Factors Influencing Physical Activity Levels in Children with Asthma;
全文
(2) 206. in the United States [6], the United States Health Interviews Survey reported that 30% of children with asthma had limited physical activity [7]. Children with asthma in the U.S. [8] and Taiwan [9] were reported to be less active than their peers. Understanding the determinants of physical activity among children with asthma will be very important to developing appropriate strategies for increasing their physical activity. Besed on the United States Surgeon General's report that emphasized the relationships between physical activity and health [10], several international recommendations of physical activity for children and adolescents have been developed and evaluated [11,12]. First, Sallis and Patrick established the Physical Activity Guidelines for Adolescents (PAGA) [13], which recommended that children and adolescents participate in more than 90 minutes per week of moderate-to-vigorous physical activity (MVPA). Second, the Healthy People 2010 objective No. 22.6 recommended that children participate in more than 150 minutes per week of MVPA. Third, the Healthy People 2010 objective No. 22.7 suggested that children take part in a minimum of 60 minutes per week of vigorous physical activity (VPA) [14]. Fourth, the guidelines for children and adolescents in the United Kingdom Expert Consensus recommended that children participate in more than 420 minutes per week of MVPA [15]. Most of the recommendations were established by computing the minutes per week of MVPA and VPA. The international recommendations of physical activity for children and adolescents were also appropriate for normal development of children with asthma. Few studies have focused on the behavioral factors that influence the amount of physical activity that healthy children and children with asthma participate in. Personal, interpersonal and environmental factors must be considered in physical activity studies [10]. Some factors that have been found to influence the physical activity of children are gender (boys are more active than girls) [16,17], and disease severity (moderately to severely ill children are less active than healthy. Physical Activity of Children with Asthma. children) [13,18]. A recent study found that perceived competence in engaging in physical activity among children with asthma was significantly correlated with aerobic fitness [17]. Physical self-perception, one aspect of selfconcept (a psychological dimension), has been shown to affect the level of physical activity and physical fitness of healthy children [19]. Perceived health status is another factor that affects health behaviors [20] and was a strong predictor of physical inactivity in the Ontario Health Survey [21]. According to Prochaska and DiClemente's Transtheoretical Theory [22], an individual's intention to change the behavior of physical activity is considered an important factor in motivating people to exercise [23]. There is a relationship between environmental factors, such as access to exercise and physical activity [15]. Access to exercise programs has been shown to significantly increase participation in physical activity among adolescents [24]. Therefore, this study was designed to describe the level of physical activity of children with asthma in Taiwan and to explore predictive factors influencing physical activity levels in this population. The ten factors explored included personal factors (gender, age), disease-related factors (asthma severity, EIA), psychological factors (stage of change, perceived health status, physical self-concept), and environmental factors (access to exercise information, access to exercise facilities, and access to team sports). MATERIALS AND METHODS Participants. This cross-sectional survey of children with asthma was conducted at three medical centers in Taiwan. Data were collected from questionnaires and activity logs completed by children and from interviews with their parents from October 2001 to December 2001. To be eligible for participation in the study, children needed to be from 8 to 11 years of age, have physician-diagnosed asthma [25], be clinically stable and show no signs of any other chronic disease or major physical disabilities. Of the 173 children recruited, 152.
