Vertigo and Stroke: A National Database Survey
Leh-Kiong Huon MD,1 Ting-Chuan Wang MHA,2 Te-Yung Fang MD,1 Li-Ju Chuang MHA,3 Pa-Chun Wang MD, MSc1,3,4,5
Affiliations/Institutions
1Department of Otolaryngology, Cathay General Hospital, Taipei, Taiwan 2Department of Medical Research, Cathay General Hospital, Taipei, Taiwan 3Cathay Medical Research Institute, Taipei, Taiwan
4Fu Jen Catholic University School of Medicine, Taipei County, Taiwan
5Department of Public Health, College of Public Health, China Medical University, Taichung, Taiwan
Running title: Stroke and vertigo Manuscript classification: Article Word count: 2,465
Financial support: None Disclosure: None
Correspondence:
Pa-Chun Wang MD, MSc
Department of Otolaryngology, Cathay General Hospital 280, Sec 4. Jen-Ai Rd, 106 Taipei, Taiwan
Telephone: 8862-27082121 ext 3333 FAX: 8862-66362836
ABSTRACT
Objective: To investigate the association between vertigo and stroke in Taiwan using the Bureau of National Health Insurance (BNHI) research database.
Methods: Information on adult patients with an index vertigo attack in 2006 was retrieved from BNHI research database. Patients having vertigo with subsequent stroke during a 1-year follow-up period were identified. Risk factors for stroke were examined. Using 2 test, t test, and a multi-level logistic regression model, patients with vertigo were categorized into stroke and nonstroke groups for comparative analyses. An age- and sex- matched control cohort was prepared for comparison.
Results: Patients with vertigo (n=527,807) (mean age, 55.1 years) accounted for 3.1% of the general Taiwanese adult population. The prevalence of stroke among vertigo patients of 0.5% (mean age, 67.8 years) was slightly higher than control (0.3%, mean age 72.3 years;
P<.0001). The types of stroke were ischemic (66.7%), nontypical (29.0%), and hemorrhage
(4.3%). The prevalence of stroke increased with age (P<.001). Patients with vertigo had higher prevalence of co-morbid conditions (P<.0001); those with diabetes mellitus, hypertension, dyslipidemia, coronary artery disease, or atrial fibrillation had a higher prevalence of stroke (P<.001). Hypertension was the most significant predictor of stroke (OR, 3.77; 95% CI, 3.36-4.23; P<.001).
Conclusions: Patients with vertigo had higher chance to develop stroke than control. Some strokes may initially manifest as peripheral vertigo, and some central vertigo may eventually evolve into a stroke. Middle aged male, diabetes, hypertension, dyslipidemia, coronary artery disease, and atrial fibrillation are risk factors for subsequent stroke in vertigo patients.
Key words: vertigo, stroke, prevalence, recurrence, risk factor, National Healthcare Insurance
INTRODUCTION
Dizziness, vertigo, and imbalance are commonly reported by patients. The prevalence of vertigo among the general population is about 4.8% to 5.2%.1,2 Vertigo may arise from dysfunction of peripheral or central balance organs. Approximately 80% of vertigo cases result from peripheral causes; central vertigo encompasses more severe diseases, including migrainous vertigo, brainstem ischemia, cerebellar infarction, and intracranial hemorrhage.3 Community surveys show that 20% to 30% of the population may have experienced
symptoms of vertigo or dizziness in their lifetime.4-6
Stroke, or cerebrovascular accident, ranks third in disease morbidity and mortality and is a major public health burden that is responsible for a large proportion of disability
worldwide.7 The prevalence of stroke is estimated to be 0.5% to 1.6% among Taiwanese adults older than 36 years, making it the second leading cause of death (60 deaths per 1,000,000) after cancer.8,9 Cerebrovascular accident is the major cause of institutional living and loss of independence among adults, and the incidence is expected to rise among aging societies.
