Regular Article
The Chinese version of the Davidson Trauma Scale:
A practice test for validation
CHIN-HUNG CHEN, md,1SHIH-KU LIN, md,2,3HWA-SHENG TANG, md,2
WINSTON W. SHEN, md3,4AND MONG-LIANG LU, md,ms3,4
1Department of Psychiatry,Tsao-Tun Psychiatric Center, Nantao,2Department of Psychiatry,Taipei City Psychiatric Center,Taipei,3Department of Psychiatry, School of Medicine,Taipei Medical University,Taipei, 4Department of Psychiatry,Taipei Medical University-Municipal Wanfang Hospital,Taipei,Taiwan
Abstract The Chinese version of the Davidson Trauma Scale (DTS-C) was developed to respond to the need of Chinese-speaking individuals. The DTS is a validated self-rating scale used in the diagno-sis of posttraumatic stress disorder (PTSD). The DTS-C is translated from DTS through a two-stage translation. Subjects were drawn from a sample of 210 survivors of the 21 September 1999, Chi-Chi Earthquake. The scale showed good internal consistency (Cronbach’s a = 0.97) and test–retest reliability (r= 0.88). Concurrent validity was obtained against the clinical diagnostic interview, with a diagnostic accuracy of 0.85 at DTS-C score of 44. It showed that the sensitivity was 0.9, specificity 0.81, positive likelihood ratio 4.74, and negative likelihood ratio 0.12. The rec-ommended stratum-specific likelihood ratios were 0.10 (95% CI: 0.05–0.20) for the score range 0–39, 4 (2.22–7.23) for the score range of 40–59, and 6.14 (3.42–11.02) for the scores above 60. In PTSD diagnosed subjects, the factor structures closely resembled the DSM-IV grouping of PTSD symptoms. The psychometric strength of DTS-C is reliable for its future use, particularly for screening for subjects with possible diagnosis of PTSD.
Key words Davidson Trauma Scale, earthquake, post-traumatic stress disorder, rating scale, Taiwan.
INTRODUCTION
Posttraumatic stress disorder (PTSD) is a disabling and chronic illness. Patients who suffer from PTSD have either experienced or witnessed a life-threatening trauma usually involving death or severe injury. This event is followed by intense feelings of fear, helplessness, or horror that may be associated with persistent re-experiencing of the event, particu-larly reliving or dreaming of the event.1Patients may
feel out of control and suffer from significant morbid-ity with occupational dysfunction and difficulty main-taining interpersonal relationships. Traumatic events that may lead to develop PTSD, include military combat, violent physical or sexual assault, severe
traffic accidents, natural disasters, etc. The National Comorbidity Survey estimates that the lifetime preva-lence of PTSD is 8% in the general population with
10.4% in women and 5% in men.2
On 21 September 1999, an earthquake hit Taiwan with a magnitude of 7.3 on the Richter scale. The 921 Chi-Chi Earthquake caused more than 2000 deaths, injured more than 8000 people, and damaged or destroyed more than 30 000 homes. Many survivors suffer from PTSD. However, the reported PTSD rates after natural disasters varied widely, ranging from
1.5% in a population affected by Hurricane Andrew3
to 67% in Armenian earthquake victims.4The
dispar-ity in postdisaster PTSD rates may be due to meth-odological differences, including differences in the magnitudes of disasters, the time elapsed between the onset of the disaster and data collection, the methods of sampling and case detection, and the diagnostic cri-teria. The survivors’ ethnicity and culture may also determine the occurrence of PTSD.5
The clinical structured interview has been regarded
as the gold standard of PTSD measurement.6 These
Correspondence address: Mong-Liang Lu, Department of Psychiatry, Taipei Medical University-Municipal Wanfang Hospi-tal, No. 111, Hsing-Long Road, Sec. 3, Taipei, Taiwan. Email: mongliang@sinamail.com
Received 14 December 2000; revised 16 February 2001; accepted 27 February 2001.
