O
UTPATIENT
D
RUG
E
XPENDITURES
AND
P
RESCRIPTION
P
OLICIES
FOR
D
ISEASES
WITH
H
IGH
C
OST
TO
THE
N
ATIONAL
H
EALTH
I
NSURANCE
S
YSTEM
IN
T
AIWAN
Hui-Chu Lang,1 Mei-Shu Lai,2 and Gau-Tzu Chen3
1Institute of Hospital and Health Care Administration, National Yang-Ming University, Taipei; 2Institute of Preventive Medicine,
School of Public Health, National Taiwan University, Taipei; 3Koo Foundation Sun Yat-Sen Cancer Center, Taipei, Taiwan.
Received: 17 April 2003 Revised: 1 August 2003 Accepted: 4 November 2003
Reprint requests and correspondence to: Dr. Hui-Chu Lang, Institute of Hospital and Health Care Administration, National Yang-Ming University, No. 155 Li-Nong Street, Section 2, Taipei 112, Taiwan.
Background and Purpose: The high cost of drugs, particularly those used to treat upper respiratory tract infections, is an increasingly important problem for the National Health Insurance system in Taiwan. This study proposed a new classification scheme for reimbursing drug cost and estimated its impact on expenditures and health care utilization.
Methods: Data were obtained from the National Health Research Institutes’ year 2000 computer file of the National
Health Insurance Academic Research Database in Taiwan. Two factors were used to classify medications: 1) urgency of medications required; and 2) patient’s self-care ability.
Results: Among the 10 diseases with the highest number of outpatient department (OPD) visits, 7 were upper
respiratory diseases. Acute upper respiratory infections (URIs) and acute nasopharyngitis were the 2 diseases with the highest number of OPD visits. Drug expenditure for acute URIs is about 6% of total expenditure for drugs. Medications suitable for URIs patients’ self-care accounted for 42.8% of the total cost of prescribed drugs for these illnesses, and treatment medications unsuitable for patients’ self-care accounted for 48.6%. Other medications used for URIs could not be grouped into these categories. The total expenditure for acute nasopharyngitis was about 1.3% of total expenditure for drugs. Medications suitable for self-care in patients with nasopharyngitis accounted for 51.8% of the total cost of medication prescribed for this illness, and medications unsuitable for patients’ self-care accounted for 36.8%.
Conclusions: Reducing the medications suitable for patients’ self-care and enforcing different levels of payment rates
on medications unsuitable for patients’ self-care may reduce the excessive use of OPD drugs, improve the appropriateness of utilization for acute URIs and the common cold, and allow medical resources to be distributed more efficiently.
Key words: Economics, pharmaceutical; Health expenditure; Health insurance; Respiratory tract infections
J Formos Med Assoc 2004;103:280-5
Expenditures by the National Health Insurance (NHI) system in Taiwan have increased each year since its inauguration on March 1, 1995. Based on the 2002 re-port of NHI statistics for the year 2001,1 drug
expendi-tures for health care in 2001 reached 82,400,000,000 New Taiwan Dollars (NTD) [equivalent to US$2,459, 701,493, where 1 NTD = 33.5 US$]. Drug expenditures accounted for 26% of these costs and the costs for drugs distributed at clinics accounted for 30% of the total medical costs for outpatient service department (OPD) expenditures. These percentages for drug costs are significantly higher than those in European countries.2 Therefore, OPD medical care utilization,
especially the appropriateness of OPD drugs prescribed with regard to control of their quality and costs, is an
important factor in determining the feasibility of the continuation of the NHI program.
Upper respiratory diseases are among the most important and the most frequent disease categories responsible for OPD visits. Although they are rarely fatal, upper respiratory diseases have a great impact on the patient’s quality of life and often lead to pa-tients taking time off from work or school because of physical discomfort; thus, the social costs of upper respiratory diseases are fairly high.3 Upper respiratory
tract infections (URIs) are usually self-limiting and subside with time. According to evidence-based medi-cine, few URIs can be cured effectively by prescription drugs. Nevertheless, prescription drugs are often over-used for the treatment of URIs,4 and sometimes may
cause serious side effects.5,6 Clinical reports have cited
the overuse of antibiotics, which do not shorten the course of acute infections due to viruses or prevent subsequent bacterial infections.7,8
A study9 found that people in Japan averaged 16.0
OPD visits per person in 1998, while visits for URIs (International Classification of Diseases, 9th edition, Clinical Modification [ICD-9-CM]: 460-465 or A-code: A312) accounted for only 6.0% of the total number of OPD visits, and the cost of drugs for URIs accounted for only 2.6% of the total costs of OPD drugs. In comparison, year 2000 data in Taiwan showed a lower average number of visits per person (13.6 vs 16.0), but the average OPD visit for URIs accounted for 30.5% of the total number of OPD visits, far more than that in Japan. The cost of drugs prescribed for URIs accounted for 13.5% of the total OPD drug costs, with up to 94% of patients receiving prescriptions for URIs. This suggests an inadequate understanding of upper respiratory diseases in Taiwan, and that little importance is attached to self-care, with heavy reliance on the use of drug treatment.
