How
early
should
VATS
be
performed
for
retained
haemothorax
in
blunt
chest
trauma?
Hsing-Lin
Lin
b,e,g,
Wen-Yen
Huang
c,
Chyan
Yang
c,
Shih-Min
Chou
f,
Hsin-I.
Chiang
d,
Liang-Chi
Kuo
b,e,g,
Tsung-Ying
Lin
b,e,g,
Yi-Pin
Chou
a,h,*
a
DivisionofTrauma,DepartmentofEmergency,VeteransGeneralHospital-Kaohsiung,Kaohsiung,Taiwan
b
DepartmentofEmergencyMedicine,KaohsiungMedicalUniversityHospital,KaohsiungMedicalUniversity,Kaohsiung,Taiwan
c
InstituteofBusinessandManagement,NationalChiaoTungUniversity-Taipei,Taipei,Taiwan
dShihChienUniversity-Kaohsiung,Kaohsiung,Taiwan e
DivisionofTrauma,DepartmentofSurgery,KaohsiungMedicalUniversityHospital,KaohsiungMedicalUniversity,Kaohsiung,Taiwan
f
DepartmentofAdministrationCenter,KaohsiungMedicalUniversityHospital,KaohsiungMedicalUniversity,Kaohsiung,Taiwan
g
DepartmentofEmergencyMedicine,FacultyofMedicine,CollegeofMedicine,KaohsiungMedicalUniversity,Kaohsiung,Taiwan
h
ResearchCenterforIndustryofHumanEcology,ChangGungUniversityofScienceandTechnology,Kweishan,Taoyuan,Taiwan
Introduction
Bluntinjuryistheleadingcauseofchesttrauma.Pneumothorax andhaemothoraxoftenoccurafterseverechesttrauma. Approxi-mately85%ofpatientswithpneumothoraxandhaemothoraxcan
be successfully treated with pain control or simple tube thoracostomies [1–3]. The remaining patients with retained pleural collections should be managed with further surgical interventionstopreventcomplicationssuchasempyemainthe earlyphaseorfibrothoraxinthelatephase.Thesecomplications willincreasemorbidityandmortality[4–6].
Video-assisted thoracoscopic surgery (VATS) has become a common and acceptable methodfor diagnosisof intra-thoracic lesionsfromthe1990sbecauseofadvanceddevelopmentsinthis surgicaltechnique[7–9].Itisalsowidelyusedintreatingretained pleural collections because it is only slightly more invasive
ARTICLE INFO
Articlehistory: Accepted24May2014
Keywords:
Video-assistedthoracoscopicsurgery Haemothorax Bluntinjury Lengthofstay Infection Ventilator Thoracicinjury ABSTRACT
Background: Bluntchestinjuryisnotuncommonintraumapatients.Haemothoraxandpneumothorax mayoccurinthesepatients,andsomeofthemwilldevelopretainedpleuralcollections.Video-assisted thoracoscopicsurgery(VATS)hasbecomeanappropriatemethodfortreatingthesecomplications,but theoptimaltimingforperformingthesurgeryanditseffectsonoutcomearenotclearlyunderstood. Materialsandmethods:Inthisstudy,atotalof136patientswhoreceivedVATSforthemanagementof retainedhaemothoraxfromJanuary2003toDecember2011wereretrospectivelyenrolled.Allpatients hadbluntchestinjuriesand90%hadassociatedinjuriesinmorethantwosites.Thetimefromtraumato operationwasrecordedandthepatientsweredividedintothreegroups:2–3days(Group1),4–6days (Group2),and7ormoredays(Group3).Clinicaloutcomessuchasthelengthofstay(LOS)atthehospital andintensivecareunit(ICU),anddurationofventilatorandchesttubeusewereallrecordedand comparedbetweengroups.
Results:Themeandurationfromtraumatooperationwas5.9days.Alldemographiccharacteristics showednostatisticaldifferencesbetweengroups.Comparedwithothergroups,Group3hadhigher ratesofpositivemicrobialculturesinpleuralcollectionsandsputum,longerdurationofchesttube insertionandventilatoruse.LengthsofhospitalandICUstayinGroups1and2showednostatistical difference,butwerelongerinGroup3.ThefrequencyofrepeatedVATSwaslowerinGroup1butwithout statisticallysignificantdifference.
Discussion: ThisstudyindicatedthatanearlyVATSinterventionwoulddecreasechestinfection.Italso reducedthedurationofventilatordependency.Theclinicaloutcomes weresignificantly betterfor patientsreceivingVATSwithin3daysunderintensivecare.Inthisstudy,wesuggestedthatVATSmight bedelayedbyassociatedinjuries,butshouldnotexceed6daysaftertrauma.