(3) Shao-Keh Hsu, et al.. completed the questionnaire with their parent's informed consent. Nineteen children did not finish the questionnaire completely. The final sample of 152 asthmatic children with valid data resulted in a response rate of 87.9%. No significant differences in demographic data were found between participants who completed the questionnaire and those who did not. Sample size (N = 152) was determined by power analysis of sampling; the significance levels were set as follows: α = 0.05, correlation = 0.4, and power level = 0.78 [26]. Questionnaire and activity log. Data on the predictive factors influencing physical activity levels were collected from a structured, self-administered questionnaire with 10 factors in four categories. Data on physical activity levels were collected from a three-day physical activity log (3-dPAL). The four categories were personal, disease-related, psychological and environmental predictive factors. Personal factors included gender and age. Disease-related factors included asthma severity and the frequency of EIA during the previous year. Asthma severity was divided into four grades (intermittent mild, mild continuous, moderate, and severe), according to the Global Initiative for Asthma [27]. Psychological factors included the contemplation stage of changing exercise behavior, perceived health status and physical self-concept. Stage of change was classified using the five stages of Transtheoretical Theory [27,28]. Perceived health status was assessed by a four-item, five-point Likert's scale modified from the Perceived Health Status scale [28,29]. Cronbach's α for the internal consistency of this scale used in the present study was 0.71. Physical self-concept was evaluated using a sixpoint, 29-item Likert's scale originally developed by Fox and Marsh [30,31] and modified for use in Taiwan by Chung [32]. This scale, which measures perceptions about one's flexibility, tolerance, agility, obesity, appearance and strength, had good reliability (α = 0.80) and construct validity. Higher scores indicated a more positive physical self-concept. Cronbach's α for. 207. this scale in our study was 0.89. The 3d-PAL was used to measure physical activity level at 15-minute intervals during the previous week. This instrument, designed by Bouchard et al [33] has been used as a convenient measure of physical activity among school-aged children in Taiwan. This instrument has good testretest reliability (r = 0.88), good criterion validity (r = 0.74) and gives results consistent with 7-day measures of physical activity level [34]. Each child was asked to record one of nine levels of physical activity on one weekday, one Saturday and one Sunday during the previous seven days. The nine physical activity levels were: level 1, sleep; levels 2 to 5, mild activity; levels 6 to 7, moderate activity and levels 8 to 9, vigorous activity. A pilot study was conducted to test the comprehension and responsiveness of 15 schoolaged children to the questionnaire. Test-retest reliability in this study was 0.78. Based on the pilot study results, the instrument was refined to be as clear as possible; for example, we provided the Chinese pronunciation of difficult words and designed a sample answer demo sheet. After these corrections, most school-aged children were able to understand the 3d-PAL. Data analysis. SPSS for Windows (version 10.0) was used to analyze descriptive and inferential statistics. The level of significance was set at α = 0.05. MVPA was classified as the time children spent at levels 6 to 9 during the previous seven days (min/wk). VPA was classified as the time that children took part in levels 8 to 9 activities (min/wk). Multiple Regression analysis was used to determine predictors of physical activity. Collinearity diagnosis was used to examine the interrelationship between factors when tested by Multiple Linear Regression. This diagnosis indicated that the interrelationship among the ten variables was low; the variance inflation factor (VIF) of predictors was around 1; the tolerance ranged from 0.7 to 0.9, and the conditional indexes were less than 30 [35]..
