Usefulness of the Mini Nutritional Assessment in predicting the nutritional status of patients with liver cancer in Taiwan
Alan C. Tsai, Wei-Chung Hsu, Shu-Ching Chan, and Tusi-Lan Chang
A. C. Tsai, S. C. Chan and T. L. Chang are affiliated with the Department of Healthcare Administration of Asia University, Taichung, Taiwan.
W. C. Hsu is affiliated with the Department of Radiation Oncology, Cheng-Ching General Hospital, Taichung, Taiwan
*Correspondence author: Alan C. Tsai, Ph. D., Visiting professor, Dept. of Healthcare Adm., Asia University, 500 Liufeng Rd., Wufeng, Taichung, Taiwan 41354. Phone: 886-4-2332 3456 x1943; Fax: 886-4-2332-1206; E-mail: atsai@umich.edu
Abstract
Liver cancer patients are confronted with additional risk of malnutrition because the disease is often associated with hepatitis, liver cirrhosis and metabolic disturbances. Nutritional intervention can improve treatment outcome but early detection is important. This study aimed to determine whether the Mini Nutritional Assessment (MNA) could effectively rate the nutritional status of patients with liver cancer in Taiwan. A total of 300 patients were evaluated for
nutritional status with two modified versions of the MNA in short- and long-forms. MNA-Taiwan version-1 adopted population-specific anthropometric cut-points whereas version-2 replaced mid-arm and calf circumferences in place of BMI. Predicted statuses were compared to results predicted by the Council on Nutrition Appetite Questionnaire (CNAQ) and analyzed for correlations with biochemical or cancer status parameters. Results showed that both versions of the MNA were effective in predicting nutritional status and predictions by the short-forms agreed well with that by the long-forms. The nutritional scores correlated well with hemoglobin, serum albumin, C-reactive protein, r-glutamyl transpeptidase, TNM (Tumor, Node, Metastasis) staging and severity of cirrhosis. These results suggest that the MNA can be an effective tool for
Introduction
Cancer patients are at high risk of malnutrition and patients with liver cancer may have additional nutritional risk because they often have hepatitis, liver cirrhosis and neoplastic cachexia. These patients are often confronted with anorexia, involuntary weight loss, muscle wasting, anemia, malnutrition and other metabolic abnormalities (1,2). Poor nutrition or depleted nutritional reserve may adversely affect a patient’s prognosis, tolerance to treatment,
susceptibility to diseases and infections, quality of life, and even survival. Early detection and timely intervention is important. Proper assessment tools are needed to monitor the progress of intervention. To be an effective routine procedure, the tool needs to be simple, reliable, low cost and non-invasive, and can be easily applied without requiring extensive professional background or training. The Mini Nutritional Assessment (MNA) is a tool that meets these conditions (3-5) but it has not yet been robustly validated for use in cancer patients although it has been suggested to be an appropriate tool for identifying cancer patients at risk of malnutrition (6). A recent study has further shown that the MNA has good sensitivity and moderate specificity using the Scored Patient-Generated Subjective Global Assessment (PGSGA) as gold standard (7).
Malignant tumor is the leading cause of death in Taiwan and liver cancer is the leading tumor in men (8). Although nutrition plays a well known role in the prognosis and treatment outcome of cancer patients, relatively little attention has been paid to monitoring their nutritional status on a routine basis. Therefore, the objective of this study was to determine the usefulness of the MNA in predicting the nutritional status of patients with liver cancer in Taiwan. Two modified versions of the MNA were examined; one using the population-specific anthropometric cut-points (a content-equivalent version) and another further with the BMI item in the scale replaced by
mid-arm and calf circumferences. A scale without BMI will eliminate the need of weight measurement which can be thrown off because of ascites or edema in cancer patients.
Methods
The study employed a convenience sampling and recruited out-patients with liver cancer of a hospital in Central Taiwan to participate in the study. Patients who were 30 years or older, able to communicate verbally and willing to sign a written study consent were recruited. A total of 300 consecutive patients (239 men and 61 women) agreed to participate in the study which took place during Aug. 15, 2007 to Jan. 31, 2008. The Institutional Review Board of the hospital approved the study protocol.