In many countries, drugs covered by insurance systems are divided into prescription drugs and non-prescription (over the counter [OTC]) categories. Generally, payment for OTC drugs is not covered by health plans. In terms of prescription drugs, few insurance systems or providers cover full payment of all prescription drugs. Some insurance plans cover costs of prescription drugs, some cover part of the costs, and some do not cover them at all. In general, insurance companies’ formularies are based on the safety, cost, and efficacy of the drugs. Many private health insurance plans now offer incentive-based formularies, in which drugs are placed into different tiers. Under these plans, most drugs are covered, but enrollees pay different copayments depending on the tier to which a drug is assigned. Two-tier plans are commonplace, with a higher copayment for brand name drugs than generic drugs. However, an increas-ing number of employers are offerincreas-ing 3-tier benefits with 3 copayment levels. These plans typically set the lowest copayment for generic drugs, the middle copayment for formulary or preferred brands, and the highest copayment for non-formulary brands.
Four plans have been proposed for NHI drug payments by the Benefit Plan for NHI Drugs sub-committee of the Medical Care Resource Allocation Group, Second Generation NHI Research Team in Taiwan.10 The first plan follows the current policy
which does not cover any expenditure for OTC drugs. The second plan reduces the benefit coverage of NHI drugs gradually. The third plan classifies health care drugs according to the character and the type of treatment and then sets different coinsurance rates.
The fourth plan sets 3-tier beneficiary deduction plans for all OPD drugs.
This study grouped medications according to the classification methods adopted by the second and third plans listed above to access doctors’ current pre-scribing habits for diseases with high OPD utilization in Taiwan and to predict the possible benefits of each of the different payment policies after this classifi-cation method is adopted.
Theoretically, use of the 2 plans that reduce the range of drugs paid for by NHI or setting different copayment rates according to the character and type of treatment may reduce the possibility of problems such as medical accessibility and the progression of minor ailments into fatal diseases if only hospital-ization cases, but not OPD visits, are covered by insur-ance (that is, a policy which insures for catastrophic but not minor illnesses). It may also lead to more efficient use of medical resources, so that drug expenditures for health care will be reduced.
The specific aims of this study were as follows. First, we aimed to determine the 10 clinical diseases accounting for the highest number of OPD visits. Then, using the 2 diseases with the highest number of OPD visits as examples, we estimated the possible impact on costs if the policy proposed above — that is, gradually reducing the scope of payment of NHI drugs and setting different copayment rates according to the type of treatment — was adopted.
M
ethods
Data in this study were obtained from National Health Research Institutes’ year 2000 records of the National Health Insurance Academic Research Database. The database includes files on ambulatory care expendi-tures by visit and details of ambulatory care orders. Both files were systematically sampled using data from 1 in every 500 cases. The 2 files were merged by identification codes. Then, the files were combined according to NHI drug constituent reimbursement category and Anatomical Therapeutic Chemical (ATC) code.
However, because the file of ambulatory care ex-penditures by visits and the file of details of ambulatory care orders were obtained by systematic sampling (i.e., 1/500), and because combination variables such as the ATC code had missing values, it was difficult to accurately estimate the actual totals in this study. Therefore, percentages were adopted to show the estimated results. Totals were obtained by multiplying 500 by the sum in the details of ambulatory care orders file, and the amount of expenditure for each category was obtained by multiplying the totals by the percent-age. Because ICD-9-CM was adopted as the disease
classification system in the year 2000, payment cannot be made by the NHI if classification is done by the A-code; thus, only a few records still use the A-code (a simplified patient classification system that is only used in Taiwan). Compared with the ICD-9 codes, the A-code classification system is rather imprecise and may include several ICD-codes in a single A-code (for example, A-code A321 covers ICD-9 codes 460, 461, 462, and 465), making it impossible to calculate the incidence of the individual diseases. According to our calculations, 5% of patients were claimed with an A-code. In this study, files that used the A-code were not included in the final calculations, and con-sequently, the total expenditures estimated in this study may be lower than the real expenditures.