interviews include the Structured Clinical Interview
for DSM-III-R (SCID),7the PTSD Interview
(PTSD-I),8the Clinician-administered PTSD Scale (CAPS),9
and the Structured Interview for PTSD (SIP).10 The
extensive use of these instruments has shown good psychometric reliability and validity. However, the major drawback of clinical structured interviews is that they are time-consuming. Therefore, self-rating scales may have clinical utility, especially in mass screening. A number of self-rating scales have been developed to assess PTSD symptoms. They include the Impact of Event Scale (IES),11the Mississippi Scale for
Combat-related PTSD (M-PTSD),12the Penn Inventory,13and
the Davidson Trauma Scale (DTS).14
The DTS is a validated 17-item self-rating scale of frequency and severity.14 The DTS items reflect the
PTSD symptoms as defined in DSM-IV.1 For each
item, the subject rates both frequency and severity during the previous week on a 5-point (0–4) scale for a total possible score of 136. The DTS has been shown to have good test–retest reliability (g = 0.86) and internal consistency (Cronbach’s a = 0.99).14 The
original DTS has the best diagnostic efficiency (83%) when the cutoff score is 40. The major strengths of DTS include its administration in a broad population of men and women exposed to different trauma, its sensitivity to detect treatment-induced changes across time, its capability of distinguishing the outcomes of different treatments, and its ability to predict later treatment response.
Four senior psychiatrists who are proficient in both English and Chinese translated DTS into Chinese through a two-stage translation with permission from Dr JRT Davidson and the agreement of Multi-Health System Inc. Two psychiatrists independently trans-lated the DTS from English to Chinese (front
transla-tion). Another two psychiatrists independently
translated the items of the front translation back to English (back translation). The final translation version was obtained after incorporating Dr Davidson’s suggestions for consistencies in item content or meaning.
The purpose of this study was to evaluate empiri-cally the reliability and validity of DTS-C on the samples exposed to earthquake trauma in Taiwan.
METHODS
Subjects and procedures
A total of 210 Taiwanese (men 83, and women 127) participated in the study. They came from three differ-ent sources: specific clinics in the earthquake area (n= 112), survivors living in the assembly houses (n= 63),
and disaster rescuers (n= 35). The mean age (± SD)
was 34.9± 12.7 years ranging from 15 to 74 years.
The demographic characteristics of survivors living in assembly houses and patients of specific clinics were similar. However, the demographic characteristics of disaster rescuers were quite different. All rescuers were male, aged 20–40 years, with relatively high edu-cational levels. All subjects underwent a clinical inter-view by senior psychiatrists to make the diagnosis. The psychiatrists interviewing the subjects remained blind to the results of DTS-C. Three psychiatrists who re-viewed the DSM-IV criteria together for PTSD before the investigation conducted the clinical interviews. All psychiatrists were certified in the psychiatric subspe-cialty and had at least 5 years experience in general psychiatric practice. All psychiatrists interviewed the first 10 respondents together and had 100% agreement in diagnosing whether the subjects suffered from PTSD. In addition, all subjects completed the 17-item DTS-C. The assessment was conducted during the period of 1–3 months after the earthquake.
Analyses
Cronbach’s a was used to evaluate the internal con-sistency.15 Test–retest reliability was assessed using
analysis of variance (anova) intraclass correlation coefficient (ICC) approach. Sensitivity, specificity, pre-dictive value, and efficiency were calculated according to standard formulae. Receiver operating characteris-tic (ROC) analysis was used to optimize the cut-off point for DTS-C.16,17 Likelihood ratios for the test
results were also calculated. Positive likelihood ratio (PLR) with a positive test result is an index of the increased likelihood that a disease is present, and is calculated by sensitivity/(1 – specificity).18 A PLR
score of 3 is considered moderately positive and a score of 10 is considered strongly positive. Negative likelihood ratio (NLR) with a negative test result is an index of the increased likelihood that a disease is absent, and is calculated by (1 – sensitivity)/specificity. An NLR score of 1 is considered neutral, and a score of 0.1 is considered strongly negative.18
However, problems for researchers and clinicians arise when possible results include non-positive and non-negative results, frequently described as interme-diate or un-interpretable results. Important informa-tion is lost with the single forced cut-off point, since all subjects are divided into two groups (e.g., cases and non-cases). The stratum-specific likelihood ratio is calculated by the proportion of diseased subjects with a test result in a given range divided by the pro-portion of non-diseased subjects with a test result in the same given range.19–21 The likelihood ratio for a
stratum with the upper and lower bounds (scores) x and y corresponding to the change in sensiti-vity divided by the change in specificity over the de-fined interval: LR(x,y)= [sensitivity(x) – sensitivity(y)] /[specificity(y) – specificity(x)]. Therefore, LR(x,y) cor-responds to the slope between two points, x and y, on the ROC curve. Confidence intervals can be com-puted as a measure of precision for the estimated likelihood ratios.22 The number of strata should be
chosen carefully, because with too many strata the likelihood ratios become unstable and degenerate. Following Peirce and Cornell20 and Furukawa et al.,21
the following rules are recommended: (i) provide suf-ficient abnormal and normal cases in each stratum to allow the stratum-specific likelihood ratio (SSLR) to be monotonically related, and (ii) collapse those strata where the SSLR are close to one another and their 95% confidence intervals easily overlap.