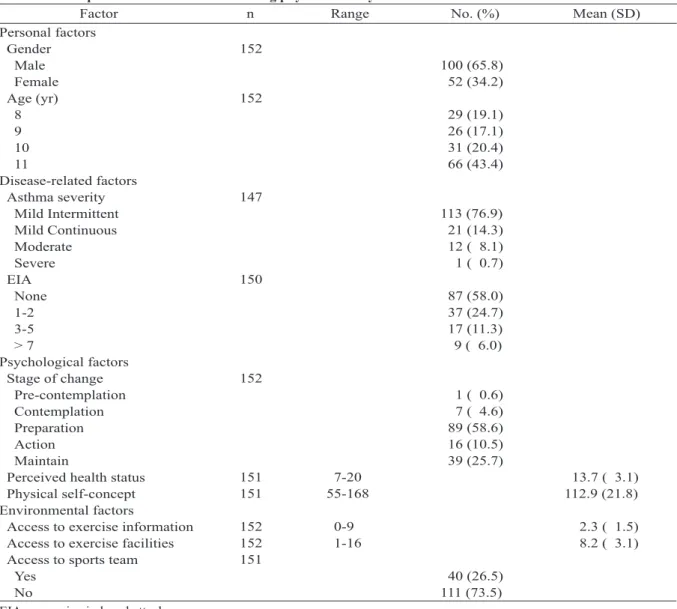
(4) 208. Physical Activity of Children with Asthma. RESULTS Participants. Of the 152 participants, 65.8% were boys and 34.2% were girls. The mean age was 9.88 years (SD = 1.17) (Table 1). Asthma severity was mild in most of the children (n = 134, 88.1%), moderate in 12 children (8.1%), and severe in one child (0.7%). Nearly half of the children had experienced EIA at least once in the previous year (n = 63, 42%). Only 39 children (25.7%) reported taking part in regular physical activity. More than half of the children (n = 97, 63.9%) did not regularly participate in physical activity. These children felt that their health status was moderate to good and that they had a moderately positive. physical self-concept. Their access to information about exercise for children was quite low, with a mean of 2.3 (SD = 1.5). Participants reported, on average, access to 8 exercise facilities, with a range of 1 to 16. Only 40 children (29.5%) had the opportunity to engage in team sports. Levels of physical activity. Thirty participants (19.7%) were defined as being inactive because they performed no moderate or vigorous activity during the seven days preceding the survey [10]. More than half of the children (n = 92, 60.5%) participated in more than the PAGA– recommended 90 min/wk of MVPA, and 62 children (40.8%) took part. Table 1. Descriptive data on factors influencing physical activity of children with asthma n Factor Range No. (%) Personal factors 152 Gender 100 (65.8) Male 52 (34.2) Female 152 Age (yr) 29 (19.1) 8 26 (17.1) 9 31 (20.4) 10 66 (43.4) 11 Disease-related factors 147 Asthma severity 113 (76.9) Mild Intermittent 21 (14.3) Mild Continuous 12 ( 8.1) Moderate 1 ( 0.7) Severe 150 EIA 87 (58.0) None 37 (24.7) 1-2 17 (11.3) 3-5 9 ( 6.0) >7 Psychological factors 152 Stage of change 1 ( 0.6) Pre-contemplation 7 ( 4.6) Contemplation 89 (58.6) Preparation 16 (10.5) Action 39 (25.7) Maintain 151 7-20 Perceived health status 151 55-168 Physical self-concept Environmental factors 152 0-9 Access to exercise information 152 1-16 Access to exercise facilities 151 Access to sports team 40 (26.5) Yes 111 (73.5) No EIA = exercise-induced attack.. Mean (SD). 13.7 ( 3.1) 112.9 (21.8) 2.3 ( 1.5) 8.2 ( 3.1).
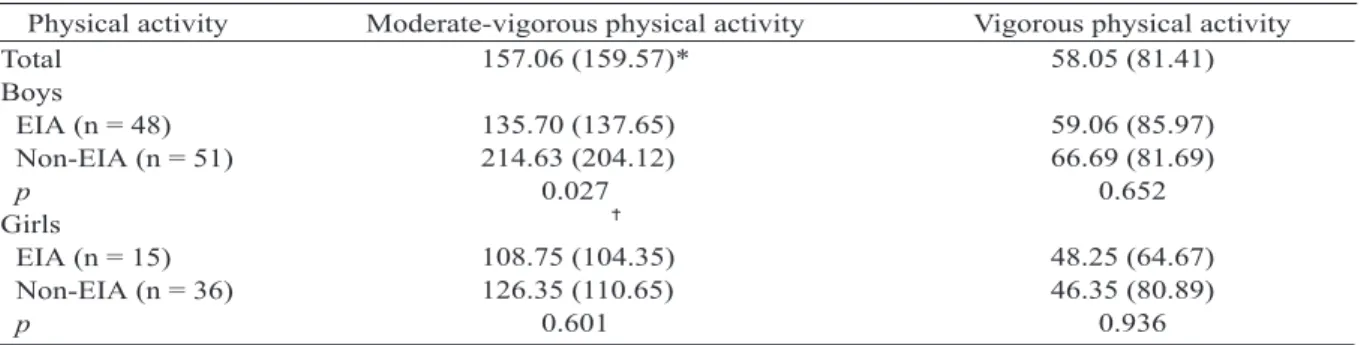
