2013/December/17
Type of manuscript: Original article
• Manuscript title: Splenectomy correlates with increased risk of pulmonary tuberculosis: a case-control study in Taiwan
• Running head: splenectomy and pulmonary tuberculosis
• Authors’ full names:
Shih-Wei Lai
1,2, I-Kuan Wang
3,4,5, Cheng-Li Lin
6,7, Hung-Jen Chen
8,9, Kuan-Fu Liao
10,11 1
School of Medicine, China Medical University and
2Department of Family Medicine, China Medical University Hospital, Taichung, Taiwan
3
Institute of Clinical Medical Science and
4Department of Internal Medicine, China Medical University, Taichung, Taiwan, and
5Division of Neprhology, China Medical University Hospital, Taichung, Taiwan
6
Department of Public Health, China Medical University and
7Management Office for Health Data, China Medical University Hospital, Taichung, Taiwan
8
Department of Respiratory Therapy, China Medical University and
9Division of Pulmonary and Critical Care Medicine and Department of Internal
Medicine, China Medical University Hospital, Taichung, Taiwan
10
Graduate Institute of Integrated Medicine, China Medical University, and
11
Department of Internal Medicine, Taichung Tzu Chi General Hospital, Taichung, Taiwan
• Corresponding author: Kuan-Fu Liao
Department of Internal Medicine, Taichung Tzu Chi General Hospital, No.66, Sec. 1, Fongsing Road, Tanzi District, Taichung City, 427, Taiwan
Phone: 886-4-2205-2121 Fax: 886-4-2203-3986
E-mail: kuanfuliao@yahoo.com.tw
Word count: 200 in the abstract, 1451 in the text, 2 tables and 19 references
Abstract
This study investigated whether there was an association between splenectomy and pulmonary tuberculosis. This was a case-control study using the database from the Taiwan National Health Insurance Program. We identified 18960 patients (aged 20 years or older) with newly diagnosed pulmonary tuberculosis as the case group and 73988 subjects without pulmonary tuberculosis as the control group from 1998 to 2011. Both groups were matched for sex, age (per 5 years) and index year of diagnosing pulmonary tuberculosis. The risk of pulmonary tuberculosis associated with splenectomy and other co-morbidities was estimated. After controlling for confounders, multivariable logistic regression analysis displayed that the odds of pulmonary tuberculosis was 1.91 in patients with splenectomy (95% CI=1.06, 3.44), as compared with the subjects without splenectomy. Chronic obstructive pulmonary diseases (OR=3.07, 95% CI=2.94, 3.21), pneumoconiosis (OR=2.20, 95% CI=1.90, 2.56), chronic kidney diseases (OR=1.49, 95% CI=1.33, 1.67), diabetes mellitus (OR=1.57, 95% CI=1.50, 1.64) and chronic liver diseases (OR=1.31, 95% CI=1.25, 1.37) were associated with an increased risk of pulmonary tuberculosis. The sub- analysis demonstrated that the odds of pulmonary tuberculosis was 4.81 (95%
CI=2.31, 10.0) for patients co-morbid with splenectomy and any of the above diseases. Splenectomy is associated with 1.9-fold increased risk of pulmonary tuberculosis in Taiwan. There is a synergistic effect between splenectomy and other co-morbidities on the risk of pulmonary tuberculosis.
Keywords: diabetes mellitus, pneumoconiosis, pulmonary tuberculosis; splenectomy
Introduction
Tuberculosis is a major public health problem due to its high prevalence and heavy socioeconomic burden. The World Health Organization (WHO) estimated that there were 12 million people having tuberculosis (ranging from 10 million to 13 million) in the world in 2011. The lungs are the major affected organ, and the result disease is called pulmonary tuberculosis. Epidemiologic studies show that multiple risk factors are associated with pulmonary tuberculosis, including chronic obstructive pulmonary disease, pneumoconiosis, chronic kidney diseases, diabetes mellitus, chronic liver diseases, cancer, HIV/AIDS, tobacco smoking and alcohol consumption .
Splenectomized patients are at an increased risk for overwhelming post-splenectomy infections from Gram-positive and Gram-negative bacteria . To our knowledge, the clinical association between splenectomy and pulmonary tuberculosis has not yet been investigated.
Our biologically plausible hypothesis was that there is a relationship between
splenectomy and pulmonary tuberculosis. In this present study, we used the database
of the Taiwan National Health Insurance Program to investigate the relationship
between splenectomy and pulmonary tuberculosis.
