Decreased risk of stroke in patients receiving traditional Chinese medicine for vertigo: A population-based cohort study
Tzung-Yi Tsaia, b, c, Chung-Yi Lid, e, Hanoch Livnehf, I-Hsin Ling, Ming-Chi Luh, i, Chia-Chou Yehg, j, ,
a Department of Medical Research, Dalin Tzuchi Hospital, The Buddhist Tzuchi Medical Foundation, 2 Minsheng Road, Dalin Township, Chiayi 62247, Taiwan
b Department of Environmental and Occupational Health, College of Medicine, National Cheng Kung University, 138 Sheng-Li Road, Tainan 70428, Taiwan
c Department of Nursing, Tzu Chi College of Technology, 880 Chien-Kuo Road Section 2, Hualien 97004, Taiwan
d Department of Public Health, College of Medicine, National Cheng Kung University, 138 Sheng-Li Road, Tainan 70428, Taiwan
e Department of Public Health, College of Public Health, China Medical University, 91 Hsueh-Shih Road, Taichung 40402, Taiwan
f Rehabilitation Counseling Program, Portland State University, Portland, OR 97207-0751, USA
g School of Post-Baccalaureate Chinese Medicine, Tzu Chi University, 701 Jhongyang Road Section 3, Hualien 97004, Taiwan
h Division of Allergy, Immunology and Rheumatology, Dalin Tzuchi Hospital, The Buddhist Tzuchi Medical Foundation, 2 Minsheng Road, Dalin Township, Chiayi 62247, Taiwan
i School of Medicine, Tzu Chi University, 701 Jhongyang Road Section 3, Hualien 97004, Taiwan
j Department of Chinese Medicine, Dalin Tzuchi Hospital, The Buddhist Tzuchi Medical Foundation, 2 Minsheng Road, Dalin Township, Chiayi 62247, Taiwan
Abstract
Ethnopharmacological relevance
Patients with vertigo are reported to exhibit a higher risk of subsequent stroke. However, it remains unclear if Traditional Chinese Medicine (TCM), the most common form of complementary and alternative medicine, can help lower the risk of stroke for these patients. So the aim of the study was to investigate the effects of TCM on stroke risk among patients with vertigo.
Materials and methods
This longitudinal cohort study used the Taiwanese National Health Insurance Research Database to identify 112,458 newly diagnosed vertigo patients aged ≥20 years who received treatment between 1998 and 2007. Among these patients, 53,203 (47.31%) received TCM after vertigo onset (TCM users), and the remaining 59,201 patients were designated as a control group (non-TCM users). All enrollees received follow-up until the end of 2012 to measure stroke incidence. Cox proportional hazards regression was used to compute the hazard ratio (HR) of stroke in recipients of TCM services.
Results
During 15-year follow-up, 5532 TCM users and 12,295 non-TCM users developed stroke, representing an incidence rate of 13.10% and 25.71% per 1000 person-years. TCM users had a significantly reduced risk of stroke compared to non-TCM users (adjusted HR=0.64; 95% confidence interval CI=0.59-0.74). The predominant effect was observed for those receiving TCM for more than 180 days (adjusted HR=0.52;
95% CI=0.49–0.56). Commonly used TCM formulae, including Ban-Xia-Bai-Zhu-Tian-Ma-Tang, Ling-Gui-Zhu-Gan-Tang, Bai Zhi (Angelica dahurica (Hoffm.) Benth. & Hook.f. ex Franch. & Sav., root), Ge Gen (Pueraria lobata (Willd.) Ohwi, root) and Hai Piao Xiao (Endoconcha Sepiae, Cuttlefish Bone) were significantly associated with lower risk of stroke.
Conclusions
Results of this population-based study support the effects of TCM on reducing stroke risk, and may provide a reference for stroke prevention strategies. The study results may also help to integrate TCM into clinical intervention programs that provide a favorable prognosis for vertigo patients.
Keywords
Cohort study; Stroke;
Traditional Chinese medicine; Vertigo
1. Introduction
Vertigo is a subtype of dizziness that is defined as an illusion of movement, and usually a sense of rotation. As such, vertigo is a common symptom of vertebrobasilar ischemia (VBI) and posterior inferior cerebellar artery (PICA) infarction (Lee et al., 2014a). Medications for treating vertigo have typically consisted of antivertiginous and antiemetic drugs, which were used mainly used to relieve symptoms of dizziness (Baloh, 1998). However, to date, no medication in daily practical use has been well established for its curative or prophylactic value or has been considered suitable for long-term palliative use (Ozdemir et al., 2013 and Yardley et al., 2004). Therefore, the related health threat of vertigo has attracted more attention. Results of a recent study showed that dizziness or vertigo was a major risk factor for subsequent vascular events (Lee et al., 2012).
Traditional Chinese Medicine (TCM) has been an important part of health care in Taiwan for centuries and continues to have growing popularity in Taiwan and many other Asian countries. In fact, TCM is fully reimbursed under the current Taiwanese National Health Insurance (NHI) system (Pan et al., 2014 and Tsai et al., 2014). TCM physicians are specialized practitioners who use meticulous approaches to gather patients' clinical symptoms and signs, which are then used to make diagnoses and determine treatment strategies (Hsu et al., 2014). As explained above, dizziness and vertigo occur frequently in vertebrobasilar ischemia (Lee et al., 2014a). In such cases, physicians may consider prescribing traditional Chinese herbal medicine (Han et al., 2015, Liu et al., 2015 and Xie et al., 2014). Results of a previous study indicated that acupuncture can improve cerebral blood flow in patients with vertigo induced by
been conducted to address whether TCM can affect the risk of developing stroke in patients with vertigo. Therefore, to address this concern, this study aimed was to assess the risk of stroke incidence among vertigo patients who either received or did not receive TCM services.