In addition to the routine clinical procedure, each participant was also interviewed with a structured questionnaire for eliciting personal demographic, lifestyle and health-related data and answers to questions in the Council on Nutrition Appetite Questionnaire (CNAQ) (9) and the MNA, and measured for weight, height, and mid-arm (MAC) and calf circumferences (CC) (10). An over-night fasting blood sample was taken for measurement of hemoglobin, blood urea nitrogen, serum albumin, cholesterol, C-reactive protein (CRP), creatinine, r-glutamyl trans-peptidase (r-GT) and alpha-fetoprotein (AFP) as a part of their routine laboratory tests.
CNAQ is a validated appetite/nutrition risk assessment tool. It can predict a 5% weight loss in six months. This 8-item questionnaire has a maximum of 40 points and those who score less than 28 points are considered having impaired appetite status (9). The nutritional status of each subject was assessed with two slightly modified versions of the MNA, Taiwan version-1 and -2 (MNA-T1 and -T2). The MNA-T1 adopts Taiwanese-specific anthropometric cut-points
and is considered a content equivalent version of the original MNA for Taiwanese (11). The MNA-T2 displaced BMI from the scale by reassigning the weighted score of BMI to the MAC and CC items (12,13).
Hepatitis status was classified according to the infected viruses: Types B, C, non B-non C and B & C. Liver cirrhosis status was graded with Child-Pugh classification (14,15). The stage of liver cancer was classified according to TNM (tumor, node & metastasis) staging set forth by the sixth edition of AJCC/UICC (American Joint Committee on Cancer and International Union against Cancer) (16).
Results were analyzed with SPSS version 12.0 (SPSS Inc., Chicago, IL, USA) computer software package. Spearman's Correlation analysis was employed to determine the significance of relationship between the MNA scores and each of the demographic, lifestyle, health and biochemical parameters. A binary classification test was used to determine the agreement between results predicted with the MNA and the CNAQ. Receiver Operating Characteristics (ROC) curves were generated for the MNA versions using CNAQ as the reference, and for the short-form MNA versions using the long-form versions as the references. Statistical significance was accepted at alpha = 0.05.
Results
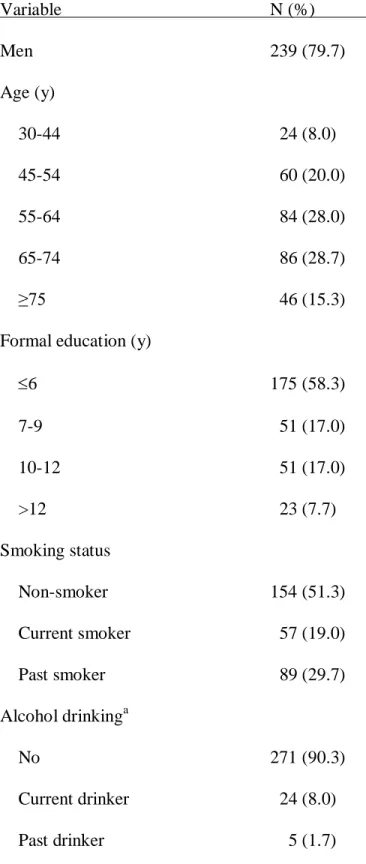
The characteristics of subjects are summarized in Table 1. The majority (80%) of patients were males. Most (77%) subjects were 45 to 74 years old. More than half (59%) of subjects had no co-morbidity, 39% had 1-3 and 2% had four or more. Thirty-nine percent of subjects were taking 1-3 kinds of prescribed medicine, 37% were taking 4 or more and 25% were not taking
any. Thirty-one percent of subjects had poor appetite, 39% had fair appetite and only 30% had good appetite according to CNAQ.
