Inclusion of Tissue Beyond a Midline Scar in the Deep Inferior
Epigastric Perforator Flap
Steven L. Henry, MD,* Chang-Cheng Chang, MD,† Alok Misra, MD, FRCS (Plast),† Jung-Ju Huang, MD,†
and Ming-Huei Cheng, MD, MHA, FACS†
Background: A lower abdominal midline scar is known to restrict the amount of tissue that can be included in a deep inferior epigastric perforator (DIEP) flap. However, reconstructive demands have occasionally led us to include substantial territory beyond the scar. The purpose of this study is to review our experience with such flaps and to determine whether a meaningful amount of tissue can be reliably harvested across a midline scar.
Methods: Within a series of 125 DIEP flaps harvested across the entire lower abdomen (zones I–IV), 11 contained a midline scar. These 11 cases were compared with the remaining 114 in terms of (1) the amount of tissue beyond the scar that could be retained with the flap based on intraoperative assess- ment of vascularity and (2) postoperative complications.
Results: A significantly smaller percentage of the flap volume could be retained in scarred abdomens (70% of the harvested ellipse [ie, 20% beyond the midline]) versus unscarred abdomens (83%; P = 0.01). Complications were more frequent in the flaps with scars (55% vs. 25%; P = 0.04), although most of these complications were easily manageable and acceptable
outcomes were achieved in all 11 cases.
Conclusion: The rate of complications is significantly higher when tissue across a midline scar is included in a DIEP flap. However, in our experience, these complications are relatively mild, and in most cases, a substantial amount of tissue beyond the midline can be used, thereby increasing the volume available for reconstruction without resorting to dual-supply proce- dures.
Key Words: deep inferior epigastric perforator flap, breast reconstruction, abdominal scar
(Ann Plast Surg 2011;67: 251–254)
he deep inferior epigastric perforator (DIEP) flap is widely considered the gold standard in autologous breast reconstruction, having excellent tissue characteristics and an essentially ideal donor site. Indeed, in our increasingly well-informed patient population, many women come to our clinic specifically requesting the DIEP procedure. As most of our Taiwanese patients are quite thin, we often need to transfer as much of the width of the flap as possible to attain adequate volume for the reconstructed breast.1 We have at
times been challenged by such patients who strongly prefer the
abdominal donor site and who require a wide flap, but who have a lower abdominal midline scar that bisects the DIEP flap territory. On these occasions, we have attempted to include some of the tissue across the midline scar (ie, part of Hartrampf zone II, or Henry and Cheng’s contralateral medial zone2) and for the most part have been
quite successful. The purpose of this study is to review our experi-ence with such flaps and to determine the average volume that can be safely harvested across a midline scar, thereby facilitating patient discussions and preoperative planning.
PATIENTS AND
METHODS
A retrospective chart review was conducted for all patients who underwent unilateral breast reconstruction with a DIEP flap by the senior author (M.H.C.) between March 2000 and April 2006. These 125 patients were divided into 2 groups: those with a lower abdominal midline scar (n = 11) and those with no scar (n = 114). The scars extended from just below the umbilicus to the pubis, and were from cesarean section in 9 patients, total abdominal hysterec-tomy in 1, and low anterior resection in 1. The mean age of the scars was 20 ± 8 years. Patients with other scars, such as appendectomy and Pfannenstiel scars, were excluded from analysis to minimize confounding variables. Patients who underwent bilateral breast re- construction with bilateral hemi-DIEP flaps were also excluded, as these flaps did not include tissue across the midline.
To test the 2 groups for similarity regarding other risk factors for flap complications, the subjects’ age, body mass index, recon-structive timing (ie, immediate vs. delayed), radiation therapy, number of perforators, and flap ischemia time were compared using Student t test (for the continuous variables) and Fisher exact test (for the categorical variables). Notably, there were no smokers in either group.