2. Material and methods
2.1. Data source
This retrospective cohort study used claims data from the Longitudinal Health
Insurance Database (LHID) of the Taiwan National Health Insurance Administration, whose information is made available to Taiwanese researchers. Taiwan launched the single-payer NHI program in 1995 to remove financial barriers to medical care for all legal residents. As of 2010, over 99% of Taiwan's population was enrolled in this program (National Health Research Institute, 2011). The LHID is a sub-dataset of the NHI program made up of 1,000,000 randomly sampled people who were alive in 2000. For this study, all medical records of these individuals were collected from 1997 to 2012. Because a multistage stratified systematic sampling method was used, no statistically significant differences regarding sex or age existed between the one million insured individuals and the general population (National Health Research Institute, 2011). This database contains all NHI enrolment files, claims data, and the registry for prescription drugs, providing comprehensive utilization information for the subjects covered by the insurance program. To date, more than 300 published papers have used this de-identified secondary database for their studies. The present study was conducted in accordance with the Helsinki Declaration and was also evaluated and approved by the local institutional review board and ethics committee of Buddhist Dalin Tzu Chi Hospital, Taiwan (No. B10004021-1). Since the LHID files contained only de-identified secondary data, the review board waived the requirement for obtaining informed consent from the patients.
Selection of study subjects is shown in Fig. 1. All diagnoses in the insurance claims data were coded with the International Classification of Disease, 9th Revision, Clinical Modification (ICD-9-CM). Inclusion criteria for the study cohort were: patients aged 20 years or older with newly diagnosed vertigo within the 1998-2007 time period (ICD-9-CM codes: 078.81, 386.XX, or 780.4). The index date was defined as the day of vertigo diagnosis. To reduce concerns of disease
misclassification, only those patients with at least three diagnoses in outpatient visits or those being admitted to a hospital with a primary diagnosis of vertigo within the observational period (n=125,640) were selected. A total of 9664 vertigo patients were then excluded because they had a prior diagnosis of stroke (ICD-9-CM: 430–437) as indicated by linking the vertigo patients to the catastrophic illness registry. In Taiwan, insured residents with major diseases (e.g., cancer, autoimmune diseases, chronic renal failure) can apply for a catastrophic illness certificate that grants exemption from co-payment. Those with a follow-up period <3 months were also excluded (n=3518). Finally, after these exclusions, the data of 112,458 vertigo patients were retained for analysis.
In Taiwan, only certified practitioners of Chinese medicine are entitled to provide TCM services. As proposed by the existing rule (Lee et al., 2014b), the frequency of patients' visits for TCM was used to verify the TCM exposure of each study subject. Vertigo patients who received TCM for more than 30 days were designated as TCM users, whereas those treated for 30 days or less were designated as non-TCM users. Follow-up person-years (PYs) of the non-TCM users were determined by calculating the time interval from the index date to the earliest diagnosis of stroke, date of withdrawal from the insurance plan, or study end-date of December 31, 2012, whichever of these dates came first. PYs of the TCM users were calculated from the
initiation of TCM services corrected by immortal time bias (selection bias), as previously described (Shariff et al., 2008).
2.3. Demographic characteristics and comorbidities
Demographic characteristics evaluated in this study included age, gender, income for estimating insurance payments, availability of TCM resources, and urbanization level of subjects' residential areas. Subjects' monthly incomes were stratified into 3 levels: ≤New Taiwan Dollar (NTD) 17,880, NTD 17,881–NTD 43,900, and ≥NTD 43,901. Urbanization levels were divided into 3 strata by population: urban (levels 1–2), suburban (levels 3–4), and rural (levels 5–7) areas. Level 1 refers to the “most urbanized” and level 7 refers to the “least urbanized” communities (Liu et al., 2006). The baseline comorbidities were evaluated by using the established Charlson-Deyo comorbidity index (Deyo et al., 1992), which is based on individual medical records one year prior to initial cohort entry.
2.4. Statistical analysis
Differences between the demographic characteristics and comorbidities of TCM users versus non-TCM users were analyzed using the χ2 test and students t-test. Cox
proportional hazards regression analysis was then applied to compute the hazard ratio (HR) with 95% confidence intervals of stroke risk in association with TCM use. To test the robustness of the relationship between TCM use and stroke risk, TCM users were divided into two subgroups, one group that used TCM for 30–180 days and another group that used TCM for more than 180 days. The relative risk of stroke between TCM users and non-TCM users was assessed by employing stratified analysis by age and gender using Cox proportional hazards regression. The
proportional-hazards assumption was verified using plots of log (−log(survival function)) versus log(time) and Schoenfeld residuals versus time. All statistical analyses were conducted using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA). P<0.05 was established as statistical significance.
