O R I G I N A L A R T I C L E
Association between
polypharmacy and dementia in
older people: A population-based
case–control study in Taiwan
ggi_800 1..8Shih-Wei Lai,1,3* Chih-Hsueh Lin,1,3* Kuan-Fu Liao,6,8Li-Ting Su,4,5 Fung-Chang Sung2,5and Cheng-Chieh Lin1,3,7
1School of Medicine, and2Department of Public Health, China Medical University,3Department of
Family Medicine,4Trauma and Emergency Center and5Management Office for Health Data, China
Medical University Hospital,6Department of Internal Medicine, Taichung Tzu Chi General Hospital,
and7Department of Health Care Administration, College of Health Science, Asia University, Taichung,
and8School of Medicine, Tzu Chi University, Hualien, Taiwan
Aim: The aim of the present study was to investigate whether polypharmacy correlates
with the risk of dementia in older people.
Methods: From representative claims data established from the National Health
Insur-ance with a population coverage rate of 99% in Taiwan, we identified 7135 newly diag-nosed patients with dementia in 2000–2008 and 2 8540 randomly selected controls
without dementia, both aged 365 years. The daily use of prescribed drugs in the past
2 years was compared between cases and controls, controlling for demographic characters and comorbidities.
Results: The incidence of dementia increased with the number of medications used and
age. Cases were older than controls, predominant with women and more likely to use five or more drugs daily (44.0% vs 32.0%, P< 0.0001). Multivariate logistic regression analysis showed that, compared with participants using zero to one drug, the odds ratios (OR) of dementia were 1.28 (95% confidence interval [CI] 1.18–1.38) for those using two to four drugs, 1.34 (95% CI 1.23–1.46) for those using five to nine drugs and 1.56 (95% CI 1.38–1.76) for those using 10 or more drugs. Cerebrovascular disease (OR 3.19), diabetes mellitus (OR 1.23), chronic kidney disease (OR 1.21) and hypertension (OR 1.08) were significant comorbidities predicting the risk of dementia. There was significant interaction between cerebrovascular disease and the number of medications used in the dementia risk.
Conclusions: The risk of dementia increases steadily with the number of medications
used and age in older people in Taiwan. Cerebrovascular disease, diabetes mellitus, chronic kidney disease and hypertension might also correlate with the risk of dementia.
Geriatr Gerontol Int 2011; ••: ••–••.
Keywords: cerebrovascular disease, chronic kidney disease, dementia, diabetes mellitus,
polypharmacy.
Introduction
Polypharmacy, concurrently with multiple medications, is a well-established risk factor for adverse drug reactions (ADR) in older people.1,2 Larson et al. found
a significant association between the number of
Accepted for publication 15 November 2011.
Correspondence: Professor Fung-Chang Sung PhD MPH, China Medical University College of Public Health, 91 Hsueh-Shih Road, Taichung 404, Taiwan. Email: fcsung1008@yahoo.com
medications used and ADR.1Compared with patients
using zero to one drug, the relative odds of ADR increased from 2.7 (95% CI 0.9–7.8) for patients using two to three drugs, to 13.7 (95% CI 3.6–51.9) for those
using six or more drugs.1 du Souich has reported
that serious ADR is an issue secondary to drug–drug interactions frequently found in older people with polypharmacy.3
The population aged 365 years in Taiwan increased
from 7.0% in 1993 to 10.4% in 2008.4Previous studies
have shown that the prevalence of dementia ranged
from 2.5 to 4.4% among older people in Taiwan.5–7
Dementia is regarded as a growing public health issue that causes a great socioeconomic burden as a result of the high cost of care and the negative impact on quality of life.8–11
Although the pathogenesis of dementia remains unclear, some epidemiological studies have shown that the ADR account for 2–12% of dementia-like cases.1,12,13As polypharmacy is a well-known risk factor
for ADR in older people, and ADR can lead to dementia-like status, we make a hypothesis that older people with polypharmacy might be at an elevated risk of dementia.
To our knowledge, the clinical association between polypharmacy and dementia using a population-based study has not yet been investigated for an Asian popu-lation. In the present study, we used the claims data of the National Health Insurance of Taiwan to investigate the relationship between polypharmacy and dementia in older people.
