2014/April/2
Type of manuscript: Original article
• Manuscript title: Increased risk of pulmonary tuberculosis among patients with appendectomy in Taiwan
• Running head: appendectomy and pulmonary tuberculosis • Authors’ full names:
Shih-Wei Lai1,2, Cheng-Li Lin3,4, Kuan-Fu Liao5,6,Sung-Mao Tsai6
1School of Medicine, China Medical University and 2Department of Family
Medicine, China Medical University Hospital, Taichung, Taiwan
3Department of Public Health, China Medical University and 4Management
Office for Health Data, China Medical University Hospital, Taichung, Taiwan 5Graduate Institute of Integrated Medicine, China Medical University, and
6Department of Internal Medicine, Taichung Tzu Chi General Hospital,
Taichung, Taiwan
• Corresponding author: Kuan-Fu Liao
Department of Internal Medicine, Taichung Tzu Chi General Hospital, No.66, Sec. 1, Fongsing Road, Tanzi District, Taichung City, 427, Taiwan
Phone: 886-4-2205-2121 Fax: 886-4-2203-3986
E-mail: kuanfuliao@yahoo.com.tw
ABSTRACT
Background. The aim of this study was to determine whether there is a relationship between appendectomy and pulmonary tuberculosis in Taiwan. Methods. We designed a case-control study by analyzing the database from the Taiwan National Health Insurance Program. In total, we found 11366 individuals (aged 20 years and older) with newly diagnosed pulmonary tuberculosis as the case group and 45464 individuals without pulmonary tuberculosis as the control group from 1998 to 2011. The case group and the control group were matched on sex, age and index year of diagnosing pulmonary tuberculosis. Using the multivariable unconditional logistic regression model, we measured the odds ratio (OR) and 95% confidence interval (CI) for risk of pulmonary tuberculosis associated with appendectomy and other
comorbidities. Results. After controlling for covariables, the multivariable unconditional logistic regression model disclosed that the OR of pulmonary tuberculosis was 1.4 in appendectomized patients (95% CI= 1.13, 1.75), when compared to individuals without appendectomy. In further analysis, co-morbid with chronic obstructive pulmonary diseases (OR = 4.63, 95% CI= 3.21, 6.68),
pneumoconiosis (OR = 7.80, 95% CI= 1.43, 42.5), chronic kidney diseases (OR = 5.65, 95% CI= 1.79, 17.8) or diabetes mellitus (OR = 2.11, 95% CI= 1.30, 3.44) increased the risk of pulmonary tuberculosis in appendectomized patients. Conclusions. Individuals with appendectomy are at a 1.4-fold increased risk of pulmonary tuberculosis. Comorbidities, including chronic obstructive pulmonary disease, pneumoconiosis, chronic kidney diseases and diabetes mellitus, enhance the risk of pulmonary tuberculosis.
INTRODUCTION
The real function of the appendix remains uncertain, but recent studies have reported it could be associated with immune function. Appendix can be recognized as a primary lymphoid organ because various kinds of immunoglobulin are detected in it . Some investigators found that the appendix could be a priming site related to the development of ulcerative colitis . Therefore, appendectomy might be associated with deceased risk of ulcerative colitis. To the contrary, appendectomy seems to be
associated with increased risk of irritable bowel syndrome, Crohn's disease, acute myocardial infarction and Clostridium difficile infection , which can be partially explained by the mechanism that removing the appendix may change immune function .
To date, tuberculosis remains a major public health concern. The annual incidence varies in the world, around from 4.3 to 231/100,000 population . Pulmonary
tuberculosis is the most common tuberculotic disorder. To the best of our knowledge, little is known about the relationship between appendectomy and pulmonary
tuberculosis. Base on the appendix having immune function and cell mediated immunity as the major immune response of tuberculosis, we hypothesize that there could be a link between appendectomy and pulmonary tuberculosis. If a relation exists, more attention can be focused on these two conditions simultaneously.
Therefore, we conducted a population-base study to explore the following questions: (1) whether appendectomized patients are at increased risk for pulmonary
tuberculosis, (2) whether there is a joint effect between appendectomy and other comorbidities on risk of pulmonary tuberculosis.