3. Results
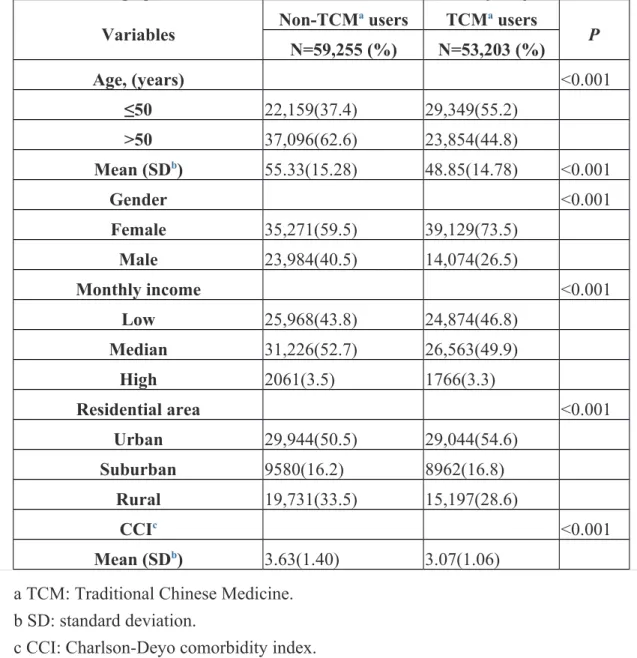
A total of 112,458 patients with vertigo were identified in the insurance database who received treatment during the period of 1998-to-2007. Of these, 53,203 subjects received TCM services (TCM users) and 59,255 did not (non-TCM users). Table 1 shows the basic characteristics of the TCM and non-TCM users. Compared to the non-TCM users, vertigo patients receiving TCM services were more likely to be female, younger, have lower monthly income and CCI scores, and to reside in an urban area (all P<0.001).
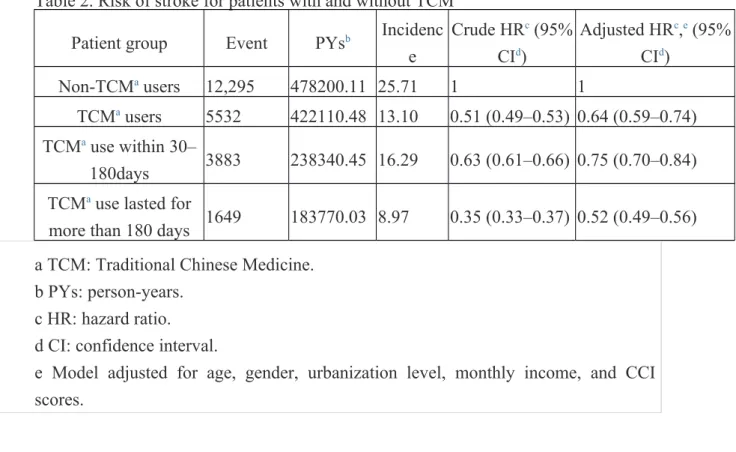
Among 422110.48 PYs observed, 5532 TCM users developed stroke.
Correspondingly, among 478,200.11 non-TCM users 12,295 had stroke events. Therefore, the incidence rate of stroke was lower in TCM users than in non-TCM users (13.10 vs. 25.71 per 1000 PYs), with an adjusted HR of 0.64 (95% CI=0.59-0.74) (Table 2). TCM users receiving services for more than 180 days were associated with a predominantly reduced risk of subsequent stroke by a magnitude of 48% (95% CI=0.49–0.56).
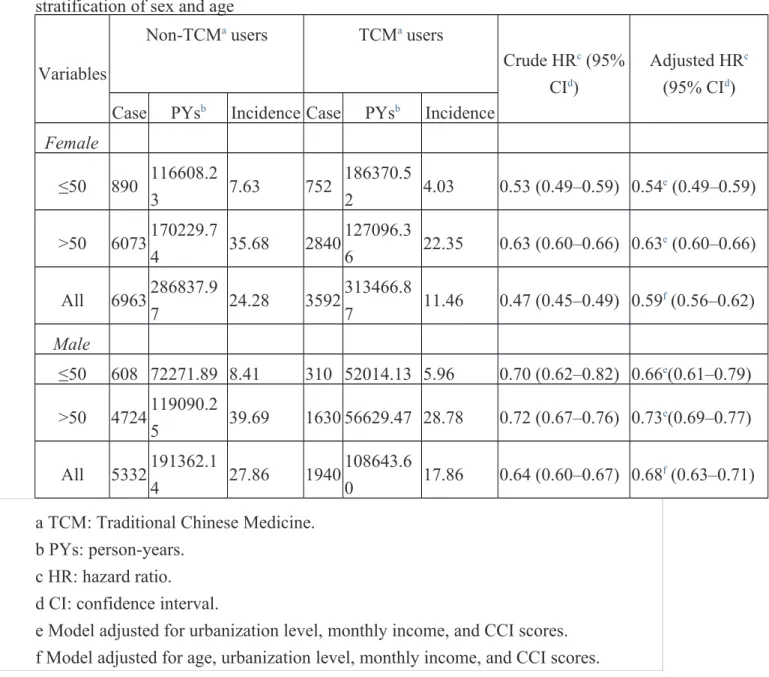
Regarding gender-specific risk of stroke, both female and male TCM users showed significantly decreased risk of stroke, with an adjusted HR of 0.59 (95% CI=0.56– 0.62) and 0.68 (95% CI=0.63–0.71), respectively (Table 3). A significant interaction between age and sex was noted in association with TCM use. Therefore, a stratified analysis by age and sex was performed to determine the effect of TCM on stroke risk (Table 3). Collectively, significant beneficial effects of TCM were observed in younger vertigo patients, regardless of their sex. In males, decreases in adjusted HR were greater for TCM users aged ≤50 years (aHR=0.66; 95% CI=0.61–0.79); in