Materials and Methods Data sources
We designed this case-control study to analyze the database from the Taiwan National Health Insurance Program. The details of insurance were described in previous studies . Briefly speaking, the National Health Research Institute cooperates with the Bureau of National Health Insurance to establish several data files annually using the National Health Insurance claims data for administrative use and research. The National Health Insurance Program was implemented in 1995, covering approximately 99% of the whole population of 23.74 million people . This study utilized two datasets of 1000000 individuals randomly selected from all insured claims data from 1998 to 2011. Diseases were coded based on the International Classification of Disease Diagnoses, Ninth Revision of Clinical Modification (ICD-9 codes). The accuracy and validity of disease diagnosis in the National Health Insurance Research Database, such as tuberculosis, chronic obstructive pulmonary disease, chronic kidney diseases,
diabetes mellitus and chronic liver diseases, were demonstrated in previous studies .
The National Health Research Institute encrypts patient's personal information for
privacy protection and provides researchers with anonymous identification numbers
associated with the relevant claim information, which includes patient's sex, date of
birth, registry of medical services and medication prescriptions. Patient consent is not
required for accessing the National Health Insurance Research Database. The study
was also approved by the Institutional Review Board of China Medical University and
Hospital (CMU-REC-101-012).
Inclusion criteria
In this case-control study, we selected subjects with newly diagnosed pulmonary tuberculosis as the case group during the period of 1998-2011 based on ICD-9 codes (010, 011, 012 and 018), who were aged 20 years or older at the date of diagnosis.
The index date for each case was the date of diagnosis of pulmonary tuberculosis.
Patients with pulmonary tuberculosis were identified at least two times from
principal/secondary diagnoses in outpatient visits or at least one time hospitalization. For each case, four control subjects were selected as the control group, who were matched for sex, age (per 5 years) and index year of diagnosing pulmonary tuberculosis.
Subjects with previous diagnosis of pulmonary tuberculosis, any cancer or HIV/AIDS before the index date were excluded.
Potential co-morbidities associated with pulmonary tuberculosis
A number of co-morbidities before the index date were examined for their possible association with pulmonary tuberculosis. These were splenectomy, chronic
obstructive pulmonary disease, pneumoconiosis, chronic kidney diseases, diabetes mellitus, and chronic liver diseases including cirrhosis, alcoholic liver damage, hepatitis B, hepatitis C and other types of chronic hepatitis. They were diagnosed with ICD-9 codes.
Statistical Analysis
We first compared pulmonary tuberculosis cases with non-pulmonary tuberculosis
controls on the proportional distributions of demographic status and comorbidities by
test for categorical variables and t-test for continuous variables. Multivariable
unconditional logistic regression analysis was used to estimate the odds ratio (OR) and 95% confidence interval (CI) for association between pulmonary tuberculosis and splenectomy, after controlling for age and other comorbidities. In addition, we
evaluated the interaction effect between splenectomy and other comorbidities on risk of pulmonary tuberculosis by using the multivariable unconditional logistic regression model. All analyses were conducted using the SAS statistical software (version 9.2 for Windows; SAS Institute, Inc., Cary, NC, USA), and all statistical tests were
performed at the two-tailed significance level of 0.05.
Results
Characteristics of the study population
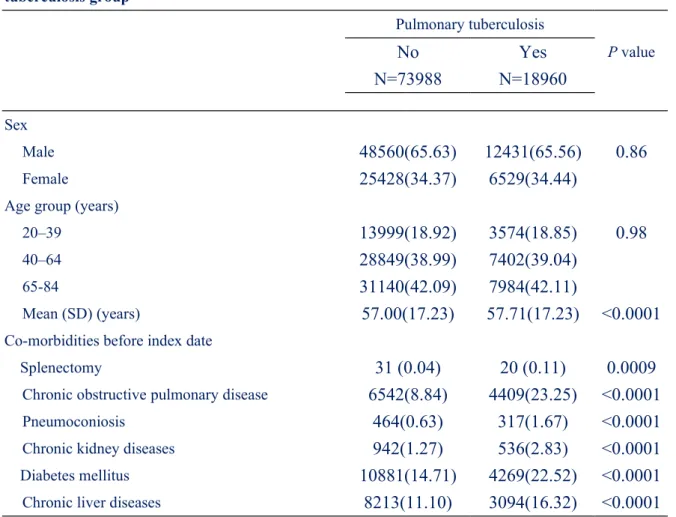
There were 18960 patients with newly diagnosed pulmonary tuberculosis as the case
group and 73988 subjects without pulmonary tuberculosis as the control group. We
compared the characteristics and co-morbidities between the pulmonary tuberculosis
group and the non-pulmonary tuberculosis group. Table 1 shows that the pulmonary
tuberculosis group was more likely to have splenectomy, chronic obstructive
pulmonary disease, pneumoconiosis, chronic kidney diseases, diabetes mellitus and chronic liver diseases, with statistical significance. The mean duration from
splenectomy to diagnosing pulmonary tuberculosis was 3.93 years (standard deviation, 3.76; range, 0.07 to 12.71, data not shown in Table 1).