MATERIALS AND METHODS Data Sources
We designed a case-control study by analyzing the database from the National Health Insurance Program in Taiwan. The details of the insurance program have been
documented previously . Briefly, The Taiwan National Health Insurance Program began in March 1995 and covered approximately 99% of the whole 23 million residents . To maintain patient privacy, all types of personal identification on files connecting with this study were replaced with surrogate identification numbers. This study was approved by the Institutional Review Board of China Medical University and Hospital (CMU-REC-101-012).
Participants
Using the International Classification of Diseases 9th Revision-Clinical
Modification (ICD-9 codes), we defined individuals with new diagnosis of pulmonary tuberculosis as the case group during the period of 1998-2011 (ICD-9 codes 010, 011, 012 and 018), who were 20 years of age and older at the date of diagnosis. We
defined the index date as the date of diagnosing pulmonary tuberculosis. To increase statistical power, for each case with pulmonary tuberculosis, we randomly selected four individuals without diagnosis of pulmonary tuberculosis from the same database as the control group that were frequency matched on sex, age (within 5 years) and index year of diagnosing pulmonary tuberculosis. To minimize a biased effect, individuals undergoing appendectomy only within one year of diagnosing pulmonary tuberculosis were excluded from the analysis. Subjects with prior diagnosis of any cancer or HIV/AIDS before the index date were also excluded from the analysis. Potential comorbidities associated with pulmonary tuberculosis
A number of comorbidities before the index date potentially associated with
pulmonary tuberculosis risk were examined. They were appendectomy,
kidney diseases, diabetes mellitus, and chronic liver diseases including cirrhosis,
alcoholic liver damage, hepatitis B, hepatitis C and other types of chronic hepatitis.
All were diagnosed with ICD-9 codes. Statistical Analysis
The differences in sex, age, and comorbidities between the case group and the control group were compared by using the Chi-square test for categorical variables. Initially, all covariables were included in univariable unconditional logistic regression model. Next, only those found significantly associated with risk of pulmonary tuberculosis were further analyzed by multivariable unconditional logistic regression model to measure the odds ratio (OR) and 95% confidence interval (CI) for risk of pulmonary tuberculosis, after simultaneously controlling for covariables. We also measured the joint effect between appendectomy and other comorbidities on risk of pulmonary tuberculosis using the multivariable unconditional logistic regression model. The level of statistical significance was set at a probability value of < 0.05 (SAS software version 9.2, SAS Institute Inc., Cary, North Carolina, USA).
RESULTS
Characteristics of the study population
The case group had 11366 individuals with new diagnosis of pulmonary tuberculosis and the control group had 45464 individuals without pulmonary tuberculosis. Table 1 reveals cases with pulmonary tuberculosis had higher proportions of appendectomy, chronic obstructive pulmonary disease,
pneumoconiosis, chronic kidney diseases, diabetes mellitus and chronic liver diseases, with statistical significance (P < 0.0001 for all). The mean ages (standard deviation) were 58.5 (17.2) years in the case group and 57.7 (17.2) years in the control group
(data not shown in Table 1). The mean period from appendectomy to diagnosing pulmonary tuberculosis was 4.96 years (standard deviation 2.94, range from 1.02 to 14.7, data not shown in Table 1).
Correlation between appendectomy and pulmonary tuberculosis
After simultaneously controlling for covariables, the multivariable unconditional logistic regression model demonstrated that the adjusted OR of pulmonary tuberculosis was 1.4 for appendectomized patients (95% CI= 1.13,
1.75), as compared to individuals without appendectomy. In addition, chronic obstructive pulmonary diseases (OR= 3.6, 95% CI= 3.42, 3.78), pneumoconiosis (OR= 1.82, 95%CI= 1.51, 2.20), chronic kidney diseases (OR= 1.67, 95% CI= 1.50, 1.87), diabetes mellitus (OR= 1.46, 95% CI= 1.38, 1.54) and chronic liver diseases (OR= 1.18, 95%CI= 1.11, 1.25), were significantly related to increased risk of pulmonary tuberculosis (Table 2).
