Occupational Health and Risk Factors Among
Healthcare Workers in Emergency Departments
Li-Ya Lin
Abstract
Improving occupational health among health care workers in emergency departments is important. Although the influences of work demands and environment on health have been highlighted in the concept of workplace health promotion, inadequate knowledge about the specific health issues and the risk factors have increased the difficulty of developing effective workplace interventions to promote occupational health for health care workers in emergency departments. Therefore, this study aims to investigate the occupational health problems and the relevant risk factors among this particular group. Study surveyed 403 health care workers in Taiwanese 9 emergency departments. Descriptive analysis was used to explore the frequency distribution of demographic data and health problems. Further analysis about the relationships between risk factors and work-related injuries or diseases was conducted using Chi-square and logistic regression model. Smoking (3%), alcohol consumption (14.7%), and overweight Assistant Professor, Department of Nursing, Tzu Hui Institute of Technology, E-mail: lly_1106@yahoo.com.tw
Manuscript received: March 15, 2019; Revised: August 24, 2019; Accepted: September 10, 2019 DOI: 10.3966/207010632018120050003
(21.5%) are identified as unhealthy lifestyles among health care workers in emergency departments. Open wounds (53.1%), musculoskeletal disorders (55%), and mental health-related disorders (24.2%) are the common work-related injuries and diseases. Health care workers with physical health problems were more likely to report a work-related injury or disease than health care workers without physical health problems (OR = 1.84, 95% CI = 1.11-3.03, p < .05) . Moreover, participating health care workers who perceived that certain postures and repetitive motions were harmful were more likely to report a work-related injury or disease than health care workers who did not (OR = 2.15, 95% CI = 1.32-3.50, p < .05). In addition, the workplace issues about managers endeavor to address the welfare among health care workers, and long-term staff shortage in emergency departments, are considered as the important factors affecting occupational health and safety among this group. This study provides the evidence of unhealthy lifestyles and occupational injuries among emergency departments workers, but also indicates the problem of working environment factors affects the perception of occupational health and safety. These results can be used as an important reference for future emergency workplace health promotion programs.
Key words: emergency department, health care workers, health promotion, occupational health and safety, workplace risk factors
Introduction
Following the international movement, a series of health promotion programs has designed to address comprehensive improvement of health and well-being in Taiwanese workplaces (Hsu et al., 2009; Huang et al., 2012). However, the outcomes and implementation appear to be limited as a result of that the majority of program designs have poor considered the specific health problems of the target population (Hsu et al., 2009; Lin & Lin, 2011).
Research found that the prevalence of health problems among workers is not uniform, but varies in different occupational categories (Huang et al., 2012). The nature of job demands and physical environment makes health care workers (HCWs) in emergency departments (EDs) become the particular group that needs more attention to their health problems (Hogarth, Beattie, & Morphet, 2016). The impacts of occupational health do not merely cause disability for individual workers, but also affect hospitals in regard to compensation, work productivity, absenteeism and sick leave (Pompeii, Lipscomb, & Dement, 2010). However, lacking data of work-related injury and illness for EDs in the governmental statistics (Bureau of Labor Insurance, Ministry of Labor, 2012), and rare studies investigating the specific workplace health and safety among this group of workers increase the difficulty in understanding their occupational health concerns and problems. This may also affect the direction and efficiency of programs development in workplace health promotion. Therefore, the aim of this study is to investigate the occupational health problems and the relevant risk factors among HCWs in EDs.
Methods
EDs were randomly selected in the areas of north, middle and south in Taiwanese hospitals (3 hospitals for each area, and each hospital has more than 500 inpatient beds). Except HCWs did not completed their probation period, all full-time and qualified HCWs including physicians, nurses, pharmacists, technicians or other professional support personnel in the selected EDs were recruited.
A structured questionnaire was specifically designed and based primarily on the sample questions of healthy workplace (World Health Organization, 1999), and was approved by experts in the fields of emergency medicine, nursing, health promotion, and occupational health and safety. In order to identify health issues among HCWs in EDs, questionnaire was proposed to investigate demographic data; physical health problems; plan of health improvement; as well as work-related injuries and diseases. After data collection, descriptive analysis was used to explore the frequency distribution of demographic data and health problems. This study used Chi-square and logistic regression to examine the correlations between self-reported work-related injuries/diseases and the different personal and workplace variables.