RESULTS
Internal consistency and test–retest reliability In all 210 subjects, Cronbach’s a for the frequency and severity items was 0.97, for the frequency items alone 0.93, and for the severity item alone 0.95.
Test–retest reliability was examined by comparing the baseline DTS-C score with a DTS-C assessment 1 week later. The subjects only included those who claimed ‘no change in PTSD symptoms’ and agreed to receive a second DTS-C assessment. Among 210 sub-jects, 82 subjects were recruited for the assessment of test–retest reliability. The test–retest reliability was 0.87 (P< 0.0001).
Concurrent validity
The results of clinical diagnostic interview were used to assess concurrent validity. Of 210 subjects, only 84
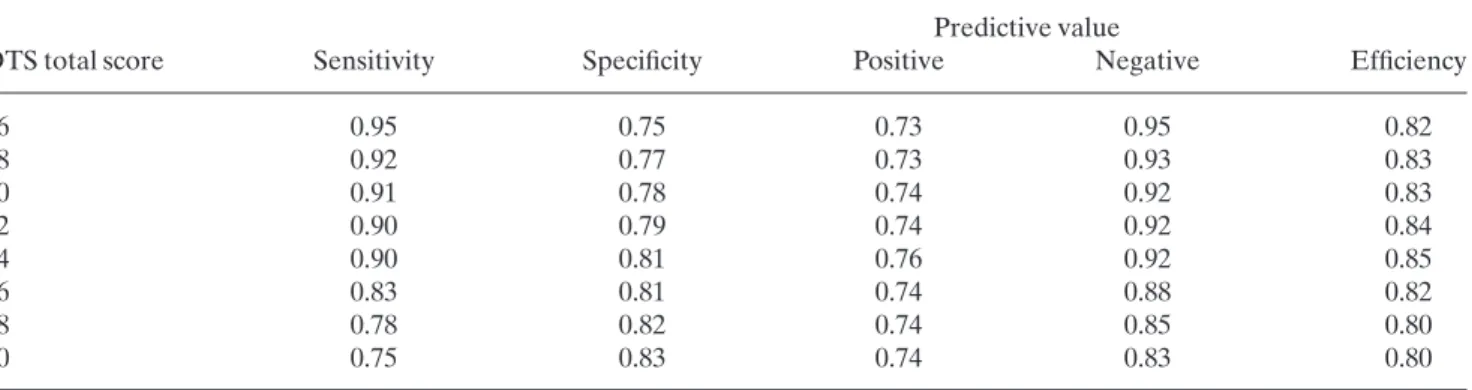
had a diagnosis of PTSD. Sensitivity, specificity, predictive value, and efficacy were calculated for all possible DTS-C scores. Table 1 shows eight different threshold scores and their corresponding sensitivity, specificity, positive and negative predictive values, and efficiency (percentage correctly categorized as with or without PTSD). The highest efficiency was found at a total score of 44. The area under the curve (± standard error) was 0.92 (± 0.02). The positive likelihood ratio was 4.74, and the negative likelihood ratio 0.12.
The recommended SSLR were 0.10 (95% CI: 0.05–0.20) for the score range 0–39, 4 (2.22–7.23) for the score range of 40–59, and 6.14 (3.42–11.02) for the scores above 60.
Factorial structures
Principal component analysis of DTS-C data on all 210 subjects revealed the presence of three main factors. The first factor was a common factor and accounted for 50% of the variance. The second factor which accounted for 9% of the variance mainly con-sisted of negative loading on numbness and avoidance items. The third factor which accounted for 5.6% of the variance mainly consisted of negative loading on hyperarousal items.