(5) Shao-Keh Hsu, et al.. in more than 150 min/wk of MVPA as recommended in the Healthy People 2010 objective No.22.6. Fifty children (32.9%) participated in more than 60 min/wk of VPA as recommended in the Healthy People 2010 objective No.22.7. Only eleven children (7.2%) participated in more than the UK experts consersus-recommended 420 min/wk of MVPA. The levels of physical activity recorded in the 3dPAL varied greatly among participants (Table 2). The variations in MVPA ranged widely, from zero to 911.25 min/wk, with a mean 157.06 min/wk. Levels of VPA were also quite dispersed, ranging from zero to 315 min/wk, with a mean 58.05 min/wk. Boys with asthma engaged in more MVPA than girls with asthma (t = 2.195, p = 0.014). The amount of MVPA differed between boys with and those without EIA. Predictors of physical activity. Of the 10 factors examined as predictors of physical activity, only four were entered into the stepwise multiple regression analysis: access to. 209. exercise facilities, EIA, gender, and access to sport teams (Table 3). None of the psychological factors influenced the time spent participating in physical activity. Access to exercise facilities, gender and EIA significantly and positively influenced the children's MVPA, explaining 13% of the variance in MVPA. Access to sport teams predicted only vigorous physical activity, with an R2 value of 0.037. Gender, EIA, and MVPA. The above results indicate that MVPA was significantly influenced by gender, EIA and access to exercise facilities. Further comparison of the influences of gender and EIA interaction on physical activity levels revealed that these factors significantly influenced MVPA in asthmatic boys with EIA (Table 2), but not in asthmatic girls with EIA. General Linear Model/Univariance testing of the interaction between gender and EIA indicated that gender affected only MVPA. EIA significantly affected boys with asthma. Neither gender nor EIA, or their interaction had a significant effect on VPA.. Table 2. Comparison of the influence of exercise-induced attack (EIA) and gender on physical activity (min/wk) in children with asthma Physical activity Moderate-vigorous physical activity Vigorous physical activity 157.06 (159.57)* 58.05 (81.41) Total Boys 135.70 (137.65) 59.06 (85.97) EIA (n = 48) 214.63 (204.12) 66.69 (81.69) Non-EIA (n = 51) 0.027 0.652 p Girls 108.75 (104.35) 48.25 (64.67) EIA (n = 15) 126.35 (110.65) 46.35 (80.89) Non-EIA (n = 36) 0.601 0.936 p. *Mean. SD. p < 0.05.. Table 3. Stepwise multiple regression of physical activity (min/wk) in children with asthma Moderate-vigorous physical activity Vigorous physical activity Predictor (β) (β) 0.235 Access to exercise facilities 0.237 EIA 0.204* Gender 0.193* Access to sport teams 0.130 0.037 R2 < 0.0001 0.017 p. *p < 0.01, p < 0.001..