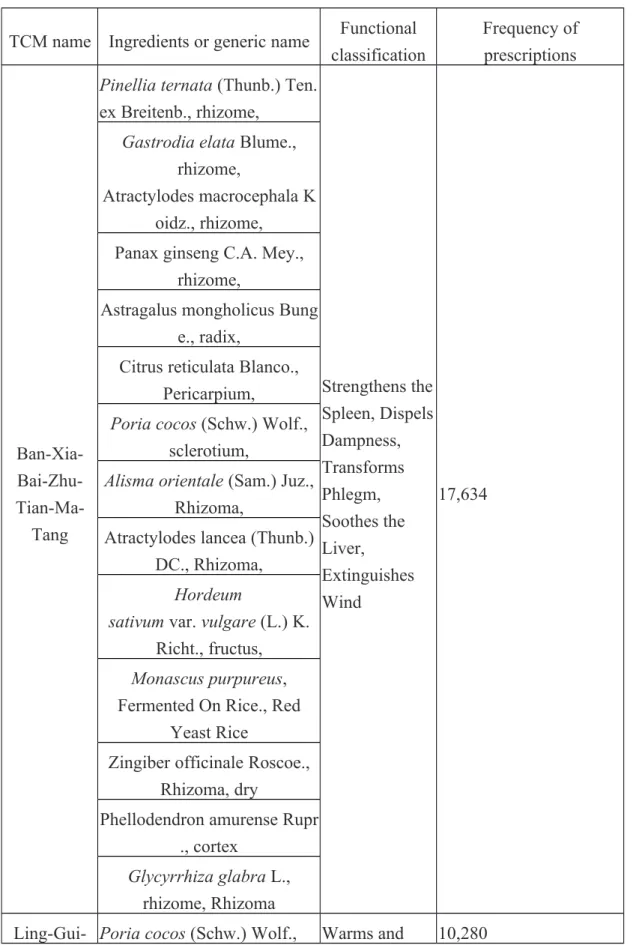
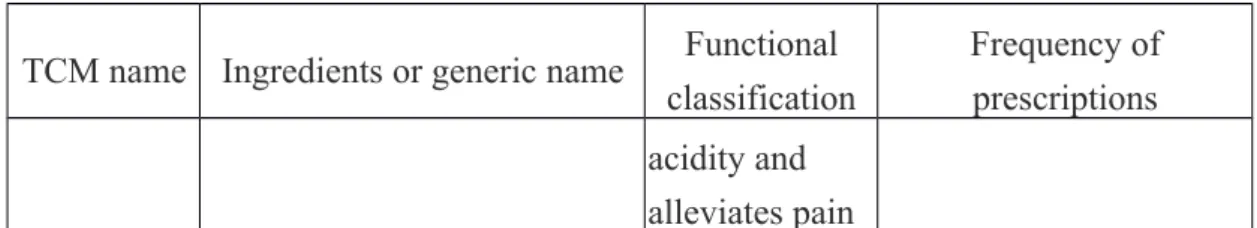
females, greater reductions in risk of stroke were observed in vertigo patients aged≦50 years (aHR=0.54; 95% CI=0.49–0.59). Additionally, the commonly prescribed herbal formulae for TCM users are summarized in Table 4. Ban-Xia-Bai-Zhu-Tian-Ma-Tang was the most frequently used herbal formula, followed by Ling-Gui-Zhu-Gan-Tang and Tian Ma. Of these 10 herbal formulae used, Ban-Xia-Bai-Zhu-Tian-Ma-Tang, Ling-Gui-Zhu-Gan-Tang, Bai Zhi, Ge Gen, and Hai Piao Xiao were found to be significantly associated with the lower risk of stroke (Table 5).
4. Discussion
To the best of our knowledge, this is the first evidence-based cohort study applying a large nationwide claims-based data source to address the association between TCM services and stroke risk among vertigo patients. The use of this large cohort allowed the more potent application of a multidisciplinary collaborative approach.
Results of this 15-year follow-up study suggest that vertigo patients who received TCM have a nearly 42% lower risk of stroke than those who did not receive TCM services, echoing findings of previous reports (Deng et al., 2015 and Liao et al., 2012). Furthermore, in the present study, stratified analysis for stroke risk subsequent to TCM intervention indicated that younger vertigo subjects (aged 50 years or
younger), regardless of gender, have the lowest adjusted HR for stroke risk after receiving TCM services. A likely explanation for this finding is that younger patients have fewer cardiovascular risk factors than older patients (Nacu et al., 2015), and traditional herbal medicines are noted for having a vascular protective effect on ischemic brain damage (Bu et al., 2013).
