Lifetime Risk and Sex Difference of Hepatocellular
Carcinoma Among Patients With Chronic
Hepatitis B and C
Yen-Tsung Huang, Chin-Lan Jen, Hwai-I Yang, Mei-Hsuan Lee, Jun Su, Sheng-Nan Lu, Uchenna H. Iloeje, and Chien-Jen Chen
Yen-Tsung Huang, Harvard University, Boston, MA; Jun Su and Uchenna H. Iloeje, Bristol-Myers Squibb, Walling-ford, CT; Chin-Lan Jen, Mei-Hsuan Lee, and Chien-Jen Chen, Academia Sinica; Chien-Jen Chen, National Taiwan University, Taipei; Hwai-I Yang, China Medical University Hospital, Taichung; and Sheng-Nan Lu, Chang Gung Memorial Hospital–Kaohsiung Medical Center, Chang Gung University College of Medicine, Kaohsiung, Taiwan. Submitted April 12, 2011; accepted June 22, 2011; published online ahead of print at www.jco.org on August 22, 2011.
Written on behalf of the Risk Evaluation of Viral Load Elevation and Associated Liver Disease/Cancer–Hepatitis B and C Virus Study Group.
Supported in part by Grant No. AI463059 from Bristol-Myers Squibb (C.-J.C.) and by the Department of Health, Executive Yuan, Taiwan. Y.-T.H. and C.-L.J. contributed equally to this work.
Authors’ disclosures of potential con-flicts of interest and author contribu-tions are found at the end of this article.
Corresponding author: Chien-Jen Chen, ScD, Genomics Research Center, Academia Sinica, 128 Academia Rd, Section 2, Nankang, Taipei 11529, Taiwan; e-mail: cjchen@ntu.edu.tw. © 2011 by American Society of Clinical Oncology
0732-183X/11/2927-3643/$20.00 DOI: 10.1200/JCO.2011.36.2335
A B S T R A C T
Purpose
Both hepatitis B (HBV) and C viruses (HCV) are causes of hepatocellular carcinoma (HCC), but lifetime risk and sex difference remain unclear. This study aimed to assess the lifetime risk and sex difference of HCC among patients with chronic HBV and/or HCV.
Methods
A prospective cohort of 23,820 residents of Taiwan age 30 to 65 years were enrolled from 1991 to 1992, with 477 instances of HCC occurring subsequently. Serum samples collected at enrollment were tested for seromarkers and viral load of HBV and HCV. Newly developed HCC was ascertained through computerized data linkage with national cancer registry and death certification systems.
Results
The cumulative lifetime (age 30 to 75 years) incidences of HCC for men and women positive for both HBV surface antigen (HBsAg) and antibodies against HCV (anti-HCV) were 38.35% and 27.40%; for those positive for HBsAg only, 27.38% and 7.99%; for those positive for anti-HCV only, 23.73% and 16.71%; and for those positive for neither, 1.55% and 1.03%, respectively. There was a significant male predominance in incidence of HCC for chronic HBV carriers but not for chronic carriers of HCV or both. Multivariate adjusted hazard ratio of developing HCC decreased with age in HBsAg-seropositive men but increased with age in anti-HCV–seropositive women. Among dual-infected participants, there was an inverse association between HBV and HCV viral load. Risk of HCC increased significantly with increasing viral load of HBV and HCV.
Conclusion
There exists a suppressive effect of HCV on HBV viral load. Individual and combined effects of the two viruses on HCC vary with sex and age.
J Clin Oncol 29:3643-3650. © 2011 by American Society of Clinical Oncology
INTRODUCTION
There are 350 million and 170 million persons chronically infected with hepatitis B virus (HBV) and hepatitis C virus (HCV) in the world, respec-tively.1Hepatocellular carcinoma (HCC) is the sixth most common cancer worldwide and the third most common cause of death resulting from cancer be-cause of its poor prognosis.2Chronic infections of HBV and HCV are well-documented etiologic fac-tors for HCC. Both viruses have been classified as human carcinogens by the International Agency for Research on Cancer.3
Taiwan is a hyperendemic area of chronic HBV. Before a national HBV vaccination program was implemented in 1984, 15% to 20% of the gen-eral population of Taiwan was chronically infected
with HBV.4 A majority of HBV surface antigen (HBsAg) –seropositive residents of Taiwan were in-fected with HBV perinatally before 3 years of age, whereas infection after 3 years of age rarely resulted in a chronic infection state.5In contrast, the preva-lence of HCV infection varies by region in Taiwan, ranging from 1.6% to 37%.6-8Horizontal routes, especially iatrogenic contact with contaminated sy-ringes or needles, are the major transmission route of HCV in Taiwan.9,10Furthermore, the seropreva-lence of antibodies against HCV (anti-HCV) is less than 1% for children younger than 12 years, and HCV infection mainly occurs in young adulthood.11 Hence, most patients with dual chronic infection of HBV and HCV in Taiwan can be assumed to be chronic HBV carriers superinfected by HCV. It has also been found that patients with HCV-associated
HCC are older than those with HBV-associated HCC,12and HCV leads to liver cirrhosis more often than HBV, which may also indicate different hepatocarcinogenic mechanisms between HBV and HCV.
There have been numerous reports on the combined effect of chronic HBV and HCV infection on HCC risk.13-24Most involved case-series and case-control studies; to our knowledge, we reported the only community-based cohort study in men.23Here we further analyze updated data for both men and women, with the estimation of cumulative lifetime (age 30 to 75 years) incidence of HCC. This community-based prospective cohort study aimed first, to estimate the lifetime risk of HCC for participants with chronic HBV and/or HCV infection by sex; second, to compare HCC risk associated with chronic HBV and/or HCV infection between men and women and between young and old carriers; and third, to assess the association with HCC risk for HBV and/or HCV viral load.
METHODS Study Cohort
The enrollment of study participants has been described previously.25-28
Briefly, we recruited 23,820 residents from seven townships of Taiwan from 1991 to 1992. They provided written informed consent for the questionnaire interview, biospecimen collection, health examinations, and computerized data linkage of health status with national cancer registry and death certifica-tion profiles.