Joint effect between appendectomy and other comorbidities on risk of pulmonary tuberculosis
Table 3 shows the joint effects between appendectomy and other comorbidities on risk of pulmonary tuberculosis. When comparing to individuals without
appendectomy and without any comorbidity, the ORs of pulmonary tuberculosis were 1.76 (95% CI= 1.29, 2.39) for individuals with appendectomy alone and 3.14 (95% CI= 3.00, 3.29) for those with at least one comorbidity but not having appendectomy. The OR increased to 3.76 (95% CI= 2.81, 5.04) for individuals with appendectomy and at least one comorbidity. Co-morbid with chronic obstructive pulmonary diseases (OR = 4.63, 95% CI= 3.21, 6.68), pneumoconiosis (OR = 7.80, 95% CI= 1.43, 42.5), chronic kidney diseases (OR = 5.65, 95% CI= 1.79, 17.8) or diabetes mellitus (OR = 2.11, 95% CI= 1.30, 3.44) raised the risk of pulmonary tuberculosis in individuals with appendectomy. Compared with individuals without appendectomy and without
chronic liver diseases, the OR in individuals with chronic liver diseases alone was 1.51 (95% CI=1.42, 1.59). The OR increased to 1.65 (95% CI=1.32, 2.07) in
individuals with appendectomy alone, and remained at similar strength in individuals with both appendectomy and chronic liver diseases (OR=1.62, 95% CI=0.95, 2.74), but not statistically significant.
DISCUSSION
Although many risk factors for pulmonary tuberculosis have been disclosed in previous studies , to the best of our knowledge, no other study focuses on the relationship between appendectomy and pulmonary tuberculosis till now. In this present study, appendectomized patients were at a 1.4-fold increased risk of
pulmonary tuberculosis, as compared to individuals without appendectomy. From a view of accessibility and quality of the Taiwan National Health Insurance Program, it does not need to spend one year from the onset of prodrome of pulmonary
tuberculosis to confirm a diagnosis. In order to minimize a biased effect, individuals undergoing appendectomy only within one year of diagnosing pulmonary tuberculosis were excluded from this study. Therefore, we can make sure that appendectomy was really undergone before the onset of prodrome of pulmonary tuberculosis. In further analysis, the risk would increase to 3.76-fold for individuals with appendectomy and co-morbid with any of the comorbidities, including chronic obstructive pulmonary disease, pneumoconiosis, chronic kidney diseases, diabetes mellitus and chronic liver diseases. We believe that there are joint effects between appendectomy and other comorbidities on risk of pulmonary tuberculosis. Whether intervention to these comorbidities among appendectomized patients could decrease the risk of pulmonary tuberculosis requires further assessment. Based on these findings, we alerts clinicians should be cautious of the possibility of pulmonary tuberculosis in patients with
appendectomy and co-morbid with other comorbidities.
Despite the role of appendectomy in the pathogenesis of pulmonary tuberculosis
can not be completely elucidated in this observational study, recent studies
showed that the appendix could be associated with immune function . Therefore,
appendectomy may change immune function , which seems to be associated with
some diseases later . This also partially provides a biological plausibility why
appendectomized patients are at higher risk of pulmonary tuberculosis, because
impaired immune function induced by appendectomy may forcefully promote the
occurrence of pulmonary tuberculosis. Moreover, further studies are required to
Funding
This study was supported in part by Taiwan Department of Health Clinical Trial and Research Center of Excellence (Grant number DOH102-TD-B-111-004) and China Medical University Hospital (Grant number 1MS1).The funding agency did not influence the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Specific author contributions:
Shih-Wei Lai: (1) substantial contributions to the conception of this article; (2) planned and conducted the study; (3) initiated the draft of the article and critically revised the article.
Cheng-Li Lin and Sung-Mao Tsai: (1) conducted data analysis; (2) critically revised the article.
Kuan-Fu Liao: (1) planned and conducted the study; (2) participated in data interpretation; (3) critically revised the article.