The groups were also compared regarding the amount of tissue retained in the flap intraoperatively. In all cases, the DIEP flap was harvested in the standard elliptical shape across the entire width of the abdomen, regardless of the presence of a midline scar. The volume of the harvested flap was measured by displacement of saline in a graduated cylinder. After transfer to the internal mam-mary vessels, the flaps were assessed visually and with pin prick for ischemia and congestion. Areas of questionable vascularity were trimmed back successively until the skin’s color and recapillariza-tion were normal and the skin edges bled appropriately (ie, bright red and not inordinately brisk, implying adequate inflow without congestion). The volume of resected tissue was measured and subtracted from the harvested volume to determine the retained volume. This value was divided by the harvested volume to calculate the percentage of flap retained. Student t test was used to compare the retained percentages of the 2 groups.
Finally, the 2 groups were compared regarding the incidence of flap complications using Student t test. For this and all statistical comparisons, a P value of less than 0.05 was considered significant.
RESULTS
Patient characteristics are summarized in Table 1. There were no statistically significant differences in any of the variables except
age, which was approximately 7 years greater in the group with midline abdominal scars (P < 0.01). This disparity is attributable to 2 factors: (1) cesarean sections, in our society, were performed through a midline incision 20 years ago, but through a Pfannenstiel incision more recently; and (2) the other procedures resulting in a midline scar (hysterectomy and colectomy) are more commonly performed in older women. Although statistically significant, this difference was deemed not to be clinically significant in terms of surgical outcome after breast reconstruction. Notably, radiation history was substantially more common in the scar group, although this difference did not reach statistical significance.
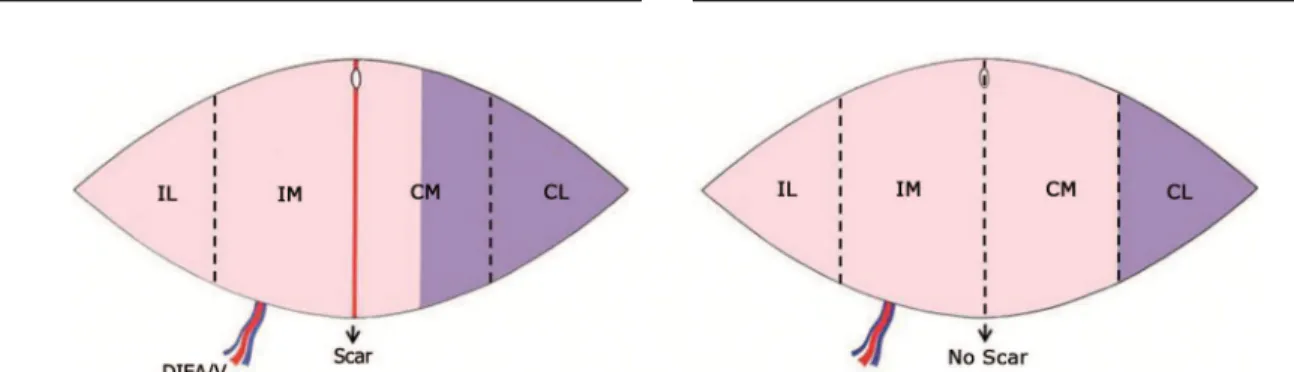
The percentage of flap retained was substantially lower in the scar group (mean, 70% of the harvested volume; range, 54%– 88%) than in the control group (mean, 83%; range, 48%–100%). This difference was statistically significant (P < 0.01). In our patient population, in which typical flap dimensions were 32 × 12 cm, the intraoperative demarcation was usually about 3 cm beyond the scar, or about half of the contralateral medial zone (Fig. 1).3
The incidence of complications was significantly higher in the flaps with midline scars, primarily in the form of marginal skin necrosis (Table 2). Not unexpectedly, this necrosis appeared along the border opposite the scar, although, in all cases, the affected area was quite small—at most a 5-mm strip. The occurrence of fat necrosis, defined as a palpable mass or firm area >1 cm3, was not
statistically different between the groups. Infection did occur at a higher rate in the scar group, although all cases were localized to the superficial wound and resolved quickly with antibiotics alone. While not statistically significant, there was a greater frequency of venous congestion in the scar group (in each case occurring in the area across the scar). Re-exploration was consequently also higher in the
scar group (Table 2). Every case of congestion was readily salvaged
with supplemental outflow through the superficial inferior epigastric vein (SIEV).