Data Collection and Blood Tests
At cohort entry, all participants were personally interviewed by well-trained research nurses using a structured questionnaire. A 10-mL peripheral blood sample was collected from each participant using a disposable vacuum syringe with needle. Blood samples were fractionated on collection day and stored in deep freezers (at⫺70°C) until use. The serum samples collected at cohort entry were tested for HBsAg by radioimmunoassay using commercial kits (Abbott Laboratories, North Chicago, IL), anti-HCV by enzyme immu-noassay using a second-generation commercial kit (Abbott Laboratories), and ALT by a serum chemistry autoanalyzer (model 736, Hitachi, Tokyo, Japan). For those seropositive for HBsAg and anti-HCV, HBV DNA (copies/mL) and HCV RNA (IU/mL) were further measured by the Cobas Amplicor HBV
monitor test kit and Cobas TaqMan HCV test v2.0 (Roche Diagnostics, Indi-anapolis, IN), respectively.
Ascertainment of HCC
At enrollment, any participant who had an elevated serum level of ALT (ⱖ 45 IU/L), AST (ⱖ 40 IU/L), or␣-fetoprotein (ⱖ 20 ng/mL); serostatus of HBsAg or anti-HCV; or family history of cirrhosis or HCC among first-degree relatives was referred for abdominal ultrasonography and confirmatory diag-nosis. None of the study participants were affected by HCC at enrollment based on health examination at cohort entry, questionnaire interview on personal history of HCC, and data linkage with the national cancer regis-try profile.
Newly developed HCC was ascertained by computerized data linkage of the national cancer registry and national death certification profiles in Taiwan for a period from January 1, 1984, to June 30, 2008. Medical record verification of all diagnoses of HCC was based on the following criteria: histopathologic examination, positive lesion detected by at least two different imaging tech-niques (abdominal ultrasonography, angiogram, or computed tomography), or imaging technique with a serum␣-fetoproteinlevelgreaterthan400ng/mL. Ascertainment of newly developed HCC was considered complete and accu-rate. More detailed information is provided in the Appendix (online only).
Statistical Analysis
For each participant, the period at risk for HCC was calculated from date of enrollment to date of diagnosis of newly developed HCC, date of death, or last date of linked data available from the national cancer registry (June 30, 2008), whichever came first. Analyses using follow-up time as the time scale with stratification of birth year and adjustment of age at enrollment showed similar results with those using age as the time scale. Cumulative lifetime (age 30 to 75 years old) incidence of HCC was estimated for men and women with chronic HBV and/or HCV infection. For further investigation of the age-varying effect of HBV and HCV, age was used as the primary time scale, with stratification of birth year and covariate adjustment of age at enrollment to fully account for the effects of both age and birth cohort throughout the study. The proportional hazards assumption was satisfied for each covariate in the final multivariate adjusted Cox model according to Schoenfeld residuals.
The hazard ratios (HRs) and 95% CIs for the groups seropositive for HBsAg only, anti-HCV only, and both were obtained with Cox proportional hazards models, using participants seronegative for both HBsAg and anti-HCV as the reference group. Multivariate adjusted HRs were derived from the Cox model, with stratification of birth year and sex and adjustment of age at enrollment (40 to 49, 50 to 59, and 60 to 65 years [reference group, 30 to 39
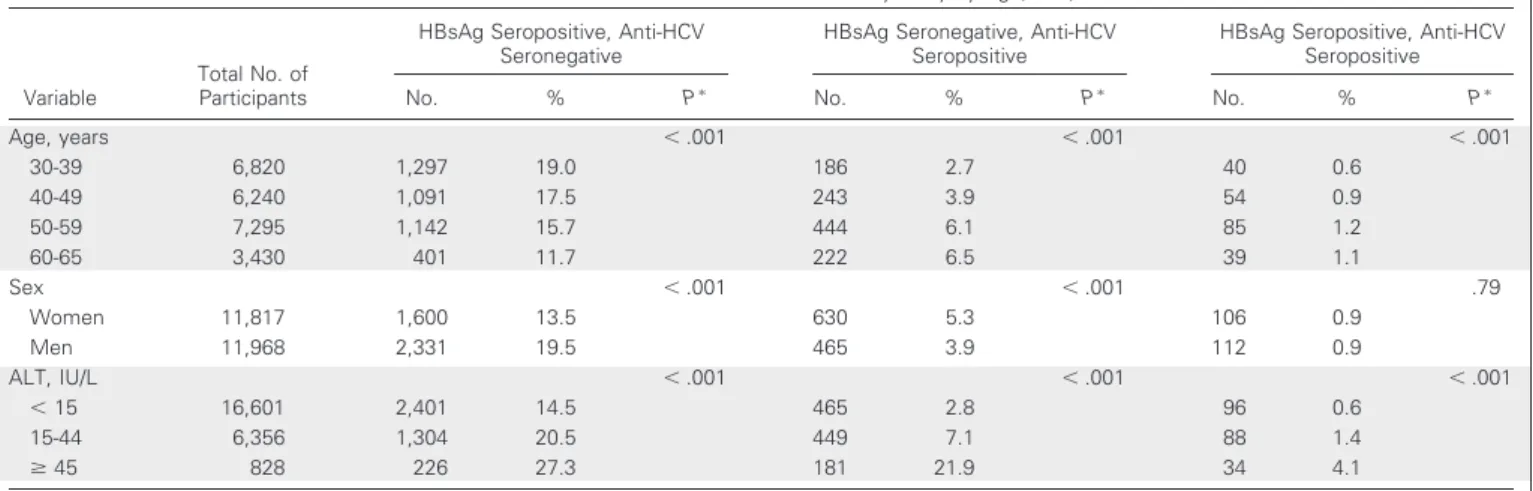
Table 1. Prevalence of HBV and HCV Infection Status at Study Entry by Age, Sex, and ALT Level
Variable
Total No. of Participants
HBsAg Seropositive, Anti-HCV Seronegative
HBsAg Seronegative, Anti-HCV Seropositive
HBsAg Seropositive, Anti-HCV Seropositive
No. % Pⴱ No. % Pⴱ No. % Pⴱ
Age, years ⬍ .001 ⬍ .001 ⬍ .001 30-39 6,820 1,297 19.0 186 2.7 40 0.6 40-49 6,240 1,091 17.5 243 3.9 54 0.9 50-59 7,295 1,142 15.7 444 6.1 85 1.2 60-65 3,430 401 11.7 222 6.5 39 1.1 Sex ⬍ .001 ⬍ .001 .79 Women 11,817 1,600 13.5 630 5.3 106 0.9 Men 11,968 2,331 19.5 465 3.9 112 0.9 ALT, IU/L ⬍ .001 ⬍ .001 ⬍ .001 ⬍ 15 16,601 2,401 14.5 465 2.8 96 0.6 15-44 6,356 1,304 20.5 449 7.1 88 1.4 ⱖ 45 828 226 27.3 181 21.9 34 4.1
Abbreviations: anti-HCV, antibodies against HCV; HBsAg, HBV surface antigen; HBV, hepatitis B virus; HCV, hepatitis C virus.