Materials and methods
Study population
This was a population-based case–control study using data from the Taiwan National Health Insurance Data-base. This insurance program began in March 1995 and has covered more than 99% of the entire population of 23 million people in Taiwan by the end of 2008.14
We obtained the claims data of 1996–2008 from the National Health Research Institutes in Taiwan, consist-ing of registries and claims reported by contracted health-care providers. The insurance program details were addressed in previous studies.15–17
Criteria and definition
Individuals aged 65 years and older with newly diag-nosed dementia in outpatient clinics in 2000–2008 were identified as cases, according to International Classifi-cation of Diseases 9th Revision Clinical ModifiClassifi-cation (ICD-9 290.0, 290.1, 290.2, 290.3, 290.4, 294.1 and 331.0). Controls were also aged 65 years and older, ran-domly selected from those without dementia in a ratio of 1 : 4 (cases vs controls). Individuals with other major
psychiatric diseases (ICD-9 291–293 and 295–298) were excluded from the present study. The other medical conditions potentially associated with dementia were included as covariates, such as obesity (ICD-9 278.00 and 278.01), diabetes mellitus (ICD-9 250), hyperten-sion 9 401-405), cerebrovascular disease (ICD-9 430–438), hyperlipidemia (ICD-(ICD-9 272.0, 272.1, 272.2, 272.3 and 272.4) and chronic kidney disease (ICD-9 585, 586, 588.8 and 588.(ICD-9).
We collected each study subject’s medication history for 2 years before the date at which the subject was identified. We estimated the average daily use of scribed drugs by calculating the total number of pre-scribed drugs in 2 years divided by 730 days. The prescribed drugs included oral, topical and injection medicines. The following was the estimating equation: The average daily use of prescribed drugs = {[(1 type of
drug) ¥ (using days)] + [(2 types of drug) ¥ (using
days)] + [(3 types of drug) ¥ (using days)] + [(4 types of drug) ¥ (using days)] + [(5 types of drug) ¥ (using days) + . . . + [(10 or more types of drug) ¥ (using days)]} / 730 days.15We have previously defined the daily
average use of five or more drugs as polypharmacy.15
Statistical analysis
Data analysis first calculated the incidence rates of dementia by the number of medications used and age group (65–74 years, 75–84 years, and 85 years and older), and followed by cases and controls comparison. Distributions of dementia and several types of comor-bidities were presented by the number of medications. We also carried out the receiver–operator characteristic analysis and presented a plot. Cases and controls were compared for demographic status, number of medica-tions used and comorbidities, and tested with the c2-test. Univariate unconditional logistic regression
analysis was applied to calculate the crude odds ratios (OR) and 95% confidence intervals (CI) for the associa-tion between potential risk factors and dementia. Sig-nificant factors found in the univariate analysis were included in the multivariate unconditional logistic regression analysis. Further analysis measured the inter-action between cerebrovascular disease and the number of medications associated with the risk of dementia. We used SAS software (version 9.1, SAS Institute, Cary, NC, USA) to analyze data with a two-sided test signifi-cance level of 0.05.
Ethical approval
All identifications in the insurance reimbursement claims data were scrambled to secure patient privacy for public access. The present study was exempt from full review by the institution review board.
Results
Retrospective characteristics of the study population
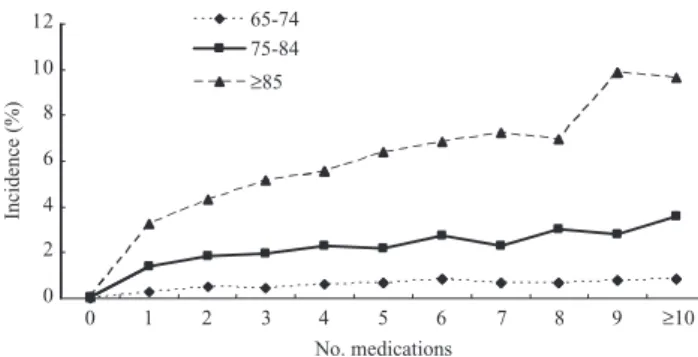
We identified 7135 newly diagnosed cases of dementia from the sub-dataset of insurance claims in 2000–2008. Figure 1 shows the distribution of average annual inci-dence of dementia markedly increased with age and the number of medications in three age groups (65– 74 years, 75–84 years and >85 years). The incidence rates among those using five drugs were 0.7%, 2.16% and 6.39%, respectively. Among subjects aged 85 years and older, the incidence of dementia increased from 3.27% for those using one drug to as high as 9.65% for those using 10 or more drugs.