Results
A total of 403 questionnaires were distributed and 326 (80.9%) questionnaires were returned. The majority of respondents were registered nurses (65.3%), university qualification (77.0%), an average of 33 years old, and an average of 5.36 years of working experience in EDs. However, around one fifth of participants (n = 70, 21.5%) could be identified as overweight because their BMI was equal or higher than 25.0 kg/m2 (Table 1). The plans and considerations for improving personal health in the year ahead, do more exercise (n = 228, 70.2%), adopt a healthy diet (n = 220, 67.7%), or remove a major source of worry, nerves or stress from life (n = 179, 55.1%) were common.
Table 1
Demographic characteristics of respondents (N = 326)
Variable n % Mean SD Occupations Physician 89 27.3 Registered nurse 213 65.3 Othersa 23 7.0 Not indicated 1 0.3 Gender Male 105 32.2 Female 220 67.5 Not indicated 1 0.3 Marital status Single 153 46.9 Married 169 51.8 Separated/Divorced 4 1.2 Age (y/o) Range = 21-62 32.78 8.07 Not indicated 1 0.3 BMI 22.39 3.55 Underweight (<18.5) 42 12.9 Normal range (18.5-24.9) 208 63.9 Overweight (≥ 25.0) 70 21.5 Not indicated 6 1.8 Educational level
Senior high school 3 0.9
Diploma 47 14.4
University 251 77.0
Postgraduate 25 7.7
a including pharmacists, radiologists or other technicians who are responsible to EDs, and
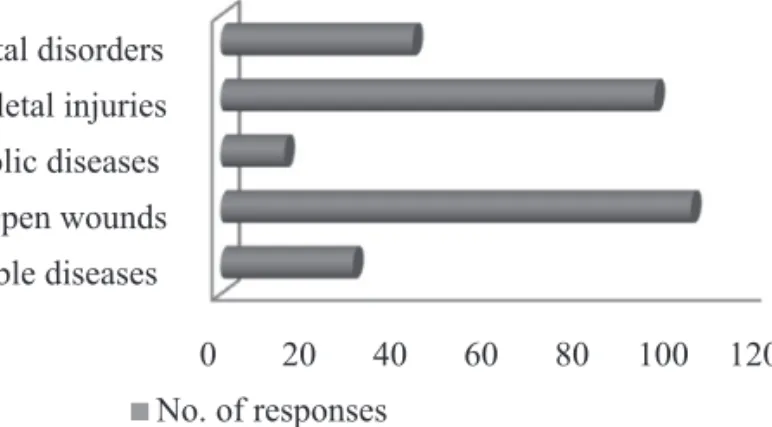
A total of 173 participating HCWs (53.1%) reported experiences of work-related injury or diseases. Among this group, open wounds (e.g. needlesticks, sharps or cutting wounds) were the most common injury, accounting for two thirds of that group (n = 103, 60%). Musculoskeletal disorders (MSDs) were reported by more than half of experienced staff (n = 95, 55%), and it is ranked as the second in frequency of occupational injuries in selected EDs. Moreover, about one quarter of experienced staff (n = 42, 24.2%) suffered from work-related mental health-related problems such as excessive stress, depression and anxiety. Nearly one fifth experienced transmissible respiratory diseases (n = 29, 16.7%) (Figure 1).