One-fifth of strokes occur in the posterior circulation, which supplies the brainstem and cerebellum, controls autonomic brain function and coordination, and originates from the vertebrobasilar arteries. Vertigo is a common clinical presentation with brainstem or cerebellar strokes, accounting for 2.1% of initial cerebrovascular accident symptoms.10 Cerebellar stroke may manifest as isolated vertigo, mimicking benign peripheral vestibular disorder, particularly at the onset of the disease. Studies have shown that isolated vertigo without other neurological symptoms can occur in 19% of patients with cerebellar stroke and
in 62% of patients with vertebrobasilar insufficiency,11 suggesting that some vertigo may indeed be caused by transient ischemia within the posterior circulation.11
Posterior circulation strokes and central vertigo may have a similar pathogenesis. It is hypothesized that some strokes may initially be misdiagnosed as peripheral vertigo and that some central vertigo may eventually evolve into a stroke. However, little is known about the association between vertigo and stroke.
Taiwan implemented its universal Bureau of National Health Insurance (NHI) program in 1995. To date, the NHI covers more than 97% of the population.12,13 The NHI has collected millions of claims that can be used for health care study. The NHI claims databases are now managed by Taiwan’s National Healthcare Research Institute and are open for academic research. Therefore, the NHI research database is a useful data source for epidemiology and medical utilization studies.
The objective of this study was to investigate the association between vertigo and stroke. Using the 2006 NHI research database, the aims of the study were (1) to report the
epidemiology of stroke among patients at 1 year following a vertigo attack and (2) to assess the effect of cardiovascular risk factors (age, sex, diabetes mellitus, hypertension,
METHODS
Data Sources
Data for this study were obtained from the NHI research database. Claims data from January to December 2006 were used. The database contains the following information: outpatient health expenditures, outpatient orders, admission health expenditures, and
admission orders. The database uses diagnostic codes from the International Classification of
Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). Population data were retrieved
from a registry for beneficiaries of the NHI. The study was approved by the institutional review board of the Cathay General Hospital.
Study Population and Study Design
The study used the following inclusion criteria and definitions of terms for data
management. Patient 18 years or older were available for inclusion in the study. Prevalence was defined as the proportion of the population with an existing disease during a 1-year period. Vertigo was identified by the presence of the following ICD-9-CM codes: 078.81, 386.00 to 386.9 (including 386.0, 386.00-386.04, 386.1, 386.10-386.12, 386.19, 386.2, 386.3, 386.30-386.35, 386.4, 386.40-386.43, 386.48, 386.5, 386.50-386.56, 386.58, 386.8, and 386.9), or 780.4. The index attack was defined as the first attack of vertigo occurring in 2006; Patients with stroke attack within 1 years prior to 2006 were excluded from this study. (10,296 patients were excluded). Each patient was tracked from the index attack for at least a 12-month follow-up period to identify all patients who had any type of stroke (ICD-9-CM codes 430-438). Stroke among patients was confirmed by imaging (NHI procedure codes
33067B, 33068B, and 33069B for brain computed tomography, or 33084B and 33085B for brain magnetic resonance imaging) and by hospitalization.
A age- and sex- matched control cohort (5:1 randomly sampled 2006 claim data from Taiwan’s 23 million population) was prepared for comparison.
Previous investigations established positive associations between the occurrence of stroke and age, sex, hypertension, diabetes, coronary artery disease, dyslipidemia, and atrial
fibrillation.14 Therefore, these comorbidities were considered in our study. Medical comorbidities were identified by diagnosis codes from medical records at the index ambulatory care visits.
Patients with vertigo were categorized into stroke and nonstroke groups for comparative analyses. The stroke group comprised patients with vertigo who experienced a stroke during a 1-year follow-up period after the index vertigo attack.
Statistical Analysis
In this study, we used descriptive statistical analyses (frequencies, percentages, and means [SDs]) to describe the characteristics and prevalence of stroke among the population with vertigo. We compared the prevalence of stroke using 2 test. Continuous variables were compared using unpaired t test. We used a multi-level logistic regression model to assess the independent effects of age, sex, diabetes, hypertension, dyslipidemia, coronary artery disease, and atrial fibrillation on the risk of stroke. All P values used in these tests were 2-tailed, with
RESULTS
General Demographics and Prevalence of Vertigo
The NHI beneficiary population 18 year or older in Taiwan comprised 16,838,659 patients in 2006 (>96% of the total population was covered). In total, 527,807 patients experienced at least 1 episode of vertigo, with a ratio of men to women of 1:2
(178,192:349,615). The mean (SD) age of the patients was 55.1 (17.3) years. There were 931,238 episodes of vertigo, which generated 1,873,040 vertigo-related outpatient visits; 6,761 episodes of vertigo generated 7,070 admissions nationwide. The 527,807 patients with vertigo accounted for 3.1% (527,807 of 16,838,659) of the general adult population. The prevalence among the general population was equivalent to 3.1 cases of vertigo per 100 adults.