Donor site morbidity was negligible in all patients. There were no bulges/hernias, seromas, wound healing problems, or other donor site complications. Overall outcome of the breast reconstruc-tion was acceptable in all cases.
DISCUSSIO
N
For breast reconstruction, no other donor site can match the abdomen’s many advantages, including ease of patient positioning, soft and pliable tissue, long pedicle, and (in the case of DIEP or superficial inferior epigastric artery [SIEA] flaps) minimal morbid-ity. Most patients also strongly favor the abdominal donor site and welcome the ancillary abdominoplasty. We therefore have been inclined to reach for the DIEP flap even when the presence of a midline scar might be inauspicious. Fortunately, our success rate remains high even in these cases.
When faced with the situation under discussion—a patient with a midline lower abdominal scar who desires the use of abdom-inal tissue for breast reconstruction—the surgeon still has several choices. The simplest and safest option is to harvest a hemiabdomi-nal flap that excludes all of the tissue across the scar. However, especially in thin patients this approach is unlikely to yield a symmetric reconstruction. In those with a full contralateral breast, it may be necessary to perform a reduction (rarely desirable in our patients) or to place an implant under the flap (also rarely desirable, as this defeats much of the purpose of autologous reconstruction).
TABLE 2. Complications TABLE
1. CharacteristicsPatient
Risk
Factor Scar Control P*
Age (yr) 51 ± 10 44 ± 8 <0.01
BMI (kg/m2) 25 ± 1 23 ± 3 0.1
Immediate reconstruction 18% 28% 0.5
History of radiation 27% 13% 0.2
No. perforators 1.6 ± 0.5 1.8 ± 0.8 0.4
Ischemia time (min) 96 ± 24 90 ± 27 0.7
Scar Control P*
Total flap loss 0 0 —
Marginal skin necrosis 27% 4% 0.02
Fat necrosis 9% 19% 0.7 Infection 36% 4% <0.01 Hematoma 0% 1% 1 Venous congestion 18% 5% 0.1 Arterial insufficiency 0 0 — Re-exploration† 18% 5% 0.1 Overall complications 55% 25% 0.04
*Fisher exact test for immediate reconstruction and radiation, and Student t test for other variables.
BMI indicates body mass index.
*Student t test.
†
All re-explorations were performed for venous congestion, which in all cases was successfully corrected with supplemental outflow through the SIEV.
FIGURE 1. Left, In flaps with a midline scar approximately 70% of the entire flap volume appeared to be well vascularized (pink area) after harvest, with intraoperative demarcation occurring roughly 3 cm beyond the scar (contralateral medial zone). Right, In comparison, in unscarred flaps approximately 83% of the entire flap volume was judged to be viable. Different zones are described as follows: Im indicates ipsilateral medial; Il, ipsilateral lateral; Cm, contralateral medial; Cl, contralateral lateral; DIEA/V, deep interior epigastric artery and vein.
Another simple solution is to shift the flap superiorly, as advocated by Takeishi et al.3 If only a short segment of the scar is
included and a few periumbilical perforators are captured, the usual amount of tissue should be viable. However, the resulting donor site scar will reside in an unfavorable location.
A more complicated option is to employ an additional blood supply to the opposite side of the flap. Various permutations of this concept have been propounded in the literature, all with proven success, but each with a significant drawback:
• The conventional bipedicled transverse rectus abdominus
myocu-taneous (TRAM) flap is a relatively straightforward solution,4 but
we feel that its potential donor site morbidity is prohibitive in the modern era of perforator flaps.5–7
• The “supercharged” TRAM is a unipedicled flap with microvas-cular anastomosis of the deep inferior epigastric artery/vein (DIEA/V [or SIEA/V]) to recipients in the chest.8,9 Although this
strategy is well-established, we find that combining pedicle and free techniques mitigates the advantages of either, while com-pounding the disadvantages of both.