ß2014TheAuthors.PublishedbyElsevierLtd.ThisisanopenaccessarticleundertheCCBY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/3.0/).
* Correspondingauthor at: Division of Trauma, Department of Emergency, VeteransGeneralHospital-Kaohsiung,386Ta-Chung1stRd.,Kaohsiung81362, Taiwan.Tel.:+88673125895x7553;fax:+88673208255.
E-mailaddress:chou2763e@yahoo.com.tw(Y.-P.Chou).
ContentslistsavailableatScienceDirect
Injury
j ou rna l h ome p a ge : w ww . e l se v i e r. co m/ l oc a te / i n j ury
http://dx.doi.org/10.1016/j.injury.2014.05.036
0020–1383/ß2014TheAuthors.PublishedbyElsevierLtd.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/ 3.0/).
comparedwithchesttubethoracostomy,andhasbeenshownasa simple technical alternative to open thoracotomy [10–12]. Although VATS offers many benefits, the optimal timing for performingthesurgeryanditseffectsonpatient’soutcomesare notclearlyunderstood.Numerousrecentstudiesdescribethatthe earliertheinterventionsofinjuredchestareperformed,thebetter the prognosis of patients [13–15]. However, there exist wide variations in the exact recommended time for operation after trauma in these studies, especially when complicated with associatedinjuries[7–9,14–16].
Themainreasonsforprolongingthehospitalisationoftrauma patients are infections and respiratory failure [1,17,18]. We hypothesised that early VATS may play a role in preventing post-traumatic infections and decrease the duration of acute respiratoryfailure,whichinturncanshortenthewholetreatment course. The purpose of this study was to identify the most appropriatetimeforimplementingVATStotreatpleuralcollection and its effects on respiratory failure in patients withmultiple traumas.
Materialsandmethods Settingandpatients
This retrospective study wasconducted in a level-1 trauma medicalcentrelocatedinsouthernTaiwan,whichhas1300beds withapproximately1200emergenttraumaticvisitspermonth.All patientswithblunt thoracicinjuries that wereadmittedto the emergency department (ED) during the study period were included.Dataofpatientsthat developedresidualhaemothorax andreceived video-assistedthoracoscopy(VATS)were prospec-tivelycollected.Patientdataincludingdemographics,mechanism of injury, numbers of rib fractures (confirmed by chest CT), associatedinjuries,injuryseverityscore(ISS),pulmonary contu-sion score, postoperative complications, respiratory failure, numberofventilatordays,lengthofstay(LOS)inintensivecare unit(ICU),andLOSinhospitalwereallcollected.Thisstudywas approvedbytheethicscommitteeofthehospitalinwhich this studywasconducted.
Patientsolderthan14yearsofagethatwereadmittedtothe traumaunitinourhospitalwithbluntchesttraumaaloneorwith other associated injuries in different anatomic regions were includedin this study. All patients with haemothorax needing tobedrainedweretreatedwitha36Fr(Thissizeofchesttubeis chosendue toAsian people having smallerbody size) straight thoracostomy tube at the time of initial evaluation. These procedureswere performed by traumasurgeons with first-line service.Patientshadminimalpleuralcollectionsinitiallywithout thoracostomytubesinsertedbutadmittedforfurtherobservation werenotincluded.Inthisstudy,patientsthatwere hemodynami-callyunstablewithmorethan1500mLofblooddrainagefromthe initialtubethoracostomyorhadongoingbloodlossesofmorethan 250mL/h lasting for at least 4h and received emergency thoracotomywereexcluded.Furthermore, patientswith disrup-tionsofmediastinalstructures(includingheart,greatvesselsand tracheobronchial trees) were excluded. Patients with severe medicaldiseaseslikelivercirrhosis,chronicobstructive pulmo-nary disease, chronic renal disease under hemodialysis, and chronic heart failure that would increase complications after traumawerealsoexcluded.
Allpatientsreceivedchest-computedtomography(CT)inthe emergency department. After completing both primary and secondarysurveysattraumabay,allpatientswereadmittedinto trauma ICU for further care because nearly all patients had multiple injured sites. Chest roentgenogram was performed routinelyafter admission. If thedensity of the following chest
X-ray showed increasing density, secondary chest CT was performedtodiagnoseandestimatetheretainedpleural collec-tions.TherearetwoindicationsforVATStobeperformed.Oneis theretainedvolumesestimatedtoexceed300mL.Theotheris formationofpara-pneumoniceffusionswhichappearedinCTas separate lobulated pleural collections. Often, retained pleural collectionsdonothappenimmediately;hence,allsecondaryCT andVATSareperformedatleast48haftertrauma.Theassociated injuries were recorded with abbreviated injury score (AIS) followingthe2005edition.PatientswithAISexceedinggrade3 werealsoexcluded.