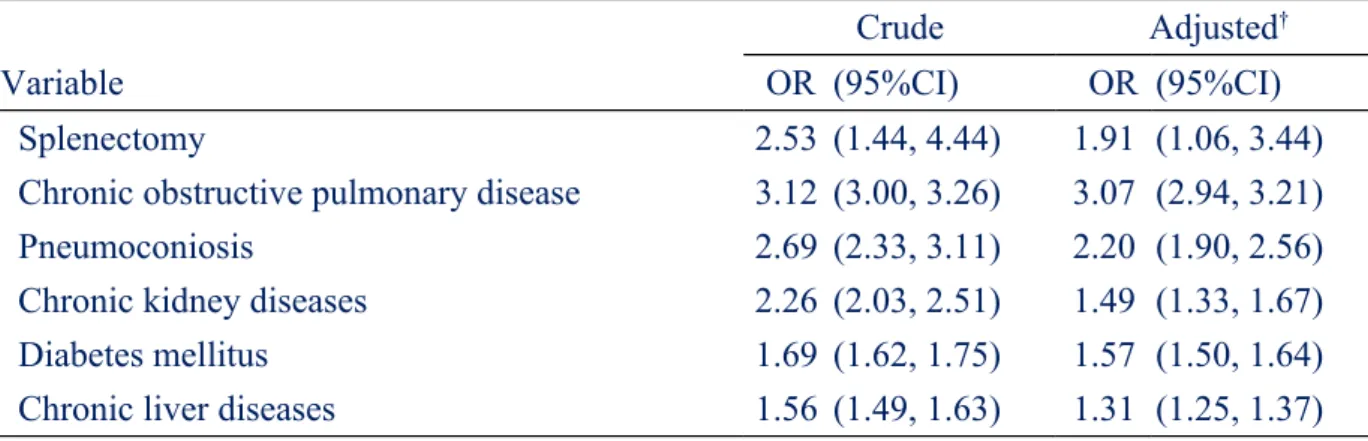
Association between splenectomy, co-morbidities and pulmonary tuberculosis After adjustment for confounders that were found significantly in crude analysis, multivariable unconditional logistic regression analysis showed that the adjusted OR of pulmonary tuberculosis was 1.91 for splenectomized patients (95% CI=1.06, 3.44), as compared to non-splenectomized patients. In addition, chronic obstructive
pulmonary diseases (OR=3.07, 95% CI=2.94, 3.21), pneumoconiosis (OR=2.20, 95%
CI=1.90, 2.56), chronic kidney diseases (OR=1.49, 95% CI=1.33, 1.67), diabetes mellitus (OR=1.57, 95% CI=1.50, 1.64) and chronic liver diseases (OR=1.31, 95%
CI=1.25, 1.37) were significantly associated with increased risk of pulmonary tuberculosis (Table 2).
Interaction between splenectomy and other comorbidities on risk of pulmonary tuberculosis
As a reference of subjects without splenectomy and without any comorbidity, the ORs were 2.60 (95% CI=1.06, 6.39) for those with splenectomy and without any
comorbidity, and as high as 4.81 (95% CI=2.31, 10.0) for those with splenectomy and presence of any co-morbidity, with statistical significance.
Discussion
Although previous literature reported that there was a link between splenectomy and
pulmonary tuberculosis , to the best of our knowledge, this is the first population-
based study to investigate the relationship between splenectomy and pulmonary
tuberculosis. In this present study, we found that splenectomized patients had 1.9-fold
increased risk of pulmonary tuberculosis. We also found that chronic obstructive pulmonary diseases, pneumoconiosis, chronic kidney diseases, diabetes mellitus and chronic liver diseases were significantly associated with increased risk of pulmonary tuberculosis, which is compatible with previous studies . Particularly, the risk would increase to 4.8-fold for those with splenectomy and presence of any co-morbidity included. We believe that there is a synergistic effect between splenectomy and other co-morbidities on risk of pulmonary tuberculosis.