(6) 210. Physical Activity of Children with Asthma. DISCUSSION. In this study, children with asthma engaged in physical activity at levels far below those recommended by the Healthy People 2010 objectives [10]. Of this sample, 19.7% were inactive, which is much higher than the target level, even for children with mildly to moderately severe asthma. According to the PAGA [13], children should engage in MVPA for ≥ 30 minutes at least 3 times per week. Only 60.5% of children in the present study (n = 92) participated in more than 90 min/wk of MVPA. The Healthy People 2010 objective No.22.7 states that children should engage in vigorous physical activity ≥ 20 minutes at least three times per week. Less than a third of the children with asthma (n = 50, 32.9%) in this study participated in more than 60 min/wk of VPA. This study explored and evaluated 10 factors which influence the physical activity levels in 152 children with asthma. Of these 10 factors, access to exercise facilities was the most significant predictor of MVPA in children with asthma. This predictor is a modifiable factor influencing physical activity behavior. This finding is consistent with other studies in healthy children [20,36] and supports the general premise that providing a supportive exercise environment will motivate children to participate in MVPA. Our findings go beyond those of previous studies on physical activity in children with asthma, which did not include environmental factors. We analyzed the 10 factors as competitive variables using regression analysis to predict the dependent variables. Environmental factors were shown to be more important than psychological factors. Pediatric clinicians should suggest that parents create more exercise facilities and motivate their asthmatic children to exercise. We also found that gender and EIA predicted which asthmatic children were at risk for physical inactivity. Girls engaged in MVPA significantly less than boys with asthma, indicating that girls need more encouragement to engage in exercise. Participation in teams sports was a predictor of VPA (Table 3). Whether gender. differences in MVPA are due to participation in sporting activities was not validated in the present study. EIA was the factor that most impacted the physical activity of children with asthma, especially in boys (Tables 2, 3). A gender difference in physical activity has been reported in many studies on healthy children [16,17]. Among healthy children, girls are always less active than boys. Trost et al [37] found that participation in sports was the primary cause for gender differences in activity of healthy schoolaged children. Pianosi reported no gender differences in BMI, asthma severity and physical fitness in children with asthma [18]. EIA, not gender, may be the main factor affecting the physical activity of children with asthma. The prevalence of EIA in the present study was 42%, a figure far less than the 90% prevalence of asthma reported by Milgrom el al [38]. This result could be because EIA frequently goes undiagnosed. They also found that 50% of asthmatic children with a negative history for EIA had a positive response to exercise challenge [38]. The limitation in this study was that EIA was measured by self-report questionnaires, which was not as precise as the exercise challenge test. Children's reporting is often doubted because of their memory and the perception about EIA. Therefore, there is a need for further study to differentiate between perceived and actual EIA. Regardless of whether EIA is perceived or actual, pediatric clinicians have to understand the patient's condition and provide necessary suggestions or treatment. Appropriate prevention strategies, such as adequate warm-up and cooldown periods, and medical therapy for EIA during exercise periods have been recommended to achieve a normal level of physical activity for children with asthma [39,40]. Although the 3d-PAL is a precise and valid tool for measuring physical activity, the findings of this study are still limited because we did not use an objective measure of physical activity and did not perform long-term monitoring. A more accurate measurement of physical activity could provide more sensitive measurements of different levels of physical activity and yield more accurate.