All patients received VATS performed by thoracic surgeons according to the same standard procedures. The surgery was performedintheoperatingroomundergeneralanaesthesiawith thepatientsinlateralpositionontheunaffectedside.Allpatients received prophylacticantibiotics before surgicalintervention. A double-lumen endobronchial tube was used for one lung procedureandprovidedabetterviewfortheassessmentofthe chestand itscontents.Twothoracostomieswereperformedfor insertingthoracoscopesandendoscopicinstruments,respectively. Allpatientshadcollectionsevacuated,clotsremoved,thepleura decorticated, and were irrigated with normal saline solutions. Thereafter,thelungwasre-expanded.Finally,two36Frdrainage tubes were fixed to the pleural cavity and the patient was transferred to the trauma ICU for further postoperative care. Routinechestroentgenogramswereperformedafteroperations.In caseofrecurrenceofretainedpleuralcollections,secondaryVATS would be performed for adequate drainages. Following either procedure,thethoracostomytubeswereremovedatthediscretion ofthethoracicsurgeonwhenthedrainagewaslessthan100mL/ 24handnoairleakwaspresent.
Post-trauma complications included the development of infections and prolonged ventilations. Postoperative outcomes indicatedhospitalmortality,numberofventilatordays,ICU,and hospitalLOS.Empyemawasdefinedasanaccumulationofpusin thepleuralspace(confirmedbybacteriaculture).Pneumoniawas definedasaninfectiveconditionwithbacteriaculturedfromthe sputumaftertrauma.Sepsiswasdefinedasasystemicresponseto lunginfectionwithbacteremia.
Statisticalanalysis
Patients were divided into three groups according to when VATSwasperformed,namelyGroup1,within2–3days;Group2, within4–6days;andGroup3,aftermorethan6days.Group1was formedonthebasisofMeyer’sprospectivestudythatshowedvery earlyVATSwithin3 daysprovidedbetterclinicaloutcomes[8]. Group3wasbasedinitiallyonintervalsthatweregreaterthanthe average,withexploratoryanalysisconfirmingthatthisgavebetter discriminationof outcome than a later cut-off point. Aninitial descriptive analysis was performed for every variable, and the frequencies and averages in the groups were determined. Numerical variables were presented as mean and standard deviation(SD)ormedianandquartiles.Thechi-squareorFisher’s test was employed to evaluate the categorical or proportional variables between groups. Thecontinuous variables were com-paredbetweengroupsusingtestsofanalysisofvariance.AP<0.05 was considered statistically significant.All data were analysed usingtheSPSS16.0statisticalsoftware.
Results
Atotalof1663patientswithchestinjurieswereadmittedtoour hospitalfromJanuary1,2003toDecember31,2011.Atotalof145 thoracoscopic drainages performed for clotted post-traumatic haemothorax were selected. A 2-year-old patient and 8 adult
patientswithpenetratinginjurieswereexcluded.The character-isticsofeachgroupareshowninTable1.Therewere107menand 29womenagedfrom16to82years(average51.9,SD=16.2).The mechanism of injury was motorcycle-related (motorcyclist or passenger) injury for 87 patients, vehicle-related (driver or passenger)injury for 14 patients, fallinginjury for 21 patients, andcyclistorpedestrianfor14patients.MedianISSforallpatients was18(quartile,13,22)andtheirmeanISSwas18.1(SD,6.1).The severityofchestinjuryisrecordedbyanatomicabbreviatedinjury score(AIS) of thoracic injuries. Fourpatients wererecordedas grade2,eighty-fourpatientsweregrade3andforty-eightpatients weregrade4.MeanAISofchestinallpatientswas3.3(SD,0.5)and medianwas3(quartiles,3,4).Allpatientshadtubethoracostomy atthetraumabayofemergencydepartmentbeforeVATS.Mean timefromtraumatoresidualpleuralcollectionsdiagnosedfrom secondaryCTis52.8h(SD,9.1).Theaveragetimeperiodbetween thetraumaandperformanceofVATSwas5.9days(SD,4.6).No patientshad their VATSproceduresconvertedtothoracotomies during surgical interventions. However, 14 patients received secondary VATS because of persistent pleural collections after operation.ThemeanLOSofICUandhospitalwere8.7(SD,7.1)and 24.2(SD,18.4)days.Rateofpost-traumainfectionsculturedfrom
sputum,pleuraleffusionandbloodwere40.5%,21.3%and11.8% respectively.Overall,themortalityofthesepatientswas2.2%(3/ 136).