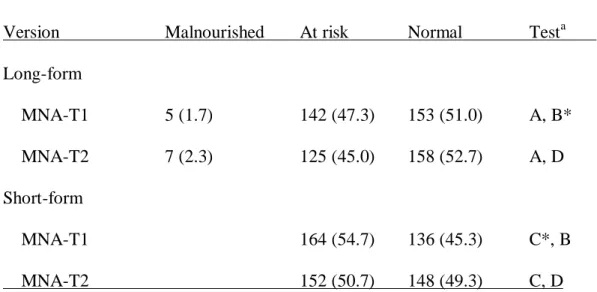
The MNA-T1-LF graded 2% of subjects malnourished, 47% at risk of malnutrition and 51% normal whereas the MNA-T2-LF graded 2, 45 and 53%, respectively (p>0.05) (Table 2). The T1-SF rated 55% at high risk of malnutrition and 45% at low risk whereas the MNA-T2-SF rated 51 and 49%, respectively (p<0.05).
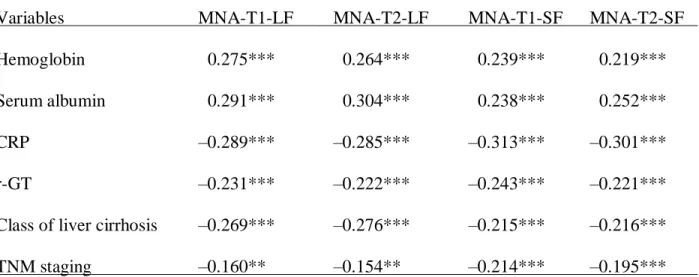
Table 3 shows the Spearman's correlation coefficients (r) of the MNA scores with each of the nutrition- or cancer status-related parameters. The strength of relationship between the two long-form MNA versions or the two short-form versions was relatively similar. Hemoglobin, serum albumin and class of liver cirrhosis had slightly stronger relationship with the long-form versions compared to that with the short-form versions. On the other hand, CRP and TNM-staging had slightly stronger relationship with the short-form versions compared to that with the long-form versions. Both long-form and short-form MNA versions had similar strength of relationship with r-GT.
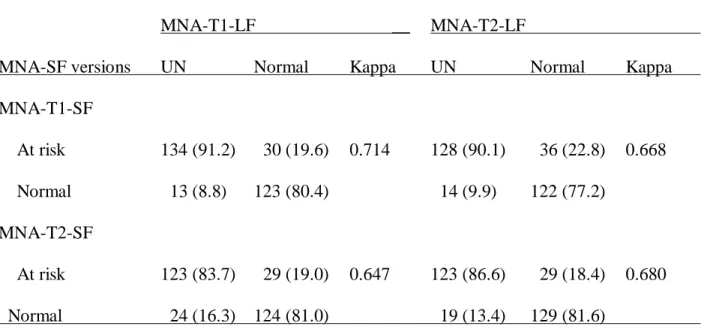
Table 4 shows the binary classification tests of the nutritional risk statuses predicted with the short-form versions using results predicted with the long-forms as “gold standard”. Test characteristics were sensitivity 0.922, specificity 0.804 and kappa 0.714 for T1-SF; 0.837, 0.810 and 0.647, respectively, for T2-SF. When using T2-LF as "gold standard", the respective values were 0.901, 0.772 and 0.668 for T1-SF, and 0.866, 0.816 and 0.680 for T2-SF.
Analysis with receiver operating characteristic (ROC) showed that areas under the curve (AUC) generated by the two versions were very similar, 0.714 and 0.720 for T1-LF and T2-LF, and 0.696 and 0.704 for T1-SF and T2-SF, respectively, using the predictions made with CNAQ as the reference (Fig. 1).
Fig. 2 shows that the AUC generated by the two short-form MNA versions agreed well with predictions made with the two long-form versions. The AUC was 0.939 for T1-SF and 0.915 for SF using MNA-T1-LF as "gold standard"; 0.926 and 0.929, respectively, using T2-LF as "gold standard". Subjects' cancer-related information, anthropometric and biochemical data, and scoring patterns of the MNA items are summarized in Appendix 1, 2 & 3, respectively.
