Kaohsiung J Med Sci January 2010 • Vol 26 • No 1 13 Neck problems are very common in adults. A
preva-lence study in the United States of America found that over 30% of adults suffered from neck and/or low
back pain [1]. Neck and back problems may led to disability, which extends beyond the pain and/or uncomfortable symptoms and can lead to overall health problems [2,3]. The impact of neck problems on quality of life is two-fold; they affect not only physical health but also the mental health [4]. A sur-vey using the multipurpose health-related quality of life (HRQOL) measure found that the physical com-ponent summary (PCS) and the mental comcom-ponent summary (MCS), as measured by the Short Form-36 Received: May 21, 2009 Accepted: Sep 23, 2009
Address correspondence and reprint requests to: Professor Yi-Jing Lue, Department of Physical Therapy, College of Health Science, Kaohsiung Medical University, 100, Shih-Chuan 1st Road, Kaohsiung 807, Taiwan.
E-mail: yijilu@kmu.edu.tw
C
ORRELATIONS
B
ETWEEN
Q
UALITY OF
L
IFE AND
P
SYCHOLOGICAL
F
ACTORS IN
P
ATIENTS
W
ITH
C
HRONIC
N
ECK
P
AIN
Rong-Fong Lin,1,2Jyh-Jong Chang,3,4Yen-Mou Lu,5Mao-Hsiung Huang,4and Yi-Jing Lue4,6
1Department of Rehabilitation Technology, Tzu Hui Institute of Technology; 2 Graduate Institute of Behavior
Science, 3Departments of Occupational Therapy and 6Physical Therapy, College of Health Science,
Kaohsiung Medical University; and Departments of 4Physical Medicine and Rehabilitation and 5Orthopaedics, Kaohsiung Medical University Hospital, Kaohsiung, Taiwan.
The purpose of this study was to investigate health-related quality of life (HRQOL) and associ-ated factors in patients with chronic neck pain (CNP). The HRQOL of patients with CNP was assessed by the Short Form-36 questionnaire in this cross-sectional study. To evaluate the psycho-logical factors related to HRQOL, the Eysenck Personality Questionnaire, Chinese Health Questionnaire, and Beck Anxiety Inventory were used. The scores for the eight subscales of Short Form-36 were all lower than the Taiwanese age-matched normative values (p< 0.001). The two most strongly affected subscales were the role–physical subscale and the bodily pain sub-scale; both scores were below half the score of the age-/sex-matched normative values. The phys-ical components summary score, a summary measure, was moderately correlated with age (r = –0.43), education level (r = 0.37) and Beck Anxiety Inventory score (r = –0.36). The mental components summary score was moderately to highly correlated with the Chinese Health Questionnaire score (r = –0.72), the neuroticism domain of Eysenck Personality Questionnaire (r = –0.52) and Beck Anxiety Inventory score (r = –0.41). The HRQOL of patients with CNP was worse than that of normal subjects across all domains. Furthermore, patients with a neurotic per-sonality, minor psychiatric morbidity and higher anxiety status showed poor mental health, as measured by the Short Form-36. We found that patients with CNP had multiple physical and mental health problems in terms of. The mental health of patients with CNP was strongly associ-ated with various psychological factors. Comprehensive assessment of the physical and mental functioning of patients with CNP can improve the management and care of these patients.
Key Words:chronic neck pain, mental health, quality of life, SF-36 (Kaohsiung J Med Sci 2010;26:13–20)
(SF-36) questionnaire, were lower in patients with chronic neck pain (CNP) than the relative normative values. Aside from perceived poor HRQOL, patients with CNP may also exhibit mental disorders. World-wide, mental health surveys have shown poor men-tal health in chronic cases; menmen-tal disorders were more common among people with chronic back and neck pain than those without [5].