Conflict of Interest Statement
REFERENCES
[1] Dasso JF, Obiakor H, Bach H, Anderson AO, Mage RG (2000) A morphological and immunohistological study of the human and rabbit appendix for comparison with the avian bursa. Dev Comp Immunol 24 (8):797-814
[2] Matsushita M, Takakuwa H, Matsubayashi Y, Nishio A, Ikehara S, Okazaki K (2005) Appendix is a priming site in the development of ulcerative colitis. World J Gastroenterol 11 (31):4869-4874
[3] Matsushita M, Uchida K, Okazaki K (2007) Role of the appendix in the pathogenesis of ulcerative colitis. Inflammopharmacology 15 (4):154-157
[4] Hallas J, Gaist D, Sorensen HT (2004) Does appendectomy reduce the risk of ulcerative colitis? Epidemiology 15 (2):173-178
[5] de Saussure P, Clerson P, Prost PL, Truong Tan N, Bouhnik Y, Gil R (2007) Appendectomy, smoking habits and the risk of developing ulcerative colitis: a case control study in private practice setting. Gastroenterol Clin Biol 31 (5):493-497 [6] Reshetnikov OV, Kurilovich SA, Denisova DV, Zav'ialova LG, Svetlova IO, Tereshonok IN, Krivenchuk NA, Eremeeva LI (2001) [Prevalence and risk factors of the development of irritable bowel syndrome in adolescents: a population study]. Ter Arkh 73 (2):24-29
[7] Kaplan GG, Jackson T, Sands BE, Frisch M, Andersson RE, Korzenik J (2008) The risk of developing Crohn's disease after an appendectomy: a meta-analysis. Am J Gastroenterol 103 (11):2925-2931
[8] Janszky I, Mukamal KJ, Dalman C, Hammar N, Ahnve S (2011) Childhood appendectomy, tonsillectomy, and risk for premature acute myocardial infarction--a nationwide population-based cohort study. Eur Heart J 32 (18):2290-2296
[9] Clanton J, Subichin M, Drolshagen K, Daley T, Firstenberg MS (2013)
Fulminant Clostridium difficile infection: An association with prior appendectomy? World J Gastrointest Surg 5 (8):233-238
[10] Bazar KA, Lee PY, Joon Yun A (2004) An "eye" in the gut: the appendix as a sentinel sensory organ of the immune intelligence network. Med Hypotheses 63 (4):752-758
[11] Kim J, Langevin M, Wylie EL, McCarthy AE (2008) The epidemiology of tuberculosis in Ottawa, Canada, 1995-2004. Int J Tuberc Lung Dis 12 (10):1128-1133 [12] Carvalho AC, Migliori GB, Cirillo DM (2010) Tuberculosis in Europe: a
problem of drug resistance or much more? Expert Rev Respir Med 4 (2):189-200 [13] van Maaren PJ (2010) Fighting the tuberculosis epidemic in the Western Pacific region: current situation and challenges ahead. Kekkaku 85 (1):9-16
[14] Mor Z, Pinsker G, Cedar N, Lidji M, Grotto I (2012) Adult tuberculosis in Israel and migration: trends and challenges between 1999 and 2010. Int J Tuberc Lung Dis 16 (12):1613-1618
[15] Lai SW, Liao KF, Liao CC, Muo CH, Liu CS, Sung FC (2010) Polypharmacy correlates with increased risk for hip fracture in the elderly: a population-based study. Medicine (Baltimore) 89 (5):295-299
[16] Lai SW, Su LT, Lin CH, Tsai CH, Sung FC, Hsieh DP (2011) Polypharmacy increases the risk of Parkinson's disease in older people in Taiwan: a population-based study. Psychogeriatrics 11 (3):150-156
[17] Lai SW, Chen PC, Liao KF, Muo CH, Lin CC, Sung FC (2012) Risk of