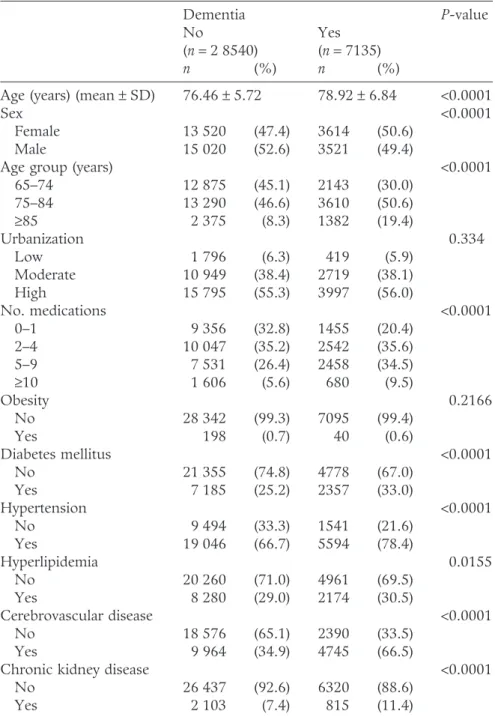
Table 1 compares the distribution of demographic characteristics, medications and other medical condi-tions between dementia cases and controls. Cases had a higher proportion of women and were older than
con-trols (both P< 0.0001). Dementia cases were more
prevalent with comorbidities than controls, including diabetes, hypertension, hyperlipidemia, cerebrovascular disease and chronic kidney disease. More than half of the study subjects lived in urbanized areas with no sta-tistical difference in population densities between cases and controls (P = 0.334).
The proportion of polypharmacy (35 drugs) was sig-nificantly higher in dementia cases (44.0%) than in con-trols (32.0%) (P< 0.001; Table 2). Compared with the first year, polypharmacy users increased by 5.6% in the dementia cases and 2.8% in the controls in the second year (data not shown). Subjects with obesity, diabetes, hypertension, hyperlipidemia, cerebrovascular disease or chronic kidney disease also were more likely to be polypharmacy users than subjects without those respec-tive diseases (P< 0.0001).
Estimated risk of dementia and associated factors
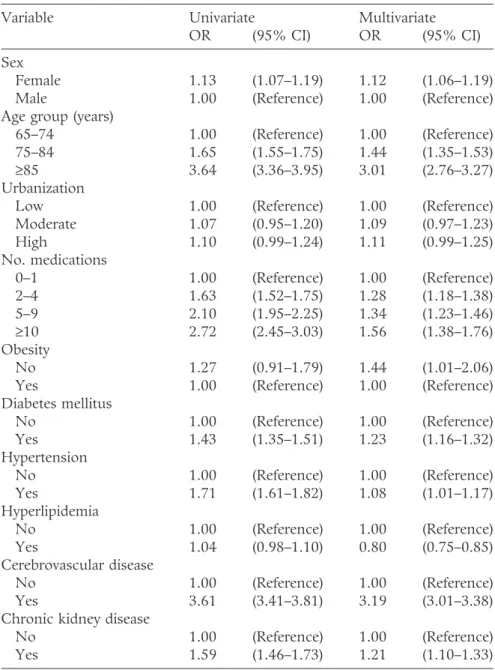
Table 3 shows the multivariate unconditional logistic regression analysis for the risk of dementia associated
with sex, age, number of medications, obesity, diabetes, hypertension, hyperlipidemia, cerebrovascular disease and chronic kidney disease. The risk of dementia increased with age. Women were at higher risk than men to be associated with dementia. Cerebrovascular disease (OR 3.19, 95% CI 3.01–3.38), diabetes mellitus (OR 1.23, 95% CI 1.16–1.32), chronic kidney disease (OR 1.21, 95% CI 1.10–1.33) and hypertension (OR 1.08, 95% CI 1.01–1.17) were independent comorbidi-ties significantly associated with dementia. There was an obvious relationship between number of medications and dementia. When compared with subjects using zero to one drug, the adjusted OR of dementia were 1.28 (95% CI 1.18–1.38) for subjects using two to four drugs, 1.34 (95% CI 1.23–1.46) for those using five to nine drugs and 1.56 (95% CI 1.38–1.76) for those using 10 or more drugs. Further data analysis considered the number of medications as a continuous variable in the multivariate regression analysis. The results showed that per drug used increased 3% of dementia risk (OR = 1.03, 95% CI 1.02–1.04; data not shown).