When principal component analysis was conducted using only subjects with a current PTSD diagnosis
(n= 84), eight factors were found with eigenvalues
exceeding unity, accounting for 73.3% of the total vari-ance. The DTS-C symptom correlation matrix was determined to be appropriate for factor analysis:
Kaiser-Meyer-Olkin measure of sampling adequency =
0.76 and Bartlett’s test of sphericity = 3641.18, P < 0.0001. We used the scree test to determine the appro-priate number of factors to be retained. The first four factors, accounting for 57.3% of total variance, were retained on the basis of the test. This four-factor
Table 1. Sensitivity, specificity, predictive value, and efficiency of the Chinese version of the Davidson Trauma Scale for eight selected total scores
Predictive value
DTS total score Sensitivity Specificity Positive Negative Efficiency
36 0.95 0.75 0.73 0.95 0.82 38 0.92 0.77 0.73 0.93 0.83 40 0.91 0.78 0.74 0.92 0.83 42 0.90 0.79 0.74 0.92 0.84 44 0.90 0.81 0.76 0.92 0.85 46 0.83 0.81 0.74 0.88 0.82 48 0.78 0.82 0.74 0.85 0.80 50 0.75 0.83 0.74 0.83 0.80
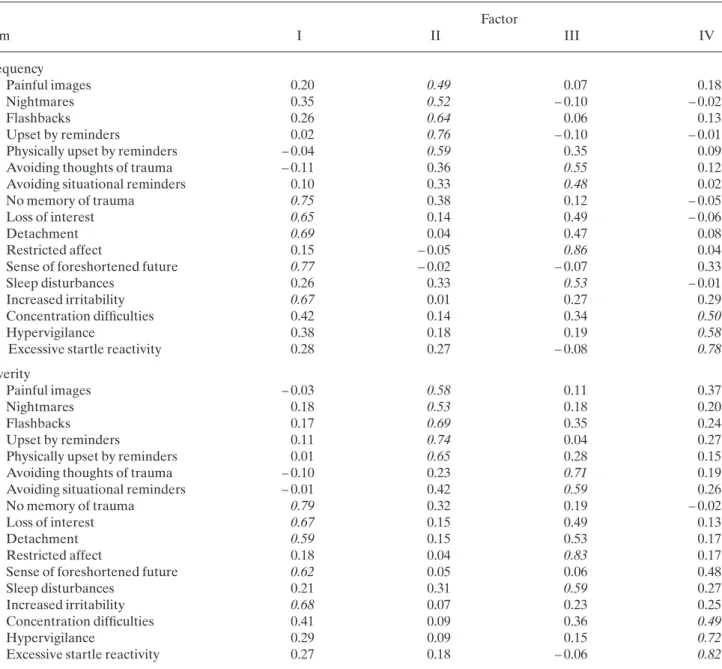
solution was then applied in a further principal axis factor analysis with varimax rotation for interpreta-tion. Table 2 shows the factorial structure from this analysis.
It was possible to construct four factors: numbness
(factor I, eigenvalue = 11.06, % of variance =
32.52%), intrusive re-experiencing (factor II,
eigen-value = 3.24, % of variance = 9.54%), avoidance
(factor III, eigenvalue = 2.62, % of variance = 7.69%), and hyperarousal (factor IV, eigenvalue = 2.57, % of variance = 7.55%). Factor I had five items: no memory
of trauma, loss of interest, detachment, sense of fore-shortened future, and increased irritability. They are classified into the numbness cluster of DSM-IV PTSD criteria, except increased irritability. Factor II in-cluded five items: painful images, nightmares, flash-backs, upset by reminders, and physically upset by reminders. They belonged to the intrusive re-experiencing cluster. Factor III included four items: avoiding thoughts of trauma, avoiding situational reminders, restricted affect, and sleep disturbance. Factor IV included three items: concentration
difficul-Table 2. Factor loadings for each item in the Chinese version of the Davidson Trauma Scale for frequency and severity domains using only subjects with posttraumatic stress disorder
Factor Item I II III IV Frequency 1. Painful images 0.20 0.49 0.07 0.18 2. Nightmares 0.35 0.52 – 0.10 – 0.02 3. Flashbacks 0.26 0.64 0.06 0.13 4. Upset by reminders 0.02 0.76 – 0.10 – 0.01
5. Physically upset by reminders – 0.04 0.59 0.35 0.09
6. Avoiding thoughts of trauma – 0.11 0.36 0.55 0.12
7. Avoiding situational reminders 0.10 0.33 0.48 0.02
8. No memory of trauma 0.75 0.38 0.12 – 0.05
9. Loss of interest 0.65 0.14 0.49 – 0.06
10. Detachment 0.69 0.04 0.47 0.08
11. Restricted affect 0.15 – 0.05 0.86 0.04
12. Sense of foreshortened future 0.77 – 0.02 – 0.07 0.33
13. Sleep disturbances 0.26 0.33 0.53 – 0.01
14. Increased irritability 0.67 0.01 0.27 0.29
15. Concentration difficulties 0.42 0.14 0.34 0.50
16. Hypervigilance 0.38 0.18 0.19 0.58
17. Excessive startle reactivity 0.28 0.27 – 0.08 0.78
Severity
1. Painful images – 0.03 0.58 0.11 0.37
2. Nightmares 0.18 0.53 0.18 0.20
3. Flashbacks 0.17 0.69 0.35 0.24
4. Upset by reminders 0.11 0.74 0.04 0.27
5. Physically upset by reminders 0.01 0.65 0.28 0.15
6. Avoiding thoughts of trauma – 0.10 0.23 0.71 0.19
7. Avoiding situational reminders – 0.01 0.42 0.59 0.26
8. No memory of trauma 0.79 0.32 0.19 – 0.02
9. Loss of interest 0.67 0.15 0.49 0.13
10. Detachment 0.59 0.15 0.53 0.17