0 20 40 60 80 100 120
Respiratory transmissible diseases Open wounds Hormonal or metabolic diseases
Musculoskeletal injuries Mental disorders
No. of responses
Figure 1 Frequency distribution of the common occupational injuries or diseases
experienced among emergency HCWs (N = 326)
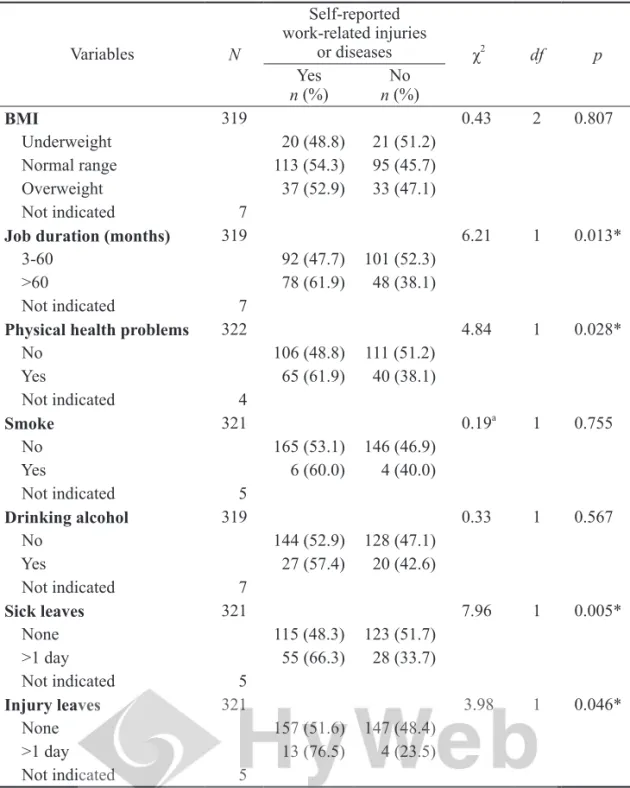
Some variables can affect work-related injuries or diseases among HCWs in EDs. The results show that there are significant differences in the distributions of marital status (χ2 = 3.86, p < .05), job duration (χ2 = 6.21, p < .05) and physical health problems (χ2 = 4.84, p < .05) between HCWs who reported work-related injuries or diseases and those who did not. In addition, HCWs with sick leave and injury leave had higher percentage of self-reported work-related injuries or diseases, respectively 66.3% and 76.5% ( p < .05) (Table 2). Such high absenteeism resulting from work-related injuries or diseases may suggest that exposures to
occupational hazards in ED workplaces were serious to HCWs. This finding may raise issues in association with not merely on health condition of individual workers, but also financial lost and normal operation in an ED.
Table 2
Self-reported work-related injuries or diseases by personal variables
Variables N Self-reported work-related injuries or diseases χ2 df p Yes n (%) n (%)No Health occupations 301 1.08 1 0.300 Physician 45 (50.6) 44 (49.4) Registered nurse 121 (57.1) 91 (42.9) Not indicated 25 Gender 324 1.45 1 0.228 Male 51 (48.6) 54 (51.4) Female 122 (55.7) 97 (44.3) Not indicated 2 Marital status 320 3.86 1 0.049* Single 73 (47.7) 80 (52.3) Married 98 (58.7) 69 (41.3) Not indicated 6 Age (y/o) 311 4.02 2 0.134 20-30 73 (48.3) 78 (51.7) 31-40 76 (60.3) 50 (39.7) 41-50 19 (55.9) 15 (44.1) Not indicated 15 Educational levels 321 0.49 2 0.784 Diploma 24 (52.2) 22 (47.8) University 137 (54.8) 113 (45.2) Postgraduate 12 (48.0) 13 (52.0) Not indicated 5 (continued)