(7) Shao-Keh Hsu, et al.. findings. The ten predictive factors of physical activity used in the regression analysis were not totally accounted for in the model; 87% of the variance in MVPA could not be explained. The failure to predict physical activity from psychological factors is disappointing, since such factors are modifiable and could be enhanced by patient education. Accurate diagnosis of EIA by biological measurement is suggested for further research. The results of this study indicate that pediatric practitioners should encourage children with asthma to be more physically active. They should also advise parents to provide an environment that supports exercise. Pediatric physicians also should give appropriate medication to prevent and treat EIA. Parents and schoolteachers also have to encourage girls with asthma to be more active. Assessing physical activity levels, providing medications to prevent EIA before exercise, and teaching children with asthma to follow exercise guidelines should be standard clinical practices in asthma clinics. ACKNOWLEDGMENTS. This study was supported by a grant from the National Science Council in Taiwan (NSC-902314-B-241-001). The authors sincerely thank all of the participants, their parents, and doctors who helped in the three pediatric clinics. REFERENCES 1. Lu KH, Hsieh KS. The changing of allergy disease during past decade in Taipei. Acta Pediatr Sin 1988; 29:104-9. 2. Sears MR. Epidemiology of childhood asthma. [Review] Lancet 1997;350:1015-20. 3. Worsnop CJ. Asthma and physical activity. Chest 2003;124:421-2. 4. Telama R, Yang X, Laakso L, et al. Physical activity in childhood and adolescence as a predictor of physical activity in young adulthood. Am J Prev Med 1997;13: 317-23. 5. Wilkerson RR. Younger and older children had different experiences of asthma and its management. Evid Based Nurs 2002;5:123. 6. National Asthma Education and Prevention Program.. 211. Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma. Bethesda: National Institutes of Health, 1997. NIH publication 97-4051. 7. Taylor WR, Newacheck PW. Impact of childhood asthma on health. Pediatrics 1999;90:657-62. 8. Lang MD, Butz AM, Duggan AK, et al. Physical activity in urban school-aged children with asthma. Pediatrics 2004;113:341-6. 9. Chiang LC, Huang JL, Fu LS. Physical activity and physical self-concept: comparison between children with and without asthma. J Adv Nurs 2006;54:653-62. 10. US Department of Health and Human Services. Physical activity and health: A report of the surgeon general. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control, Chronic Disease Prevention and Health Promotion. The President's Council on Physical Fitness and Sports. 1996. 11. Pate RR, Freedson PS, Sallis JF, et al. Compliance with physical activity guidelines: prevalence in a population of children and youth. Ann Epidemiol 2002;12:303-8. 12. Liou YM, Chiang LC. Levels of physical activity among school-age children in Taiwan: a comparison with international recommendations. J Nurs Res 2004; 12:307-16. 13.Sallis JF, Patrick K. Physical guidelines for adolescents: consensus statement. Pediatr Exer Sci 1994;6:302-14. 14. Welk GJ. Physical activity assessments for healthrelated research. Champaign, IL: Human Kinetics Publishers, 2002. 15. Cavill N, Biddle S, Sallis J. Health enhancing physical activity to young people: Statement of the United Kingdom Expert Consensus Conference. Pediatr Exer Sci 2001;13:12-25. 16. Taylor WC, Sallis JF. Determinants of physical activity in children. In: Simopolous, AP, Pavlou KN, eds. Nutrition and Fitness: Metabolic and Behavioral Aspects in Health and Disease, Basel. Switzerland: Krager, 1997:159-67. 17. Sallis JF, Zakarian JM, Hovell MF, et al. Ethnic, socioeconomic, and sex differences in physical activity among adolescents. J Clin Epidemiol 1996; 49:125-34. 18. Pianosi PT, Davis HS. Determinants of physical fitness in children with asthma. Pediatrics 2004;113(3):e2259..