11. Restricted affect 0.18 0.04 0.83 0.17
12. Sense of foreshortened future 0.62 0.05 0.06 0.48
13. Sleep disturbances 0.21 0.31 0.59 0.27
14. Increased irritability 0.68 0.07 0.23 0.25
15. Concentration difficulties 0.41 0.09 0.36 0.49
16. Hypervigilance 0.29 0.09 0.15 0.72
17. Excessive startle reactivity 0.27 0.18 – 0.06 0.82
ties, hypervigilance, and excessive startle reactivity. They are classified into the hyperarousal cluster. The factor structures of subjects with PTSD closely resembled the symptom clusters of DSM-IV.
DISCUSSION
Davidson Trauma Scale, which was developed as a self-rating scale measuring frequency and severity of each DSM-IV PTSD symptom, showed good internal consistency and test–retest reliability in English
ver-sion. The Cronbach’s a of DTS-C was 0.97, and that
of DTS 0.99. The test–retest reliability of DTS-C was 0.88, and that of DTS 0.86 in DTS. The DTS-C also showed good reliability as compared with the English version of DTS. The test–retest interval was 7 days in our study. However, the longer the test–retest inter-val, the greater the possibility of changes in the clini-cal conditions. Therefore, only subjects who claimed no changes in clinical conditions entered this reliabil-ity study. Due to the stressful experiences about the earthquake, some subjects refused to have the second assessment. Consequently, only 82 subjects were
enrolled in the test–retest study, nevertheless
the result of test–retest reliability was still quite satisfactory.
The best diagnostic accuracy was 85% when the cut-off point of DTS-C was 44. The optimum cut-off point of DTS-C was slightly higher than that of DTS. The difference could be due to the many reasons. The characteristics and severity of stressor may influence risk of developing PTSD.23,24The Chi-Chi Earthquake
was one of the most devastating natural disasters in Taiwan. Our subjects were all lived in the major earthquake area and suffered traumatic experiences. Therefore, they might have greater risk of developing PTSD and have more severe PTSD symptoms. Sam-pling bias might have effects. Our respondents who were all earthquake-related subjects, had the same painful experiences about this natural disaster and could be more willing to talk about them.3The
influ-ence of media might also contribute to it. After the earthquake, television programs and newspapers con-tinued to feature the PTSD. People who knew much about these diseases, could admit the symptoms more easily.4The gender differences might also contribute
to it. Female gender may be the risk factor for PTSD.2
Female subjects constitute 60% of respondents in the present study, but have only 40% in DTS study.
The best cut-off point to achieve optimum sensitiv-ity and specificsensitiv-ity may vary considerably from one setting to another. As theoretically predicted, the positive and negative predictive values for each recommended cut-off point often differ significantly
among studies when the base rate was different. The fixed ‘optimal’ cut-off point approach cannot accom-modate the wide variations actually present in clinical practices. SSLR have been advocated as a more infor-mative alternative to the fixed threshold approach. SSLR, like the sensitivity and specificity but unlike the positive and negative predictive values and unlike the single ‘optimal’ cut-off point, do not depend on the base rate of target disorder.20 SSLR reduce the
spectrum bias that might arise if only two categories (cases and non-cases) are chosen.21Therefore, SSLR
is an alternative methodology for analyzing test results that adapt to populations with different preva-lence of mental disorders.