• The “turbocharged” TRAM (also described as the “recharged” or “parasite” TRAM) is similar to the supercharged TRAM, but with anastomosis of the opposite DIEA/V to the distal end of the ipsilateral DIEA/V, so that the opposite side of the flap is supplied by retrograde runoff from the pedicled side.10,11 While
this tech- nique eliminates the need to dissect a recipient site on the chest, it otherwise retains the disadvantages of combined pedicle and free techniques.
• A dual-pedicled DIEP/SIEA flap (or 2 separate hemi-DIEP/SIEA flaps) would be appropriate if an exceptionally large amount of tissue were needed,12–14 but it requires that 2 pedicles be dissected
and 2 sets of anastomoses be performed. Insetting such a construct can also be challenging.
• Various “crossover” free flaps have been used successfully for patients with midline scars. Utilizing a free TRAM flap, Penning-ton et al dissected a DIEP pedicle from the opposite side of the flap and anastomosed it to the distal end of the DIEA/V of the main pedicle, thereby connecting the 2 sides of the flap “in series.”15 Schoeller et al adopted the same crossover strategy with
a DIEP flap.16 A slightly different tactic was employed by Lam
and Sellars, who connected the opposite DIEP pedicle to a premuscular branch of the main pedicle of a free TRAM flap, creating a “parallel circuit” for the 2 sides.17 Ali et al performed
the same crossover anastomosis in a DIEP flap, but divided and stacked the 2 halves of the flap18 (Whether a series or parallel
configuration is hemodynamically preferable is unclear). All of these clever variations have the advantage of requiring only 1 recipient site on the chest, and we would probably chose one of them if we needed to retain the entirety of the tissue beyond the midline scar. However, the procedure remains complex and time consuming.
Another option—the one we chose—is to base the flap on 1 pedicle and include as much of the contralateral tissue as is ade-quately perfused. In this series, the average limit of perfusion, as assessed individually and determined intraoperatively in each flap, was approximately 3 cm beyond the scar, or about half of the contralateral medial zone. This amount of tissue is obviously less than what would typically be available to us in a scarless abdomen, but substantially more (in our patient population, approximately 75–125 mL) than what would be present in a hemi-DIEP flap (Fig. 2). Considering the tribulations of a dual-supply procedure, we believe this may be an acceptable tradeoff; although as part of this tradeoff, we (and the patient) must accept a greater risk of compli-cations.
FIGURE 2. Example of a patient in whom a relatively large amount (88%, 375/425 g) of tissue across a midline scar was successfully included in a DIEP flap. In this very thin pa- tient, use of only the ipsilateral half of the abdominal ellipse would have resulted in a smaller-than-desired breast.
Our assessment of tissue viability was based entirely on clinical judgment—specifically, by trimming back questionable tis-sue until normal skin color, recapillarization, and bleeding edges were reached. Importantly, in many flaps we still encountered a small area of marginal skin necrosis, which leads us to recommend that a thin (perhaps, 5–10 mm) margin of healthy-appearing tissue also be resected and the wound should be loosely closed to minimize complications. Other means of assessing tissue perfusion, such as indocyanine green or tissue oximetry, could perhaps improve the accuracy of intraoperative assessment and would be an interesting direction for future studies. However, clinical judgment would likely remain the gold standard, considering that even if hypoperfusion were seen acutely, choke vessels may later open and render the tissue viable.
One might argue that the higher rate of complications en-countered in our series should contraindicate the inclusion of tissue across a midline scar in a DIEP flap. Based strictly on statistics, this is certainly a defensible argument, and for some surgeons the higher rate may be unacceptable. However, in our experience, the magni-tude and consequence of those complications are quite mild. Many cases of marginal necrosis required only bedside debridement, and in no case was the volume of the flap appreciably reduced. The rate of fat necrosis was not higher, implying that the retained subcuta-neous tissue was adequately vascularized. All cases of infection were mild and were successfully treated with antibiotics alone. Finally, although a greater percentage of flaps were re-explored for apparent venous congestion, all improved with supplementary out-flow through the SIEV and went on to heal uneventfully. All of this being said, it is important to note that many of the patients in the scar group who developed complications had previously undergone chest wall radiation; while this was not identified as a risk factor unique to the scar group, it certainly may have contributed to the complica- tions in those particular patients.
