Trauma
Head injuries in adolescents in Taiwan: a comparison between
urban and rural groups
Ming-Fu Chiang, MD, PhD
a,1, Wen-Ta Chiu, MD, PhD
b,c,1, H. Jasmine Chao, PhD
d,
Wan-Lin Chen, MD
c,e, Shu-Fen Chu, RN
c, Shiu-Jau Chen, MD
a,
Ching-Chang Hung, MD
b, Shin-Han Tsai, MD, PhD
c,e,f,4
a
Department of Neurosurgery, Mackay Memorial Hospital, Mackay Medicine, Management and Nursing College, Taipei, Taiwan
b
Division of Neurosurgery, andcInstitute of Injury Prevention and Control, Taipei Medical University-Wan Fang Medical Center, Taipei, Taiwan
d
Graduate Institute of Public Health, Taipei Medical University, Taipei, Taiwan
e
Division of Neurosurgery, Taipei City Hospital Renai Branch, Taipei, Taiwan
f
Department of Critical Care and Emergency Medicine, Taipei Medical University-Wan Fang Medical Center, Taipei, Taiwan Received 20 April 2006; accepted 21 August 2006
Abstract Background: Data pertaining to head injuries in adolescents in Taiwan are scarce. The purpose of
this study was to investigate the trend and pattern of head injuries in adolescents in both urban and rural areas in Taiwan.
Methods: We collected data from major hospitals in the urban (20) and in the rural (4) areas of Taiwan for a period of 3 years. Data were obtained from the Head Injury Registry, a 10-year electronic database of head injury in Taiwan. The inpatient medical records of adolescents with head injury were thoroughly reviewed. Severity of head injury was classified by the GCS score, and patient outcome at discharge from hospital was measured by the Glasgow Outcome Scale. Differences and correlation between study groups (13-15 and 16-18 years old) in the urban and rural areas were examined using 2-tailed t and v2tests.
Results: A total of 469 head injury cases in the urban area and 131 in the rural area were identified. Traffic accidents were the major cause of head injury, and motorcycles were the most predominant vehicles causing traffic accidents in both urban and rural areas. Intracranial hemorrhages were the most prevalent injury pattern in the study population. In both urban and rural areas, the severities of injury were not significantly different ( P = .184), but the outcomes at discharge were significantly better in urban areas ( P = .032). The correlation between the initial GCS and outcomes in both areas was significant ( P b .001). Craniotomy was performed more frequently in the rural area than in the urban area (15.3% vs 7.2%). The mean hospital stay was shorter in the latter than in the former ( P b .001). Education on helmet use, input of neurosurgical staff, and facility and emergency medical transportation service of head-injured patients following guidelines proposed by the WFNS are crucial for head injury and better control in rural areas.
Conclusions: The causes, patterns, and outcomes of head injury were statistically different between the 2 age groups of adolescents in urban and rural areas. Further studies on adolescent head injury are necessary. D 2006 Elsevier Inc. All rights reserved.
Keywords: Adolescent; Glasgow Coma Scale; Glasgow Outcome Scale; Head injury; Helmet use law; Intracranial hemorrhage; Motorcycle
0090-3019/$ – see front matterD 2006 Elsevier Inc. All rights reserved. doi:10.1016/j.surneu.2006.08.029
Abbreviations: EDH, epidural hematoma; GCS, Glasgow Coma Scale; GOS, Glasgow Outcome Scale; ICHs, intracranial hemorrhages; JHS, junior high school; SAH, subarachnoid hemorrhage; SDH, subdural hematoma; SHS, senior high school; TBI, traumatic brain injury; WFNS, World Federation of Neurosurgical Societies.
4 Corresponding author. Institute of Injury Prevention and Control, Taipei Medical University, Taipei, 110 Taiwan. Tel.: +886 2 27390217; fax: +886 2 27390387.
E-mail address: shtsai@tmu.edu.tw (S.-H. Tsai).