Table 2 (continued) Variables N Self-reported work-related injuries or diseases χ2 df p Yes n (%) n (%)No BMI 319 0.43 2 0.807 Underweight 20 (48.8) 21 (51.2) Normal range 113 (54.3) 95 (45.7) Overweight 37 (52.9) 33 (47.1) Not indicated 7
Job duration (months) 319 6.21 1 0.013*
3-60 92 (47.7) 101 (52.3)
>60 78 (61.9) 48 (38.1)
Not indicated 7
Physical health problems 322 4.84 1 0.028*
No 106 (48.8) 111 (51.2) Yes 65 (61.9) 40 (38.1) Not indicated 4 Smoke 321 0.19a 1 0.755 No 165 (53.1) 146 (46.9) Yes 6 (60.0) 4 (40.0) Not indicated 5 Drinking alcohol 319 0.33 1 0.567 No 144 (52.9) 128 (47.1) Yes 27 (57.4) 20 (42.6) Not indicated 7 Sick leaves 321 7.96 1 0.005* None 115 (48.3) 123 (51.7) >1 day 55 (66.3) 28 (33.7) Not indicated 5 Injury leaves 321 3.98 1 0.046* None 157 (51.6) 147 (48.4) >1 day 13 (76.5) 4 (23.5) Not indicated 5
a There is more than 20% of total cells having expected count < 5. The result is Fisher’s
Exact Test. *p < .05
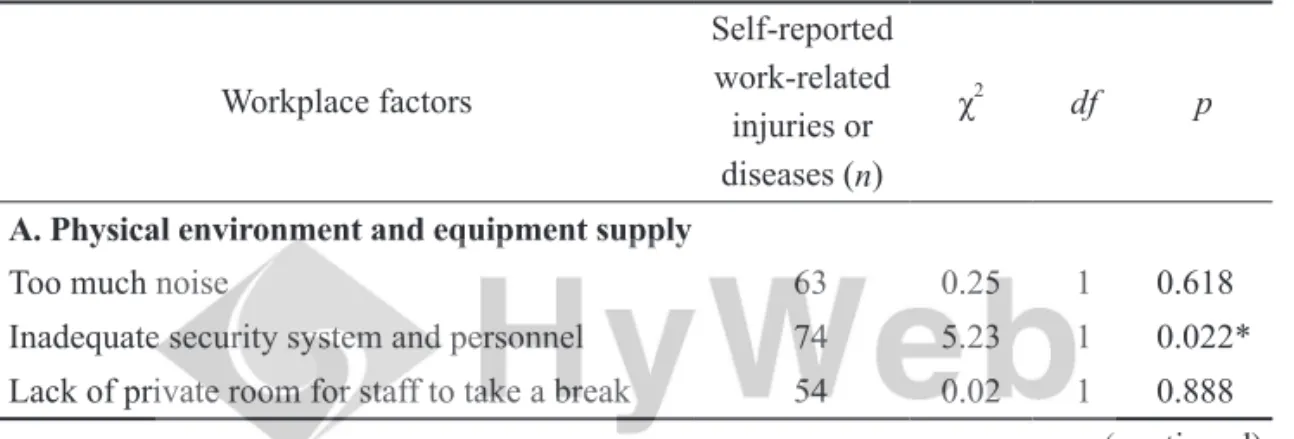
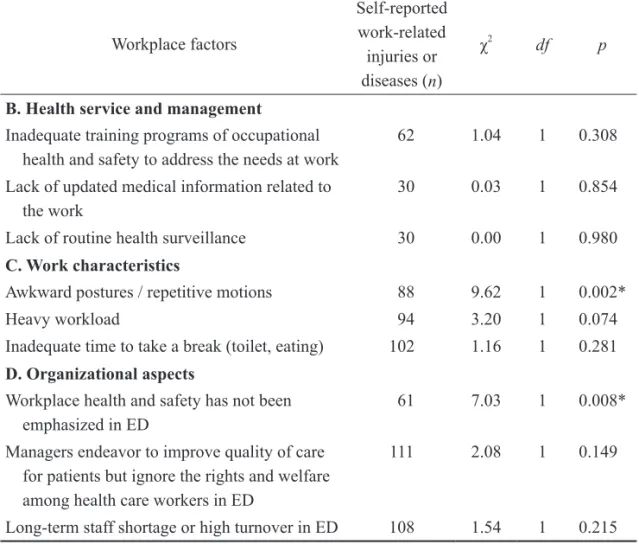
Alongside the individual health problems, and health-related behaviors, occupational health and safety (OHS) status among HCWs in EDs can also be attributed to various workplace factors. This study investigated four elements of workplace factors which may cause exposure incidents or concerns among HCWs. These are: physical environment and equipment supply, health service and management, work characteristics, and organizational aspects.
Table 3 presents the top 3 common concerns about workplace factors affecting OHS in each element of ED workplaces. Among these issues, “managers endeavor to improve quality of care for patients but ignore the rights and welfare among HCWs in ED,” and “long-term staff shortage or high turnover in ED” are the highest ranking in all elements. Results indicate that organizational aspects pose greater concerns regarding health and safety to HCWs than other elements of workplace factors. Moreover, these two issues highlight the importance for hospital managers of reviewing current efforts to address the interests of HCWs, as well as of developing effective strategies to retain and recruit ED staff.