Factor analysis of the sample as a whole revealed that the factor structure of DTS-C did not correspond to the group clusters of DSM-IV. Factor analysis of subjects with PTSD revealed that the factor structure of the DTS-C was near to the DSM-IV formulation of symptom groupings in PTSD. However, there are three items misclassified into different symptom clus-ters. Several factors might contribute to the differ-ence. The DTS-C measured each DSM-IV symptoms of PTSD on 5-point frequency and severity scales rather than dichotomus scales. This difference might have influence on factor structures. Several previous studies showed that the DSM symptom clusters of PTSD could not always be detected in factor-analyti-cal study.14,25,26 Critics may argue that DSM criteria
are imperfect and that PTSD instruments should not be limited by them. Most individuals with PTSD meet the criteria for at least one other psychiatric disorder,2
particularly major depressive disorder. High rates of comorbidity may suggest an epiphenomenon of the diagnostic criteria used.27
The translation and use of psychiatric rating scales in languages and populations other than those for which they were developed, is based on the assump-tion that psychological disturbances or psychiatric dis-orders are constant, or at least very similar, between cultures.28 No truly etic self-reported measures exist
because all of these tests are ultimately based on the respondents’ subjective sense of distress, which is a function of culture and language and requires an emic perspective.29 Previous research revealed that PTSD
seemed to surmount the barriers of culture and lan-guage.30–32Our DTS-C through a two-stage translation
may minimize the influences of culture and language. There are some limitations of our studies. Our sub-jects are all earthquake-related victims. The applica-tion to other populaapplica-tions (e.g. criminal violence, traffic accident, etc.) requires further study. About 10% of our research subjects, especially the elder, are illiterate. The interviewee had to read the scale for
these illiterate subjects, then record according to their response. Therefore, we had to design a guideline of the spoken DTS-C for interviewee. But some dialect and culture differences still exist between individuals, and some minor modifications in spoken DTS-C were necessary. All our research subjects belong to a popu-lation with high rate of PTSD. The reliability and validity of DTS-C needs to be assessed in larger and non-skewed populations.
CONCLUSIONS
In summary, the psychometric strength documented in this presented study of the DTS-C is relatively reli-able for its future use. Slight language modifications might be needed because of different dialects among Chinese ethnic groups. Further studies are required to establish the clinical and research utility of the DTS-C in other populations including a general primary care setting where the prevalence of PTSD is low. REFERENCES
1. American Psychiatric Association. Diagnostic and Sta-tistical Manual of Mental Disorders, 4th edn. American Psychiatric Association, Washington DC, 1994.
2. Kessler RC, Sonnega A, Bromet E, Hughes MA, Nelson CB. Posttraumatic stress disorder in the national comor-bidity survey. Arch. Gen. Psychiatry 1995; 52: 1048–1060. 3. Garrison CZ, Bryant ES, Addy CL, Spurrier PG, Freedy JR, Kilpatrick DG. Posttraumatic stress disorder in ado-lescents after Hurricane Andrew. J. Am. Acad. Child. Adolesc. Psychiatry 1995; 34: 1193–1201.
4. Goenjian AK, Najarian LM, Pynoos RS et al. Posttrau-matic stress disorder in elderly and younger adults after the 1988 earthquake in Armenia. Am. J. Psychiatry 1994; 151: 895–901.
5. World Health Organization. Psychological Conse-quences of Disasters: Prevention and Management. World Health Organization, Geneva, 1992.
6. Gerardi R, Keane TM, Penk W. Sensitivity and speci-ficity in developing diagnostic tests of combat-related post-traumatic stress disorder (PTSD). J. Clin. Psychol. 1989; 45: 691–703.
7. Spitzer RL, Williams JBW, Gibbons ML, First MB. Structured Clinical Interview for DSM-III-R. American Psychiatric Press Inc, Washington DC, 1990.
8. Watson CG, Juba MP, Maniford V et al. The PTSD inter-view: Rationale, description, reliability, and concurrent validity of a DSM-III-based technique. J. Clin. Psychol. 1991; 47: 179–188.