Discussion
Predicting the nutritional status
Results of the present study suggest that the MNA is effective in predicting the nutritional status of patients with liver cancer. Both versions (T1 and T2) rated similar proportions of
patients malnourished or at risk of malnutrition. The nutritional scores rated with the two versions are strongly correlated with nutritional indicators such as serum albumin and
hemoglobin levels. Results also agree well with the appetite status evaluated with the CNAQ. These results suggest the MNA is capable of predicting the nutritional status of patients with liver cancer.
The MNA has been suggested as a tool that can potentially help determine the most appropriate diagnostic procedures and the best therapeutic strategies by identifying individuals at risk of malnutrition and measuring the efficacy of nutritional interventions in cancer patients (6). However, few studies have demonstrated the usefulness of the MNA in grading the nutritional status of cancer patients. Slaviero et al. (17) observed strong interrelationships between
biochemical and anthropometric measures and the MNA scores in cancer patients and found that the baseline weight loss status was highly correlated with MNA scores and plasma CRP.
More recently, Read et al. (7) evaluated the predictive ability of the MNA using predictions made with PGSGA as the reference and found that the MNA had good sensitivity (79-97%) but more moderate specificity (54-82%) at various stages of a nutritional intervention in cancer patients. These results suggest that the MNA is capable of correctly classifying patients who are truly malnourished but slightly less able identifying those who are truly not
malnourished using the PGSGA as the reference.
Short-form vs. long-form
As demonstrated in the ROC curves, results predicted with both short-form MNA versions agree well with that predicted with long-form versions. Binary classification tests also show that both short-form versions have high sensitivity against long-form versions. The two short-form versions can identify 84 to 92% of those who are identified at risk by the long-form versions. The rate of false positive is also relatively low (18-23%). Further, it should be
remembered that nutritional risk is in a continuum, the false positives and the false negatives are likely to be in an ambiguous state. When compared to independent nutritional or cancer staging or severity indicators, the short-form MNA versions generally perform favorably and in some cases even better than the long-form versions. These results suggest the short-form versions are capable of identifying most patients with cancer at risk of malnutrition. With frequent screening, the risk of missing a positive case would be relatively low.
MNA-T1 vs. T2
Results suggest that the MNA-T1 and -T2 have comparable ability in predicting the nutritional status and in reflecting the stage of liver cancer or functional status of patients with liver cancer. MNA-T2 has been shown to be an effective alternative to MNA-T1 in elderly from various living settings (12,13,18,19). The availability of an alternative version without weight
and height measurements is a significant improvement and would improve the applicability of the MNA in places where weighing scale is not a common household item or for patients who have ascites or edema which may throw off weight measurement.
The MNA in addition to predicting the nutritional status also reflects liver functional status. The nutritional scores graded with the MNA-T1 and T2 are positively correlated with nutritional indicators such as hemoglobin and serum albumin and are negatively correlated with liver inflammation indicators (CRP), the severity of liver cirrhosis, the stage of liver tumor and serum r-GT. Serum albumin reflects nutritional status but is also indicative of liver functional status. In patients with liver cancer, nutritional status is influenced not only by nutrient intake but also by the functional status of the liver. As the tumor progresses, hepatitis and cirrhosis (which are often associated with liver tumor) can impair liver function. Thus, in these patients, drastic changes in appetite and nutritional status can occur abruptly. Close monitoring of nutritional status is important in cancer patients.
Limitations of the study
This study has some obvious limitations. Cancer patients vary in the type and stage of cancer, comorbidity, treatment, and self-imposed life-style changes. Results of the present study reflect the general condition and treatment of the participating subjects. The present study involved only community home-dwelling subjects from one hospital in Central Taiwan. Thus, the generalizability of study results should be interpreted with caution. In patients with advanced liver cancer, ascites may be a problem and that can complicate anthropometric measurements. Since patients' appetite is impacted by both dietary intake and liver functional status, the nutritional status of liver cancer patients can change rather drastically and abruptly. Frequent monitoring would be especially important in these patients.