ⴱP values calculated by Cochran-Armitage trend test for age at enrollment (30-39, 40-49, 50-59, and 60-65 years) and ALT level (⬍ 15, 15-44, and ⱖ 45 IU/L) and by Fisher exact test for sex.
years]), cigarette smoking (yes or no), alcohol consumption (yes or no), and serum ALT level (ⱖ 45 and 15 to 44 IU/L [reference group, ⬍ 15 IU/L]). Multivariate adjusted cumulative incidences of HCC at age 75 years were estimated from the Cox model. To investigate the dose-response relationship of HBV and HCV viral load and HCC risk, the penalized spline was imple-mented in the Cox model. Age-varying effects (⬎ 65 and ⱕ 65 years) of the four HBV and/or HCV carrier groups on HCC were estimated by time-varying Cox model.
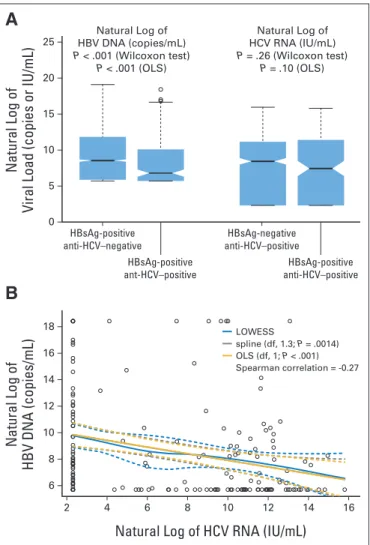
The viral load of HBV and HCV in participants with mono- and dual infection was compared by Wilcoxon rank sum test and multiple linear regression analysis (ordinary least squares). HBV and HCV viral loads were natural log transformed because of their skewness. Among participants with dual infection, the association between HBV and HCV viral load was further investigated by Spearman correlation, locally weighted scatterplot smoothing, and multivariate linear model regressing natural log of HBV viral load on spline or linear term of natural log of HCV viral load with multivariate adjustment.
RESULTS
TheseroprevalenceofHBsAgandanti-HCVamongstudyparticipantsby age at enrollment, sex, and serum ALT level is shown in Table 1. There were 4,149 (17.44%) and 1,313 participants (5.52%) seropositive for HBsAg and anti-HCV, respectively. The seroprevalence of HBsAg de-creased with age (P⬍.001fortrend),whereasthatofanti-HCVinde-creased with age (P⬍.001fortrend).MenhadahigherseroprevalenceofHBsAg than women (P⬍ .001), and women had a higher seroprevalence of anti-HCV than men (P⬍ .001). Serum ALT levels were associated with chronic HBV and/or HCV (P⬍ .001 for trend).
Seromarkers of HBV and HCV
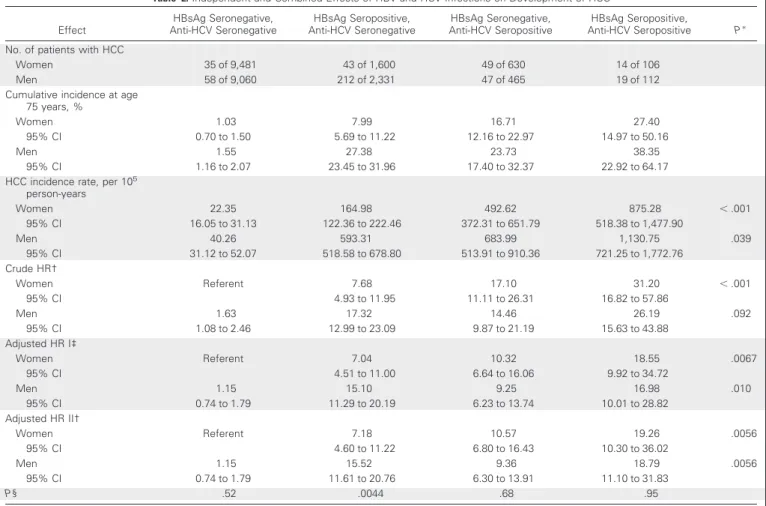
As listed in Table 2, the cumulative lifetime (age 30 to 75 years) incidences of HCC for men and women positive for both HBsAg and
Table 2. Independent and Combined Effects of HBV and HCV Infections on Development of HCC Effect HBsAg Seronegative, Anti-HCV Seronegative HBsAg Seropositive, Anti-HCV Seronegative HBsAg Seronegative, Anti-HCV Seropositive HBsAg Seropositive, Anti-HCV Seropositive Pⴱ No. of patients with HCC
Women 35 of 9,481 43 of 1,600 49 of 630 14 of 106
Men 58 of 9,060 212 of 2,331 47 of 465 19 of 112
Cumulative incidence at age 75 years, %
Women 1.03 7.99 16.71 27.40
95% CI 0.70 to 1.50 5.69 to 11.22 12.16 to 22.97 14.97 to 50.16
Men 1.55 27.38 23.73 38.35
95% CI 1.16 to 2.07 23.45 to 31.96 17.40 to 32.37 22.92 to 64.17
HCC incidence rate, per 105 person-years Women 22.35 164.98 492.62 875.28 ⬍ .001 95% CI 16.05 to 31.13 122.36 to 222.46 372.31 to 651.79 518.38 to 1,477.90 Men 40.26 593.31 683.99 1,130.75 .039 95% CI 31.12 to 52.07 518.58 to 678.80 513.91 to 910.36 721.25 to 1,772.76 Crude HR† Women Referent 7.68 17.10 31.20 ⬍ .001 95% CI 4.93 to 11.95 11.11 to 26.31 16.82 to 57.86 Men 1.63 17.32 14.46 26.19 .092 95% CI 1.08 to 2.46 12.99 to 23.09 9.87 to 21.19 15.63 to 43.88 Adjusted HR I‡ Women Referent 7.04 10.32 18.55 .0067 95% CI 4.51 to 11.00 6.64 to 16.06 9.92 to 34.72 Men 1.15 15.10 9.25 16.98 .010 95% CI 0.74 to 1.79 11.29 to 20.19 6.23 to 13.74 10.01 to 28.82 Adjusted HR II† Women Referent 7.18 10.57 19.26 .0056 95% CI 4.60 to 11.22 6.80 to 16.43 10.30 to 36.02 Men 1.15 15.52 9.36 18.79 .0056 95% CI 0.74 to 1.79 11.61 to 20.76 6.30 to 13.91 11.10 to 31.83 P§ .52 .0044 .68 .95
Abbreviations: anti-HCV, antibodies against HCV; HBsAg, HBV surface antigen; HBV, hepatitis B virus; HCC, hepatocellular carcinoma; HCV, hepatitis C virus; HR, hazard ratio. ⴱP values were obtained with tests for homogeneity of effects among those with HBsAg-seropositive and anti-HCV–seronegative, HBsAg-seronegative and anti-HCV–seropositive, and HBsAg-seropositive and anti-HCV–seropositive statuses in crude incidence rates of HCC, crude HRs, and HRs adjusted for age at enrollment, cigarette smoking status, alcohol consumption, and ALT and stratified by birth year and sex.