Although patients with CNP show impaired HRQOL, few studies have investigated the associ-ation between HRQOL and underlying psychologi-cal factors. Understanding the association between HRQOL and psychological status would provide a clear profile of CNP, and useful suggestions could be derived to improve strategies for managing CNP. Psychological factors might be closely related to pain behavior. People with chronic pain may suffer from a variety of negative emotion, such as depression, anxi-ety, frustration, anger or fear. Personality also appears to exert a substantial influence on emotion and ill-ness behavior in pain processing [6–10]. The purpose of this study was to investigate the HRQOL and explored its correlated factors of patients with CNP. Eight health subscales and two summary measures of SF-36 were used, and the association between over-all health status and psychological factors (including personality, minor psychiatric distress and anxiety) was analyzed in this study.
M
ETHODSSubjects
Participants with CNP were recruited from the out-patient Orthopedic and Rehabilitation Departments at Kaohsiung Medical University Hospital in Taiwan. Patients with neck pain (with or without arm symp-toms) for over 6 months met the participant selection criterion. Patients were identified based on symptoms, physical signs and imaging study results by physi-cians. The diagnoses of CNP included degenerative joint disease, herniated intervertebral disc, strain and sprain, and non-specific neck pain. Patients suffering from other types of pain predominantly without neck problems, such as shoulder diseases, inflammatory rheumatic disease, and pain caused by cancer, were excluded. The study was approved by the hospital’s institutional review board, and written informed con-sent was obtained from all participants.
Instruments
The SF-36 measures eight health attributes: physical functioning (PF), role limitations due to physical health problems (role–physical, RP), bodily pain, general health, vitality, social functioning, role limitation due to emotional problems (role–emotional, RE) and men-tal health. The two summary measures, PCS and MCS, were calculated from these eight subscales to demon-strate the overall physical and mental function respec-tively [11]. The Taiwanese version of SF-36 has shown good reliability and validity [12,13].
The Chinese brief version of the Eysenck Personality Questionnaire (EPQ) was used to measure personal-ity characteristics [14]. The brief EPQ measures two types of personality, neuroticism (EPQ-N) and extra-version (EPQ-E). The EPQ brief extra-version has good internal consistency, test–retest reliability and concur-rent validity [15].
The Chinese Health Questionnaire (CHQ) was de-veloped for use in community surveys of psychiatric illness. The CHQ was used to measure psychiatric morbidity. We used the 12-item CHQ in this study; the scores range from 0 to 12 [16]. The sensitivity and specificity were 69.6% and 94.8%, respectively, and the cut-off point was 2/3 in community clinics. It is valid and appropriate for use as a screening instrument for psychiatric morbidity in clinical settings [17,18].
The Beck Anxiety Inventory (BAI) is a 21-item self-report questionnaire measuring symptoms of anxiety [19]. Scores over 10 suggest mild anxiety and scores over 19 indicate moderate anxiety. The BAI confirmed better ability to differentiate anxiety from depression than the State-Trait Anxiety Inventory [20].
Procedures
Patients meeting the eligibility criteria were invited to participate in this study. Patients were asked to com-plete a questionnaire before evaluation and treatment of their condition. The participants participated in per-sonal interviews, and the questionnaire was completed in a quiet room. The questionnaire contained demo-graphic questions, the SF-36 Taiwan version [12], EPQ [14], CHQ-12 [16], and BAI [19] questionnaires. The SF-36 was used to measure the HRQOL, and the EPQ, CHQ-12 and BAI questionnaires were used to measure psychological status. Pain intensity was re-corded based on the answer to the seventh question of the SF-36, “How much bodily pain have you had during the past 4 weeks?” The question is scored on a
six-point scale (range, 1–6), with 1 representing no pain and 6 representing very severe pain. Participants were allowed to take a short rest while answering the questionnaires; completion took about 20–50 minutes.