Table 4 shows the synergistic interactions between cerebrovascular disease and the number of medications associated with dementia, using patients with zero to one drug, and with and without cerebrovascular disease separately as the reference group. The OR of dementia increased, from 1.12 (95% CI 1.01–1.25) for those with cerebrovascular disease and using two to four drugs, to 1.16 (95% CI 1.03–1.29) for those with cerebrovascular disease and using five to nine drugs, and 1.38 (95% CI 1.19–1.59) for those with cerebrovascular disease and using 10 or more drugs. Among patients without cere-brovascular disease, those taking multiple drugs had a greater risk of dementia. The OR increased from 1.41 (95% CI 1.26–1.57) for those taking two to four drugs, to 1.57 (95% CI 1.39–1.78) for those taking five to nine drugs, and 1.79 (95% CI 1.44–2.21) for those taking 10 drugs or more. However, the prevalence of demen-tia was much higher in patients with cerebrovascular disease than in those without the disease (32.3% vs 11.4%).
Discussion
Although the real cause of dementia remains to be explored, many known risk factors have been well inves-tigated. Meador suggests that, in addition to acute toxic effects, drugs might also act as the primary cause of
dementia.18 Studies have claimed that drug-induced
dementia accounts for 2–12% of all dementia cases.1,12,13
To date, there is still not a consensus definition for polypharmacy. Two available definitions for polyphar-macy have been addressed. The first one is the use of drugs not clinically indicated, representing unnecessary or inappropriate medications.19–21 The other definition
is the concurrent use of multiple drugs, but how many 10 12 65-74 75-84 6 8 ≥85 2 4 Incidence (%) 0 No. medications 0 1 2 3 4 5 6 7 8 9 ≥10
Figure 1 Age-specific rate of newly diagnosed dementia by
number of medications and age among population aged 65 years and older in Taiwan, 2000–2008.
drugs remains unsettled. Because of the natural limita-tions of a case–control study, recall bias of the number of medications used daily by each patient was possible. Therefore, we used a new equation to measure the average daily use of prescribed drugs by the subject,
which was designed in our previous study.15 In the
present study, the estimated risk of dementia increased markedly as the average daily number of medications increased. The OR of dementia were 1.28 for subjects using two to four drugs daily, 1.34 for subjects using five to nine drugs daily and 1.56 for subjects using 10 drugs
or more daily, compared with subjects using one drug or less (Table 3). Some other studies have defined the daily use of five or more drugs as polypharmacy.22–24
However, our analysis of the receiver–operator curve showed that dementia might significantly increase for those who took 2.86 drugs (data not shown). We further used patients taking zero to two drugs as a reference and found that OR of dementia were 1.12 for subjects using three to four drugs daily, 1.18 for subjects using five to nine drugs daily and 1.38 for subjects using 10 drugs or more daily.
Table 1 Comparison by sociodemographic factors and other medical
conditions between dementia cases and controls in Taiwan, 2000–2008
Dementia P-value
No Yes
(n = 2 8540) (n = 7135)
n (%) n (%)
Age (years) (mean1 SD) 76.461 5.72 78.921 6.84 <0.0001
Sex <0.0001
Female 13 520 (47.4) 3614 (50.6)
Male 15 020 (52.6) 3521 (49.4)
Age group (years) <0.0001
65–74 12 875 (45.1) 2143 (30.0) 75–84 13 290 (46.6) 3610 (50.6) 385 2 375 (8.3) 1382 (19.4) Urbanization 0.334 Low 1 796 (6.3) 419 (5.9) Moderate 10 949 (38.4) 2719 (38.1) High 15 795 (55.3) 3997 (56.0) No. medications <0.0001 0–1 9 356 (32.8) 1455 (20.4) 2–4 10 047 (35.2) 2542 (35.6) 5–9 7 531 (26.4) 2458 (34.5) 310 1 606 (5.6) 680 (9.5) Obesity 0.2166 No 28 342 (99.3) 7095 (99.4) Yes 198 (0.7) 40 (0.6) Diabetes mellitus <0.0001 No 21 355 (74.8) 4778 (67.0) Yes 7 185 (25.2) 2357 (33.0) Hypertension <0.0001 No 9 494 (33.3) 1541 (21.6) Yes 19 046 (66.7) 5594 (78.4) Hyperlipidemia 0.0155 No 20 260 (71.0) 4961 (69.5) Yes 8 280 (29.0) 2174 (30.5) Cerebrovascular disease <0.0001 No 18 576 (65.1) 2390 (33.5) Yes 9 964 (34.9) 4745 (66.5)
Chronic kidney disease <0.0001
No 26 437 (92.6) 6320 (88.6)
Polypharmacy has been regarded as a risk factor of ADR in older people. Nguyen et al. have found, in a geriatric nursing home study, residents using nine medications or more were 2.33-fold (95% CI 1.54–3.52) more likely than controls to experience an ADR.25One
longitudinal study in Sweden showed that older people using five or more drugs were 2.6-fold (95% CI 1.1–6.1) more likely to have a dementia-like state in approxi-mately 3 years of follow up than those not using drugs.26
In the present study, we reviewed the medication history of each subject for 2 years before the date at which dementia was diagnosed. That is, use of polyp-harmacy preceded the diagnosis of dementia. In the present study, drug-related dementia was increasingly identified as the number of medications increased, par-ticularly in older people. This appears as an obvious relationship between the number of medications and dementia, strongly supporting the hypothesis that polypharmacy is significantly related to the risk of dementia in older people.