†Cox model with age as time scale (in crude and adjusted HR II), adjusted for age at enrollment (40-49, 50-59, and 60-65 years, with those age 30-39 years as reference group), cigarette smoking (yes v no), alcohol drinking (yes v no), and ALT level (15-44 andⱖ 45 IU/L, with those with ALT ⬍ 15 IU/L as reference group) and stratified by birth year (adjusted HR II).
‡Stratified Cox model with follow-up time as time scale, adjusted for age at enrollment (40-49, 50-59, and 60-65 years, with those age 30-39 years as reference group), cigarette smoking (yes v no), alcohol drinking (yes v no), and ALT level (15-44 andⱖ 45 IU/L, with those with ALT ⬍ 15 IU/L as reference group) and stratified by birth year and sex.
§P values were obtained with tests for difference of HRs between men and women in multivariate adjusted Cox model with age as time scale, stratification of birth year, and adjustment of covariates as mentioned.
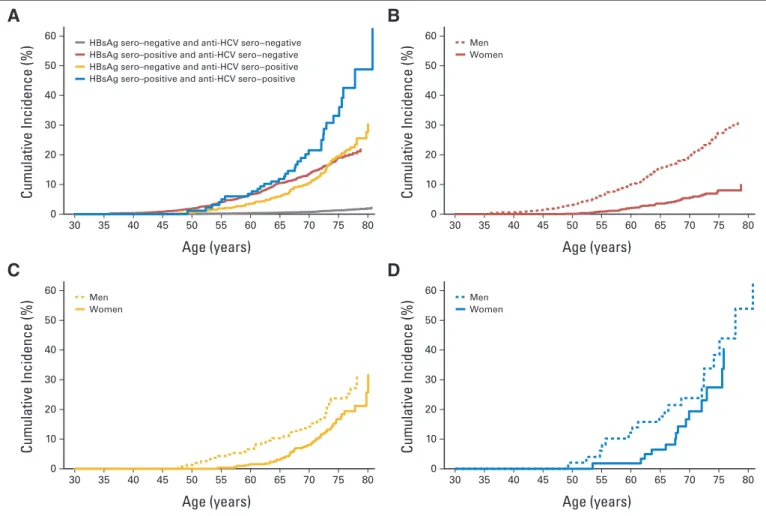
anti-HCV were 38.35% and 27.40%; for those positive for HBsAg only, 27.38% and 7.99%; for those positive for anti-HCV only, 23.73% and 16.71%; and for those positive for neither, 1.55% and 1.03%, respectively. The corresponding HCC incidence rates per 100,000 person-years were 1130.75, 593.31, 683.99, and 40.26, respectively, in men and 875.28, 164.98, 492.62, and 22.35, respectively, in women. In the Cox model, multivariate adjusted HRs (95% confidence interval) of developing hepatocellular carcinoma were 19.5 (95% CI, 12.9 to 29.4), 12.9 (95% CI, 10.2 to 16.5), 10.3 (95% CI, 7.6 to 13.9), and 1.0 (reference group), respectively, after adjustment for age, sex, habits of cigarette smoking and alcohol drinking, and serum ALT levels. With adequate adjustment, results with age or follow-up time as the time scale were similar, as shown in Table 2. The HR of cigarette smoking (yes v no) was 1.20 (95% CI, 0.96 to 1.51; P⫽ .12), and that of alcohol consumption (yes v no) was 1.45 (95% CI, 1.13 to 1.86; P⫽ .0035). As shown in Table 2 and Figure 1, HCC risk was significantly higher in those with dual infection of HBV and HCV than in those with monoinfection (P ⫽ .030 and .0019, respectively), especially in women (P⫽ .0016 and .049, respectively). However, the interactive effect on HCC of HBV and HCV was significant away from the multiplicative interaction (P ⬍ .001). There was a significant
male predominance in incidence of HCC for chronic HBV carriers (P⫽ .0044), but no sex difference in HCC risk was found for chronic carriers of HCV, both HBV and HCV, or neither, as shown in Table 2 and Figure 1.
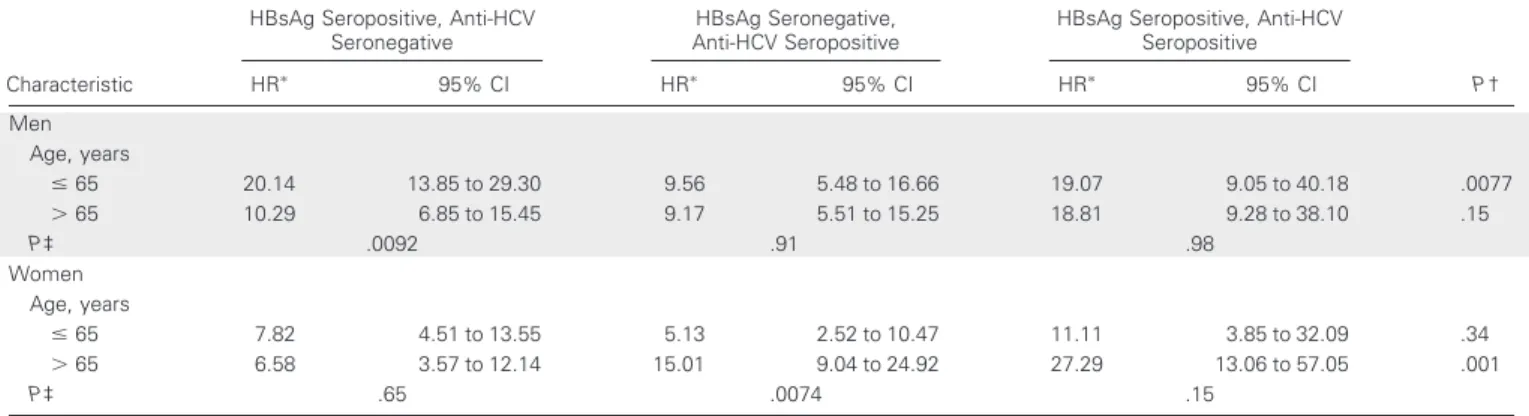
The HR of developing HCC associated with serostatus of HBsAg and/or anti-HCV also varied with age, as shown in Table 3 and Figure 1. The multivariate adjusted HR of developing HCC significantly decreased with age in HBsAg-seropositive men (from 20.14 to 10.29; P⫽ .0092) and significantly increased with age in anti-HCV–seropositive women (from 5.13 to 15.01; P⫽ .0074). Because the age-specific HCC HR was derived by comparing non-carriers with those in the reference group of the same age, whose HCC risk also increased with age, the HBV-associated HCC HR might thus be lower.