According to TCM concepts, vertigo is caused by a loss of nourishment in the upper orifices as a result of pathogenic wind, heat, phlegm, and energy deficiency or stasis. Vertigo symptoms are thought to be closely related to the functioning of the liver, kidney, heart, and spleen (Deng et al., 2015). The commonly used herbal formulae of TCM aim to treat vertigo patients according to the TCM functional classifications shown in Table 4. Ban-Xia-Bai-Zhu-Tian-Ma-Tang are typically used for wind phlegm, qi stagnation, stomach and spleen qi deficiency. Symptoms caused by such deficiencies may include vertigo, dizziness, headache, nausea, vomiting, excessive
sputum, chronic fatigue, hypertension, and gastrointestinal disorders found in clinical therapy. Recent scientific evidence has demonstrated that Ban-Xia-Bai-Zhu-Tian-Ma-Tang, including Tian Ma, successfully treated dementia and migraine (Chang et al., 2014 and Lin et al., 2015). Tian Ma is used to treat clinical conditions such as
headache, dizziness, and convulsion, and also provides sedative effects against vertigo and paralysis (Chen and Sheen, 2011 and Ojemann et al., 2006). In TCM practice, Gastrodiae Rhizoma (Tian Ma) and Gastrodia elata (Ge Gen) are often used together in Chinese clinical prescriptions. Injections of these TCM formulae are used in combinations for treatment of certain cardiocerebrovascular diseases treated in clinics, especially for treatment of vertigo due to vertebrobasilar ischemia. The bioactive substances of Tian Ma and Ge Gen are gastrodin and puerarin. The clinical effects of these substances on vasodilatation are close to those of verapamil ( Jiang et al., 2013). Another frequently prescribed medication in China and Taiwan, Ling-Gui-Zhu-Gan-Tang, is also used in other Asian countries to treat bronchial asthma, chronic
bronchitis, vertigo (Meniere's syndrome), heart palpitations, heart valve disease, hypertension, and ear problems.
Research also indicates that Ling-Gui-Zhu-Gan-Tang can successfully treat stress-induced pathophysiological conditions (Ding et al., 2005 and Wang et al., 2007). For example, Bai Zhi has been used in TCM to treat migraine headaches (Liang et al., 2012). Migraines often overlap with symptoms of other causes of dizziness, especially Ménière's disease, and benign paroxysmal positional vertigo, as well as vertigo of central or peripheral origin.
Another TCM, Bai Zhi, effectively targets the 5-HT receptors located in the cerebellum and the lateral vestibular nucleus that influence depressive symptoms
(Ahn et al., 2009). Bai Zhi possesses robust antidepressant efficacy, mediated by activation of 5-HT receptors (Gu et al., 2014). Although Bai Zhi is used in traditional Chinese medicine to treat harmful external influences on the skin, including cold, heat, dampness and dryness (Li et al., 1991), its potential use for treating depression has been noted. In the present study, all of above mentioned TCM services are associated with relieving the symptoms of vertigo and decreasing the risk of developing stroke.
The strengths of this study include the immediate availability of data, the
comprehensiveness of the database, and the statistical power derived from the large sample size, all of which limit the possibility of selection bias and provide results that can be a valuable basis for policymaking. In addition, this 15-year follow-up study allowed us to examine the effects of TCM confidently on the association between vertigo and the risk of stroke over a long latency period. Despite the above strengths, several limitations should be noted when interpreting results of the present study. First, the identification of TCM exposure and outcomes were based on the ICD-9-CM, and misclassification is possible. To minimize this error, we selected subjects with either vertigo or stroke only after they were recorded as having at least three outpatient visits reporting consistent diagnoses or one inpatient admission. It should also be noted that the NHI of Taiwan randomly samples claims from hospitals, interviews patients, and reviews medical charts to verify the accuracy of medical records. Second, information on smoking, social network relationships, religious beliefs, and educational level was unavailable from the claims data. Smoking is an important risk factor associated with stroke. The failure to adjust for the confounding effect of smoking could possibly lead to biased estimates of risk of stroke in our
stroke for vertigo patients receiving TCM regardless of gender, while the smoking rate for females and males in Taiwan are 4.3% and 46.8%, respectively (Wen et al., 2005). This observation suggests that the confounding effect of smoking was unlikely to compromise the results of this study. Third, we were unable to contact the enrolled patients directly regarding use of Chinese herbs due to the anonymity of identification numbers in the database. However, nearly 95% of dosing frequencies in Chinese herbs are typically only used for one week in clinical practice, so those who continued to receive the same prescription for a longer period of time were therefore likely to have consumed the prescribed medication (Lai et al., 2010). Additionally,
prescriptions for medications issued before 1996 were not reflected in data analysis in the present study. This omission could possibly result in underestimating the
cumulative frequencies and may weaken the effect of the specified Chinese herbal products.
5. Conclusions
Results of this 15-year follow-up cohort study suggest that the use of TCM during treatment of vertigo was associated with a 36% lower risk of developing stroke compared to the risk among non-TCM users. These findings could serve as a reference for healthcare providers to help establish more effective therapeutic interventions to improve the prognosis of patients with vertigo
Authors' contributions
Conceived and designed the experiments: TYT, CCH. Performed the experiments: TYT. Analyzed the data: TYT, CYL. Contributed reagents/material/analysis tools: HL/IHL/MCL. Wrote the paper: TYT, CCH.
Conflict of interest
The authors have no conflicts of interest to declare.
Acknowledgements
This study is based in part on data from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health and managed by the National Health Research Institutes. The interpretation and conclusions contained herein do not represent those of the Taiwan Bureau of National Health Insurance, Department of Health or the National Health Research Institutes. This research was supported by Buddhist Dalin Tzuchi Hospital (Grant number DTCRD101-E-08). Tsai TY and Li CY contributed equally in this work.
References
Ahn, S.K., Khalmuratova, R., Jeon, S.Y., Kim, J.P., Park, J.J., Hur, D.G., Kim, D.W., Balaban, C.D., 2009. Colocalization of 5-HT1F receptor and glutamate in neurons of the vestibular nuclei in rats. Neuroreport 20, 111–115.
Baloh, R.W., 1998. Vertigo. Lancet 352, 1841–1846.Bu, Y., Lee, K., Jung, H.S., Moon, S.K., 2013. Therapeutic effects of traditional herbal medicine on cerebral ischemia: a perspective of vascular protection. Chin. J. Integr. MEd. 19, 804–814.