The control cohort comprised of 105,498 subjects, with a ratio of men to women of 1:1.7 (35,609:69,889). The mean (SD) age of the subjects was 55.05 (17.3).
Prevalence of Stroke
The prevalence of stroke among the population with vertigo was 0.5 cases per 100 adults with vertigo, with a case number ratio of men to women of 1:1 (1184:1173). The mean (SD) age of the patients with stroke was 67.8 (12.1) years.
Ischemic stroke (66.7%) was the most common type of stroke among the patients with vertigo. It was followed by nontypical stroke (29.0%) and hemorrhagic stroke (4.3%).
The prevalence of stroke among the control population with vertigo was 0.3 cases per 1000 adults, with a case number ratio of men to women of 1:1.1 (152:167). The mean (SD) age of the patients with stroke was 72.3 (10.1) years.
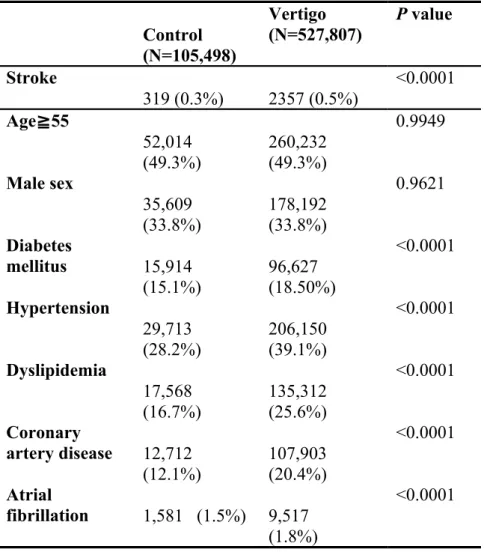
There was significance difference in the prevalence of stroke between vertigo patients and control cohort. (0.5% vs. 0.3%, P<0.0001, 2 test) The prevalence(s) of co-morbid conditions were higher in vertigo patients than the age- sex-matched control cohort. (Table 1).
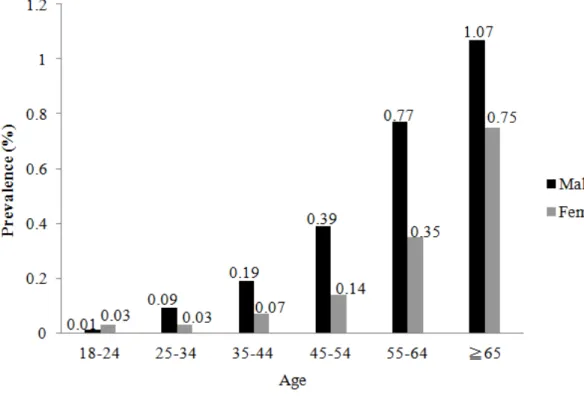
Effect of Sex
Women comprised 66.2% of the population with vertigo. The prevalence of vertigo was 2.2% among men and 4.0% among women. However, the prevalence of stroke among patients with vertigo was significantly higher in men (0.7% male [1184 of 178,192] vs 0.3% female [1173 of 349,615]; P<.001, 2 test) of all age groups. (Table 2, Figure 1).
Effect of Age
Patients were categorized into the following age groups: 18 to 24, 25 to 34, 35 to 44, 45 to 54, 55 to 64, and 65 years or older. The prevalence of stroke among adults with vertigo increased significantly with age (P<.001, 2 test) (Figure 1).