Although the immune response of tuberculosis depends mostly on cell mediated immunity, recent evidence has illustrated that B cells and humoral immunity can play a modulatory role in the immune response to various intracellular microorganisms, including tuberculosis . The spleen has a well established fundamental role in protecting the human body against invading microorganisms by bactericidal capacity of lymphoid cells and macrophages and by the humoral immune response . The spleen also produces immunoglobulin M memory B cells, which are more important in protecting against invading microorganisms . In the absence of spleen, phagocytic activities and the humoral immune response would be markedly impaired . We think that altered immune function caused by splenectomy could potentially precipitate the development of pulmonary tuberculosis.
Some points should be addressed in the present study. First, some risk factors of pulmonary tuberculosis, such as tobacco smoking, alcohol consumption,
socioeconomic status and history of incarceration were not recorded due to the
inherent limitation of this database. Second, due to the same limitation, we did not
know whether cases/controls received post-splenectomy antibiotic prophylaxis. Third,
though comorbid conditions were included before the date of diagnosis of pulmonary
tuberculosis, we could not make sure whether these conditions were really present prior to tuberculosis symptoms. Forth, some malignancies, such as leukemia and lymphoma, can be an indication for splenectomy and can be an independent risk factor for pulmonary tuberculosis. To reduce confounding effects, subjects with a diagnosis of any cancer or HIV/AIDS before the index date were excluded from the study. The strength of this present study is that the set of ICD-9 codes used has been validated in previous published studies . The present study was based on a
biologically plausible hypothesis and its long-term follow-up allowed for a valid assessment of the time course from splenectomy to diagnosis of pulmonary
tuberculosis. This study used a large population-based database that would strengthen the power of the findings.
We conclude that splenectomy is associated with 1.9-fold increased risk of pulmonary tuberculosis in Taiwan. The risk would increase to 4.8-fold for those with
splenectomy and presence of any co-morbidity. Based on these findings, regular
surveillance of pulmonary tuberculosis can be recommended for patients with
splenectomy and other co-morbidities. Further prospective studies are needed to
confirm our findings.
Acknowledgements
The authors thank the National Health Research Institute in Taiwan for providing the insurance claims data. The authors thank Professor Fung-Chang Sung for his critical review of this manuscript.
Specific author contributions
Shih-Wei Lai: (1) substantially contributed to the conception of this article; (2) planned and conducted the study; (3) initiated the draft of the article and critically revised the article.
I-Kuan Wang and Hung-Jen Chen: (1) participated in data interpretation; (2) critically revised the article.
Cheng-Li Lin: (1) conducted data analysis; (2) critically revised the article.
Kuan-Fu Liao: (1) substantially contributed to the concept and design, as well as data acquisition; (2) critically revised the article.
Funding
This study was supported in part by Taiwan Department of Health Clinical Trial and Research Center of Excellence (DOH102-TD-B-111-004) and China Medical
University Hospital (Grant number 1MS1). The funding agency did not influence the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest Statement
The authors disclose no conflicts of interest.
References
1 World Health Organization. Global tuberculosis report 2012.
http://www.who.int/tb/publications/global_report/gtbr12_mainpdf. [cited in 2013 June].
2 Wu HP, Pan YH, Hua CC, Shieh WB, Jiang BY, Yu TJ. Pneumoconiosis and liver cirrhosis are not risk factors for tuberculosis in patients with pulmonary infection. Respirology. 2007; 12: 416-419.
3 Gupta S, Shenoy VP, Mukhopadhyay C, Bairy I, Muralidharan S. Role of risk factors and socio-economic status in pulmonary tuberculosis: A search for the root cause in patients in a tertiary care hospital, south india. Trop Med Int Health. 2011; 16: 74-78.
4 Lee CH, Lee MC, Shu CC, et al. Risk factors for pulmonary tuberculosis in patients with chronic obstructive airway disease in taiwan: A nationwide cohort study. BMC Infect Dis. 2013; 13: 194.
5 Altamura M, Caradonna L, Amati L, Pellegrino NM, Urgesi G, Miniello S.
Splenectomy and sepsis: The role of the spleen in the immune-mediated bacterial clearance. Immunopharmacol Immunotoxicol. 2001; 23: 153-161.
6 Jirillo E, Mastronardi ML, Altamura M, et al. The immunocompromised host:
Immune alterations in splenectomized patients and clinical implications. Curr Pharm Des. 2003; 9: 1918-1923.
7 Morgan TL, Tomich EB. Overwhelming post-splenectomy infection (opsi): A case report and review of the literature. J Emerg Med. 2012; 43: 758-763.