Conclusion
Using CNAQ and a list of nutritional and cancer staging or liver functional indicators as references, this study has demonstrated that the MNA is a useful tool in predicting the nutritional status of patients with liver cancer. Results also have demonstrated that a modified version without BMI can function adequately compared to a content-equivalent version of the MNA that adopted Taiwanese-specific anthropometric cut-points. The study further shows that both of the short-form versions perform well compared to the long-form versions. These results suggest that both the long-form and short-form of both versions can be used to monitor the nutritional risk of patients with liver cancer.
Acknowledgments and notes
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. We thank the patients for their cooperation in this study. Address correspondence to A. C. Tsai, Dept. of Healthcare Adm., Asia University, 500 Liufeng Rd., Wufeng, Taichung, Taiwan 41354. Phone: 886 4 2332 3456 x-1943. E-mail:
References
1. Argiles JM: Cancer-associated malnutrition. Eur J Oncol Nurs 9, (Suppl 2), S39-S50, 2005. 2. Davies M: Nutritional screening and assessment in cancer- associated malnutrition. Eur J
Oncol Nurs, 9 (Suppl 2), S64-73, 2005.
3. Guigoz Y, Vellas BJ, Garry PJ: The Mini Nutritional Assessment (MNA): A practical assessment tool for grading the nutritional state of elderly patients. In Facts and Research in Gerontology, New York, Sprinker, 1994, pp 15-59.
4. Guigoz Y, Vellas B, Garry PJ: Assessing the nutritional status of the elderly: The mini
nutritional assessment as part of the geriatric evaluation. Nutr Rev 54 (suppl), S59-S65, 1996. 5. Guigoz Y, Lauque S, Villas BJ: Identifying the elderly at risk for malnutrition. The Mini
Nutritional Assessment. Clin Geriatr Med 18, 737-757, 2002.
6. Zulian GB, Gold G, Herrmann F, Michel JP: Mini Nutritional Assessment and cancer. Nestle Nutr Workshop Ser Clin Perform Programme 1, 93-100, 1999.
7. Read JA, Crockett N, Volker DH, MacLennan P, Choy STB, et al.: Nutritional Assessment in Cancer: Comparing the Mini-Nutritional Assessment (MNA) with the Scored
Patient-Generated Subjective Global Assessment (PGSGA). Nutr Cancer 53, 51-56, 2005. 8. Death Cause Statistics of 2008, Taiwan.
http://www.doh.gov.tw/CHT2006/DM/DM2_2.aspx?now_fod_list_no=10642&class_no=44 0&level_no=3. (Accessed Oct. 21, 2009)
9. Wilson MMG, Thomas DR, Rubenstein LZ, Chibnall JT, Anderson S, et al.: Appetite
assessment: simple appetite questionnaire predicts weight loss in community-dwelling adults and nursing home residents. Am J Clin Nutr 82, 1074-1081, 2005.
10. Lee RD, Nieman DC: Biochemical assessment of nutritional status. In Nutritional assessment. 3rd edition. Lee RD & Nieman DC (eds). New York, McGraw-Hill Higher Education, A Division of the McGraw-Hill Companies, 2003, pp 303-337.
11. Tsai AC, Ho CS, Chang MC: Population-specific anthropometric cut-points improve the functionality of the Mini Nutritional Assessment (MNA) in elderly Taiwanese. Asia Pacific J Clin Nutr 16, 656-662, 2007.
12. Tsai AC, Ku PY & Tsai J-D: Population-specific anthropometric cutoff standards improve functionality of the Mini-Nutritional Assessment without BMI in institutionalized elderly in Taiwan. J Nutr Health Aging 12, 696-700, 2008.
13. Tsai AC, Chou YT, Chang TL, Chang-Lee SN, Tsay SF: A modified Mini Nutritional Assessment without BMI can effectively assess the nutritional status of neuropsychiatric patients. J Clin Nurs 18, 1916-1922, 2009.
14. Child CG, Turcotte JG. Surgery and portal hypertension. In: The liver and portal hypertension. Child CG III, ed. Philadelphia, WB Saunders; 1964, pp 57-72.