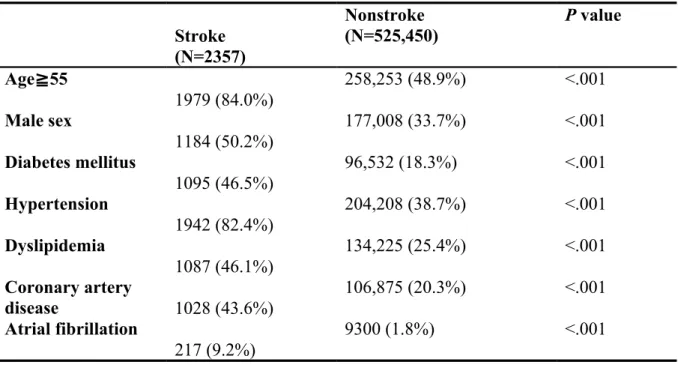
Effect of Risk Factors
hypertension, dyslipidemia, coronary artery disease, and atrial fibrillation, had various effects on the occurrence of stroke in patients with vertigo. These results are summarized in Table 3.
Among the population with vertigo, patients who had hypertension demonstrated a greater than 3-fold increased risk (odds ratio 3.77, 95% confidence interval 3.36-4.23) of developing stroke compared with those who did not have hypertension. The association was also significant in patients with diabetes, dyslipidemia, coronary artery disease, or atrial fibrillation (Table 3).
DISCUSSION
This study reports the probability of stroke occurrence among Taiwanese patients with vertigo in the short term. We found that patients with vertigo accounted for 3.1% (527,807 of 16,838,659) of the general adult population of Taiwan. The prevalence of vertigo was
equivalent to 3.1 cases per 100 adults. Point 5 percent of vertigo patients would experience a stroke within 1 year following the index vertigo attack; the prevalence was slightly higher than population control. Our results demonstrate that the experience of episodic vertigo, along with additional risk factors (such as age, sex, diabetes, hypertension, dyslipidemia, and atrial fibrillation), may predispose a patient to the occurrence of stroke. Control of associated comorbid conditions may be an important strategy to prevent patients with vertigo from developing stroke.
The mechanism by which vertigo may lead to stroke is unclear. The following are 2 potential scenarios: First, a stroke event can have clinical features that mimic a vertigo attack. Episodic vertigo frequently occurs in patients experiencing ischemia in the distribution of the vertebro-basilar circulation. It may occur in isolation, in conjunction with other symptoms of vertebro-basilar insufficiency, or with persisting symptoms and signs of infarction of the brainstem and cerebellum.10,11 Because the inner ear is supplied by the vertebro-basilar circulation, inner ear symptoms are common with ischemia in this distribution. The labyrinth may be selectively vulnerable because it represents an end circulation with minimal
collaterals.15 Isolated episodic vertigo, with or without auditory symptoms, may be the only manifestation of transient ischemia within the vertebro-basilar circulation. Isolated episodic vertigo may particularly occur when there is stenosis of the caudal or middle portion of the basilar artery (presumably close to the antero-inferior cerebellar artery origin). Most strokes
following vertigo were ischemic (66.7%). The inner ear ischemia theory for the pathogenesis of vertigo may be partially explained by our findings. However, it is still unclear whether isolated episodic vertigo originates from the brainstem or from the inner ear.
Second, vertigo and stroke may have occurred remotely in time, in which case vertigo might be a necessary coexisting factor but not a sufficient single cause of stroke. Most ischemic stroke cases in our study were examples of this second scenario. It may be that other risk factors for stroke interact to affect the pathogenesis of vertigo; this can be attested by the higher prevalence(s) of co-morbid conditions among vertigo patients. (Table 1)
The Framingham Study in the United States, a prospective epidemiological study on chronic disease since 1948, elucidated that risk factors for stroke include age, the use of antihypertensive agents, elevated systolic blood pressure, diabetes, smoking, cardiovascular disease, atrial fibrillation, and left ventricular hypertrophy.7,14,16 In the present study, the risk profile from the Framingham Study provided substantial predictive power for the risk of stroke among patients with vertigo (P<.001) (Table 2). It is noteworthy that the risk of stroke among patients with vertigo who had hypertension was approximately 3.77 times (95% CI, 3.36-4.28) higher than that among those who did not have hypertension (P<.001). Therefore, more aggressive interventions are needed to decrease blood pressure in patients with vertigo to reduce the risk of stroke.