That the option we chose is often disregarded—and that surgeons would go to such great lengths in order to “charge” the tissue across a midline scar—is not unreasonable, given the infor-mation provided in anatomic and animal studies. Two frequently cited examples are the cadaveric injection study by Moon and Taylor, wherein the 1 abdominal specimen with a midline scar demonstrated “virtually no midline (arterial) crossover at any anas-tomotic level,”19 and the rat TRAM flap study by Sano et al, who
observed a 100% incidence of complete necrosis of the portion opposite a midline scar.20 It must be remembered, however, that
these investigational modalities do not replicate human physiology. Even the intraoperative angiography study by Ohjimi et al, wherein ex vivo angiograms of 2 free TRAM flaps with midline scars showed no crossing arteries,21failed to account for the myriad
factors that determine tissue perfusion in situ.
Furthermore, not all such studies and experiences are in concert. Santamaria injected the DIEA in 7 patients with a midline scar and observed contrast material in the contralateral medial zone in all of them. He also reported the successful incorporation of the contralateral medial zone in 16 free TRAM flaps with a midline scar.22 Likewise, Heller et al, in a series of 43 free TRAM flaps
involving a midline scar, found that the contralateral medial zone was well vascularized (by intraoperative inspection) and could be retained in 9 flaps (21%), with no incidents of fat necrosis.23
Clearly, the amount of blood that crosses a scar can be clinically significant, even if no angiographically visible vessels are ob-served. There is histologic support for this notion: a recent investigation showed that microvessel density is increased in cutaneous scars— even those matured beyond 1 year— compared with unscarred dermis.24
Heller et al, in their study of free TRAM flaps, did warn that retaining “uncharged” tissue across a midline scar should not be attempted with a DIEP flap, in which overall vascularity is thought to be more tenuous.23 We would agree that the free TRAM flap may
be more robust, but nonetheless our results show that a substantial part of the contralateral medial zone can often be retained in a DIEP flap. Thus, in patients with a midline scar for whom a hemi-DIEP flap would be too small but a dual-supply procedure would be unnecessary, our practice is to harvest a DIEP flap per our routine, assess the viability of the tissue beyond the scar, and transfer as much tissue as appears safe intraoperatively (minus a few millime-ters to reduce the risk of marginal skin necrosis). We also keep a very low threshold for employing the SIEV for supplementary venous drainage. Based upon our experience, we can expect to retain up to 3 cm in width beyond the scar and can counsel our patients accordingly with regard to the need for a contralateral balancing procedure.
CONCLUSION
The inclusion of tissue across a midline scar in a DIEP flap results in a high rate of complications, including marginal skin necrosis, infection, and venous congestion. However, in our expe-rience, those complications are relatively mild and easily managed, and a significant amount of tissue that would otherwise be discarded can be successfully used to increase the volume of the reconstruc- tion. An acceptable result can therefore be achieved without resort- ing to complicated dual-supply procedures. Conservative judgment of tissue viability is recommended, as intraoperative clinical assess- ment can overestimate the amount of viable tissue.
ACKNOWLEDGMEN
TS
The authors thank Miffy Chia-Yu Lin and Chin-Yu Yang for their assistance in the preparation of this manuscript.
REFERENCES
1. Cheng MH, Robles JA, Ulusal BG, et al. Reliability of zone IV in the deep inferior epigastric perforator flap: a single center’s experience with 74 cases. Breast. 2006;15:158 –166.
2. Henry SL, Cheng MH. A call for clarity in TRAM/DIEP zones. Plast Reconstr Surg. 2010;125:210e–211e.
3. Takeishi M, Shaw WW, Ahn CY, et al. TRAM flaps in patients with abdominal scars. Plast Reconstr Surg. 1997;99:713–722.
4. Grotting JC, Anderson ED. In discussion: strategies and options for free TRAM flap breast reconstruction in patients with midline abdominal scars. Plast Reconstr Surg. 2005;116:760 –761.
5. Kroll SS, Schusterman MA, Reece GP, et al. Abdominal wall strength, bulging, and hernia after TRAM flap breast reconstruction. Plast Reconstr Surg. 1995;96:616 – 619.