Epidemiological studies have consistently shown a strong association between age and dementia.27–30 The
present study also showed the OR of dementia increased to 3.01 for people aged 85 years or more, compared with the younger group. Further analysis
showed that the daily use of medications also increased with age. However, it is not clear whether there was a higher risk of dementia for the older group mainly because of polypharmacy or other factors correspond-ing to age.
In the present study, women were at an elevated risk of dementia (OR 1.12). However, epidemiological studies regarding the role of sex in association with dementia have shown conflicting results. A large Italian population study found sex is not associated with dementia risk for older people.28In contrast, a Spanish
study showed women are more likely to have dementia than men.29Thus, the geographic variation of dementia
between men and women might be dependent on the population characteristics.
Epidemiological studies have consistently reported the association between dementia and comorbidities, particularly diabetes mellitus,31–35 hypertension34,35 and
cerebrovascular disease.29,30,33 In the present study, the
higher proportion of cerebrovascular disease in subjects with dementia and a strong association with cerebrovas-cular disease (OR 3.19) show that cerebrovascerebrovas-cular disease is associated with dementia. Nearly half of the patients with cerebrovascular disease were users of five and more drugs. Our data showed that polypharmacy
Table 2 Proportional distribution of medication by dementia and other medical conditions in Taiwan,
2000–2008 No. medications 0–1 2–4 5–9 310 n (%) n (%) n (%) n (%) Dementia No 9 356 (32.8) 10 047 (35.2) 7531 (26.4) 1606 (5.6) Yes 1 455 (20.4) 2 542 (35.6) 2458 (34.5) 680 (9.5) Obesity No 10 782 (30.4) 12 503 (35.3) 9903 (28.0) 2249 (6.3) Yes 29 (12.2) 86 (36.1) 86 (36.1) 37 (15.6) Diabetes mellitus No 9 905 (37.9) 9 569 (36.6) 5710 (21.9) 949 (3.6) Yes 906 (9.5) 3 020 (31.7) 4279 (44.8) 1337 (14.0) Hypertension No 6 672 (60.5) 3 242 (29.4) 999 (9.0) 122 (1.1) Yes 4 139 (16.8) 9 347 (37.9) 8990 (36.5) 2164 (8.8) Hyperlipidemia No 9 679 (38.4) 8 875 (35.2) 5616 (22.3) 1051 (4.1) Yes 1 132 (10.9) 3 714 (35.5) 4373 (41.8) 1235 (11.8) Cerebrovascular disease No 8 453 (40.3) 7 399 (35.3) 4336 (20.7) 778 (3.7) Yes 2 358 (16.0) 5 190 (35.3) 5653 (38.4) 1508 (10.3)
Chronic kidney disease
No 10 461 (31.9) 11 699 (35.7) 8733 (26.7) 1864 (5.7)
Yes 350 (12.0) 890 (30.5) 1256 (43.0) 422 (14.5)
Table 3 Crude and adjusted odds ratios and 95% confidence intervals of
dementia and associated factors in Taiwan, 2000–2008
Variable Univariate Multivariate
OR (95% CI) OR (95% CI)
Sex
Female 1.13 (1.07–1.19) 1.12 (1.06–1.19)
Male 1.00 (Reference) 1.00 (Reference)
Age group (years)
65–74 1.00 (Reference) 1.00 (Reference)
75–84 1.65 (1.55–1.75) 1.44 (1.35–1.53)
385 3.64 (3.36–3.95) 3.01 (2.76–3.27)
Urbanization
Low 1.00 (Reference) 1.00 (Reference)
Moderate 1.07 (0.95–1.20) 1.09 (0.97–1.23) High 1.10 (0.99–1.24) 1.11 (0.99–1.25) No. medications 0–1 1.00 (Reference) 1.00 (Reference) 2–4 1.63 (1.52–1.75) 1.28 (1.18–1.38) 5–9 2.10 (1.95–2.25) 1.34 (1.23–1.46) 310 2.72 (2.45–3.03) 1.56 (1.38–1.76) Obesity No 1.27 (0.91–1.79) 1.44 (1.01–2.06)
Yes 1.00 (Reference) 1.00 (Reference)
Diabetes mellitus No 1.00 (Reference) 1.00 (Reference) Yes 1.43 (1.35–1.51) 1.23 (1.16–1.32) Hypertension No 1.00 (Reference) 1.00 (Reference) Yes 1.71 (1.61–1.82) 1.08 (1.01–1.17) Hyperlipidemia No 1.00 (Reference) 1.00 (Reference) Yes 1.04 (0.98–1.10) 0.80 (0.75–0.85) Cerebrovascular disease No 1.00 (Reference) 1.00 (Reference) Yes 3.61 (3.41–3.81) 3.19 (3.01–3.38)
Chronic kidney disease
No 1.00 (Reference) 1.00 (Reference)
Yes 1.59 (1.46–1.73) 1.21 (1.10–1.33)
Table 4 Interaction between cerebrovascular disease and number of medications associated with dementia in