1 M.-F. Chiang and W.-T. Chiu contributed equally to this work.
1. Introduction
Since 1989, patients with head injury have had a 10-fold higher mortality than those bluntly traumatized without head injury [15]. Head injury is the leading cause of death in accidents, and motorcycle-related traffic accidents compose the majority (71%) of accidents in Taiwan[3,5,9,12,13,20]. In the analysis of age groups with accident mortality, the 10-to 19-year age group had the highest mortality rate, especially in the 15- to 19-year age group [3,14,18,21,22]. As most victims of motorcycle-related head injuries were young, the resulting cognitive, psychological, and neuro-logic sequelae were overwhelmingly damaging to society
[3]. How to prevent and control the mortality and morbidity of head injury in adolescents is therefore a challenging problem in Taiwan.
A long-term trend (1989-2000) showed that fatal head injuries in the age group from 15 to 20 years were
decreasing [18]. On June 1, 1997, the helmet use law was
implemented in Taiwan. Thereafter, the number of motorcycle-related head injuries and the severity of injury
decreased, and better outcomes were obtained [3].
How-ever, data regarding current status of head injuries in adolescents, especially the differences between urban and rural areas are lacking in Taiwan. Therefore, we conducted this study to investigate the distributions and patterns of head injuries in adolescents in both the urban and rural areas in Taiwan.
2. Materials and methods 2.1. Data collection
The data of patients with TBI in Taipei and Hualien were extracted from the Head Injury Registry. In the setting of the study, Taipei is defined as the urban area and Hualien County is defined as the rural area. These 2 areas differ in population density, the density and distribution of neuro-surgical centers, manpower personnel, and facilities.
Taipei City is the capital of Taiwan. It covers an area of
271.8 km2 and has a population of 2 630 000, with a
population density of 9737/km2. There are 20 major
neurosurgical centers equally distributed throughout the whole city district. A board-certified neurosurgeon serves about 17 533 people. It takes an average of 15 minutes to transport a patient with TBI by ambulance to a neurosur-gical center.
Hualien County, located at the eastern part of Taiwan, is a mountainous area. The area of the county is 4638.6 km2(the largest county in Taiwan) and population is 400 000; the population density is 133/km2. There are only 4 neurosur-gical centers in Hualien, all located downtown. A board-certified neurosurgeon serves about 26 667 people in Hualien. However, the geographic limitations in Hualien make transportation of patients with TBI time-consuming. It takes, on average, more than 1 hour to transport patients with TBI from the periphery or hills to each center.
In this collaborative case-series study, data on adoles-cents (aged between 13 and 18 years) with head injuries were collected from July 1, 2001, to June 30, 2004. We divided the adolescents into 2 age groups, the 13- to 15-year group (JHS) and the 16- to 18-year group (SHS). Data were collected from 20 major hospitals in an urban area and 4 major hospitals in a rural area.
Data were also obtained from the Head Injury Registry, a 10-year electronic database with more than 100 000 cases of head injury in Taiwan. The inpatient medical records of adolescents with head injury were thoroughly reviewed. Information pertaining to head injury including sex, age, GCS, cause and pattern of injury, presence of multiple systemic injuries, length of hospital stay, and GOS at discharge was analyzed. Diagnosis was made by brain computed tomography scans and skull x-rays to show various patterns of head injury: skull fracture, brain swelling/edema, and ICHs (epidural hematoma, subdural hematoma, ICH, subarachnoid hemorrhage).