Chang, Y.Y., Tsai, Y.T., Lai, J.N., Yeh, C.H., Lin, S.K., 2014. The traditional Chinese medicine prescription patterns for migraine patients in Taiwan: a populationbased study. J. Ethnopharmacol. 151, 1209–1217.
Chen, P.J., Sheen, L.Y., 2011. Gastrodiae Rhizoma (Iān Ma): a review of biological activity and antidepressant mechanisms. J. Tradit. Complement. Med. 1, 31–40.
Deng, S.Z., Zhao, X.F., Huang, L.H., He, S., Wen, Y., Zhang, C., Tian, G., Wang, T.,Wu, F.F., Meng, Z.H., Shi, X.M., 2015. The quantity-effect relationship and physiological mechanisms of different acupuncture manipulations on posterior circulation ischemia with vertigo: study protocol for a randomized controlled trial. Trials 16, 152.
Deyo, R.A., Cherkin, D.C., Ciol, M.A., 1992. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J. Clin. Epidemiol. 45, 613–619.
Ding, G., Yu, G., Zhang, J., Liang, S., Liu, L., Huang, P., Chen, H., Xiao, A., Li, X., Cai, Y., 2005. The therapeutic effects of Ling-Gui-Zhu-Gan-Tang mixture in 50 psychotic patients with obesity induced by the psychoactive drugs. J. Tradit. Chin. Med. 25, 25–28.
Gu, X., Zhou, Y., Wu, X., Wang, F., Zhang, C.Y., Du, C., Shen, L., Chen, X., Shi, J., Liu, C., Ke, K., 2014. Antidepressant-like effects of auraptenol in mice. Sci. Rep. 4, 4433.
Han, L., Liu, E., Kojo, A., Zhao, J., Li, W., Zhang, Y., Wang, T., Gao, X., 2015. Qualitative and quantitative analysis of Eclipta Prostrata L. by LC/MS. Sci. World J. 2015, 15.
Hsu, P.C., Tsai, Y.T., Lai, J.N., Wu, C.T., Lin, S.K., Huang, C.Y., 2014. Integrating traditional Chinese medicine Healthcare into diabetes care by reducing the risk of developing kidney failure among type 2 diabetic patients: a population-based case control study. J. Ethnopharmacol. 156, 358–364.
Jiang, L., Dai, J., Huang, Z., Du, Q., Lin, J.,Wang, Y., 2013. Simultaneous
determination of gastrodin and puerarin in rat plasma by HPLC and the application to their interaction on pharmacokinetics. J. Chromatogr. B. Anal. Technol. Biomed. Life Sci., 915–916.
Lai, M.N.,Wang, S.M., Chen, P.C., Chen, Y.Y.,Wang, J.D., 2010. Population-based casecontrol study of Chinese herbal products containing aristolochic acid and urinary tract cancer risk. J. Natl. Cancer Inst. 102, 179–186.
Lee, C.C., Ho, H.C., Su, Y.C., Chiu, B.C.H., Su, Y.C., Lee, Y.D., Chou, P., Chien, S.H., Huang, Y.S., 2012. Increased risk of vascular events in emergency room patients discharged home with diagnosis of dizziness or vertigo: a 3-year follow-up study. PLoS One 7, e35923.
Lee, J.O., Park, S.H., Kim, H.J., Kim, M.S., Park, B.R., Kim, J.S., 2014a.
Vulnerability of the vestibular organs to transient ischemia: implications for isolated vascular vertigo. Neurosci. Lett. 558, 180–185.
Lee, Y.W., Chen, T.L., Shih, Y.R., Tsai, C.L., Chang, C.C., Liang, H.H., Tseng, S.H., Chien, S.C., Wang, C.C., 2014b. Adjunctive traditional Chinese medicine therapy improves survival in patients with advanced breast cancer: a population-based study. Cancer 120, 1338–1344.
Li, H., Dai, Y., Zhang, H., Xie, C., 1991. Pharmacological studies on the Chinese drug radix angelicae dahuricae. Zhongguo Zhong Yao ZA Zhi 16, 560–562.
Liang, X.L., Liao, Z.G., Zhu, J.Y., Zhao, G.W., Yang, M., Yin, R.L., Cao, Y.C., Zhang, J., Zhao, L.J., 2012. The absorption characterization effects and mechanism of radix angelicae dahuricae extracts on Baicalin in Radix Scutellariae using in vivo and in vitro absorption models. J. Ethnopharmacol. 139, 52–57.
Liao, C.C., Lin, J.G., Tsai, C.C., Lane, H.L., Su, T.C., Wang, H.H., Sung, F.C., Chen, T.L., Shih, C.C., 2012. An investigation of the use of traditional Chinese medicine in stroke patients in Taiwan. Evid. Based Complement. Altern. Med. 2012, 8.
Lin, S.K., Tsai, Y.T., Lai, J.N., Wu, C.T., 2015. Demographic and medication characteristics of traditional Chinese medicine users among dementia patients in Taiwan: a nationwide database study. J. Ethnopharmacol. 161, 108–115.
Liu, C.Y., Hung, Y.T., Chuang, Y.L., Chen, Y.J., Weng, W.S., Liu, J.S., Liang, K.Y., 2006. Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J. Health Manag. 4, 1–22.
Liu, W., Yi, D.D., Guo, J.L., Xiang, Z.X., Deng, L.F., He, L., 2015. Nuciferine, extracted from Nelumbo nucifera Gaertn, inhibits tumor-promoting effect of nicotine involving Wnt/β-Catenin signaling in non-small cell lung cancer. J.