hepatocellular carcinoma in diabetic patients and risk reduction associated with anti-diabetic therapy: a population-based cohort study. Am J Gastroenterol 107 (1):46-52 [18] Liao KF, Lai SW, Li CI, Chen WC (2012) Diabetes mellitus correlates with increased risk of pancreatic cancer: a population-based cohort study in Taiwan. J Gastroenterol Hepatol 27 (4):709-713
[19] Wu HP, Pan YH, Hua CC, Shieh WB, Jiang BY, Yu TJ (2007) Pneumoconiosis and liver cirrhosis are not risk factors for tuberculosis in patients with pulmonary infection. Respirology 12 (3):416-419
[20] Gupta S, Shenoy VP, Mukhopadhyay C, Bairy I, Muralidharan S (2011) Role of risk factors and socio-economic status in pulmonary tuberculosis: a search for the root cause in patients in a tertiary care hospital, South India. Trop Med Int Health 16 (1):74-78
[21] Lee CH, Lee MC, Shu CC, Lim CS, Wang JY, Lee LN, Chao KM (2013) Risk factors for pulmonary tuberculosis in patients with chronic obstructive airway disease in Taiwan: a nationwide cohort study. BMC Infect Dis 13:194
[22] Randal Bollinger R, Barbas AS, Bush EL, Lin SS, Parker W (2007) Biofilms in the large bowel suggest an apparent function of the human vermiform appendix. J Theor Biol 249 (4):826-831
[23] Ansaloni L, Catena F, Pinna AD (2009) What Is the Function of the Human Vermiform Appendix? European Surgical Research 43 (2):67-71
[24] Barlow A, Muhleman M, Gielecki J, Matusz P, Tubbs RS, Loukas M (2013) The vermiform appendix: A review. Clinical Anatomy 26 (7):833-842
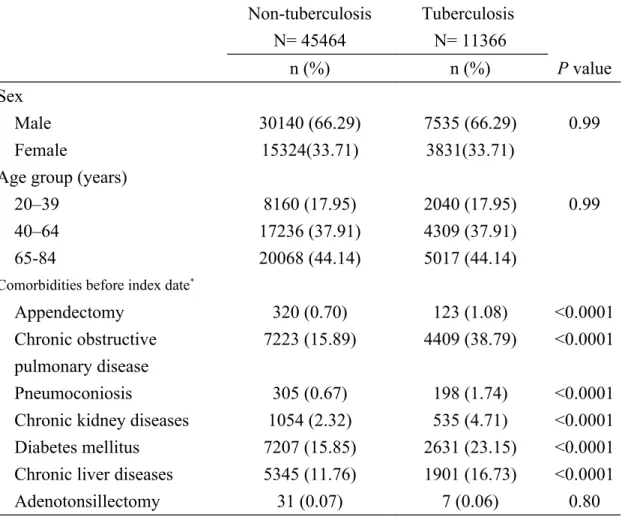
Table 1. Information and comorbidities between pulmonary tuberculosis cases and non-pulmonary tuberculosis individuals
Non-tuberculosis N= 45464 Tuberculosis N= 11366 n (%) n (%) P value Sex Male 30140 (66.29) 7535 (66.29) 0.99 Female 15324(33.71) 3831(33.71)
Age group (years)
20–39 8160 (17.95) 2040 (17.95) 0.99
40–64 17236 (37.91) 4309 (37.91)
65-84 20068 (44.14) 5017 (44.14)
Comorbidities before index date*
Appendectomy 320 (0.70) 123 (1.08) <0.0001
Chronic obstructive pulmonary disease
7223 (15.89) 4409 (38.79) <0.0001
Pneumoconiosis 305 (0.67) 198 (1.74) <0.0001
Chronic kidney diseases 1054 (2.32) 535 (4.71) <0.0001 Diabetes mellitus 7207 (15.85) 2631 (23.15) <0.0001 Chronic liver diseases 5345 (11.76) 1901 (16.73) <0.0001
Adenotonsillectomy 31 (0.07) 7 (0.06) 0.80
Data are presented as the number of individuals in each group, with percentages given in parentheses.
Chi-square test comparing individuals with and without pulmonary tuberculosis
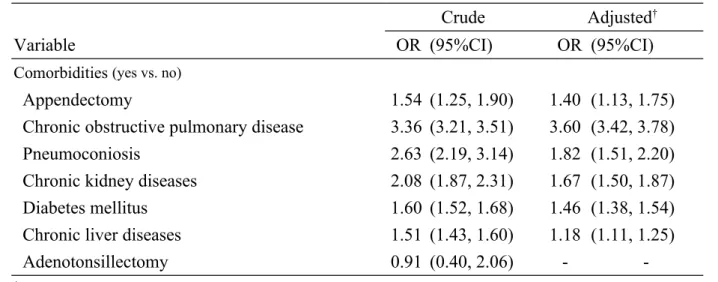
Table 2. Multivariable logistic regression model for odds ratio and 95% confidence interval of pulmonary tuberculosis associated with appendectomy and comorbidities
Crude Adjusted†
Variable OR (95%CI) OR (95%CI)
Comorbidities (yes vs. no)
Appendectomy 1.54 (1.25, 1.90) 1.40 (1.13, 1.75)
Chronic obstructive pulmonary disease 3.36 (3.21, 3.51) 3.60 (3.42, 3.78)
Pneumoconiosis 2.63 (2.19, 3.14) 1.82 (1.51, 2.20)
Chronic kidney diseases 2.08 (1.87, 2.31) 1.67 (1.50, 1.87)
Diabetes mellitus 1.60 (1.52, 1.68) 1.46 (1.38, 1.54)
Chronic liver diseases 1.51 (1.43, 1.60) 1.18 (1.11, 1.25)
Adenotonsillectomy 0.91 (0.40, 2.06) -
-†Covariables which were significantly associated with risk of pulmonary tuberculosis in
univariable unconditional logistic regression model were further analyzed by multivariable unconditional logistic regression model.