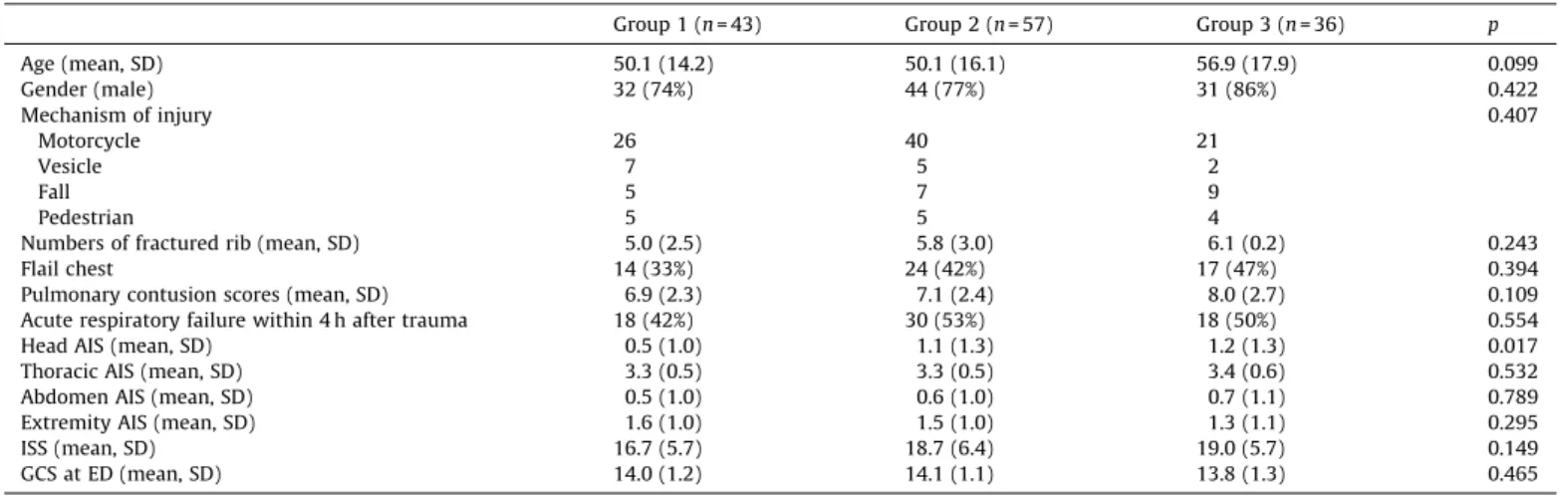
Fig.1shows thatshorterhospitallengths ofstayweremost common in those withshorter intervals fromtrauma toVATS. Patients with positive microbial culture had longer meantime periodsfromtraumatoVATS(9.1daysvs.5.0days,p=0.004),as didthosewithpositivemicrobialcultureofsputum(7.8daysvs. 4.6days,p=0.001).Whenpatientsweredividedintothreegroups accordingtothetimefromtraumatoperformanceoftheVATS(2– 3days,average2.6,SD,0.5;4–6days,average4.6,SD,0.8;>6days after trauma, average 11.9, SD, 5.2), they were compared for demographicandpreoperativestatus(Table2).Group3hashigher headAISthantheothersbuttheGlasgowcomascaleatemergency department, AISofotherregionsand theoverallISSshowedno statisticalsignificantdifferencesbetweenthethreegroups.Other basicdemographics,suchasage,gender,mechanismofinjury,and numberofribfractures,rateofflailchest,pulmonarycontusion scores, rateofacuterespiratoryfailure within4haftertrauma, retainedpleuralcollectionsdiagnosedtimeshowednostatistical differencesbetweenthesegroups;thus,thedemographicand pre-operativestatusofpatientsinthethreegroupsweresimilar.
TheoutcomesofthethreegroupsareshowninTable3.Ascan beseen,Group3hadlongerICULOSandin-hospitalLOSthanthe
Table1
DemographicanalysisofpatientstreatedwithVATSforblunttrauma(n=136). Meanage(yr)(SD) 51.9(16.2)
Males(%) 107(78.7%)
Mechanismsofinjury
Motorcyclist 87
Vesicledriverorpassenger 14
Fallaccident 21
Cyclistorpedestrian 14 Anatomicinjuryscore(AIS)ofthoracicinjury(mean,SD) 3.3(0.5) Associatedinjuries Headinjury(%) 55(40.4%) Abdominalinjury(%) 39(28.7%) Extremityinjury(%) 100(73.5%) Multipletrauma 120(88.2%) ISS(mean,SD) 18.1(6.0)
Positivemicrobialculturesaftertrauma
Fromsputum 54(39.7%)
Frompleuraleffusion 29(21.3%)
Fromblood 16(11.8%)
TimefromtraumatoperformVATS(days)(mean,SD) 5.9(4.6)
SecondaryVATS 14(10.3%)
Timeofventilatoruse(days)(mean,SD) 7.8(11.4) Timeofchesttubeuse(days)(mean,SD) 12.7(9.1) ICUlengthofstay(days)(mean,SD) 8.7(7.1) In-hospitallengthofstay(days)(mean,SD) 24.1(18.4) Mortality(nonerelatedtoVATS) 3(2.2%)
Fig.1.RelationbetweenLOSinhospitalandtimingofVATS.