Ethnopharmacol.165, 83–93.
Nacu, A., Fromm, A., Sand, K.M., Waje-Andreassen, U., Thomassen, L., Naess, H., 2015. Age dependency of ischaemic stroke subtypes and vascular risk factors in western Norway: the Bergen Norwegian stroke cooperation study. Acta Neurol. Scand. 133, 202–207.
National Health Research Institute, Longitudinal Health Insurance Research Database. 〈http://nhird.nhri.org.tw/date_cohort.html〉, 2011.
Ojemann, L.M., Nelson, W.L., Shin, D.S., Rowe, A.O., Buchanan, R.A., 2006. Tian ma, an ancient Chinese herb, offers new options for the treatment of epilepsy and other conditions. Epilepsy Behav. 8, 376–383.
Ozdemir, H., Akinci, E., Coskun, F., 2013. Comparison of the effectiveness of intravenous piracetam and intravenous dimenhydrinate in the treatment of acute peripheral vertigo in the emergency department. Singap. Med. J. 54, 649–652.
Pan, J.C., Tsai, Y.T., Lai, J.N., Fang, R.C., Yeh, C.H., 2014. The traditional Chinese medicine prescription pattern of patients with primary dysmenorrhea in Taiwan: a large-scale cross sectional survey. J. Ethnopharmacol. 152, 314–319.
Shariff, S.Z., Cuerden, M.S., Jain, A.K., Garg, A.X., 2008. The secret of immortal time bias in Epidemiologic studies. J. Am. Soc. Nephrol. 19, 841–843.
Tsai, Y.T., Lai, J.N., Wu, C.T., 2014. The use of Chinese herbal products and its influence on tamoxifen induced endometrial cancer risk among female breast cancer patients: a population-based study. J. Ethnopharmacol. 155, 1256–1262.
Wang, L., Muxin, G., Nishida, H., Shirakawa, C., Sato, S., Konishi, T., 2007.
Psychological stress-induced oxidative stress as a model of sub-healthy condition and the effect of TCM. Evid. Based Complement. Altern. Med. 4, 195–202.
Wen, C.P., Levy, D.T., Cheng, T.Y., Hsu, C.C., Tsai, S.P., 2005. Smoking behaviour in Taiwan, 2001. Tob. Control, Suppl 1, i51-i55.
Xie, Q., Li, Y.Y., Xie, Y.M., Yang, W., Zhao, W., Zhuang, Y., Wang, Y.Y., 2014. Characteristics and drug analysis associated with vertigo disease in real world. Zhongguo Zhong Yao ZA Zhi 39, 3514–3518.
Yardley, L., Donovan-Hall, M., Smith, H.E., Walsh, B.M., Mullee, M., Bronstein, A.M., 2004. Effectiveness of primary care–based vestibular rehabilitation for chronic dizziness. Ann. Intern. Med. 141, 598–605.
Table 1. Demographic data and selected comorbidities of the study subjects Variables Non-TCM a users TCMa users P N=59,255 (%) N=53,203 (%) Age, (years) <0.001 ≤50 22,159(37.4) 29,349(55.2) >50 37,096(62.6) 23,854(44.8) Mean (SDb) 55.33(15.28) 48.85(14.78) <0.001 Gender <0.001 Female 35,271(59.5) 39,129(73.5) Male 23,984(40.5) 14,074(26.5) Monthly income <0.001 Low 25,968(43.8) 24,874(46.8) Median 31,226(52.7) 26,563(49.9) High 2061(3.5) 1766(3.3) Residential area <0.001 Urban 29,944(50.5) 29,044(54.6) Suburban 9580(16.2) 8962(16.8) Rural 19,731(33.5) 15,197(28.6) CCIc <0.001 Mean (SDb) 3.63(1.40) 3.07(1.06) a TCM: Traditional Chinese Medicine.
b SD: standard deviation.
Table 2. Risk of stroke for patients with and without TCM
Patient group Event PYsb Incidenc
e Crude HRc (95% CId) Adjusted HRc,e (95% CId) Non-TCMa users 12,295 478200.11 25.71 1 1 TCMa users 5532 422110.48 13.10 0.51 (0.49–0.53) 0.64 (0.59–0.74) TCMa use within 30– 180days 3883 238340.45 16.29 0.63 (0.61–0.66) 0.75 (0.70–0.84)
TCMa use lasted for
more than 180 days 1649 183770.03 8.97 0.35 (0.33–0.37) 0.52 (0.49–0.56)
a TCM: Traditional Chinese Medicine. b PYs: person-years.
c HR: hazard ratio. d CI: confidence interval.
e Model adjusted for age, gender, urbanization level, monthly income, and CCI scores.
Table 3. Incidence and stroke risk for vertigo patients with and without TCM in the stratification of sex and age
Variables
Non-TCMa users TCMa users
Crude HRc (95%
CId)
Adjusted HRc
(95% CId)
Case PYsb Incidence Case PYsb Incidence
Female ≤50 890 116608.2 3 7.63 752 186370.5 2 4.03 0.53 (0.49–0.59) 0.54 e (0.49–0.59) >50 6073170229.7 4 35.68 2840 127096.3 6 22.35 0.63 (0.60–0.66) 0.63 e (0.60–0.66) All 6963286837.9 7 24.28 3592 313466.8 7 11.46 0.47 (0.45–0.49) 0.59 f (0.56–0.62) Male ≤50 608 72271.89 8.41 310 52014.13 5.96 0.70 (0.62–0.82) 0.66e(0.61–0.79) >50 4724119090.2 5 39.69 1630 56629.47 28.78 0.72 (0.67–0.76) 0.73 e(0.69–0.77) All 5332191362.1 4 27.86 1940 108643.6 0 17.86 0.64 (0.60–0.67) 0.68 f (0.63–0.71)
a TCM: Traditional Chinese Medicine. b PYs: person-years.
c HR: hazard ratio. d CI: confidence interval.
e Model adjusted for urbanization level, monthly income, and CCI scores. f Model adjusted for age, urbanization level, monthly income, and CCI scores.