Previously reported prevalences and incidences of vertigo were higher among women than among men.17,18 The data herein attest to a predominance of vertigo among women. However, evidence shows that the mean 10-year age-adjusted probability of stroke is higher among men,16 which is also applicable to patients with vertigo according to our results herein.
(Figure 1)
In this study, the risk of stroke among patients with vertigo increased gradually with age, but the odds of stroke occurrence may vary between men and women in association with aging. Among patients younger than 55 years, the stroke risk among men was approximately 3-fold higher than that among women (Figure 1). Among those 55 years or older, the odds gradually decreased from 2.2 (0.77 for men vs 0.35 for women in the group aged 55-64 years) to 1.4 (1.07 for men vs 0.75 for women in the group aged ≥65 years). The increased risk of stroke among female patients with vertigo may be attributed to the menopausal metabolic syndrome,19 characterized by high systolic blood pressure, weight gain, lipid profile changes, insulin resistance, endothelial dysfunction, and elevated coagulation factors. Estrogen deficiency becomes evident in women after menopause, which may predispose them to an unfavorable risk profile for stroke.
Our data suggest that patients with vertigo and cardiovascular comorbidities are at increased risk of subsequent stroke, even in the short term. Clinicians should maintain vigilance among middle-aged patients with vertigo to modify risk factors for stroke, such as diabetes, hypertension, dyslipidemia, coronary artery disease, and atrial fibrillation.7,14
There are several limitations to our study. The NHI research database is a useful data source to provide epidemiological information on stroke following a vertigo attack. However, the data set contains no clinical or disease severity information. The accuracy of diagnosis coding by health care providers may affect the validity of the data, although the NHI has adopted several measures to cross-check and monitor the accuracy. We found that most providers were unable to accurately differentiate an actual diagnosis of vertigo at the index
visit. The prevalence of Meniere disease, benign paroxysmal positional vertigo, or vestibular neuritis cannot be estimated from our study findings. However, imaging-confirmed and hospitalized patients with a principal diagnosis of stroke were chosen to reduce misdiagnosis. Some cardiovascular risk factors, such as tobacco use, dietary habits, body mass index, blood glucose level, and blood pressure, were unavailable in the database.16
In conclusion, limited epidemiological data are available in the literature about the association between vertigo and stroke. Our data confirmed that, 0.5% of patients with vertigo may experience a stroke within 1 year; the prevalence was higher than age- and sex- matched general adult population. Some strokes may initially manifest as peripheral vertigo, and some central vertigo may eventually evolve into a stroke. Middle age, male sex, diabetes, hypertension, dyslipidemia, coronary artery disease, and atrial fibrillation are risk factors for subsequent stroke in patients with vertigo that should warrant long-term medical attention.
ACKNOWLEDGMENT
This study is based in part on data from the National Health Insurance research database provided by the Bureau of National Health Insurance, Department of Health, and managed by the National Health Research Institutes. The interpretation and conclusions herein do not represent those of the Bureau of National Health Insurance, Department of Health, or National Health Research Institutes of Taiwan, Republic of China.
REFERENCES
1. Neuhauser HK, von Brevern M, Radtke A, et al. Epidemiology of vestibular vertigo: a neurotologic survey of the general population. Neurology 2005;65:898-904.
2. Neuhauser HK, Radtke A, von Brevern M, et al. Burden of dizziness and vertigo in the community. Arch Intern Med 2008;168:2118-24.
3. Kroenke K, Hoffman RM, Einstadter D. How common are various causes of dizziness?
South Med J 2000;93:160-7.
4. Kroenke K, Price RK. Symptoms in the community: prevalence, classification, and psychiatric comorbidity. Arch Intern Med 1993;153:2474-80.
5. Yardley L, Owen N, Nazareth I, et al. Prevalence and presentation of dizziness in a general practice community sample of working age people. Br J Gen Pract 1998;48:1131-5.
6. Hannaford PC, Simpson JA, Bisset AF, et al. The prevalence of ear, nose and throat problems in the community: results from a national cross-sectional postal survey in Scotland.
Fam Pract 2005;22:227-33.
7. Gorelick PB, Sacco RL, Smith DB, et al. Prevention of a first stroke: a review of
guidelines and a multidisciplinary consensus statement from the National Stroke Association.