2.2. Severity and outcomes
The severity of head injury was classified by the GCS score[11,19]as follows: (1) severe, score of 8 or below; (2) Table 1
Demography of study adolescents in urban and rural areas
Urban Rural P No. of cases 469 131 M:F 306:163 = 1.9 78:53 = 1.5 JHS 127 (27.1) 46 (35.1) SHS 342 (72.9) 85 (64.9) Causes b .001 Traffic 264 (56.3) 100 (76.3) Fall 81 (17.3) 8 (6.1) Assault 72 (15.4) 9 (6.9) Sports 26 (5.5) 3 (2.3) Traffic .002 Motorcycle 163 (34.8) 78 (59.5) Bicycle 19 (4.1) 10 (7.6) Walking 32 (6.8) 32 (6.8) Rider 129 (27.5) 55 (42) .025 Patterns .011 Skull fracture 75 (16) 18 (13.7) Swelling 67 (14.3) 7 (5.3) ICHs 118 (25.2) 29 (22.1) Craniotomy 34 (7.2) 20 (15.3) .011 GCS (JHS/SHS) .184 3-8 30 (6.4) (8/22) 13 (9.9 (3/10) 9-12 25 (5.3) (6/19) 12 (9.2) (6/6) 13-15 414 (88.3) (113/301) 106 (80.9) (37/69) Outcomes and GCS score (severe/ moderate/mild) b .001 Dead 13 (2.8) (11/2/0) 7 (5.3) (6/1/0) Vegetative 3 (0.6) (2/1/0) 3 (2.3) (2/1/0) Dependent 7 (1.5) (4/2/1) 7 (5.3) (2/2/3) Independent 25 (5.3) (4/3/18) 8 (6.1) (1/3/4) Good 421 (89.8) (9/17/395) 106 (80.9) (2/5/99) Values are presented as n (%).
moderate, score of 9 to 12, and the patient received neurosurgical intervention or had abnormal computed tomography scan findings; (3) mild, score of 13 to 15 or conditions not meeting any of the above criteria[3,9]. The
GOS [10]was used to categorize the outcome of patients
with head injury at the time of discharge from the hospital as follows: (1) death; (2) persistent vegetative state; (3) severe disability, conscious but dependent; (4) moderate disability, disabled but independent; (5) good recovery.
2.3. Statistical analysis
The incidence rates for head-injured adolescents were not calculated because the official statistics of the study population in both areas were not available. Differences and correlations between study groups and areas were examined by using 2-tailed t and v2 tests. A P value less than .05 was considered significant, and a P value between .05 and .10 was considered marginally significant.
3. Results
During the survey period, 469 adolescents (127 in JHS, 342 in SHS) with head injuries in the urban area and 131 (46 in JHS, 85 in SHS) in the rural area were identified. In the urban area, there were 306 (65%) teenaged boys and 163 (35%) girls with a male to female ratio of 1.9. In the rural area, there were 78 (60%) boys and 53 (40%) girls with a ratio of 1.5.
3.1. Causes of injury
In the urban area, the causes of injury included traffic accidents in 264 cases, falls in 81, assaults in 72, sports injuries in 26, falling objects in 3, and other causes in 23. In the rural area, the recorded accidents consisted of 100 traffic accidents, 11 hits by falling objects, 9 assaults, 8 falls, and 3 sports injuries. The differences in causes of head injury
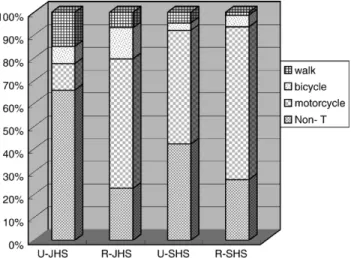
between the 2 areas were significantly different ( P b .001). In the causes of traffic accidents, there were 163 (34.8%) cases caused by motorcycles, 32 (6.8%) while walking, and 19 (4.1%) caused by bicycles in the urban area. In the rural area, there were 78 (59.5%) by motorcycles, 10 (7.6%) by bicycles, and 4 (3.1%) by walking (Table 1). The difference in causes of traffic accidents between the 2 areas was also significant ( P = .002). In the JHS and SHS groups of the urban area, causes of traffic accidents were 18 (14.2%) and 14 (4.1%) by walking, 14 (11%) and 149 (43.6%) by motorcycles, and 9 (7.1%) and 10 (2.9%) by bicycles, respectively ( P b .001). In the rural area, the causes were 25 (54.3%) and 53 (62.4%) by motorcycles, 6 (13%) and 4 (4.7%) by bicycles, and 3 (6.5%) and 1 (1.2%) by walking for the JHS and SHS groups, respectively ( P = .063) (Fig. 1
and Table 2). The causes of traffic accidents between the urban and rural areas in the groups were significantly different ( P b .001) (Table 2). In the motorcycle-related traffic accidents, 129 (73%) and 55 (65%) cases were riders of motorcycles in the urban and rural areas, respectively ( P = .025). There were 205 (43.7%) nontraffic injuries in the urban area and 31 (23.7%) in the rural area ( P = .004) (Table 1).