Table 4. Top ten commonly prescribed herbal formulae for treating vertigo in TCM services during study period.
TCM name Ingredients or generic name Functional
classification Frequency of prescriptions Ban-Xia- Bai-Zhu- Tian-Ma-Tang
Pinellia ternata (Thunb.) Ten.
ex Breitenb., rhizome, Strengthens the Spleen, Dispels Dampness, Transforms Phlegm, Soothes the Liver, Extinguishes Wind 17,634
Gastrodia elata Blume.,
rhizome,
Atractylodes macrocephala K oidz., rhizome,
Panax ginseng C.A. Mey., rhizome,
Astragalus mongholicus Bung e., radix,
Citrus reticulata Blanco., Pericarpium,
Poria cocos (Schw.) Wolf.,
sclerotium,
Alisma orientale (Sam.) Juz.,
Rhizoma,
Atractylodes lancea (Thunb.) DC., Rhizoma,
Hordeum
sativum var. vulgare (L.) K.
Richt., fructus,
Monascus purpureus,
Fermented On Rice., Red Yeast Rice
Zingiber officinale Roscoe., Rhizoma, dry
Phellodendron amurense Rupr ., cortex
Glycyrrhiza glabra L.,
TCM name Ingredients or generic name Functional classification Frequency of prescriptions Zhu-Gan-Tang sclerotium transforms Phlegm and congested Fluids, Strengthens the Spleen, Resolves Dampness, Improves metabolic function Cinnamomum loureiroi Nees.
ramulus
Atractylodes macrocephala
Koidz., rhizome
Glycyrrhiza glabra L., rhizome, honeyed.
Ge Gen Pueraria lobata (Willd.)
Ohwi, rhizoma Discharges Exterior conditions and releases the muscles, especially of the neck and upper back
6360
Gou Teng
Uncaria rhynchophylla (Miq.) Miq. ex Havil., stems with hooks Extinguishes Wind and alleviates spasms 6123
Tian Ma Gastrodia elata Blume.,
rhizoma
Extinguishes Wind, calms the Liver and stops spasms and tremors
5607
Man Jing Zi Vitex trifolia L., fructus
Disperses Wind and clears Heat
5166
Bai Zhi Angelica dahurica (Hoffm.)
Benth. & Hook.f. ex Franch. & Sav., rhizoma
Expels
Wind, eliminat es Dampness, unblocks the
TCM name Ingredients or generic name Functional classification Frequency of prescriptions nasal passages, dispels Cold and alleviates pain
Dan Shen Salvia miltiorrhiza Bunge.,
rhizoma Invigorates the Blood and dispels Blood Stasis 3504 Tian-Ma- Gou-Teng-Yin
Gastrodia elata Blume.,
rhizoma, Uncaria
rhynchophylla (Miq.) Miq. ex
Havil., stems with hooks,
Calms the Liver,Extinguis hes Wind, Clears Heat, Invigorates the Blood, Tonifies the Liver and Kidneys
3293
Haliotis diversicolor Reeve.,
shell,
Gardenia jasminoides J.Ellis., fructus
Scutellaria baicalensis Georgi. , rhizome
Leonurus
heterophyllus Sweet. Herba
Cyathula officinalis K.C. Kuan., root
Eucommia ulmoides Oliv., dried bark
Taxillus chinensis (DC.) Danser., Herba
Polygonum molliiforme Boiss ., rhizoma
Poria cocos (Schw.) Wolf.,
sclerotium Hai Piao Xiao Endoconcha Sepiae, Cuttlefish Bone Restrains, holds in and stops bleeding, 1783
TCM name Ingredients or generic name Functional classification Frequency of prescriptions acidity and alleviates pain
Table 5. Risk of stroke in relation to the top 10 commonly used herbal formulae Crude HRa (95% CIb) Adjusted HRa,c (95% CI b) Ban-Xia-Bai-Zhu-Tian-Ma-Tang 0.78(0.71–0.85) 0.81(0.72–0.92) Ling-Gui-Zhu-Gan-Tang 0.67(0.59–0.75) 0.80(0.70–0.90) Tian Ma 0.93(0.79–1.12) 0.97(0.82–1.15) Gou Teng 0.83(0.71–0.95) 0.95(0.82–1.09) Dan Shen 0.82(0.70–0.94) 0.92(0.80–1.07) Man Jing Zi 0.74(0.65–0.90) 0.93(0.77–1.12) Bai Zhi 0.63(0.52–0.76) 0.82(0.67–0.96) Ge Gen 0.62(0.54–0.74) 0.80(0.68–0.94) Tian-Ma-Gou-Teng-Yin 1.05(0.96–1.15) 1.02(0.89–1.17)
Hai Piao Xiao 0.73(0.58–0.94) 0.88(0.67–0.98)
a HR: hazard ratio. b CI: confidence interval.