Data management and statistical analyses
The scores for the eight subscales provided by the participants with CNP were compared with the nor-mative values provided for the SF-36 Taiwan version [13]. These normative values were derived from the 2001 Health Interview Survey, which established the normative values in a valid sample of 17,515 subjects of aged 12 and above. The normative values of the SF-36 Taiwan version were available with age and sex stratification. We derived the scores from the nor-mative values by matching each patient’s age and sex, and the group was used for comparison. To determine the magnitude of deviation of scores across the eight subscales of HRQOL versus the general population, the age-/sex-matched normative values were sub-tracted from the scores of participants with CNP to derive the impact score [21].
Multivariate analysis of variance was performed for the eight subscales of SF-36 to compare the dif-ference between scores for participants with CNP and age-/sex-matched normative values. The method is commonly used to test the significance of univari-ate repeunivari-ated measures factors with more than two levels, and decreases the type I error from multiple comparison.
The relationships between HRQOL (PCS and MCS) and possible correlated factors (psychological status and demographic data) were tested with Spearman’s correlation coefficients. Statistical analyses were per-formed with SPSS release 14.0 (SPSS Inc., Chicago, IL, USA) for Windows.
R
ESULTSStudy population
A total of 52 patients with CNP participated in this study. One subject was excluded from the study be-cause of incomplete answers on the SF-36-item form. The demographic data for the study participants are shown in Table 1. The number of females (n= 36) was more than twice that of males (n= 15). The age and education level of the participants were widely dis-tributed. The pain severity of patients with CNP
ranged from very mild to very severe; most partici-pants suffered from moderate pain.
HRQOL
We used the eight subscales of SF-36 to explore the HRQOL. The results for study participants with CNP and the age-/sex-matched normative values are shown in Table 2. Considering the physical and men-tal aspects of quality of life, the scores for the eight subscales of participants with CNP were much lower (range, 34.8–70.7) than the age-/sex-matched norma-tive values (range, 66.6–91.3). For the eight subscales, the score was lowest for the RP subscale and highest for the PF subscale. The scores for all subscales for participants with CNP were significantly different from the age-/sex-matched normative score (p< 0.001). The three most strongly affected subscales were RP Table 1. Demographic data of patients with chronic neck pain (n= 51)* Patients Age (yr) 43.6± 13.9 (18–77) < 30 17.7 30–39 25.5 40–49 13.7 50–59 29.4 ≥ 60 13.7 Sex Male 29.4 Female 70.6 Educational level Elementary school 29.4 High school 25.5 University 45.1 Occupation Office worker 37.3 Laborer 15.7 Housewife 29.4 Student 9.8 Retired 7.8 Pain intensity Very mild 3.9 Mild 29.4 Moderate 41.2 Severe 21.6 Very severe 3.9 Diagnosis
Degenerative joint disease 45.1 Herniated intervertebral disc 25.5 Strain and sprain 5.9 Non-specific neck pain 23.5
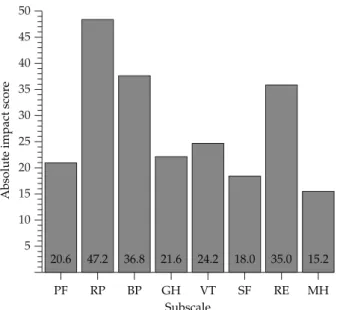
(–47.2), bodily pain (–36.8) and RE (–35.0). The impact scores for the eight subscales are represented in the Figure.
Association with summary measures
We used the summary measures (PCS and MCS) to analyze the relationship between physical/mental HRQOL and demographic/psychological factors. The mean values for EPQ-N, EPQ-E, CHQ-12 and BAI of the study participants were 5.7± 2.7, 7.1 ± 2.9, 3.8± 3.0 and 14.4 ± 9.4, respectively. The distributions of scores for the psychological measures are shown in Table 3. The correlation coefficients of the summary measures are shown in Table 4. BAI was significantly
and moderately correlated with PCS and MCS (r=−0.36 and −0.41, respectively, p < 0.05). The demographic data (age and educational level) were moderately cor-related with PCS (r= −0.46 and 0.37, respectively,
p< 0.05). Psychological status (CHQ-12 and EPQ-N)
was highly/moderately correlated with the MCS score (r= −0.72 and −0.52, respectively, p < 0.01).