6. Mizgala CL, Hartrampf CR Jr, Bennett GK. Assessment of the abdominal wall after pedicled TRAM flap surgery: 5- to 7-year follow-up of 150 consecutive patients. Plast Reconstr Surg. 1994;93:988 –1002; discussion 1003–1004.
7. Petit JY, Rietjens M, Ferreira MA, et al. Abdominal sequelae after pedicled TRAM flap breast reconstruction. Plast Reconstr Surg. 1997;99:723–729. 8. Marck KW, van der Biezen JJ, Dol JA. Internal mammary artery and vein
supercharge in TRAM flap breast reconstruction. Microsurgery. 1996;17: 371–374.
9. Lee JW, Lee YC, Chang TW. Microvascularly augmented transverse rectus abdominis myocutaneous flap for breast reconstruction–reappraisal of its value through clinical outcome assessment and intraoperative blood gas analysis. Microsurgery. 2008;28:656 – 662.
10. Semple JL. Retrograde microvascular augmentation (turbocharging) of a single-pedicle TRAM flap through a deep inferior epigastric arterial and venous loop. Plast Reconstr Surg. 1994;93:109 –117.
11. Berrino P, Casabona F, Adami M, et al. The “parasite” TRAM flap for autogenous tissue breast reconstruction in patients with vertical midabdomi-nal scars. Ann Plast Surg. 1999;43:119 –126.
12. Blondeel PN, Boeckx WD. Refinements in free flap breast reconstruction: the free bilateral deep inferior epigastric perforator flap anastomosed to the internal mammary artery. Br J Plast Surg. 1994;47:495–501.
13. Das-Gupta R, Busic V, Begic A. Deep inferior epigastric perforator flap (DIEP) breast reconstruction in the presence of a midline vertical scar. J Plast Reconstr Aesthet Surg. 2006;59:675– 676.
14. Beahm EK, Walton RL. The efficacy of bilateral lower abdominal free flaps for unilateral breast reconstruction. Plast Reconstr Surg. 2007;120:41–54. 15. Pennington DG, Nettle WJ, Lam P. Microvascular augmentation of the blood
supply of the contralateral side of the free transverse rectus abdominis musculocutaneous flap. Ann Plast Surg. 1993;31:123–126; discussion 126 – 127.
16. Schoeller T, Wechselberger G, Roger J, et al. Management of infraumbilical vertical scars in DIEP-flaps by crossover anastomosis. J Plast Reconstr Aesthet Surg. 2007;60:524 –528.
17. Lam TC, Sellars GD. Free perforator crossover TRAM flap for breast reconstruction. Ann Plast Surg. 2003;50:126 –131.
18. Ali RS, Garrido A, Ramakrishnan V. Stacked free hemi-DIEP flaps: a method of autologous breast reconstruction in a patient with midline abdominal scarring. Br J Plast Surg. 2002;55:351–353.
19. Moon HK, Taylor GI. The vascular anatomy of rectus abdominis musculo-cutaneous flaps based on the deep superior epigastric system. Plast Reconstr Surg. 1988;82:815– 832.
20. Sano K, Hallock GG, Rice DC. A vertical midline scar is a ‘high-risk’ factor for maximum survival of the rat TRAM flap. Ann Plast Surg. 2003;51:403– 408.
21. Ohjimi H, Era K, Fujita T, et al. Analyzing the vascular architecture of the free TRAM flap using intraoperative ex vivo angiography. Plast Reconstr Surg. 2005;116:106 –113.
22. Santamaria E. Paper presented at: The Annual Meeting of the World Society of Reconstructive Microsurgery; Jun 11–14, 2003; Heidelberg, Germany. 23. Heller L, Feledy JA, Chang DW. Strategies and options for free TRAM flap
breast reconstruction in patients with midline abdominal scars. Plast Reconstr Surg. 2005;116:753–759; discussion 760 –751.
24. Brown NJ, Smyth EA, Cross SS, et al. Angiogenesis induction and regression in human surgical wounds. Wound Repair Regen. 2002;10:245– 251.