Taiwan, 2000–2008 Cerebrovascular disease
No. medications
0–1 drug 2–4 drugs 5–9 drugs 310 drugs
n/N n/N n/N n/N
OR(95% CI) OR(95% CI) OR(95% CI) OR(95% CI)
No 754/7699 903/6496 608/3728 125/653
1.00 (reference) 1.41 (1.26–1.57) 1.57 (1.39–1.78) 1.79 (1.44–2.21)
Yes 701/1657 1639/3551 1850/3803 555/953
1.00 (reference) 1.12 (1.01–1.25) 1.16 (1.03–1.29) 1.38 (1.19–1.59)
Adjusted for sex, age, obesity, diabetes mellitus, hypertension, hyperlipidemia and chronic kidney disease. CI, confidence interval; n, number of dementia cases; N, sample size; OR, odds ratio.
interacts with cerebrovascular disease and further increases the risk of dementia. The OR of dementia increased for 38% for patients with both cerebrovascu-lar disease and using310 drugs, compared with patients with cerebrovascular disease and using zero to one drug. The present study shows a dose–response relationship between polypharmacy and dementia among patients without cerebrovascular disease.
In addition, we found dementia also has a significant association with chronic kidney disease (OR 1.21). Only limited studies have explored this relationship. The REGARDS Study has suggested that impaired renal function is associated with a dementia-like state for USA adults after adjustment for cardiovascular risk fac-tors.36Two other studies carried out by Elias et al. and
by Etgen et al. also showed a similar trend.37,38Madero
et al. have reviewed several studies on dementia and
concluded that patients in all stages of chronic kidney disease are at an elevated risk of dementia with a sig-nificant impact on their quality of life.39Therefore, early
detection of dementia in the early course for patients with chronic kidney disease is highly recommended.
The topic is fascinating and original. The present pilot study has the strength of using a representative population to identify a large number of cases for a nested case–control observation, as a national electronic medical record offers significant power to assess these relationships. A risk factor reported in the present study, but not found elsewhere, is polypharmacy. The risk of dementia increases with the number of medica-tions. Thus, we emphasize that polypharmacy might correlate with the risk of dementia. A cross-sectional study by Doraiswamy et al.40has reported that 61% of
patients with Alzheimer’s disease had three or more coexisting medical conditions. From a clinical view, our data also support the concept that cerebrovascular disease, diabetes mellitus, chronic kidney disease and hypertension are significantly related to the risk of dementia.
There are limitations to the present study. First, there were a small number of patients with Alzheimer’s disease identified in the data analysis. How much the early stages of dementia could have contributed to the excessive use of medications was not clear. Confirma-tion of the risk variaConfirma-tion of dementia subtypes associ-ated with polypharmacy should be encouraged. Second, the other potential risk factors of dementia, such as genetic factors, smoking, education level, homocysteine level, folate level, environmental factors, family history of dementia and non-prescription drugs were not spe-cifically analyzed separately because of the inherent limitation of insurance data.
Third, use of drugs without clinical indication could also act as a risk factor for dementia, but it is not clearly differentiated by this dataset. Fourth, interpretation of these results should be done very carefully, as dementia
is really related to pre-existing comorbidities, parti-cularly cardiovascular diseases, which if optimally managed will need polypharmacy. Thus, further well-designed prospective studies are needed to confirm the association between polypharmacy and ADR in older people, and to explore whether minimizing the number of medications used might prevent ADR and further reduce the risk of dementia.