3.2. Pattern of injury
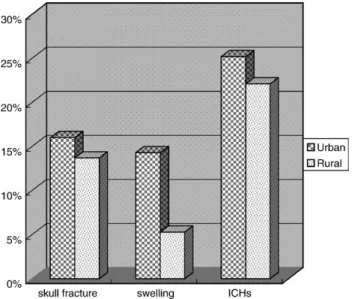
The patterns of head injury were available in 55.5% of cases in the urban area, including 75 (16%) cases with skull fracture, 67 (14.3%) with brain swelling, and 118 (25.2%) with ICHs. In the rural area, 41% of cases had disclosed injury pattern, consisting of 18 (13.7%) skull fractures, 7
(5.3%) brain swellings, and 29 (22.1%) ICHs (Table 1and
Fig. 1. Causes of head injury in groups (JHS, SHS) of adolescents in urban (U) and rural (R) areas. There were more motorcycle injuries in rural areas and nontraffic injuries in JHS groups of urban areas. Non-T indicates nontraffic.
Table 2
Data in groups of adolescents
JHS (age, 13-15 y) SHS (age, 16-18 y) P Urban, n (%) 127 (27.1) 342 (72.9) Rural, n (%) 46 (35.1) 85 (64.9) Causes U/R b .001 Motorcycle 14/25 149/53 Bicycle 9/6 10/4 Walk 18/3 14/1 Patterns, U/R .057 Skull fracture 20/6 55/12 Swelling 22/5 45/2 ICHs 23/10 95/19 Severity, U/R .111 GCS 3-8 8/3 22/10 GCS 9-12 6/6 19/6 GCS 13-15 113/37 301/69 Outcome U/R .170 Dead 4/2 9/5 Vegetative 1/1 2/2 Dependent 3/2 4/5 Independent 8/5 17/3 Good 115/38 306/68 Craniotomy, U/R 16/7 18/13 b .001 Length of stay, U/R (d) 5.19/9.82 7.62/7.78 b .001
Fig. 2). The difference in patterns of injury between both areas was statistically significant ( P = .011). In the JHS and SHS groups in the urban area, the patterns of injury were as follows: 20 (15.7%) and 55 (16.1%) with skull fracture, 22 (17.3%) and 45 (13.2%) with brain swelling, and 23 (18.1%) and 95 (27.7%) with ICHs, respectively. In the rural area, the patterns in the JHS and SHS groups were as follows: 6 (13%) and 12 (14.1%) with skull fracture, 5 (10.9%) and 2 (2.4%) with brain swelling, and 10 (21.7%) and 19 (22.4%) with ICHs, respectively. The differences of injury patterns between the urban and rural areas in the groups were marginally significant ( P = .057) (Table 2). 3.3. Associated injuries
There were 59 (46.5%) cases in the JHS and 198 (57.9%) cases in the SHS group in the urban area, and 19 (41.3%) cases in the JHS and 45 (52.9%) cases in the SHS group in the rural area sustaining associated injuries ( P = .437). Cervical spine injuries were found in 1 case in the JHS and 2 cases in the SHS group in the urban area (0.6%), as well as in 2 cases in the JHS group in the rural area (1.5%). 3.4. Severity of injury (GCS) and outcomes (GOS)
During the study period, there were 30 severe, 25 mod-erate, and 414 mild head injuries reported in the urban area, and 13 severe, 12 moderate, and 106 mild head injuries in
the rural area ( P = .184) (Table 1). The outcomes at
discharge were as follows: dead, 13 cases; vegetative, 3; dependent, 7; independent, 25; and good recovery, 421 in the urban area, and dead, 7 cases; vegetative, 3; dependent, 7; independent, 8; and good recovery, 106 in the rural area. The outcomes in the urban and rural areas were
signifi-cantly different ( P = .032) (Table 1). The initial GCS
scores and outcomes in both areas had a significant correlation (higher GCS scores had better outcomes) ( P b .001) (Table 1 and Fig. 3).