Table 3
The association between the workplace factors and self-reported work-related injuries or diseases among HCWs (N = 326) (only the top 3 factors)
Workplace factors Self-reported work-related injuries or diseases (n) χ2 df p
A. Physical environment and equipment supply
Too much noise 63 0.25 1 0.618
Inadequate security system and personnel 74 5.23 1 0.022* Lack of private room for staff to take a break 54 0.02 1 0.888
Table 3 (continued) Workplace factors Self-reported work-related injuries or diseases (n) χ2 df p
B. Health service and management
Inadequate training programs of occupational health and safety to address the needs at work
62 1.04 1 0.308
Lack of updated medical information related to the work
30 0.03 1 0.854
Lack of routine health surveillance 30 0.00 1 0.980 C. Work characteristics
Awkward postures / repetitive motions 88 9.62 1 0.002*
Heavy workload 94 3.20 1 0.074
Inadequate time to take a break (toilet, eating) 102 1.16 1 0.281 D. Organizational aspects
Workplace health and safety has not been emphasized in ED
61 7.03 1 0.008*
Managers endeavor to improve quality of care for patients but ignore the rights and welfare among health care workers in ED
111 2.08 1 0.149
Long-term staff shortage or high turnover in ED 108 1.54 1 0.215 *p < .05
This study further explores the associations between the factors of workplace concern and self-reported work-related injuries or diseases among emergency HCW. Chi-square tests indicate that there are significant differences in the distributions of “inadequate security system and personnel” (χ2 = 5.23, df = 1, p < .05); “awkward postures / repetitive motions” (χ2 = 9.62, df = 1, p < .05); and “workplace health and safety has not been emphasized in ED” (χ2 = 7.03, df = 1, p < .05) between HCWs with reported work-related injuries or diseases and HCWs
without reported work-related injuries or diseases ( p < .05) (Table 3).
As can be seen from the Table 3, it is interesting to note that the most common concerns about potential factors affecting OHS in ED workplaces seem do not distinguish between people with and without work-related injuries or diseases. “Too much noise” is an example. A possible explanation for this might be that the risk perception can affect individual’s behavior for self-protection (Gralton, Rawlinson, & McLaws, 2013).
Logistic regression was performed to assess the impact of a number of personal factors and workplace factors on the likelihood that participating HCWs would report work-related injuries or diseases. Six significant variables (marital status; job duration; physical health problems; inadequate security system and personnel; awkward postures / repetitive motions; and workplace health and safety has not been emphasized in ED) were analyzed together. The results show that all predictors were statistically significant (χ2 = 31.93, p < .001) in distinguishing between participating HCWs who reported and those who did not report a work-related injury or disease. Among these six variables, only the variables of “physical health problems” and “awkward postures / repetitive motions” were statistically significant in work-related injuries or diseases (Table 4). The results show that participating HCWs with physical health problems were more likely to report a work-related injury or disease than HCWs without physical health problems (OR = 1.84, 95% CI = 1.11-3.03, p < .05) . Moreover, participating HCWs who perceived that certain postures and repetitive motions were harmful were more likely to report a work-related injury or disease than HCWs who did not (OR = 2.15, 95% CI = 1.32-3.50, p < .05).
Table 4
The relationships between predictors and self-reported work-related injuries or diseases
Variables OR 95% CI
Marital statusa 1.37 0.82-2.31
Job durationb 1.67 0.99-2.81
Physical health problemsc 1.84* 1.11-3.03
Inadequate security system and personneld 1.54 0.93-2.55
Awkward postures / repetitive motionse 2.15* 1.32-3.50
Workplace health and safety has not been
emphasized in EDsf 1.70 0.99-2.90
aReferent is single; bReferent is less than 5 years; cReferent is no physical health problems; dReferent is no concern about inadequate security system and personnel; eReferent is
no concern about awkward posture / repetitive motions; fReferent is no concern about
workplace health and safety has not been emphasized in EDs. *p < .05
Discussions
Following the initiative of health promotion, the majority of hospitals in this study have designed and implemented some programs aimed at unhealthy behaviors changes for hospital workers (Lee, Chen, & Chu, 2013). But the evidence in this study shows that smoking, overweight, alcohol consumption and physical exercise had not been successfully addressed. It is important to review current outcomes of health improvement for HCWs. Health promotion program managers and hospital executives may need to consider the subsequences of these unhealthy behaviors, such as “presenteeism” at work and the burden of health costs (Cancelliere, Cassidy, Ammendolia, & Côté, 2011; Scarborough et al., 2011).