We conclude that the present study has shown that polypharmacy might correlate with the risk of dementia in older people in Taiwan. Cerebrovascular disease, dia-betes mellitus, chronic kidney disease and hypertension are also significantly related to the risk of dementia. Cerebrovascular disease might interact with polyphar-macy and further increase the dementia risk.
Acknowledgement
The authors thank the National Health Research Insti-tute in Taiwan for providing us the insurance claims data. This study was supported in part by grants from the Department of Health, Taiwan (DOH 97-HP-1101, 2008–2010), the Clinical Trial and Research Center of Excellence (DOH100-TD-B-111-004), the Cancer Research Center of Excellence (DOH100-TD-C-111-005), the National Science Council (NSC 99–2621-M-039-001) and China Medical University Hospital (1MS1). The funding agencies had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
Disclosure statement
The authors disclose no conflicts of interest.
References
1 Larson EB, Kukull WA, Buchner D, Reifler BV. Adverse drug reactions associated with global cognitive impairment in elderly persons. Ann Intern Med 1987; 107: 169–173. 2 Hajjar ER, Hanlon JT, Artz MB et al. Adverse drug reaction
risk factors in older outpatients. Am J Geriatr Pharmacother 2003; 1: 82–89.
3 du Souich P. In human therapy, is the drug-drug interac-tion or the adverse drug reacinterac-tion the issue? Can J Clin
Pharmacol 2001; 8: 153–161.
4 Ministry of the Interior inTaiwan. Resident population by 5-year, 10-year age group. [Cited 1 Jun 2009.] Available from URL: http://sowf.moi.gov.tw/stat/month/m1-06.xls 5 Liu CK, Lin RT, Chen YF, Tai CT, Yen YY, Howng SL.
Prevalence of dementia in an urban area in taiwan. J Formos
Med Assoc 1996; 95: 762–768.
6 Lin RT, Lai CL, Tai CT, Liu CK, Yen YY, Howng SL. Prevalence and subtypes of dementia in southern Taiwan: impact of age, sex, education, and urbanization. J Neurol Sci 1998; 160: 67–75.
7 Liu HC, Fuh JL, Wang SJ et al. Prevalence and subtypes of dementia in a rural Chinese population. Alzheimer Dis Assoc
8 Hay JW, Ernst RL. The economic costs of Alzheimer’s disease. Am J Public Health 1987; 77: 1169–1175.
9 Chiu L, Shyu WC. Estimation of the family cost of private nursing home care versus home care for patients with dementia in Taiwan. Chang Gung Med J 2001; 24: 608–614. 10 Lopez-Bastida J, Serrano-Aguilar P, Perestelo-Perez L, Oliva-Moreno J. Social-economic costs and quality of life of Alzheimer disease in the Canary Islands, Spain.
Neurol-ogy 2006; 67: 2186–2191.
11 Malone DC, McLaughlin TP, Wahl PM et al. Burden of Alzheimer’s disease and association with negative health outcomes. Am J Manag Care 2009; 15: 481–488.
12 Katz IR, Parmelee P, Brubaker K. Toxic and metabolic encephalopathies in long-term care patients. Int
Psychoge-riatr 1991; 3: 337–347.
13 Moore AR, O’Keeffe ST. Drug-induced cognitive impair-ment in the elderly. Drugs Aging 1999; 15: 15–28. 14 Cheng TM. Taiwan’s national health insurance system:
high value for the dollar. In: Okma KGH, Crivelli L, eds.
Six Countries, Six Reform Models: Their Healthcare Reform, Experience of Israel, the Netherlands, New Zealand, Singapore, Switzerland and Taiwan. New Jersey, NJ: World scientific,
2009; 171–204.
15 Lai SW, Liao KF, Liao CC, Muo CH, Liu CS, Sung FC. Polypharmacy correlates with increased risk for hip frac-ture in the elderly: a population-based study. Medicine
(Bal-timore) 2010; 89: 295–299.
16 Lai SW, Muo CH, Liao KF, Sung FC, Chen PC. Risk of acute pancreatitis in type 2 diabetes and risk reduction on anti-diabetic drugs: a population-based cohort study in taiwan. Am J Gastroenterol 2011; 106: 1697–1704.
17 Lai SW, Su LT, Lin CH, Tsai CH, Sung FC, Hsieh DP. Polypharmacy increases the risk of Parkinson’s disease in older people in Taiwan: a population-based study.
Psycho-geriatrics 2011; 11: 150–156.