Before age 65 years, the HRs for dual infection are subadditive of those for single infection, especially in men. After age 65 years, the HR for dual infection was consistently higher than that for single infection of HBV and HCV in all participants (22.38 v 8.94 and 12.34; P⬍ .001 and⫽ .023, respectively), men (18.81 v 10.29 and 9.17; P ⫽ .084 and .059, respectively), and women (27.29 v 6.58 and 15.01; P⬍ .001 and⫽ .096, respectively). However, the interactive effects on HCC of
B
A
HBsAg sero–negative and anti-HCV sero−negative HBsAg sero–positive and anti-HCV sero−negative HBsAg sero–negative and anti-HCV sero−positive HBsAg sero–positive and anti-HCV sero−positive
Cumulative Incidence (%) Age (years) 60 50 40 20 30 10 0 35 30 40 45 50 55 60 65 70 75 80 Men Women Cumulative Incidence (%) Age (years) 60 50 40 20 30 10 0 35 30 40 45 50 55 60 65 70 75 80
D
C
Men Women Cumulative Incidence (%) Age (years) 60 50 40 20 30 10 0 35 30 40 45 50 55 60 65 70 75 80 Men Women Cumulative Incidence (%) Age (years) 60 50 40 20 30 10 0 35 30 40 45 50 55 60 65 70 75 80Fig 1. Multivariate adjusted cumulative incidence of hepatocellular carcinoma by serostatus of hepatitis B virus surface antigen (HBsAg) and antibodies against hepatitis C virus (anti-HCV). Cumulative incidence was estimated from multivariate adjusted Cox model with age as time scale, stratified by birth year and sex and adjusted for age at enrollment, cigarette smoking, alcohol consumption, and serum ALT level. (A) All patients (N ⫽ 23,785); (B) HBsAg-seropositive and anti-HCV–seronegative patients (n⫽ 3,931); (C) HBsAg-seronegative and anti-HCV–seropositive patients (n ⫽ 1,095); (D) HBsAg- and anti-HCV–seropositive patients (n⫽ 218).
HBV and HCV were still significantly different from the multiplica-tive interaction.
Viral Loads of HBV and HCV
As shown in Figure 2A, serum HBV DNA levels were significantly lower in those with dual infection than in those with HBV monoin-fection (geometric mean⫾ standard deviation: 5,258.1 ⫾ 48.5 v 16,737.7⫾ 62.9 copies/mL; P ⬍ .001), especially in men (4,684.3 ⫾ 45.8 v 20,422.4⫾ 64.1 copies/mL; P ⬍ .001). Furthermore, there was a significant inverse association between serum HBV DNA and HCV RNA levels (Spearman correlation⫽ ⫺0.27; P ⬍ .001) among partic-ipants with dual infection (Fig 2B), which was also more significant in men (Spearman correlation⫽ ⫺0.28; P ⬍ .001).
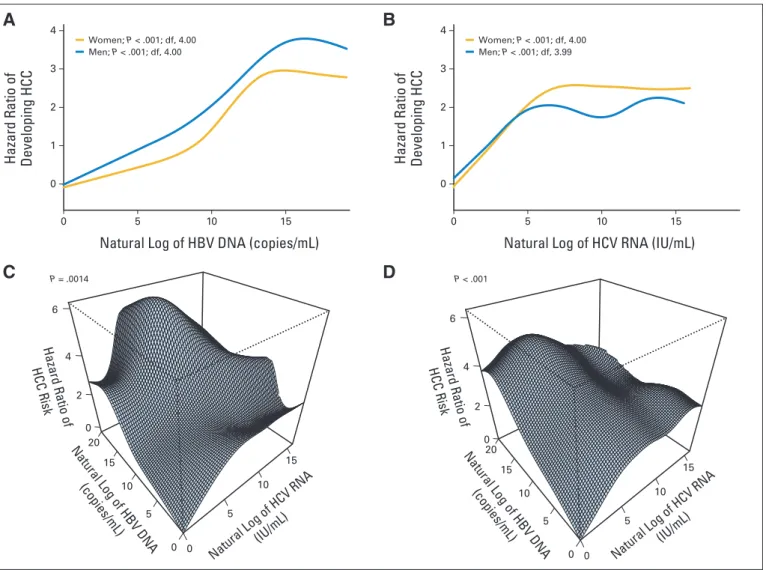
Both HBV and HCV viral loads (in natural log scale) were asso-ciated with increasing HCC HR (in natural log scale) and then reached a plateau (Figs 3A, 3B). In women, superimposed infection by HCV with moderate viral load increased HCC risk more dramatically (Fig 3C). In men, HCC risk of HBV carriers superimposed by HCV infec-tion increased along with the increase of HCV viral load, reached a plateau when HBV viral load was low to moderate, and then started to decline when HBV viral load was high (Fig 3D). The convexity of dose-response surfaces in men indicated strong submultiplicative in-teraction (P⬍.001).Theapexofthesurface(highestriskofHCC)was located in the combination of high HBV viral load and moderate to low HCV viral load.
DISCUSSION
The decreasing seroprevalence of HBsAg with age observed in this study is consistent with previous findings in Taiwan.29,30It may be the result of the following: first, patients seropositive for HBsAg had an increased mortality compared with those who were seronegative; sec-ond, spontaneous negative seroconversion of HBsAg accumulated with age; and third, older birth cohorts had a lower infection rate at birth or in early childhood than younger cohorts.31The decrease in HBsAg seroprevalence with increasing age also suggests that almost all
chronic HBV carriers in this study were infected in infancy or early childhood. The increasing seroprevalence of anti-HCV with age found in this study is also similar to previous findings in Taiwan.9,32This may be attributable to the increased cumulative risk of HCV infection with age and the long-term seropositivity of anti-HCV after infection.