D
ISCUSSIONCompared with the Taiwan normative population, patients with CNP in this study showed poor HRQOL, 5 10 15 20 25 30 35 40 45 50
Absolute impact scor
e
PF RP BP GH VT SF RE MH Subscale
20.6 47.2 36.8 21.6 24.2 18.0 35.0 15.2
Figure. Absolute impact scores for the eight subscales of the Short Form-36 in patients with chronic neck pain. PF= physical functioning; RP= role–physical; BP = bodily pain; GH = general health; VT=vitality; SF= social functioning; RE=role–emotional;
MH= mental health.
Table 2.Scores for the eight subscales of the Short Form-36 in patients with chronic neck pain and age-/sex-matched normative values
Subscale Chronic neck pain Age-/sex-matched normative values p
PF 70.7± 20.9 91.3± 7.6 < 0.001 RP 34.8± 41.3 82.0± 9.9 < 0.001 BP 46.1± 16.9 82.9± 5.6 < 0.001 GH 45.5± 19.4 67.1± 7.0 < 0.001 VT 42.4± 21.5 66.6± 4.3 < 0.001 SF 68.4± 23.5 86.4± 3.1 < 0.001 RE 44.4± 44.1 79.4± 4.6 < 0.001 MH 56.8± 22.5 72.1± 2.4 < 0.001
PF= physical functioning; RP = role–physical; BP = bodily pain; GH = general health; VT = vitality; SF = social functioning; RE = role– emotional; MH= mental health.
Table 3. Distribution of scores of psychological mea-sures in patients with chronic neck pain
Patients Neuroticism Extraversion Score domain domain EPQ 0–2 11.8% 3.9% 3–5 31.4% 27.5% 6–8 37.3% 31.4% 9–11 19.6% 31.4% 12–13 – 5.9% CHQ 0–2 43.1% 3–5 31.4% 6–8 17.6% 9–10 7.8% BAI 0–10 39.2% 11–18 31.4% 19–37 29.4%
EPQ= Eysenck Personality Questionnaire; CHQ = Chinese Health Questionnaire; BAI= Beck Anxiety Inventory.
not only in terms of perceived poor physical health status but also poor mental health status. Mental health status was strongly associated with several psycho-logical factors, as indicated by the moderate to high correlation with neuroticism (EPQ-N), psychiatric morbidity (CHQ) and anxiety (BAI).
Considering the physical HRQOL, the scores of the RP and bodily pain subscales were the two with the greatest impact (–47.2 and –36.8, respectively). These results are consistent with previous studies in patients with neck or back pain [4,22]. However, the impact on the PF subscale was smaller, as expected in this study; the impact score was only about –20. It is possible that, because many items (7 of 10) of the PF subscale ask about the limitation of activities on lower extremity function (running, climbing stairs, bending, kneeling, stooping and walking) and only three items correlate to neck or arm function (moving a table, car-rying groceries and bathing or dressing), with neck problems often inducing symptoms of the upper limbs, the PF subscale may inadequately represent items that robustly demonstrate the limitation of PF in patients with CNP.
The important finding of our study was that pa-tients with CNP commonly had poor mental sub-scales in HRQOL. These mental subsub-scales include the RE, mental health (only measuring mental health), general health, vitality, and social functioning sub-scales (measuring both the mental and physical health) [23]. All mental health subscales for patients with CNP were significantly lower than the age-/ sex-matched normative values. The vitality and RE subscales were the two most greatly impacted (–24.2
and –35.0, respectively), and were greater than those reported in other neck pain studies [4]. The reason for this may be due to the chronic condition of the patients, because all of our patients reported symp-toms persisting for over 6 months, while only half of the patients in Daffner’s study reported similar symptom persistence. This may be explained by a four-stage model of pain; the first is the sensory-discriminative dimension, the second is the immedi-ate affective response, the third is pain involving long-term cognitive processes, and the final is pain behavior [24]. Patients with CNP may express more illness-related behaviors in combination with more psychological problems, and these may hamper the ability to participate in activities.