15. Pugh RNH, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg 60, 649-649, 1973.
16. Greene FL, Page DL, Fleming ID, Fritz A, Balch CM, et al.: Part III-14. Liver (Including Intrahepatic Bile Ducts). In AJCC Cancer Staging Manual. Sixth ed. Greene FL, Page DL, Fleming ID, Fritz A, Balch CM, Haller DG, Morrow M. (eds). New York: Springer-Verlag New York Inc.; 2002, pp 131-138.
17. Slaviero KA, Read JA, Clarke SJ, Rivory LP: Baseline nutritional assessment in advanced cancer patients receiving palliative chemotherapy. Nutr Cancer 46, 148-157, 2003.
18. Tsai AC, Shih CL: A population-specific Mini Nutritional Assessment can effectively grade the nutritional status of stroke rehabilitation patients in Taiwan. J Clin Nurs 18, 82-88, 2008. 19. Tsai AC, Lu SJ, Chang TL: Modified Mini Nutritional Assessment can effectively assess the
(Legend to Figure 1)
Figure 1. Receiver operating characteristic (ROC) curves for T1-LF ( ) and MNA-T2-LF ( ) scores (Chart A), and MNA-T1-SF ( ) and MNA-T2-SF ( ) scores (Chart B) using CNAQ score (≤28 points) as the reference in liver cancer patients. The areas under the curve (AUC) were 0.714 (95% CI = 0.644-0.783) and 0.720 (0.649-0.791) for T1-LF and T2-LF, respectively, in Chart A, and 0.696 (0.627-0.765) and 0.704 (0.636-0.772) for T1-SF and T2-SF, respectively, in Chart B (All p<0.05).
(Legend to Figure 2)
Figure 2. Receiver operating characteristic (ROC) curves for T1-SF ( ) and MNA-T2-SF ( ) using MNA-T1-LF (MNA score ≤23.5) (Chart A) and MNA-T2-LF (Chart B) as the reference, respectively. The areas under the curve (AUC) were 0.939 (95% CI = 0.915-0.963) and 0.915 (0.885-0.945) for MNA-T1-SF and MNA-T2-SF, respectively, in Chart A; and 0.926 (0.898-0.954) and 0.929 (0.902-0.955) for MNA-T1-SF and MNA-T2-SF, respectively in Chart B. (All p<0.05).
Table 1. Characteristics of Subjects (N = 300) Variable N (%) Men 239 (79.7) Age (y) 30-44 24 (8.0) 45-54 60 (20.0) 55-64 84 (28.0) 65-74 86 (28.7) ≥75 46 (15.3)
Formal education (y)
6 175 (58.3) 7-9 51 (17.0) 10-12 51 (17.0) >12 23 (7.7) Smoking status Non-smoker 154 (51.3) Current smoker 57 (19.0) Past smoker 89 (29.7) Alcohol drinkinga No 271 (90.3) Current drinker 24 (8.0) Past drinker 5 (1.7)
Betel nut-chewing No 279 (93.0) Yes 21 (7.0) Routine exerciseb No 128 (42.7) Yes 172 (57.3) Co-morbidity c 0 177 (59.0) 1-3 118 (39.3) ≥4 5 (1.7)
No. of prescribed medicine
0 74 (24.7)
1-3 116 (38.7)
≥4 110 (36.6)
Appetite status (CNAQ)d
Poor 92 (30.7)
Average 117 (39.0)
Good 91 (30.3)
a
Defined as ≥1 time/month. But all positive responders drank >3 times/wk. b≥2 times/wk and ≥30 min/day.
c
Co-morbidities included heart disease, diabetes mellitus, hypertension, hyperlipidemia, respiratory disease, kidney disease and stroke.
d
Table 2. Distribution (N, %) of Nutritional Status Graded with the Long-form and Short-form MNA-T1 and T2
__________________________________________________________________
Version Malnourished At risk Normal Testa
Long-form MNA-T1 5 (1.7) 142 (47.3) 153 (51.0) A, B* MNA-T2 7 (2.3) 125 (45.0) 158 (52.7) A, D Short-form MNA-T1 164 (54.7) 136 (45.3) C*, B MNA-T2 152 (50.7) 148 (49.3) C, D
MNA = Mini Nutritional Assessment, T1 & T2 = Taiwan version 1 & 2. a
Distributions indicated by the same alphabet are compared for significant difference with Wilcoxon Matched-Pairs Signed-Rank Test. Comparison A: Z = -0.905 (p>0.05); B: Z = -2.592 (p<0.05); C: Z = -3.00 (p<0.05); and D: Z = -1.443 (p>0.05).