JAMA 1999;281:1112-20.
8. Lee TH, Hsu WC, Chen CJ, et al. Etiologic study of young ischemic stroke in Taiwan.
Stroke 2002;33:1950-5.
9. Liu HM, Tu YK, Yip PK, et al. Evaluation of intracranial and extracranial carotid steno-occlusive diseases in Taiwan Chinese patients with MR angiography: preliminary experience.
Stroke 1996;27:650-3.
10. Rathore SS, Hinn AR, Cooper LS, et al. Characterization of incident stroke signs and symptoms: findings from the atherosclerosis risk in communities Study. Stroke
11. Moubayed SP, Saliba I. Vertebrobasilar insufficiency presenting as isolated positional vertigo or dizziness: a double-blind retrospective cohort study. Laryngoscope 2009;119:2071-6.
12. Cheng TM. Taiwan’s new National Health Insurance program: genesis and experience so far. Health Aff (Millwood) 2003;22:61-76.
13. Lu JF, Hsiao WC. Does universal health insurance make health care unaffordable? lessons from Taiwan. Health Aff (Millwood) 2003;22:77-88.
14. Straus SE, Majumdar SR, McAlister FA. New evidence for stroke prevention: scientific review. JAMA 2002;288:1388-95.
15. Lee H, Sohn SI, Cho YW, et al. Cerebellar infarction presenting isolated vertigo: frequency and vascular topographical patterns. Neurology 2006;67:1178-83.
16. D’Agostino RB, Wolf PA, Belanger AJ, et al. Stroke risk profile: adjustment for antihypertensive medication: the Framingham Study. Stroke 1994;25:40-3.
17. Neuhauser HK. Epidemiology of vertigo. Curr Opin Neurol 2007;20:40-6.
18. Guilemany JM, Martínez P, Prades E, et al. Clinical and epidemiological study of vertigo at an outpatient clinic. Acta Otolaryngol 2004;124:49-52.
19. Spencer CP, Godsland IF, Stevenson JC. Is there a menopausal metabolic syndrome?
FIGURE LEGENDS
TABLES AND FIGURES
Table 1. Prevalence of Stroke and Risk Factors in Control and Vertigo Cohorts Control (N=105,498) Vertigo (N=527,807) P value Stroke 319 (0.3%) 2357 (0.5%) <0.0001 Age≧55 52,014 (49.3%) 260,232 (49.3%) 0.9949 Male sex 35,609 (33.8%) 178,192 (33.8%) 0.9621 Diabetes mellitus 15,914 (15.1%) 96,627 (18.50%) <0.0001 Hypertension 29,713 (28.2%) 206,150 (39.1%) <0.0001 Dyslipidemia 17,568 (16.7%) 135,312 (25.6%) <0.0001 Coronary artery disease 12,712 (12.1%) 107,903 (20.4%) <0.0001 Atrial fibrillation 1,581 (1.5%) 9,517 (1.8%) <0.0001
Table 2. Prevalence of risk factors among patients having vertigo with or without stroke. Stroke (N=2357) Nonstroke (N=525,450) P value Age≧55 1979 (84.0%) 258,253 (48.9%) <.001 Male sex 1184 (50.2%) 177,008 (33.7%) <.001 Diabetes mellitus 1095 (46.5%) 96,532 (18.3%) <.001 Hypertension 1942 (82.4%) 204,208 (38.7%) <.001 Dyslipidemia 1087 (46.1%) 134,225 (25.4%) <.001 Coronary artery disease 1028 (43.6%) 106,875 (20.3%) <.001 Atrial fibrillation 217 (9.2%) 9300 (1.8%) <.001
Table 3. Regression analysis predicting the risk of stroke among patients with vertigo. Odds Ratio 95% CI P value Age≧55 2.22 1.98-2.50 <.001 Male sex 1.78 1.64-1.93 <.001 Diabetes mellitus 1.95 1.79-2.13 <.001 Hypertension 3.77 3.36-4.23 <.001 Dyslipidemia 1.36 1.25-1.48 <.001
Coronary artery disease 1.30 1.12-1.41 <.001 Atrial fibrillation 2.71 2.35-3.14 <.001