3.5. Age and GCS/GOS
In the urban area, there were 8 (6.3%) severe, 6 (4.7%) moderate, and 113 (89%) mild head injuries in the JHS group, and 22 (6.5%) severe, 19 (5.5%) moderate, and 301 (88.%) mild head injuries in the SHS group. In the rural area, 3 (6.5%) severe, 6 (13%) moderate, and 37 (80.4%) mild head injuries were found in the JHS group, and 10 (11.8%) severe, 6 (7.1%) moderate, and 69 (81.2%) mild head injuries in the SHS group. The severities in the groups of urban and rural areas were not statistically different ( P = .111) (Table 2).
In the urban area, the outcomes were as follows: dead, 4 cases; vegetative, 1; dependent, 3; independent, 8; and good recovery, 115 in the JHS group, and dead, 9 cases; vegetative, 2; dependent, 4; independent, 17; and good recovery, 306 in the SHS group. In the rural area, the outcomes were as follows: dead, 2 cases; vegetative, 1; dependent, 2; independent, 5; and good recovery, 38 in the JHS group, and dead, 5 cases; vegetative, 2; dependent, 5; independent, 3; and good recovery, 68 in the SHS group. The outcomes of the groups in both areas were not statistically different ( P = .170) (Table 2).
3.6. Craniotomy and hospital stay
There were 34 cases (7.2%; 16 cases in JHS and 18 in SHS) in the urban area and 20 cases (15.3%, 7 cases in JHS and 13 in SHS) in the rural area who underwent craniotomy during the study period ( P b .011) (Tables 1 and 2). The mean length of hospital stay in the urban area was 5.19 days in the JHS group and 7.62 days in the SHS group. In the rural area, the mean length was 9.82 days in the JHS group and 7.78 days in the SHS group ( P b .001) (Table 2). 4. Discussion
The head injury rate in Taiwan is still very high
[9,12,20]. It was reported that the incidence rate was near Fig. 2. Patterns of head injury in urban and rural areas. Lesions were more
in urban areas and ICHs were the most prevalent lesions.
Fig. 3. Severity of head injury classified by GCS (severe, moderate, mild) and outcomes measured by GOS in urban (U) and rural (R) areas. The outcome was significantly affected by the severity of injury.
2-fold higher in the rural area than in the urban area
[3,9,12,20]. After the enactment of preventive policies, the incidence rate and mortality from head injury decreased in various countries [3,15,21]. Therefore, we conducted this study to examine the head injury rate of adolescents in both urban and rural areas in Taiwan after the helmet use law was enforced. The accurate incidence rates of head injuries in this study could not be calculated because a suitable denominator (the size of the study population) was not available during the study period. However, by a rough estimation, the adolescents in the rural area had a higher incidence rate than those in the urban area (data not shown). This estimation is consistent with the report of Woodward et al[21]. We also found that males had more head injuries than females, a finding similar to the results of other studies
[2,3,6,9,12,13,22].
4.1. Cause and pattern of injury
Traffic accidents are the leading cause of head injury
[2,4,6,9,22], and motorcycle-related injury is the major etiology [5,7,9,12,13]. In this study, motorcycle-related injury was the principal etiology for head injury in both groups of the rural area and in the SHS group of the urban area. In the JHS group of the urban area, nontraffic injury was the major cause of head injury.
Lesions were found more frequently in the urban (55.5%) than in the rural (44%) area. Skull fracture and impaired consciousness were important indices in determining the risk of developing surgically significant intracranial hema-tomas[1,8]. ICHs were the major pattern of injury in both areas (Table 1andFig. 2). In the urban area, the SHS group had more ICHs than the JHS group (Table 2). More injuries with ICHs indicated that the higher severity of injury was caused by motorcycles in the SHS group.