Table 3. Spearman's Correlation Coefficient (r) of the MNA Scores with Each of the Biochemical and Anthropometric Parameters (N=300)
Variables MNA-T1-LF MNA-T2-LF MNA-T1-SF MNA-T2-SF
Hemoglobin 0.275*** 0.264*** 0.239*** 0.219***
Serum albumin 0.291*** 0.304*** 0.238*** 0.252***
CRP –0.289*** –0.285*** –0.313*** –0.301***
r-GT –0.231*** –0.222*** –0.243*** –0.221***
Class of liver cirrhosis –0.269*** –0.276*** –0.215*** –0.216***
TNM staging –0.160** –0.154** –0.214*** –0.195***
MNA = Mini Nutritional Assessment, T1 & T2 = Taiwan version 1 & 2, CRP = C-reactive protein, r-GT= r-glutamyl transpeptidase.
Table 4. Binary Classification Tests of the Nutritional Status of Patients Graded with Short-form MNA Versions against the Outcome Graded with the Long-form Versions.
______________________________________________________________________________
MNA-T1-LF __ MNA-T2-LF
MNA-SF versions UN Normal Kappa UN Normal Kappa
MNA-T1-SF At risk 134 (91.2) 30 (19.6) 0.714 128 (90.1) 36 (22.8) 0.668 Normal 13 (8.8) 123 (80.4) 14 (9.9) 122 (77.2) MNA-T2-SF At risk 123 (83.7) 29 (19.0) 0.647 123 (86.6) 29 (18.4) 0.680 Normal 24 (16.3) 124 (81.0) 19 (13.4) 129 (81.6)
MNA = Mini Nutritional Assessment, T1 & T2 = Taiwan version 1 & 2, LF = long-form, SF = short-form, UN =Undernutrition (Malnourished + at risk portions).
Appendix 1. Cancer-Related Information of Subjects (N = 300) ________________________________________________ Type of hepatitis N (%) Non-B, C 30 (10.0) B 148 (49.3) C 108 (36.0) B and C 14 (4.7)
Liver cirrhosis statusa
A 202 (67.4) B 88 (29.3) C 10 (3.3) TNM stagesb I 22 (7.3) II 103 (34.3) III 126 (42.0) IV 49 (16.3) a
Child Classification of liver cirrhosis. Class A (5-7 points) is mild, B (8-10 points) is moderate, and C (11-15 points) is severe cirrhosis.
b
TNM (Tumor, Node, Metastasis) staging--based on AJCC/UICC (American Joint Committee on Cancer and International Union Against Cancer) criteria. Stage I is T1,N0 & M0; Stage II is T2, N0 & M0; stage III is T3/4, N0 & M0, or any T, N1 & M0; and Stage IV is M1 and any T & any N). T-staging (tumor size) has four stages T1, T2, T3 & T4; N-staging (lymph node metastasis)
is classified N0 (no regional metastasis) or N1 (regional metastasis); and M-staging is classified M0 (no distant metastasis) or M1 (distant metastasis).