18 Meador KJ. Cognitive side effects of medications. Neurol
Clin 1998; 16: 141–155.
19 Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother 2007; 5: 345–351. 20 Ballentine NH. Polypharmacy in the elderly: maximizing
benefit, minimizing harm. Crit Care Nurs Q 2008; 31: 40–45.
21 Fulton MM, Allen ER. Polypharmacy in the elderly: a lit-erature review. J Am Acad Nurse Pract 2005; 17: 123–132. 22 Chan DC, Hao YT, Wu SC. Characteristics of outpatient
prescriptions for frail Taiwanese elders with long-term care needs. Pharmacoepidemiol Drug Saf 2009; 18: 327–334. 23 Robbins AS, Rubenstein LZ, Josephson KR, Schulman BL,
Osterweil D, Fine G. Predictors of falls among elderly people. Results of two population-based studies. Arch Intern
Med 1989; 149: 1628–1633.
24 Jorgensen T, Johansson S, Kennerfalk A, Wallander MA, Svardsudd K. Prescription drug use, diagnoses, and health-care utilization among the elderly. Ann Pharmacother 2001;
35: 1004–1009.
25 Nguyen JK, Fouts MM, Kotabe SE, Lo E. Polypharmacy as a risk factor for adverse drug reactions in geriatric nursing
home residents. Am J Geriatr Pharmacother 2006; 4: 36– 41.
26 Monastero R, Palmer K, Qiu C, Winblad B, Fratiglioni L. Heterogeneity in risk factors for cognitive impairment, no dementia: population-based longitudinal study from the Kungsholmen Project. Am J Geriatr Psychiatry 2007; 15: 60–69.
27 Kukull WA, Higdon R, Bowen JD et al. Dementia and Alzheimer disease incidence: a prospective cohort study.
Arch Neurol 2002; 59: 1737–1746.
28 Ravaglia G, Forti P, Maioli F et al. Incidence and etiology of dementia in a large elderly Italian population. Neurology 2005; 64: 1525–1530.
29 Fernandez Martinez M, Castro Flores J, Perez de Las Heras S, Mandaluniz Lekumberri A, Gordejuela Menocal M, Zarranz Imirizaldu JJ. Risk factors for dementia in the epidemiological study of Munguialde County (Basque Country-Spain). BMC Neurol 2008; 8: 39.
30 Magalhaes MO, Peixoto JM, Frank MH et al. Risk factors for dementia in a rural area of Northeastern Brazil. Arq
Neuropsiquiatr 2008; 66: 157–162.
31 Peila R, Rodriguez BL, Launer LJ. Type 2 diabetes, APOE gene, and the risk for dementia and related pathologies: the Honolulu-Asia Aging Study. Diabetes 2002; 51: 1256– 1262.
32 Schnaider Beeri M, Goldbourt U, Silverman JM et al. Dia-betes mellitus in midlife and the risk of dementia three decades later. Neurology 2004; 63: 1902–1907.
33 Rastas S, Pirttila T, Mattila K et al. Vascular risk factors and dementia in the general population aged >85 years: pro-spective population-based study. Neurobiol Aging 2010; 31: 1–7.
34 Whitmer RA, Sidney S, Selby J, Johnston SC, Yaffe K. Midlife cardiovascular risk factors and risk of dementia in late life. Neurology 2005; 64: 277–281.
35 Sakurai H, Hanyu H, Kanetaka H et al. Prevalence of coex-isting diseases in patients with Alzheimer’s disease. Geriatr
Gerontol Int 2010; 10: 216–217.
36 Kurella Tamura M, Wadley V, Yaffe K et al. Kidney function and cognitive impairment in US adults: the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Am J Kidney Dis 2008; 52: 227– 234.
37 Elias MF, Elias PK, Seliger SL, Narsipur SS, Dore GA, Robbins MA. Chronic kidney disease, creatinine and cog-nitive functioning. Nephrol Dial Transplant 2009; 24: 2446– 2452.
38 Etgen T, Sander D, Chonchol M et al. Chronic kidney disease is associated with incident cognitive impairment in the elderly: the INVADE study. Nephrol Dial Transplant 2009; 24: 3144–3150.
39 Madero M, Gul A, Sarnak MJ. Cognitive function in chronic kidney disease. Semin Dial 2008; 21: 29–37. 40 Doraiswamy PM, Leon J, Cummings JL, Marin D,
Neumann PJ. Prevalence and impact of medical comorbid-ity in Alzheimer’s disease. J Gerontol A Biol Sci Med Sci 2002;