Table2
Comparisonofbasicdemographicsbetweenpatientgroups.
Group1(n=43) Group2(n=57) Group3(n=36) p
Age(mean,SD) 50.1(14.2) 50.1(16.1) 56.9(17.9) 0.099 Gender(male) 32(74%) 44(77%) 31(86%) 0.422 Mechanismofinjury 0.407 Motorcycle 26 40 21 Vesicle 7 5 2 Fall 5 7 9 Pedestrian 5 5 4
Numbersoffracturedrib(mean,SD) 5.0(2.5) 5.8(3.0) 6.1(0.2) 0.243
Flailchest 14(33%) 24(42%) 17(47%) 0.394
Pulmonarycontusionscores(mean,SD) 6.9(2.3) 7.1(2.4) 8.0(2.7) 0.109 Acuterespiratoryfailurewithin4haftertrauma 18(42%) 30(53%) 18(50%) 0.554
HeadAIS(mean,SD) 0.5(1.0) 1.1(1.3) 1.2(1.3) 0.017
ThoracicAIS(mean,SD) 3.3(0.5) 3.3(0.5) 3.4(0.6) 0.532
AbdomenAIS(mean,SD) 0.5(1.0) 0.6(1.0) 0.7(1.1) 0.789
ExtremityAIS(mean,SD) 1.6(1.0) 1.5(1.0) 1.3(1.1) 0.295
ISS(mean,SD) 16.7(5.7) 18.7(6.4) 19.0(5.7) 0.149
other groups (p<0.05, respectively). The total durations of ventilatorusageandnumbersofpost-VATSventilatordaysare bothlongerinGroup3(p<0.05,respectively).Durationsofchest tubeusagewereshorterinGroup1(p<0.05).However,therewas nostatisticaldifferenceindurationofpostVATStubedrainage betweenthethreegroups(p=0.172).AlthoughVATSperformed withinthreedayshadthebestclinicaloutcomes,therewereno significantdifferencesbetweenGroup1andGroup2.Post-trauma infections were all higher in Group 3 for positive microbial cultures from sputum (23.3%, 38.6%, 63.9%, p=0.001), pleural effusion(11.6%,17.5%, 38.9%,p=0.009)andblood (4.7%, 7.0%, 27.8%,p=0.002).TheratesofsecondaryVATSwereequalinthree groups.Patientsin thesethreegroupsshowednodifferencein mortality.
Discussion
WiththeadvanceddevelopmentandtechniquesforVATS,itis widelyappliedinthediagnosisandtreatmentofvitalsignsstable chest-injured patients [7–9]. VATS could provide excellent visualisation ofthe pleural cavity,which is more beneficial for evacuating pleural collections compared to secondary tube thoracostomies.Althoughthereis a tendencythatVATSshould beconsideredearly,theexacttimingisvariedinmanyresearch studies[9,14].Inthisstudy,wefoundthatinterventionbyVATS within6dayscouldreducetheLOSinhospitalandICU,durationof ventilatoruse,andpostoperativecomplicationswithbetterclinical outcomes.
Post-trauma infectionsare themostimportantfactors influ-encingthedurationsofin-hospitalcoursesforchestinjuries[1,18]. These infections are usually derived from retained pleural collections.Furthermanagementsshouldbeperformed totreat ortopreventthesecomplications[2,3,13,17,19].Withadvancesin developmentandtechniquesforVATS,itiswidelyappliedinthe diagnosisandtreatmentofchest-injuredpatientswithstablevital signs[10–12].VATScouldprovideexcellentvisualisationof the pleural cavity, which is more beneficial for evacuating pleural collectionscomparedwithsecondarytubethoracostomies[9,12]. Itisalsomuchlessinvasivethanexploratorythoracotomy,thus providingshorterrecoverytimefortraumapatients.Despiteofits many advantages, the exact time for performing VATS varies widelyinmanyresearchstudies.Landreneauetal.suggestedearly performancebutdidnotmentiontheexacttimeforVATStobe performed[8].Henifordetal.recommendedthatVATSshouldbe performed within 7 days after trauma [7]. Meyer et al. also evaluatedthebenefitsofearlyVATSforretainedhaemothorax[9]
andindicatedthatreplacingadditionaltubethoracostomieswith
earlyVATSperformedwithinthreedaysaftertraumamayshorten overalldurationsoftubethoracostomiesandin-hospitallengthof stay.ThesameresultswereobtainedbySmithetal.exceptthatthe timeforVATSperformancewassuggestedwithinfivedaysafter trauma[15].MoralesUribeetal.alsosupportedthatearlyVATS withinfivedaysaftertraumacouldincreasethesuccessrateand decrease therateof conversionto thoracotomy[14]. However, recent researchbytheAmericanAssociation for theSurgery of Trauma (AAST) Retained Haemothorax study group found no relationship between timing and success rate of VATS [17]. AlthoughthereisatendencythatVATSshouldbeconsideredas earlyaspossibleinmanystudies,thedefinitetimingisnotvery clearlyunderstood.