Appendix 2. Anthropometric and Serum Biochemical Parameters (Mean ± SD) of subjects (N = 300)a Parameter (Mean ± SD) % Height (cm) Men 166.0 ± 6.2 Women 154.4 ± 5.6 Weight (kg) Men 64.3 ± 11.0 Women 54.8 ± 10.1 BMI (kg/m2) Men 23.3 ± 3.6 Women 23.0 ± 4.0 Mid-arm circumference (cm) Men 27.2 ± 3.3 Women 27.1 ± 3.8 Calf circumference (cm) Men 35.0 ± 3.8 Women 32.8 ± 3.9 Hemoglobin (g/dL) 12.6 ± 2.0 <12/10b g/dL 28.7 Serum albumin (g/dL) 3.6 ± 1.9 <3.5 g/dL 46.3
Serum cholesterol (mg/dL) 173.7 ± 48.7 <150 mg/dL 34.0 Serum CRP (mg/dL) 2.1 ± 3.4 > 1.0 mg/dL 42.2 BUN (mg/dL) 18.0 ± 11.2 >20 mg/dL 25.2 Serum creatinine (mg/dL) 1.3 ± 1.2 >1.5 mg/dL 16.8 r-GT (U/L) 219.3 ± 261.1 >75 U/L 71.8 AFP (ng/mL) 11.5×103 ± 24.3×103 >400 ng/mL 42.8
CRP = C-reactive protein; r-GT = r-glutamyl transpeptidase; AFP = alpha-fetoprotein; BUN = blood urea nitrogen.
a
239 men and 61 women. b
Appendix 3. Scoring Patterns of the MNA Questions (N = 300)
______
Component (item score) Assigned score %
A. Food intake declined over the past 3 month (2)
Severe 0 6.0
Moderate 1 44.0
No decline 2 50.0
B. Weight loss during last month (3)
>3 kg 0 31.0
Does not know 1 3.3
1-3 kg 2 24.0
No loss 3 41.7
C. Mobility (2)
Bed or chair-bound 0 0.7
Able to get out bed but does not go out 1 4.6
Goes out 2 94.7
D. Psychological stress/acute disease during past 3 months (2)
Yes 0 31.3
No 2 68.7
E. Neuropsychological problems (2)
Severe dementia or depression 0 1.0
Mild dementia 1 2.0
F. BMI (kg/m2) (3) (a) T1 <17 0 1.7/4.9a 17-19 1 7.9/13.1 19-21 2 17.6/8.2 >21 3 72.8/73.8
(b) T2 (0) Replaced with CC, item R) G. Live independently (1)
No 0 5.7
Yes 1 94.3
H. Takes 4 or more kinds of prescribed drugs/day (1)
Yes 0 36.7
No 1 63.3
I. Pressure sores or skin ulcers (1)
Yes 0 5.3
No 1 94.7
J. Full meals daily (2)
1 0 0.7
2 1 7.6
3 2 91.7
K. Daily consumption of protein-rich food (1)
0 or 1 “yes” 0 4.0
3 “yes” 1 70.7 L. Consumes ≥2 servings of fruits or vegetables per day (1)
No 0 10.7
Yes 1 89.3
M. Cups of water/fluid consumed (1)
<3 0 0.0
3-5 0.5 29.0
>5 1 71.0
N. Mode of feeding (2)
Unable to eat without assistance 0 0.3
Self-fed with difficulty 1 2.0
Self-fed with any problem 2 97.7
O. Self view of nutritional status (2)
Views self as being malnourished 0 26.0
Uncertain of nutritional status 1 34.0
No nutritional problem 2 40.0
P. Self view of health status compared to peers (2)
Not as good 0 54.0
Does not know 0.5 17.7
As good 1 20.6
Better 2 7.7
Q. MAC (cm) (a) T1 (1)
<22.5/21a 0 5.1/3.3a 22.5-23.5/21-22 0.5 5.4/6.5 >23.5/22 1 89.5/90.2 (b) T2 (2) <22.5/21 0 5.1/3.3 22.5-23.5/21-22 1 5.4/6.5 >23.5/22 2 89.5/90.2 R. CC (cm) (a) T1 (1) <28/25 0 1.7/6.6 >28/25 1 98.3/93.4 (b) T2 (3) <28/25 0 1.7/1.6 28-29/25-26 1 3.8/0.0 29-30/26-27 2 2.9/3.3 >30/27 3 91.6/95.1
MNA = Mini Nutritional Assessment, BMI = body mass index, MAC = mid-arm circumference, CC = calf circumference.
a