In this study, we first documented the cumulative lifetime (age 30 to 75 years) risk of developing HCC for men and women chronically infected with HBV and/or HCV. Lifetime risk estimates are important for the delineation of the natural history of chronic HBV and HCV and for the evaluation of the cost effectiveness of antiviral treatments for both diseases. By the age of 75 years, one quarter of patients or more affected by chronic viral hepatitis will be affected by HCC. Thus, it is essential to treat chronic HBV and HCV and monitor HCC development regularly. For the age group of 65 years or older, men and women with dual infection had a significantly higher HCC risk than those with single infection. More intensive clinical management of patients with dual infection of HBV and HCV is recommended.
In this study, the interactive effect of HBV and HCV on HCC ranged from sub- to superadditive but was much smaller than that with multiplicative interaction. Many studies have aimed to assess the combined effect of chronic HBV and HCV infections on development of HCC.13-24Statistically, the interactive effect (ie, relative risks for HBV single infection, HCV single infection, and dual infection) has varied from above multiplicative (24.6, 4.0, and infinity, respec-tively)20to superadditive (20.4, 23.6, and 135.0, respectively,21and 15.6, 8.1, and 35.7, respectively24), additive (14.0, 27.1, and 40.1, re-spectively),17and subadditive (53.4, 32.3, and 46.2, respectively,22and 38.5, 21.5, and 30.4, respectively23). The discrepancy among studies may have resulted from the following reasons: first, the number of controls with dual infection was too small to derive an accurate esti-mation of the interactive effect in previous studies, which might have led to a wide range of estimates for interactive effect; second, most previous studies were based on cross-sectional observations, in which reverse causation might be of concern (eg, nosocomial infection of HCV33may occur in patients with severe chronic HBV because of complicated liver disease and long hospitalization); and third, there Table 3. Independent and Combined Age-Varying Effects (ageⱕ 65 and ⬎ 65 years) of HBV and HCV Infections on Development of HCC
Characteristic
HBsAg Seropositive, Anti-HCV Seronegative
HBsAg Seronegative, Anti-HCV Seropositive
HBsAg Seropositive, Anti-HCV Seropositive P† HRⴱ 95% CI HRⴱ 95% CI HRⴱ 95% CI Men Age, years ⱕ 65 20.14 13.85 to 29.30 9.56 5.48 to 16.66 19.07 9.05 to 40.18 .0077 ⬎ 65 10.29 6.85 to 15.45 9.17 5.51 to 15.25 18.81 9.28 to 38.10 .15 P‡ .0092 .91 .98 Women Age, years ⱕ 65 7.82 4.51 to 13.55 5.13 2.52 to 10.47 11.11 3.85 to 32.09 .34 ⬎ 65 6.58 3.57 to 12.14 15.01 9.04 to 24.92 27.29 13.06 to 57.05 .001 P‡ .65 .0074 .15
Abbreviations: anti-HCV, antibodies against HCV; HBsAg, HBV surface antigen; HBV, hepatitis B virus; HCC, hepatocellular carcinoma; HCV, hepatitis C virus. ⴱMultivariate adjusted HRs; stratified Cox model with age as time scale, stratified by birth year and adjusted for age at enrollment (40-49, 50-59, and 60-65 years, with those age 30-39 years as reference group), sex, cigarette smoking (yes v no), alcohol consumption (yes v no), ALT level (15-44 andⱖ 45 IU/L, with those with ALT⬍ 15 IU/L as reference group), effects of which were assumed constant across different ages and sexes, with noncarriers (men and women) as reference group.
†P values were calculated to test difference of effect estimates across three virus-carrying statuses among patients ageⱕ 65 or ⬎ 65 years. ‡P values were calculated to test difference between effect estimates of ageⱕ 65 and ⬎ 65 years.
were different distributions of age, sex, ethnicity, and prevalence of chronic HBV and HCV infections in different studies.
The finding that dual infection was associated with a subadditive combined effect before age 65 years (Table 3) and later onset of HCC than single infection of HBV (Fig 1) may indicate an antagonistic effect between HBV and HCV on the development of HCC at the beginning of superimposed HCV infection. The antagonism between HCV and HBV is also consistent with the inverse association between HBV and HCV viral loads (Figs 2A, 2B) and compatible with that the submultiplicative interactive effect of viral load on HCC. Thus, we conclude that HCC risk with dual infection is higher than that with single infection, but the magnitude is submultiplicative or even sub-additive in men and in the younger population.
The suppression of HBV replication by HCV was first described in chimpanzee studies34and case-series studies.35,36The suppression of expression and replication of HBV by the core protein of HCV have also been reported in in vitro and in vivo studies.37,38In humans, it was reported that seroclearance of HBsAg was higher in patients with dual infection than in those with HBV infection alone.35The higher HCC
risk with dual infection may result from the chronic necroinflamma-tion of the liver through repeated attacks of the host immune system against both HBV and HCV.31,39Thus, the malignant transformation of hepatocytes occurs as a result of continuous cell death and reactive proliferation. In addition to the common mechanism, HBV DNA can integrate into human genome and may initiate hepatocarcinogen-esis,31which enables HBV to transform hepatocytes even in the ab-sence of chronic inflammation. It may also be reflected by our finding that HBV-associated HCC involves earlier onset.
Our analyses revealed that the risk of HBV-associated HCC was higher in men than in women, and the risk of HCV-associated HCC tended to increase when women became postmenopausal. Both find-ings imply the role of sex hormones in the virus-associated hepatocar-cinogenesis. It has been reported that elevated serum testosterone is associated with development of HCC,40and hepatic androgen receptor increases HBV-induced hepatocarcinogenesis in mice.41In women, the ratio of estradiol to testosterone has been shown to be significantly lower in patients with HCC.42The role of sex hormone imbalance in hepatocarcinogenesis may also explain the later onset of HCC in women, mostly after menopause. However, it remains unclear what role sex hormones play in the different patterns of HBV and HCV interactive effects on HCC.
This study has the advantages of a prospective community-based design, large sample size, and long-term follow-up. It has the limita-tion of unknown age at viral infeclimita-tion, especially for HCV. However, we may assume that chronic HBV infection occurred before the age of 3 years, and chronic HCV infection occurred mainly in late childhood and early adulthood.5,11Another limitation is competing cause of death in the analysis of age-dependent HCC risk. We may not exclude the possi-bilitythatthedecreaseinHCCriskresultsfromthehighmortalityofother diseases. In the analysis of liver-related disease mortality and overall mor-tality, women with chronic HCV infection seemed to have higher mortality resulting from liver-related diseases than men. But the dose-response relationships with viral load were similar in HCC incidence, HCC mortality, and liver-related disease mortality.