Additionally adjusted for age, chronic obstructive pulmonary disease, pneumoconiosis, chronic kidney diseases, diabetes mellitus and chronic liver diseases.
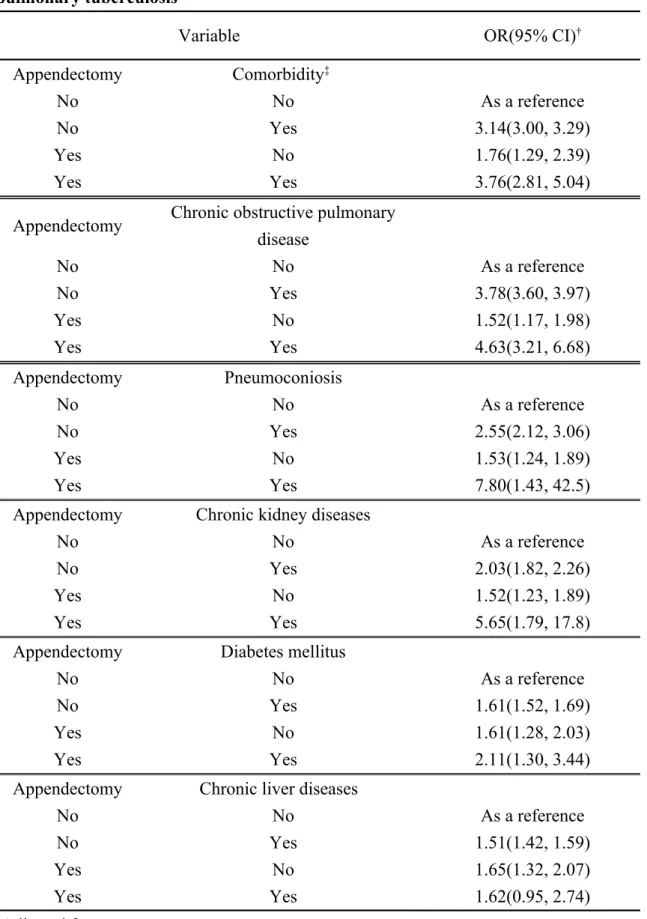
Table 3. Joint effects between appendectomy and comorbidities on risk of pulmonary tuberculosis
Variable OR(95% CI)†
Appendectomy Comorbidity‡
No No As a reference
No Yes 3.14(3.00, 3.29)
Yes No 1.76(1.29, 2.39)
Yes Yes 3.76(2.81, 5.04)
Appendectomy Chronic obstructive pulmonary disease No No As a reference No Yes 3.78(3.60, 3.97) Yes No 1.52(1.17, 1.98) Yes Yes 4.63(3.21, 6.68) Appendectomy Pneumoconiosis No No As a reference No Yes 2.55(2.12, 3.06) Yes No 1.53(1.24, 1.89) Yes Yes 7.80(1.43, 42.5)
Appendectomy Chronic kidney diseases
No No As a reference
No Yes 2.03(1.82, 2.26)
Yes No 1.52(1.23, 1.89)
Yes Yes 5.65(1.79, 17.8)
Appendectomy Diabetes mellitus
No No As a reference
No Yes 1.61(1.52, 1.69)
Yes No 1.61(1.28, 2.03)
Yes Yes 2.11(1.30, 3.44)
Appendectomy Chronic liver diseases
No No As a reference
No Yes 1.51(1.42, 1.59)
Yes No 1.65(1.32, 2.07)
Yes Yes 1.62(0.95, 2.74)
‡Individuals with any of the comorbidities (chronic obstructive pulmonary disease,
pneumoconiosis, chronic kidney diseases, diabetes mellitus and chronic liver diseases) were classified as the comorbidity group.