CHQ scores of 3 or more represent people with psychiatric morbidity. In this study, 56.9% of the patients had CHQ scores of 3 or more; therefore, over half of the patients may have psychiatric morbidity. The rate of psychiatric morbidity in this study was high, nearly twice that in Taiwanese communities (about 25%) [17]. Therefore, patients with CNP may need much attention for their psychological problems. The design CHQ-12 includes items focusing on anxi-ety, depression, sleep disturbance, somatic symptoms and interpersonal difficulties [25]. Most patients with CNP may suffer from different psychiatric problems such as depression, anxiety and psychosomatic dis-order. Therefore, consultation with psychiatrists is strongly recommended to assess the psychological condition of patients with CNP. Furthermore, the demo-graphic data of our cases were similar to the popula-tion distribupopula-tion of individuals with depression; thus more detailed assessment of depression may be needed.
Previous studies primarily focused on work-related physical and psychosocial factors associated with neck pain. In fact, the problems in many cases with neck pain are not related to work problems, because the patient groups include retired individuals, house-wives and students. In this study, 47% of the subjects were retirees, housewives or students. Therefore, psy-chological measures focused on personality, anxiety status and depression status are needed for patients with CNP who did or did not work.
This study reported the association between HRQOL, which was assessed using the SF-36 ques-tionnaire, and multiple psychological measures. The MCS score was moderately to highly correlated with Table 4.Correlation coefficients between demographic
data and psychological measures
PCS MCS Demographic data Age −0.46* 0.16 Educational level 0.37† −0.05 Psychological measure CHQ 0.03 −0.72* EPQ-N −0.13 −0.52* EPQ-E 0.29 0.11 BAI −0.36† −0.41* †p< 0.05; *p < 0.01. PCS = physical component summary; MCS= mental component summary; CHQ = Chinese Health Questionnaire; EPQ-N= Eysenck Personality Questionnaire– neuroticism; EPQ-E= Eysenck Personality Questionnaire– extraversion; BAI= Beck Anxiety Inventory.
psychological measures (EPQ-N, CHQ and BAI). Greater neurotic personality scores were associated with higher CHQ scores (psychiatric morbidity) while higher BAI score (more anxiety) were associ-ated with lower MCS scores (poor mental HRQOL). This indicates that, in terms of SF-36 questions, MCS could reflect problems with mental health of patients with CNP.
Our study supports the concept that psychiatric distress and neurotic personality are important fac-tors associated with CNP. A longitudinal study in the general population found a clear trend for increasing incidence of neck pain across high CHQ scores [26]. Psychiatric distress was believed to be important in the transition from acute to chronic spinal pain [9]. Because the SF-36 MCS scores were strongly associ-ated with the CHQ score, low MCS scores may be a good indicator for clinical practice to suspect possi-ble psychiatric morbidity and identify patients who may need further evaluation. Our study found that psychiatric morbidity and neurotic personality were associated with lower MCS scores; however, anxiety was associated with low MCS and low PCS scores. BAI is used to measure the anxiety symptoms in 1 week, while the SF-36 is used to enquire about the HRQOL in 1 month. Therefore, HRQOL may be in-fluenced by anxiety status and may be rated over shorter-term duration for quality measurements. An appropriate educational program would be useful to decrease such anxiety [27]. Good education of patients about neck problems may improve physical and mental HRQOL.
The limitations of our study are worth noting. There was a small number of patients with CNP from a single center. Multicenter studies with larger sam-ple sizes are needed to improve generalizability. Fur-thermore, our study did not focus on individuals with specific diseases; we included many different diag-noses for neck pain. In further studies, the HRQOL and associated factors could be investigated for a spe-cific diagnosis, such as degenerative joint disease or herniated intervertebral disc, and may offer more pre-cise conclusions. Furthermore, in this study, we can-not determine whether perceived poor mental HRQOL induces psychological problems or vice versa. Further studies are needed to analyze how personality, anxi-ety and psychiatric distress influence the self-reported mental health among patients with CNP. Similarly, lon-gitudinal follow-up studies of self-reported mental
health and psychological measures are needed to understand the progression of mental problems in patients with CNP.