In ourhospital, we managedretainedpleural collections by VATS.However,thetimeperiodsfromtraumatooperationsvaried widely.ToanalysetherelationshipbetweentimingofVATSand better clinical outcomes, the patients were divided into three groups in contrast to previous studies. Moreover, patients managedwithin2–3 dayswerestudied toexploretheroles of veryearlyVATSinpreventionofpost-traumaticinfections.There aretworeasonsforsuch.Oneisthatretainedpleuralcollections usually happen 48h after trauma, and the other is that post-traumatic infections often occur after 72h [1,18]. The main purposeisnotonlytodeterminetheoptimaltimingforperforming VATS,butalsotoexplorethepossiblebenefitsofveryearlysurgical interventions.
There are several strengths of this study. First, although outcomes are retrospectively reviewed,all data werecollected prospectively.Secondary,allthedemographicsandpreoperative characteristicsineachgroupweresimilar.Thirdly,thesecondary CT was arranged in all patients suspected for retained pleural collections. This procedure could help differentiate retained haemothoraxfromlungparenchymalesions(e.g.,lungcontusions orhospital-acquiredpneumonia).Allthesefavourablesituations enhancedthereliabilityofresultsobtainedinthisstudy.According to thepresent findings, Groups 3 had higher rates of all post-traumaticinfections.UltraearlyVATSinterventionsinGroup1led tothelowestpost-traumaticinfectiousrates.Eventhoughthere arenostatisticallysignificantdifferencescomparedwithGroup2, VATSperformedearliercouldpreventandcontrolinfectionsearly, thusleadingtobetterclinicaloutcomes.Thelengthsofstayand periodsoftubeusageweresignificantlyshorterforGroups1and2 comparedwithGroup3.Theperiodsofventilatorusagewerealso shorterinGroups1and2.Betterclinicaloutcomesmaybederived frompreventionorearlycontrolofpost-traumaticchestinfections. The other factors that decreased post-trauma complications includeearlyrestorationoflungfunctioningbyearlyVATS.Pleural
Table3
Comparisonofclinicaloutcomesbetweenpatientgroups.
Group1(n=43) Group2(n=57) Group3(n=36) p ICULOS(mean,SD) 5.0(2.3) 7.7(5.0) 14.6(9.6) <0.001* HospitalLOS(mean,SD) 16.2(9.6) 21.3(13.0) 38.2(25.0) <0.001* Numberoftotalventilatordays(mean,SD) 2.6(1.9) 6.8(8.0) 15.5(17.2) <0.001* Numberofpost-VATSventilatordays(mean,SD) 0.9(1.4) 5.2(9.1) 12.1(17.2) <0.001* Durationoftotaltubedrainage(mean,SD) 8.2(3.7) 11.6(6.3) 19.8(12.7) <0.001* Durationofpost-VATStubedrainage(mean,SD) 6.9(3.0) 8.3(5.6) 9.5(9.3) 0.172*
SecondaryVATS(mean,SD) 1(2%) 8(14%) 5(14%) 0.115#
Posttraumainfections
Sputumculturepositive 10(23%) 22(38%) 23(64%) 0.001# Pleuraleffusionculturepositive 5(11%) 10(17%) 14(39%) 0.009#
Bloodculturepositive 2(5%) 4(7%) 10(28%) 0.002#
Mortality 0 1(2%) 2(5%) 0.235#
*
Analysisbyone-wayanalysisofvariancewithPosthoctestbyLeastSignificantDifference.Whenthethreeperiodswerecomparedforthosevariableswheretherewasa statisticallysignificantassociationoverall,groups1and2didnotdiffersignificantlyinanyinstance,whilegroups2and3alwaysshowedstatisticallysignificantdifferences.
collectionsretainedinthepleuralcavitywillinducethelungsto collapse.TheearliertheVATSisperformed,theearlierthelung parenchymacanbeexpandedandlungfunctionscanberestored morerapidly,whichcanshortenthedurationofventilationuse.