4.2. Associated injuries
There were more associated injuries among the SHS than in the JHS groups in both areas, although not statistically significant. It could be due to more motorcycle-related injuries in the SHS group. According to the results of Chiu et al[3], the incidence rate of associated injuries decreased dramatically after the helmet use law was enforced (from
64.2%-72.2% to 41.3%-57.9%) [3]. In this study, cervical
spine injury was found in only a few cases of the JHS groups in both areas. The incidence of cervical spine injury was also found to decrease in adolescents after the implementation of the helmet use law (from 2.6%-3.6% to 0.6%-1.5%)[3].
4.3. Severity (GCS) and outcomes (GOS)
There were more mild head injuries than severe ones in both urban and rural areas, although not statistically significant (Tables 1 and 2). The SHS groups in both areas had more cases with severe head injuries (Table 2)[22]. The distributions of injury severity in the urban and rural areas were similar to those of other studies[9,12,13,18].
The outcomes at discharge were significantly different between the urban and rural areas ( P = .032) (Table 1). The initial GCS scores and outcomes in both areas were also different (Table 1 and Fig. 3). The outcome was signifi-cantly affected by the injury severity. Education on helmet use, input of neurosurgical staff, and facility and emergency medical transportation service of patients with head injury were crucial for head injury and control in rural areas
[2,9,12,20].
4.4. Operation and hospital stay
It is reported that the incidence of neurosurgical intervention in head injury ranges between 2.5% and 23.7% [2,3,14,22]. In this study, craniotomy in the rural group was more than 2-fold higher than that in the urban group (15.3% vs 7.2%). The length of hospital stay was longer in the rural group (7.78-9.82 days) than in the urban
group (5.19-7.62 days) [21]. The mean length of hospital
stay was 10.2 days before the enforcement of helmet use law in Taiwan and 8.7 days thereafter[3].
In both urban and rural areas, the referral pattern was the same and basically followed the criteria of neurosurgical consultation and admission proposed previously. However, because of the shortage of neurosurgeons in rural areas and longer distance of transportation, the outcomes may not be related to the referral pattern.
4.5. Study limitations
The exact incidence rates of head injuries in the study populations could not be derived. We used the tertiary hospital–based data, which might not reflect the overall head injury distributions in the study areas. Tertiary hospitals usually receive more seriously head injured patients referred from surrounding subsidiary hospitals[16]. Craniotomy was done more frequently in the rural group (urban, 7.2%; rural, 15.3%); even more severity was found in the urban group. The different numbers of subtypes of intracranial hemorrhages (acute EDH, SDH, contusion ICH) will result in different incidence of craniotomy between the 2 groups. In the urban group, quality of intensive care, medical and nursing staff, and the distribution of facilities may be the major factors resulting in fewer borderline craniotomies, on which lie difficulties in decision making. 4.6. Preventive strategies
The enactment of compulsory helmet and seat belt use laws has led to a decrease in head injuries and change in injury patterns worldwide [3,17,18]. The preventive strate-gies should be tailored to different age groups with diverse causes. The helmet use law for motorcyclists should be strongly enforced in the SHS age group in both the urban and rural areas. Regulations for bicycle helmet use and pedestrian traffic rules should be enacted, especially for the JHS groups in both areas. Adolescents are at increased risk especially for nontraffic injuries in the urban area. Urban factors associated with elevated injury rate include high
traffic volume, frequency of walking, and paucity of off-street areas[6]. Community interventions, such as creation of safe playgrounds, traffic engineering improvement, traffic safety education, and supervision of activities for off-school time, may be effective in preventing traffic injuries in adolescents[6].
5. Conclusions
The difference in causes, patterns, and outcomes of head injury between the 2 age groups of adolescents disclosed the clinical significance of subdivision in adolescents into JHS and SHS groups. Continuing studies, enhanced community interventions, and additional preventive strategies are clearly needed.
Acknowledgments
This study was supported by research grants DOH94-TD-B-111-002 from the Department of Health, Executive Yuan, Taiwan, NHRI-EX94-9106PN from the National Health Research Institute, NHRI-EX95-9106PN from the Topnotch Stroke Research Center Grant, Ministry of Education, the National Health Institute, and grant 94 MMH-TMU-18 from the Collaborative Research Foundation of Mackay Memorial Hospital and Taipei Medical University (Taipei, Taiwan). We gratefully acknowledge the contributions of the National Head Injury Program and the assistance of Ms Shu-Fen Chu in data collection for this study.