determines to occupational health among HCWs in EDs. The common work-related injuries and illnesses found in this study were open wounds and musculoskeletal injuries. One unanticipated finding was that although 13% of respondents reported mental health-related illnesses such as excessive stress, anxiety and depression, no record of reported mental health disorders among the relevant groups was found in the statistics released from the government authority (Bureau of Labor Insurance, Ministry of Labor, 2014). In addition to a common phenomenon of underreporting in hospital workplaces (Ouyang et al., 2017), this discrepancy might be caused by a lack of confirmation through medical diagnosis. It is important to note that psychological complaints are very personal feelings, especially the levels of stress. Although the symptomatic manifestations may not meet the diagnostic criteria of mental health disorders, these psychological distresses are more related to self-perceptions of poor health (Schreuder et al., 2012), and being significant predictors of intentions to leave the profession among HCWs (Vermeir et al., 2018).
With respect to occupational exposures, the research to date has tended to focus on risk behaviors and workplace conditions (Cheung, Szeto, Lai, & Ching, 2018; Hogarth et al., 2016). However, our study found a strong relationship between individual’s physical health problems and the probability of work-related injuries. This result can be supported by previous evidence which indicated that overweight and obesity are crucial in developing or exacerbating the symptoms of MSDs (Shiri, Karppinen, Leino-Arjas, Solovieva, & Viikari-Juntura, 2010). Further research regarding the impacts of individual health problems would be of great help in developing appropriate interventions to reduce the risk of hazards exposure.
Conclusions
This study provides the evidence of unhealthy lifestyles and occupational injuries among ED workers, but also indicates the problem of working environment
factors affects the perception of occupational health and safety. The study results must be interpreted with caution since the study was limited to HCWs in Taiwanese EDs. Moreover, self-reporting was adopted as the measure to collect data of occupational health, the validity of data reporting by respondents may need to be considered. Nevertheless, the findings of this study can be a valuable reference for understanding current occupational health and safety among HCWs in EDs. As EDs are one of risky workplaces in hospitals, executives should place importance on the issues of unhealthy lifestyles and occupational hazard exposures on developing effectiveness of health programs in contemporary hospital settings.
References
Bureau of Labor Insurance, Ministry of Labor. (2012). Annual report 2012. Retrieved from http://www.bli.gov.tw/en/sub.aspx?a=A0cWbbyNSr8%3d
Bureau of Labor Insurance, Ministry of Labor. (2014). Occupational diseases cash
benefits, by cause and industry. Retrieved from https://events.bli.gov.tw/report.
aspx?y=103&f=h380
Cancelliere, C., Cassidy, J. D., Ammendolia, C., & Côté, P. (2011). Are workplace health promotion programs effective at improving presenteeism in workers? A systematic review and best evidence synthesis of the literature. BMC Public
Health, 11, 395.
Cheung, K., Szeto, G., Lai, G. K. B., & Ching, S. S. Y. (2018). Prevalence of and factors associated with work-related musculoskeletal symptoms in nursing assistants working in nursing homes. International Journal of Environmental
Research and Public Health, 15(2), 265-279.
Gralton, J., Rawlinson, W. D., & McLaws, M. L. (2013). Health care workers’ perceptions predicts uptake of personal protective equipment. American Journal
of Infection Control, 41(1), 2-7.
Hogarth, K. M., Beattie, J., & Morphet, J. (2016). Nurses’ attitudes towards the reporting of violence in the emergency department. Australasian Emergency
Nursing Journal, 19(2), 75-81.
Hsu, S.-W., Lin, J.-D., Lee, K.-T., Loh, C.-H., Yen, C.-F., Lin, L.-P., ...Chou, Y.-C. (2009). Employees’ perception of workplace health promotion initiatives in Taiwan: Across-sectional survey of 30 worksites. Industrial Health, 47(5), 551-559.
Huang, S.-L., Lee, H.-S., Li, R.-H., Lai, Y.-M., Chen, L.-C., & Tang, F.-C. (2012). Differences in health complaints among Taiwanese workers in different
occupational categories. Journal of Occupational Health, 54(3), 241-249.