Thisstudyhadtwointerestingfindings.Onewasnostatistical differencesindurationofpost-VATStubeusageamongthethree groups;andtheotherwassecondaryVATSrequiredby14patients in this study. Although Group 3 had a higher percentage of secondary VATS required, the overall failure rate of the first operationshowednostatisticallysignificantdifferencebetween groups.ThesetwofindingsimplysimilarsuccessratesofVATSin all groups regardless when VATS was performed, which is compatiblewiththefindingsoftheAASTRetainedHaemothorax studygroup[16].ThehigherfailurerateinGroup3mayberelated to multiple adhesions in pleural cavity. These fibrotic bands complicatedtheimplementationofVATSandinducedinadequate drainage. Many previous studies did not recommend delaying VATS for more than 10 days because the clotted blood would becomepleurally adhesive, thus complicating themanagement
[7,19]. Fortunately, no complications occurred in patients after secondaryVATSinthisstudy.
AlthoughearlyVATShaveadvantagesinpreventinginfections, thetimingof VATSperformanceis usually influenced bymany factors.Vitalsignsandassociatedinjuriesarethemostimportant factorsthataffectthetimingofoperation.Headinjuryisthemost commonreasonfordelayingVATSbecausetherecoveryofcerebral auto-regulationneedsatleast96h[20].ThatiswhymostVATSare usually performed beyond the 4th day after trauma. In this retrospectivestudy,43patientsreceivedVATSwithin3daysafter trauma.Mostof thesepatientshad associated limbinjuries for which early reconstruction or early damage control surgeries shouldbeperformedtopreventfurtherperipheralneuro-vascular injuries. VATS was performed together with these regional surgeries.Incontrast,Group3hadmoreheadinjuries thanthe othergroups.Thisgroupalsohasthelowestrateoflimbinjury,so VATSwasdelayedtilltheconditionsofheadinjuriesbecamemore stable.AlthoughtheAISofheadwashigherinGroup3thaninthe othertwogroupswithstatisticalsignificance,theGCSandISSwere allequalin thethree groups.Therateofpneumoniacausedby enterobacteriawasthesamein allgroups(7.0%,8.8%and8.3%, respectively; p=0.946). That is, the possibility of aspiration pneumonia induced by unconscious status is the same in all patients.ItmeansthathigherinfectionratesofGroup3arenot attributed to the higher incidence of head injuries. Instead, differentassociatedinjuriesarethemajorreasonsbehinddifferent timings for VATSperformed, which couldinfluencethe clinical outcomes.
Therearesomepotentiallimitationsinthisstudy.First,thiswas aretrospectivestudy.Allthedataandparameterswerecollected from chart reviews, and there might be recording errors. Nevertheless,alldatawerecollectedwithastandardformwithout missingdataandthedataweredouble-checkedbyaseniortrauma surgeon.Second,althoughthetreatmentguidelinesarethesame, thetimingarrangedandoperationmethodsperformedbythoracic surgeonsmaystillbedifferent.However,thepreoperativestatus anddemographicmatchingofthethreegroupscandecreasethe biascausedbyinterraterdifferences.Third,onlylessthan15%of bluntchesttraumapatientsmayhaveretainedpleuralcollections. Although the number of VATS cases is small, the outcome parameters showed statistically significant differences. Fourth, many factors couldinfluence the duration of acute respiratory failure.Severeassociatedinjuriesfromtheheadandabdomenare themostcommonthatcouldlengthenthein-hospitalstay.Chronic medicalproblemssuchaschronicobstructivepulmonarydisease, livercirrhosisandchronicheartfailurecouldincreasemorbidity andmortality.Allthesebiaseswereexcludedbeforeenrolmentin
thisstudy.Fifth,hospital-acquiredpneumoniaisanother impor-tantfactorthatprolongsthein-hospitallengthofstay.Itisdifficult todifferentiatethepost-traumaticinfectionoflungfrom hospital-acquired pneumonia in trauma patients because these two conditions could happen simultaneously or in close sequence. Because therelationshipbetween hospital-acquired pneumonia andacuterespiratoryfailureishigh,therateofthelattercouldbe calculatedtoestimatethepossibilityoftheformer.Inthisstudy, theratesofacuterespiratoryfailurewithin4haftertraumaarethe same in all three groups. This could decrease the bias due to hospital-acquired pneumonia that would influence the clinical outcomes.
Conclusion
Inthisstudy,alloutcomesworsenedwhentheinterventionwas performed after 6 days. Although there were no significant differences inclinical outcomeswithVATSperformed within 6 days,earlyVATSevacuationwithin3dayscouldobtainthelowest post-traumatic complications and improve the outcome. We postulatethatundersuitableconditions,patientsshouldreceive VATSearlierwhensurgicalinterventionisindicated.
Conflictofinterest
Allauthorshavenoconflictsofinterest.