References
[1] Chan KH, Mann KS, Yue CP. The significance of skull fracture in acute traumatic intracranial hematomas in adolescents: a prospective study. J Neurosurg 1990;72:189 - 94.
[2] Chen CL, Wong MK. Head injuries in children and adolescents: treatment and outcome. J Formos Med Assoc 1995;94:S10-9. [3] Chiu WT, Kuo CY, Hung CC, et al. The effect of the Taiwan
motorcycle helmet law on head injuries. Am J Public Health 2000; 90:793 - 6.
[4] Dias MS, Lillis KA, Calvo C, et al. Management of accidental minor head injuries in children: a prospective outcomes study. J Neurosurg 2004;101:38 - 43.
[5] Ding SL, Wang JD, Chen KT. Estimation of case fatality rate and incidence rate of traffic injury in Taiwan—analysis of 4,329 victims at a medical center. J Formos Med Assoc 1993;92:S76 - S81.
[6] Durkin MS, Laraque D, Lubman I, et al. Epidemiology and prevention of traffic injuries to urban children and adolescents. Pediatrics 1999;103:e74 - e81.
[7] Ghahreman A, Bhasin V, Chaseling R, et al. Nonaccidental head injuries in children: a Sydney experience. J Neurosurg 2005;103:213 - 8. [8] Hung CC, Chiu WT, Lee LS, et al. Risk factors predicting surgically
significant intracranial hematomas in patients with head injuries. J Formos Med Assoc 1996;95:294 - 7.
[9] Hung CC, Chiu WT, Tsai JC, et al. Epidemiological study of head injury in Hualian County. J Formos Med Assoc 1991;90:1227 - 33. [10] Jennett B, Bond M. Assessment of outcome after severe brain
damage—a practical scale. Lancet 1975;1:480 - 4.
[11] Kraus JF, Black MA, Hessol N, et al. The incidence of acute brain injury and serious impairment in a defined population. Am J Epidemiol 1984;119:186 - 201.
[12] Lee LS, Shih YS, Chiu WT, et al. Epidemiologic study of head injuries in Taipei city, Taiwan. Chin Med J (Taipei) 1992;50:219 - 25. [13] Lee ST, Lui TN, Chang CN, et al. Review of head injury. Analysis of
10,000 cases. J Surg Assoc ROC 1989;22:400 - 6.
[14] Nestvold K, Lundar T, Blikra G, et al. Head injuries during one year in a central hospital in Norway: a prospective study. Neuroepidemiology 1988;7:134 - 44.
[15] Patel HC, Bouamra O, Woodford M, et al. Trends in head injury outcome from 1989 to 2003 and the effect of neurosurgical care: an observational study. Lancet 2005;366:1538 - 44.
[16] Phuenpathom N, Tiensuwan M, Ratanaleri S, et al. The changing pattern of head injury in Thailand. J Clin Neurosci 2000;7:223 - 5. [17] Servadei F, Begliomini C, Gardini E, et al. Effect of Italy’s motorcycle
helmet law on traumatic brain injuries. Inj Prev 2003;9:257 - 60. [18] Steudel WI, Cortbus F, Schwerdtfeger K. Epidemiology and
prevention of fatal head injuries in Germany—trends and the impact of the reunification. Acta Neurochir 2005;147:231 - 42.
[19] Teasdale G, Jennett B. Assessment of coma and impaired conscious-ness: a practical scale. Lancet 1974;2:81 - 4.
[20] Wang YC, P’eng TK, Yang DY, et al. Epidemiological study of head injuries in central Taiwan. Chin Med J (Taipei) 1995;55:50 - 7. [21] Woodward A, Dorsch MM, Simpson D. Head injuries in country and
city. A study of hospital separations in South Australia. Med J Aust 1984;141:13 - 7.
[22] Wu DM, Chiu WT, Hung CC. A study of head injury among teenagers. J Med Sci 1991;12:104 - 15.