This study shows that patients with CNP have poor HRQOL for multiple health problems, both in physical and mental health. Individuals, in whom neuroticism, psychiatric morbidity and high anxiety dominate, show poor self-reported mental HRQOL. We suggest that assessment and treatment of the im-paired physical health and mental health of patients with CNP are necessary.
REFERENCES
1. Strine TW, Hootman JM. US national prevalence and correlates of low back and neck pain among adults.
Arthritis Rheum 2007;57:656–65.
2. Andersen JH, Kaergaard A, Frost P, et al. Physical, psy-chosocial, and individual risk factors for neck/shoulder pain with pressure tenderness in the muscles among workers performing monotonous, repetitive work.
Spine 2002;27:660–7.
3. Viikari-Juntura E, Takala ER, Riihimäki H, et al. Predictive validity of symptoms and signs in neck and shoulders. J Clin Epidemiol 2000;53:800–8.
4. Daffner SD, Hilibrand AS, Hanscom BS, et al. Impact of neck and arm pain on overall health status. Spine 2003;28:2030–5.
5. Demyttenaere K, Bruffacerts R, Lee S, et al. Mental dis-orders among persons with chronic back or neck pain: results from the world mental health surveys. Pain 2007;129:323–42.
6. Wade JB, Price DD, Hamer RM, et al. An emotional component analysis of chronic pain. Pain 1990;40: 303–10.
7. Harkins SW, Price DD, Braith J. Effects of extraversion and neuroticism on experimental pain, clinical pain, and illness behavior. Pain 1989;36:209–318.
8. Lichtenberg PA, Skehan MW, Swensen CH. The role of personality, recent life stress and arthritis severity in predicting pain. J Psychosom Res 1984;28:231–6. 9. Linton SJ. A review of psychological risk factor in back
and neck pain. Spine 2001;25:1148–56.
10. Wade JB, Dougherty LM, Hart RP, et al. A canonical correlation analysis of the influence of neuroticism and extraversion on chronic pain, suffering and pain behavior. Pain 1992;51:67–73.
11. Ware JE Jr, Kosinski M, Bayliss MS, et al. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcome Study. Med Care 1995;33:AS264–79.
12. Lu JFR, Tseng HM, Tsai YJ. Assessment of health-related quality of life in Taiwan (I): development and
psychometric testing of SF-36 Taiwan version. Taiwan J
Public Health 2003;22:501–11.
13. Tseng HM, Lu JFR, Tsai YJ. Assessment of health-related quality of life in Taiwan (II): norming and vali-dation of SF-36 Taiwan version. Taiwan J Public Health 2003;22:512–8.
14. Lu L. University transition: major and minor life stres-sors, personality characteristics and mental health.
Psychol Med 1994;24:81–7.
15. Sato T. The Eysenck Personality Questionnaire Brief Version: factor structure and reliability. J Psychol 2005; 139:545–52.
16. Chong MY, Wilkinson G. Validation of 30- and 12-item versions of the Chinese Health Questionnaire (CHQ) in patients admitted for general health screening.
Psychol Med 1989;19:495–505.
17. Cheng TA. A community study of minor psychiatric morbidity in Taiwan. Psychol Med 1988;18:953–68. 18. Chen CS, Tsang HT, Chong MY, et al. Validation
of the Chinese Health Questionnaire (CHQ-12) in community elders. Kaohsiung J Med Sci 2000;16: 559–65.
19. Beck AR, Epstein N, Brown G, et al. An inventory for measuring clinical anxiety: psychometric properties.
J Consult Clin Psychol 1988;56:893–7.