Acknowledgements
Thefirsttwoauthorsmadeequalcontributionstothisworkand areequallyconsideredtobefirstauthor.Thelasttwoauthorsmade equalcontributionstothisworkandareequallyconsideredtobe correspondingauthors.Weappreciatethehelpfromeditorsand anonymousrefereesforthecriticalreviewandstatistical sugges-tions.
References
[1]HellingTS,Gyles3rdNR,EisensteinCL,SoraccoCA.Complicationsfollowing bluntandpenetratinginjuriesin216victimsofchesttraumarequiringtube thoracostomy.JTrauma1989;29:1367–70.
[2]McManusK,McGuiganJ.Minimallyinvasivetherapyinthoracicinjury.Injury 1994;25:609–14.
[3]RichardsonJD,CarrilloE.Thoracicinfectionaftertrauma.ChestSurgClinNAm 1997;7:401–27.
[4]EddyAC, LunaGK,CopassM.Empyemathoracisin patientsundergoing emergent closed tube thoracostomy for thoracic trauma. Am J Surg 1989;157:494–7.
[5]EtochSW,Bar-NatanMF,MillerFB,RichardsonJD.Tubethoracostomy.Factors related to complications. Arch Surg(Chicago IL:1960) 1995;130:521–5. discussion5–6.
[6]ChouY-P,KuoL-C,SooK-M,TarngY-W,ChiangH-I,HuangF-D,etal.Theroleof repairinglunglacerationsduringvideo-assistedthoracoscopicsurgery eva-cuationsforretainedhaemothoraxcausedbybluntchesttrauma.EurJ Cardio-ThoracSurg2013;1:5.http://dx.doi.org/10.1093/ejcts/ezt523.
[7]HenifordBT,CarrilloEH,SpainDA,SosaJL,FultonRL,RichardsonJD.Theroleof thoracoscopyinthemanagementofretainedthoraciccollectionsaftertrauma. AnnThoracSurg1997;63:940–3.
[8]LandreneauRJ,KeenanRJ,HazelriggSR,MackMJ,NaunheimKS.Thoracoscopy forempyemaandhemothorax.Chest1996;109:18–24.
[9]MeyerDM,JessenME,WaitMA,EstreraAS.Earlyevacuationoftraumatic retainedhemothoracesusingthoracoscopy:aprospective,randomizedtrial. AnnThoracSurg1997;64:1396–400.discussion400–1.
[10]CarrilloEH,RichardsonJD.Thoracoscopyfortheacutelyinjuredpatient.AmJ Surg2005;190:234–8.
[11]Lang-LazdunskiL,MourouxJ,PonsF,GrosdidierG,MartinodE,ElkaimD,etal. Roleofvideothoracoscopyinchesttrauma.AnnThoracSurg1997;63:327–33.
[12]LiuDW,LiuHP,LinPJ,ChangCH.Video-assistedthoracicsurgeryintreatment ofchesttrauma.JTrauma1997;42:670–4.
[13]CoselliJS,MattoxKL,BeallJrAC.Reevaluationofearlyevacuationofclotted hemothorax.AmJSurg1984;148:786–90.
[14]MoralesUribeCH,VillegasLanau MI,PetroSanchez RD.Besttiming for thoracoscopic evacuation of retained post-traumatic hemothorax. Surg Endosc2008;22:91–5.
[15]SmithJW,FranklinGA,HarbrechtBG,RichardsonJD.EarlyVATSforbluntchest trauma:amanagementtechniqueunderutilizedbyacutecaresurgeons.J Trauma2011;71:102–5.discussion5–7.
[16]DuBoseJ,InabaK,DemetriadesD,ScaleaTM,O’ConnorJ,MenakerJ,etal. Managementofpost-traumaticretainedhemothorax:aprospective, observa-tional,multicenterAASTstudy.JTraumaAcuteCareSurg2012;72:11–22. discussion-4;quiz316.
[17]DuBose J, InabaK,Okoye O,Demetriades D, ScaleaT, O’ConnorJ,et al. Development of posttraumatic empyema in patients with retained
hemothorax:resultsofaprospective,observationalAASTstudy.JTrauma AcuteCareSurg2012;73:752–7.
[18]RichardsonJD,MillerFB,CarrilloEH,SpainDA.Complexthoracicinjuries.Surg ClinNAm1996;76:725–48.
[19]ErenS,EsmeH,SehitogullariA,DurkanA.Theriskfactorsandmanagementof posttraumaticempyemaintraumapatients.Injury2008;39:44–9.
[20]YokoboriS,WatanabeA,MatsumotoG,OndaH,MasunoT,FuseA,etal.Time courseofrecoveryfromcerebralvulnerabilityafterseveretraumaticbrain injury:amicrodialysisstudy.JTrauma2011;71:1235–40.