In conclusion, there is an inverse association between HBV and HCV viral load, and the effect of dual infection on HCC is higher than that of monoinfection, although in a submultiplicative pattern. Risk of HBV-associated HCC decreases with age in men, and HCV-associated HCC risk increases with age in women. More intensive clinical man-agement is recommended for patients with dual HBV and HCV infec-tion, especially for men of all ages and menopausal women.
AUTHORS’ DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Although all authors completed the disclosure declaration, the following author(s) indicated a financial or other interest that is relevant to the subject matter under consideration in this article. Certain relationships marked with a “U” are those for which no compensation was received; those relationships marked with a “C” were compensated. For a detailed description of the disclosure categories, or for more information about ASCO’s conflict of interest policy, please refer to the Author Disclosure Declaration and the Disclosures of Potential Conflicts of Interest section in Information for Contributors.
Employment or Leadership Position: Jun Su, Bristol-Myers Squibb (C);
Uchenna H. Iloeje, Bristol-Myers Squibb (C) Consultant or Advisory
Role: None Stock Ownership: Jun Su, Bristol-Myers Squibb; Uchenna
H. Iloeje, Bristol-Myers Squibb Honoraria: None Research Funding:
Natural Log of
Viral Load (copies or IU/mL)
25 20 15 10 5 0 HBsAg-positive anti-HCV–negative HBsAg-positive ant-HCV–positive HBsAg-negative anti-HCV–positive HBsAg-positive anti-HCV–positive Natural Log of HBV DNA (copies/mL) 18 16 14 10 6 12 8 2 4 6 8 10 12 14 16
Natural Log of HCV RNA (IU/mL)
A
B
LOWESS spline (df, 1.3; P = .0014) OLS (df, 1; P < .001) Spearman correlation = -0.27 Natural Log of HBV DNA (copies/mL) P < .001 (Wilcoxon test) P < .001 (OLS) Natural Log of HCV RNA (IU/mL) P = .26 (Wilcoxon test) P = .10 (OLS)Fig 2. Association between hepatitis B virus (HBV) and hepatitis C virus (HCV) viral load. (A) Viral load compared between groups with mono- and dual infection (both men and women); (B) additional investigation of association between two viral loads. Anti-HCV, antibodies against HCV; df, degree of freedom; HBsAg, serostatus of HBV surface antigen; LOWESS, locally weighted scatterplot smoothing; OLS, ordinary least squares.
Chien-Jen Chen, Bristol-Myers Squibb Expert Testimony: None Other
Remuneration: None
AUTHOR CONTRIBUTIONS
Conception and design: Yen-Tsung Huang, Chin-Lan Jen, Hwai-I Yang,
Jun Su, Sheng-Nan Lu, Uchenna H. Iloeje, Chien-Jen Chen
Financial support: Hwai-I Yang, Jun Su, Chien-Jen Chen Administrative support: Hwai-I Yang, Chien-Jen Chen
Provision of study materials or patients: Chin-Lan Jen, Hwai-I Yang,
Chien-Jen Chen
Collection and assembly of data: Chin-Lan Jen, Hwai-I Yang,
Mei-Hsuan Lee, Chien-Jen Chen
Data analysis and interpretation: Yen-Tsung Huang,
Chin-Lan Jen, Hwai-I Yang, Sheng-Nan Lu, Uchenna H. Iloeje, Chien-Jen Chen
Manuscript writing: All authors Final approval of manuscript: All authors
REFERENCES
1. Lauer GM, Walker BD: Hepatitis C virus infec-tion. N Engl J Med 345:41-52, 2001
2. Parkin DM, Bray F, Ferlay J, et al: Global cancer statistics, 2002. CA Cancer J Clin 55:74-108, 2005
3. Hepatitis viruses. IARC Monogr Eval Carcinog Risks Hum 59:1-255, 1994
4. Chen CJ, Wang LY, Yu MW: Epidemiology of hepatitis B virus infection in the Asia-Pacific region. J Gastroenterol Hepatol 15:E3-E6, 2000 (suppl)
5. Hsu HY, Chang MH, Chen DS, et al: Baseline seroepidemiology of hepatitis B virus infection in
children in Taipei, 1984: A study just before mass hepatitis B vaccination program in Taiwan. J Med Virol 18:301-307, 1986
6. Wu JS, Lu CF, Chou WH, et al: High prevalence of hepatitis C virus infection in aborigines in Taiwan. Jpn J Med Sci Biol 45:165-174, 1992
7. Lu SN, Chue PY, Chen IL, et al: Incidence of hepatitis C infection in a hepatitis C endemic town-ship in southern Taiwan. Kaohsiung J Med Sci 13:605-608, 1997
8. Sun CA, Chen HC, Lu CF, et al: Transmission of hepatitis C virus in Taiwan: Prevalence and risk factors based on a nationwide survey. J Med Virol 59:290-296, 1999
9. Lee SD, Chan CY, Wang YJ, et al: Seroepide-miology of hepatitis C virus infection in Taiwan. Hepatology 13:830-833, 1991
10. Sun CA, Chen HC, Lu SN, et al: Persistent hyperendemicity of hepatitis C virus infection in Taiwan: The important role of iatrogenic risk factors. J Med Virol 65:30-34, 2001
11. Lu SN, Chen HC, Tang CM, et al: Prevalence and manifestations of hepatitis C seropositivity in children in an endemic area. Pediatr Infect Dis J 17:142-145, 1998
12. Lee SD, Lee FY, Wu JC, et al: The prevalence of anti-hepatitis C virus among Chinese patients with hepatocellular carcinoma. Cancer 69:342-345, 1992
B
A
D
C
Women; P < .001; df, 4.00 Men; P < .001; df, 4.00Hazard Ratio of Developing HCC
Natural Log of HBV DNA (copies/mL)
4 3 2 1 0 5 0 10 15 Women; P < .001; df, 4.00 Men; P < .001; df, 3.99
Hazard Ratio of Developing HCC
Natural Log of HCV RNA (IU/mL)
4 3 2 1 0 5 0 10 15
Natural Log of HCV RNA (IU/mL)
0 5
10 15
Natural Log of HBV DNA (copies/mL) 0 5 10 15 20 Hazard Ratio of HCC Risk Hazard Ratio of HCC Risk 0 2 4 6
Natural Log of HCV RNA (IU/mL)
0 5
10 15
Natural Log of HBV DNA (copies/mL) 0 5 10 15 20 0 2 4 6 P < .001 P = .0014
Fig 3. Independent and combined effects of hepatitis B virus (HBV) and hepatitis C virus (HCV) viral load on hepatocellular carcinoma (HCC). Dose-response relationship of HBV and/or HCV viral load against risk of HCC were estimated for (A, B) marginal and (C, D) combined effects using penalized spline in Cox model. df, degree of freedom.