8 Lai SW, Liao KF, Liao CC, Muo CH, Liu CS, Sung FC. Polypharmacy correlates with increased risk for hip fracture in the elderly: A population- based study. Medicine (Baltimore). 2010; 89: 295-299.
9 Lai SW, Chen PC, Liao KF, Muo CH, Lin CC, Sung FC. Risk of
hepatocellular carcinoma in diabetic patients and risk reduction associated with anti-diabetic therapy: A population-based cohort study. Am J
Gastroenterol. 2012; 107: 46-52.
10 Lai SW, Liao KF, Chen PC, Tsai PY, Hsieh DP, Chen CC. Antidiabetes drugs correlate with decreased risk of lung cancer: A population-based observation in taiwan. Clin Lung Cancer. 2012; 13: 143-148.
11 Liao KF, Lai SW, Li CI, Chen WC. Diabetes mellitus correlates with increased risk of pancreatic cancer: A population-based cohort study in taiwan. J Gastroenterol Hepatol. 2012; 27: 709-713.
12 Yu YH, Liao CC, Hsu WH, et al. Increased lung cancer risk among patients
with pulmonary tuberculosis: A population cohort study. J Thorac Oncol.
2011; 6: 32-37.
13 Lai SW, Muo CH, Liao KF, Sung FC, Chen PC. Risk of acute pancreatitis in type 2 diabetes and risk reduction on anti-diabetic drugs: A population-based cohort study in taiwan. Am J Gastroenterol. 2011; 106: 1697-1704.
14 Cheng KC, Chen YL, Lai SW, Mou CH, Tsai PY, Sung FC. Patients with chronic kidney disease are at an elevated risk of dementia: A population-based cohort study in taiwan. BMC Nephrol. 2012; 13: 129.
15 Mileno MD, Bia FJ. The compromised traveler. Infect Dis Clin North Am.
1998; 12: 369-412.
16 Nakasone E, Mato N, Nakayama M, Bando M, Sugiyama Y. A case of
pulmonary tuberculosis with false negative quantiferon TB-2G test. Kekkaku.
2012; 87: 9-13.
17 Kozakiewicz L, Phuah J, Flynn J, Chan J. The role of b cells and humoral immunity in mycobacterium tuberculosis infection. Adv Exp Med Biol. 2013;
783: 225-250.
18 Kraal G. Cells in the marginal zone of the spleen. Int Rev Cytol. 1992; 132:
31-74.
19 Kruetzmann S, Rosado MM, Weber H, et al. Human immunoglobulin m
memory b cells controlling streptococcus pneumoniae infections are generated
in the spleen. J Exp Med. 2003; 197: 939-945.
Table 1. Characteristics between the pulmonary tuberculosis group and non-pulmonary tuberculosis group
Pulmonary tuberculosis
No N=73988
Yes N=18960
P value
Sex
Male 48560(65.63) 12431(65.56) 0.86
Female 25428(34.37) 6529(34.44)
Age group (years)
20–39 13999(18.92) 3574(18.85) 0.98
40–64 28849(38.99) 7402(39.04)
65-84 31140(42.09) 7984(42.11)
Mean (SD) (years) 57.00(17.23) 57.71(17.23) <0.0001
Co-morbidities before index date
Splenectomy 31 (0.04) 20 (0.11) 0.0009
Chronic obstructive pulmonary disease 6542(8.84) 4409(23.25) <0.0001
Pneumoconiosis 464(0.63) 317(1.67) <0.0001
Chronic kidney diseases 942(1.27) 536(2.83) <0.0001
Diabetes mellitus 10881(14.71) 4269(22.52) <0.0001
Chronic liver diseases 8213(11.10) 3094(16.32) <0.0001
Data are presented as the number of subjects in each group, with percentages given in
parentheses or mean, with SD given in parentheses.
Table 2. Odds ratio and 95% confidence interval of pulmonary tuberculosis associated with splenectomy and co-morbidities
Crude Adjusted
†Variable OR (95%CI) OR (95%CI)
Splenectomy 2.53 (1.44, 4.44) 1.91 (1.06, 3.44)
Chronic obstructive pulmonary disease 3.12 (3.00, 3.26) 3.07 (2.94, 3.21)
Pneumoconiosis 2.69 (2.33, 3.11) 2.20 (1.90, 2.56)
Chronic kidney diseases 2.26 (2.03, 2.51) 1.49 (1.33, 1.67)
Diabetes mellitus 1.69 (1.62, 1.75) 1.57 (1.50, 1.64)
Chronic liver diseases 1.56 (1.49, 1.63) 1.31 (1.25, 1.37)
†