Lee, C. B., Chen, M. S., & Chu, C. M.-Y. (2013). The health promoting hospital movement in Taiwan: Recent development and gaps in workplace. International
Journal of Public Health, 58(2), 313-317.
Lin, Y.-W., & Lin, Y.-Y. (2011). Health-promoting organization and organizational effectiveness of health promotion in hospitals: A national cross-sectional survey in Taiwan. Health Promotion International, 26(3), 362-375.
Ouyang, B., Li, L. D. X., Mount, J., Jamal, A. J., Berry, L., Simone, C., ...Tai, R. W. M. (2017). Incidence and characteristics of needlestick injuries among medical trainees at a community teaching hospital: A cross-sectional study. Journal of
Occupational Health, 59(1), 63-73.
Pompeii, L. A., Lipscomb, H. J., & Dement, J. M. (2010). Predictors of lost time from work among nursing personnel who sought treatment for back pain. Work, 37(3), 285-295.
Scarborough, P., Bhatnagar, P., Wickramasinghe, K. K., Allender, S., Foster, C., & Rayner, M. (2011). The economic burden of ill health due to diet, physical inactivity, smoking, alcohol and obesity in the UK: An update to 2006-07 NHS costs. Journal of Public Health, 33(4), 527-535.
Schreuder, J. A. H., Roelen, C. A. M., Groothoff, J. W., van der Klink, J. J. L., Magerøy, N., Pallesen, S., ...Moen, B. E. (2012). Coping styles relate to health and work environment of Norwegian and Dutch hospital nurses: A comparative study.
Nursing Outlook, 60(1), 37-43.
Shiri, R., Karppinen, J., Leino-Arjas, P., Solovieva, S., & Viikari-Juntura, E. (2010). The association between obesity and low back pain: A meta-analysis. American
Journal of Epidemiology, 171(2), 135-154.
Vermeir, P., Blot, S., Degroote, S., Vandijck, D., Mariman, A., Vanacker, T., ...Vogelaers, D. (2018). Communication satisfaction and job satisfaction among critical care nurses and their impact on burnout and intention to leave: A questionnaire study.
Intensive and Critical Care Nursing, 48, 21-27.
World Health Organization. (1999). Regional guidelines for the development of healthy
workplaces. Retrieved from https://www.who.int/occupational_health/regions/en/
急 診 室 醫 療 人 員 的 職 業 健 康
與 危 險 因 子
林麗雅
摘要
改善急診室醫療人員的職業健康非常重要。儘管在工作場所健康促進的 概念中已強調工作需求和環境對健康的影響,但對特定健康問題和風險因素 的了解不足,造成工作場所為急診醫療人員制定相關提升職業健康措施的難 度。因此,本研究旨在調查該特定群體的職業健康問題和相關風險因素。本 研究調查臺灣九個急診室共403個醫護人員,利用描述性分析來探討人口統 計學的分布情況與常見的健康問題;利用卡方檢驗和邏輯迴歸模型進一步分 析風險因素與工作相關的傷害或疾病之間的關係。研究結果發現,急診醫護 人員的不健康生活型態包括吸菸 (3%)、飲酒 (14.7%)、體重過重 (21.5%);最 常見的工作傷害與疾病則是開放性傷口 (53.1%)、肌肉骨骼疾病 (55%) 和心理 健康相關疾病 (24.2%)。有身體健康問題的醫護人員表示工作造成的受傷或疾 病的可能性,是沒有身體健康問題醫護人員的1.8倍;而認為某些姿勢和重複 性動作有害健康的醫護人員表示造成工作相關傷害或疾病的可能性,是沒有 認為姿勢和重複性動作有害健康醫護人員的兩倍多。此外,管理階層的努力 與急診醫護人員短缺的議題,被認為是影響職業健康安全的重要工作環境因 素。本研究顯示急診醫護人員不健康的生活型態與疾病傷害的比例,同時也 發現工作環境因素的問題影響職業健康與安全的認知,本研究結果可作為未 來急診工作場所健康促進計畫的重要參考依據。 慈惠醫護管理專科學校護理科助理教授,E-mail: lly_1106@yahoo.com.tw 通訊地址:屏東縣南州鄉三民路367號,聯絡電話:08-8647367轉341關鍵詞: 急診室、醫護人員、健康促進、職業健康與安全、工作場所風險因 素