13. Tzonou A, Trichopoulos D, Kaklamani E, et al: Epidemiologic assessment of interactions of hepatitis-C virus with seromarkers of hepatitis-B and -D viruses, cirrhosis and tobacco smoking in hepatocellular carci-noma. Int J Cancer 49:377-380, 1991
14. Kaklamani E, Trichopoulos D, Tzonou A, et al: Hepatitis B and C viruses and their interaction in the origin of hepatocellular carcinoma. JAMA 265:1974-1976, 1991
15. Simonetti RG, Camma C, Fiorello F, et al: Hepatitis C virus infection as a risk factor for hepa-tocellular carcinoma in patients with cirrhosis: A case-control study. Ann Intern Med 116:97-102, 1992
16. Chuang WL, Chang WY, Lu SN, et al: The role of hepatitis B and C viruses in hepatocellular carci-noma in a hepatitis B endemic area: A case-control study. Cancer 69:2052-2054, 1992
17. Chuang WL, Chang WY, Lu SN, et al: The role of hepatitis C virus in chronic hepatitis B virus infection. Gastroenterol Jpn 28:23-27, 1993 (suppl 5)
18. Tsai JF, Chang WY, Jeng JE, et al: Effects of hepatitis C and B viruses infection on the develop-ment of hepatocellular carcinoma. J Med Virol 44: 92-95, 1994
19. Chang CC, Yu MW, Lu CF, et al: A nested case-control study on association between hepatitis C virus antibodies and primary liver cancer in a cohort of 9,775 men in Taiwan. J Med Virol 43:276-280, 1994
20. Sun CA, Farzadegan H, You SL, et al: Mutual confounding and interactive effects between hepa-titis C and hepahepa-titis B viral infections in hepatocellu-lar carcinogenesis: A population-based case-control study in Taiwan. Cancer Epidemiol Biomarkers Prev 5:173-178, 1996
21. Donato F, Boffetta P, Puoti M: A meta-analysis of epidemiological studies on the combined effect of hepatitis B and C virus infections in causing hepatocellular carcinoma. Int J Cancer 75:347-354, 1998
22. Kuper HE, Tzonou A, Kaklamani E, et al: Hepatitis B and C viruses in the etiology of hepa-tocellular carcinoma: A study in Greece using third-generation assays. Cancer Causes Control 11:171-175, 2000
23. Sun CA, Wu DM, Lin CC, et al: Incidence and cofactors of hepatitis C virus-related hepatocellular carcinoma: A prospective study of 12,008 men in Taiwan. Am J Epidemiol 157:674-682, 2003
24. Shi J, Zhu L, Liu S, et al: A meta-analysis of case-control studies on the combined effect of hepatitis B and C virus infections in causing hepato-cellular carcinoma in China. Br J Cancer 92:607-612, 2005
25. Chen CJ, Yang HI, Su J, et al: Risk of hepato-cellular carcinoma across a biological gradient of serum hepatitis B virus DNA level. JAMA 295:65-73, 2006
26. Chen CL, Yang HI, Yang WS, et al: Metabolic factors and risk of hepatocellular carcinoma by chronic hepatitis B/C infection: A follow-up study in Taiwan. Gastroenterology 135:111-121, 2008
27. Iloeje UH, Yang HI, Jen CL, et al: Risk and predictors of mortality associated with chronic hep-atitis B infection. Clin Gastroenterol Hepatol 5:921-931, 2007
28. Lee MH, Yang HI, Lu SN, et al: Hepatitis C virus seromarkers and subsequent risk of hepato-cellular carcinoma: Long-term predictors from a community-based cohort study. J Clin Oncol 28: 4587-4593, 2010
29. Chung DC, Ko YC, Chen CJ, et al: Seroepide-miological studies on hepatitis B and D viruses infection among five ethnic groups in southern Tai-wan. J Med Virol 26:411-418, 1988
30. Chang MH, Hsu HY, Hsu HC, et al: The significance of spontaneous hepatitis B e antigen seroconversion in childhood: With special emphasis on the clearance of hepatitis B e antigen before 3 years of age. Hepatology 22:1387-1392, 1995
31. You SL, Yang HI, Chen CJ: Seropositivity of hepatitis B e antigen and hepatocellular carcinoma. Ann Med 36:215-224, 2004
32. Sheu JC, Wang JT, Wang TH, et al: Preva-lence of hepatitis C viral infection in a community in Taiwan: Detection by synthetic peptide-based assay and polymerase chain reaction. J Hepatol 17:192-198, 1993
33. Forns X, Martı´nez-Bauer E, Feliu A, et al: Nosocomial transmission of HCV in the liver unit of a tertiary care center. Hepatology 41:115-122, 2005 34. Tsiquaye KN, Portmann B, Tovey G, et al: Non-A, non-B hepatitis in persistent carriers of hep-atitis B virus. J Med Virol 11:179-189, 1983
35. Liaw YF: Role of hepatitis C virus in dual and triple hepatitis virus infection. Hepatology 22:1101-1108, 1995
36. Koike K, Yasuda K, Yotsuyanagi H, et al: Dominant replication of either virus in dual infection with hepatitis viruses B and C. J Med Virol 45:236-239, 1995
37. Shih CM, Lo SJ, Miyamura T, et al: Suppres-sion of hepatitis B virus expresSuppres-sion and replication by hepatitis C virus core protein in HuH-7 cells. J Virol 67:5823-5832, 1993
38. Schu¨ttler CG, Fiedler N, Schmidt K, et al: Suppression of hepatitis B virus enhancer 1 and 2 by hepatitis C virus core protein. J Hepatol 37:855-862, 2002
39. Anzola M: Hepatocellular carcinoma: Role of hepatitis B and hepatitis C viruses proteins in hepa-tocarcinogenesis. J Viral Hepat 11:383-393, 2004
40. Yu MW, Chen CJ: Elevated serum testoster-one levels and risk of hepatocellular carcinoma. Cancer Res 53:790-794, 1993
41. Wu MH, Ma WL, Hsu CL, et al: Androgen receptor promotes hepatitis B virus-induced hepato-carcinogenesis through modulation of hepatitis B virus RNA transcription. Sci Transl Med 2:32-35, 2010
42. Farinati F, De Maria N, Marafin C, et al: Hepatocellular carcinoma in alcoholic cirrhosis: Is sex hormone imbalance a pathogenetic factor? Eur J Gastroenterol Hepatol 7:145-150, 1995