (2.42, 3.21) 1.93 (1.65, 2.26)
Chronic obstructive pulmonary disease 1.39 (1.30, 1.49) 0.99 (0.91, 1.07)
Diabetes mellitus 2.41 (2.25, 2.58) 1.92 (1.77, 2.07)
Hepatitis B 2.37 (2.06, 2.73) 2.01 (1.72, 2.26)
Hepatitis C 2.81 (2.33, 3.38) 1.76 (1.42, 2.17)
Hyperparathyroidism 4.23 (2.22, 8.06) 2.61 (1.27, 5.35)
Hypertriglyceridemia 2.39 (2.17, 2.62) 1.70 (1.53, 1.89)
†Adjustment for alcohol-related disease, biliary stone, cardiovascular disease, chronic kidney
disease, chronic obstructive pulmonary disease, diabetes mellitus, hepatitis B, hepatitis C, hyperparathyroidism and hypertriglyceridemia