9. Blake DD, Weathers FW, Nagy LM et al. The develop-ment of a clinician-administered PTSD scale. J. Trauma Stress 1995; 8: 75–90.
10. Davidson JRT, Malik MA, Travers J. Structured interview for PTSD (SIP): Psychometric validation for DSM-IV criteria. Depress. Anxiety 1997; 5: 127–129.
11. Horowitz M, Wilner N, Alvarez W. Impact of event scale: A measure a subjective distress. Psychosom. Med. 1979; 41: 209–218.
12. Keane TM, Caddell JM, Taylor KL. Mississippi scale for combat-related posttraumatic stress disorder: Three studies in reliability and validity. J. Consul. Clin. Psychol. 1988; 56: 85–90.
13. Hammarberg M. Penn inventory for posttraumatic stress disorder: Psychometric properties. Psychol. Assess. 1992; 4: 67–76.
14. Davidson JRT, Book SW, Colket JT et al. Assessment of a new self-rating scale for posttraumatic stress disorder. Psychol. Med. 1997; 27: 153–160.
15. Cronbach LJ. Coefficient alpha and the internal struc-ture of tests. Psychometrika 1951; 16: 297–334.
16. Swets JA. ROC analysis applied to the evaluation of medical imaging techniques. Invest. Radiol. 1979; 14: 365–377.
17. Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 1982; 143: 29–36.
18. Rampes H, Warner JP, Blizard R. How to appraise an article on diagnosis. Psychiatr. Bull. 1998; 22: 506–509. 19. Simel DL, Samsa GP, Matchar DB. Likelihood ratios for
continuous test results: Making the clinicians’ job easier or harder. J. Clin. Epidemiol. 1993; 46: 85–93.
20. Peirce JC, Cornell RG. Integrating stratum-specific like-lihood ratios with the analysis of ROC curves. Med. Decision Making 1993; 13: 141–151.
21. Furukawa T, Hirai T, Kitamura T, Takahashi K. Applica-tion of the Center for Epidemiologic Studies Depres-sion Scale among first-visit psychiatric patients: A new approach to improve its performance. J. Affect Disord. 1997; 46: 1–13.
22. Simel DL, Samsa GP, Matchar DB. Likelihood ratios with confidence: Sample size estimation for diagnostic test studies. J. Clin. Epidemiol. 1991; 44: 763–770. 23. Shore JH, Tatum E, Vollmer WM. Psychiatric reactions
to disaster: The Mt. St. Helen’s experience. Am. J. Psy-chiatry 1986; 143: 590–595.
24. Winfield I, George LK, Swartz M, Blazer DG. Sexual assault and psychiatric disorders among a community sample of women. Am. J. Psychiatry 1990; 147: 335– 341.
25. Davidson J, Smith R, Kudler H. Validity and reliability of the DSM-III criteria for posttraumatic stress disor-der: Experience with a structured interview. J. Nerv. Ment. Dis. 1989; 177: 336–341.
26. Taylor S, Kuch K, Koch WJ, Crockett DJ, Passey G. The structure of posttraumatic stress symptoms. J. Abnorm. Psychol. 1998; 107: 154–160.
27. Keane T, Kaloupek D. Comorbid psychiatric disorders in PTSD. Ann. NY. Acad. Sci. 1997; 821: 24–34.
28. Kinzie JD, Manson SM. The use of self-rating scales in cross-cultural psychiatry. Hosp. Community Psychiatry 1987; 38: 190–196.
29. Alarcón RD, Westermeyer J, Foulks EF, Ruiz P. Clinical relevance of contemporary psychiatry. J. Nerv. Ment. Dis. 1999; 187: 465– 471.
30. Sack WH, Seeley JR, Clarke GN. Does PTSD transcend cultural barriers? A study from the Khmer adolescent refugee project. J. Am. Acad. Child. Adolesc. Psychiatry 1997; 36: 49–54.
31. Howard WT, Loberiza FR, Pfohl BM, Thorne PS, Mag-pantay RL, Woolson RF. Initial results, reliability, and
validity of a mental health survey of Mouth Pinatubo disaster victims. J. Nerv. Ment. Dis. 1999; 187: 661–672. 32. Wang X, Gao L, Shinfuku N, Zhang H, Zhao C, Shen Y.
Longitudinal study of earthquake-related PTSD in a randomly selected community sample in north China. Am. J. Psychiatry 2000; 157: 1260–1266.