20. Creamer M, Foran J, Bell R. The Beck Anxiety Inventory in a non-clinical sample. Behav Res Ther 1995;33:477–85. 21. King JT Jr., McGinnis KA, Roberts MS. Quality of life assessment with the medical outcomes study short form-36 among patients with cervical spondylotic myelopathy. Neurosurgery 2003;52:113–21.
22. Pahl MA, Brislin B, Boden S, et al. The impact of four common lumbar spine diagnoses upon overall health status. Spine J 2006;6:125–30.
23. Ware JE, Snow KK, Kosinski M, et al. SF-36 Health
Survey: Manual and Interpretation Guide. 1st edition.
Lincoln: QualityMetric, 2000;3:1–10.
24. Price DD, Harkins SW, Baker C. Sensory-affective rela-tionships among different types of clinical and experi-mental pain. Pain 1987;28:297–307.
25. Cheng TA, Williams P. The design and development of a screening questionnaire (CHQ) for use in community studies of mental disorders in Taiwan. Psychol Med 1986;16:415–22.
26. Croft PR, Lewis M, Papageorgiou AC, et al. Risk fac-tors for neck pain: a longitudinal study in the general population. Pain 2001;93:317–25.
27. Lue YJ, Chang JK, Liu MF, et al. Anxiety in patients with lower extremity arthroplasty. Formos J Phys Ther 2003;28:317–23.
收文日期:98 年 5 月 21 日 接受刊載:98 年 9 月 23 日 通訊作者:呂怡靜助理教授 高雄醫學大學健康科學院物理治療學系 高雄市 807 三民區十全一路 100 號
慢性頸部疼痛病患之生活品質與
其心理因子之相關性探討
林榮豐1,2 張志仲3,4 呂衍謀5 黃茂雄4 呂怡靜4,6 1 慈惠醫護管理專科學校 物理治療科 高雄醫學大學 2行為科學研究所 3健康科學院 職能治療學系 6物理治療學系 高雄醫學大學附設醫院 4復健科 5骨科 本研究的目的為探討慢性頸部疼痛患者健康相關生活品質和探討其相關之因素。研究 方法以自我健康狀態量表 SF-36 (Short Form-36)評估慢性頸部疼痛患者之健康相 關生活品質,並與台灣常模比較。為研究心理因素對健康相關生活品質的影響,以艾 氏 人 格 問 卷(Eysenck Personality Questionnaire, EPQ), 華 人 健 康 問 卷 (Chinese Health Questionnaire, CHQ), 與 貝 氏 焦 慮 量 表(Beck AnxietyInventory, BAI) 評 估。 並 檢 驗 各 因 素 與 SF-36 生 理 功 能 總 分(physical components summary, PCS)與心理功能總分(mental components summary, MCS) 之 相 關 性。 結 果 發 現 病 患 之 SF-36 全 部 8 個 面 向 顯 著 低 於 常 模(p < 0.001)。其中影響最大的面向為生理功能受限情形(role-physical)與身體疼痛情
形(bodily pain)。患者之 PCS 與年齡(rho = –0.43)、教育水準(rho = 0.37) 及 BAI(rho = –0.36)得分有中度相關;而 MCS 與 CHQ 得分(rho = –0.72)、神 經質面向之 EPQ 得分(rho = –0.52)及 BAI 得分(rho = –0.41)有中度到高度相 關。有神經質人格、輕度憂鬱狀態傾向和較高的焦慮狀態者會呈現較差的心理健康狀 態。結論,慢性頸部疼痛患者呈現多面向健康相關生活品質較差,不僅表現在身體健 康狀況,也表現在心理健康狀況。慢性頸部疼痛患者自覺心理健康之生活品質與各種 心理因素有高度相關,因此提供患者完整的生理與心理評估,瞭解慢性頸部疼痛者生 理與心理健康狀況對規劃治療計畫將有助益。 關鍵詞:慢性頸部疼痛,心理健康,生活品質,自我健康狀態量表 ( 高雄醫誌 2010;26:13–20)