(8) 212. 19. Raudesepp L, Liblik R, Hannus A. Children's and adolescents' physical self-perceptions as related to moderate to vigorous physical activity and physical fitness. Pediatr Exer Sci 2002;14:97-106. 20. Pender NJ, Walker SN, Sechrist KR, et al. Predicting health-promoting lifestyles in the workplace. Nurs Res 1990;39:326-32. 21. Allison KR. Predictors of inactivity: an analysis of the Ontario Health Survey. Can J Public Health 1996;87: 354-8. 22. Prochaska Jo, Velicer WF. The transtheoretical model of health behavior change. [Review] Am J Health Promot 1997;12:38-48. 23. Walton J, Hoerr S, Heine L, et al. Physical activity and stages of change in fifth and sixth graders. J Sch Health 1999;69:285-9. 24. Garcia AW, Broda MA, Frenn M, et al. Gender and developmental differences in exercise beliefs among youth and prediction of their exercise behavior. J School Health 1995;65:213-9. 25. Department of Health. Guidelines for asthma diagnosis and treatment. Taipei: Department of Health, Taiwan (Republic of China), 2002. 26. Borenstein M, Rothstein H, Cohen J, et al. Sample power (2.0). SPSS, Inc., 2000. 27. Global Initiative for Asthma: Global strategy for asthma management and prevention. Updated from NHLBI/WHO Workshop Report. Bethesda: National Institute of Health, 2002. NIH publication 02-3659. 28. Yoos H, McMullen A, Bezek S, et al. An asthma management program for urban minority children. J Pediatr Health Care 1997;11:66-74. 29. Hunt SM, McKenna SP, McEwen J, et al. A quantization approach to perceived health status: a validation study. J Epidemiol Community Health 1980; 34:281-6. 30. Fox KR, Corbin CB. The physical self-perception profile: development and preliminary validation. J Sport Exerc Psychol 1989;11:408-30.. Physical Activity of Children with Asthma. 31. Marsh HW. Physical fitness self-concept: relations to field and technical indicators of physical fitness for boys and girls aged 9-15. J Sport Exerc Psychol 1993; 15:184-206. 32. Chung BF. The construct of physical self-concept and its relations to a construct of physical fitness among children, Taiwan. Taipei: National College of Physical Education and Sports, 1996. (Thesis) 33. Bouchard C, Tremblay A, Leblanc C, et al. A method to assess energy expenditure in children and adults. Am J Clin Nutr 1983;37:461-7. 34. Lu CM, Lee MS, Chen SC. Determinants of physical activity in urban primary school children. J Health Educ (Taiwan) 2000;14:95-111. 35.Betsley DA, Kuh E, Welsch RE. Regression diagnostics: identifying influential data and sources of collinearity. New York: Jones Wiley, 1980. 36. Zakarian JM, Hovell MF, Hofstetter CR, et al. Correlates of vigorous exercise in a predominantly low SES and minority high school population. Prev Med 1994;23:314-21. 37. Trost SG, Pate RR, Dowda M, et al. Gender differences in physical activity and determinants of physical activity in rural fifth grade children. J School Health 1996;66:145-50. 38. Milgrom H, Taussig LM: Keeping children with exercise-induced asthma active. [Review] Pediatrics 1999;104(3):e38. 39. Clark CJ, Cochrane LM. Physical activity and asthma. [Review] Curr Opin Pulm Med 1999;5:68-75. 40. National Heart, Lung, and Blood Institute: Asthma & Physical Activity in the School: Making a Difference. National Asthma Education and Prevention Program (NAEPP): School Asthma Education Subcommittee. U.S. Department of health and human services, Public Health Service, National Institutes of Health, 1995. NIH publication 95-3651..
(9) 213. 1. 2. 3 1. 2. 3. 152. 8. 11. 3. 32.9% 2010. 20 85% (p < 0.001). 2006;11:205-13. 404. 91. 2006. 6. 2. 2006. 8. 25. 2006. 8. 18.
(10)
數據
相關文件
This paper will present a Bayes factor for the comparison of an inequality constrained hypothesis with its complement or an unconstrained hypothesis. Equivalent sets of hypotheses
Sexual Abuse of Children with Autism: Factors that Increase Risk and Interfere with Recognition of Abuse.... ASD –
The IEC endeavours to ensure that the information contained in this presentation is accurate as of the date of its presentation, but the information is provided on an
When risk factors are high and protective factors are low, proximal risk factors. (or stressors) can interact with a person’s long term or underlying
The fuzzy model, adjustable with time, is first used to consider influence factors with different features such as macroeconomic factors, stock and futures technical indicators..
Peppard, J., “Customer Relationship Management (CRM) in Financial Services”, European Management Journal, Vol. H., "An Empirical Investigation of the Factors Influencing the
The purposes of this research are to find the factors of raising pets and to study whether the gender, age, identity, marital status, children status, educational level and
To understand the Internet addiction behaviors, this study inquires the personal and family related factors, online experience related factors, interpersonal interactions