The 10 OPD diseases with the highest number of OPD visits in NHI were determined by referring to the first 3 digits of ICD-9-CM codes for diseases in the ambulatory care expenditures by visits file. The second and the third plans proposed by the Medical Care Resource Allocation subcommittee of the second-generation NHI were then applied, which respectively aim to reduce the benefit coverage of NHI drugs gradually and set different copayment rates according to the character and the type of treatment, and then classify health care drugs. The following 2 factors are considered in the classification:11 urgency of
medi-cations required and the patient’s self-care ability. In terms of urgency of medications, there are 3 levels: A) medications used when life is threatened; B) medi-cations used to treat and control common diseases; and C) medications mainly used to eliminate symp-toms. In terms of the patient’s self-care circumstances, there are 2 levels: 1) medications unsuitable for patients’ self-care; and 2) medications suitable for patients’ self-care. Taking these 2 classification factors together, medications can be grouped into 1 of 6 types — A1, B1, C1, A2, B2, and C2, with an additional group for medications that cannot be grouped or with evident controversy. In this study, classification was done by an experienced clinical pharmacist. The percentage of each type of medication and the total
medical care expenditure were then calculated. Based on the 2 diseases with the highest number of OPD visits, this study estimated the possible impacts of instituting the new policy mentioned in this study (gradually reducing the scope of payment of NHI drugs and setting different copayment levels accord-ing to the type of treatment).
R
esults
Diseases with the highest number of OPD
visits
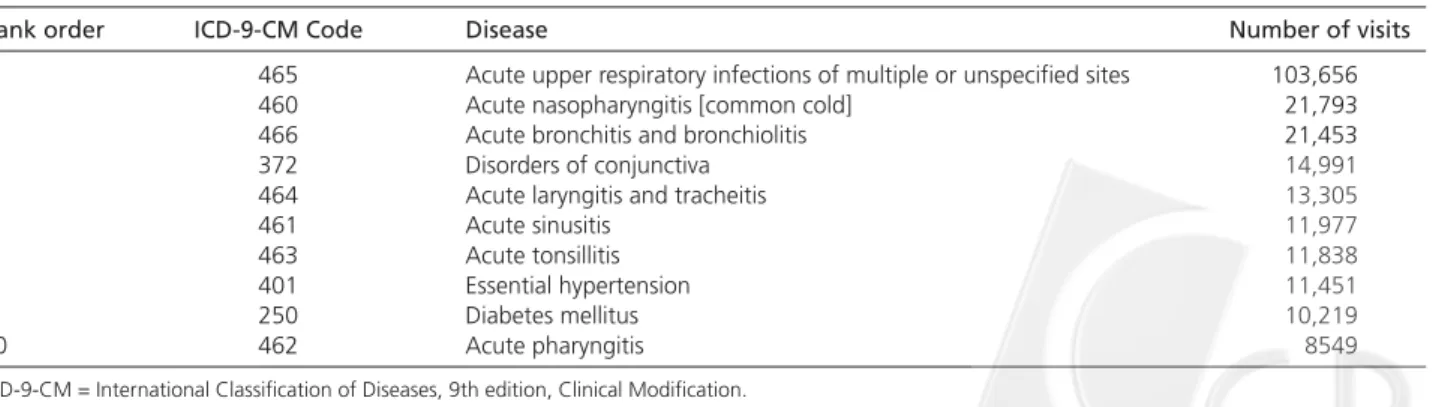
Among the 10 diseases with the highest number of OPD visits, 7 were upper respiratory diseases. These included, in rank order, acute URIs (first; ICD-9: 465), acute nasopharyngitis (common cold; second; ICD-9: 460), acute bronchitis and bronchiolitis (third; 9: 466), acute laryngitis and tracheitis (fifth; ICD-9: 464), acute sinusitis (sixth; ICD-ICD-9: 461), acute tonsillitis (seventh; ICD-9: 463), and acute pharyngitis (tenth; ICD-9: 462) [Table 1].
Drug cost distributions for acute URI and
common cold
In this study, we analyzed the 2 diseases with the highest OPD utilization rate, that is, acute URIs and acute nasopharyngitis (common cold). Table 2 shows the total costs and drug costs alone of URIs and common cold. As expected, health care costs were significantly different among hospital levels, departments and patients of different ages. Primary care clinics had the lowest claims for URIs in both total cost (range, 319 to 564 NTD) and drug cost (range, 91 to 247 NTD) per visit. Similar results were found for common cold in total cost (range, 316 to 605 NTD) and drug cost (range, 92 to 230 NTD) per visit. In terms of department and patient age, although significant differences were found within departments and patient age groups, these cost differences were much smaller compared with the effect of hospital level.
Table 1. Diseases with the highest number of outpatient department visits for the year 2000.
Rank order ICD-9-CM Code Disease Number of visits
1 465 Acute upper respiratory infections of multiple or unspecified sites 103,656
2 460 Acute nasopharyngitis [common cold] 21,793
3 466 Acute bronchitis and bronchiolitis 21,453
4 372 Disorders of conjunctiva 14,991
5 464 Acute laryngitis and tracheitis 13,305
6 461 Acute sinusitis 11,977
7 463 Acute tonsillitis 11,838
8 401 Essential hypertension 11,451
9 250 Diabetes mellitus 10,219
10 462 Acute pharyngitis 8549
Effect of gradually reducing scope of NHI
prescription benefit
We classified drug expenditures (excluding pharmacy service fees) for each disease according to the classifi-cation method mentioned above in order to predict the possible impact of adopting different NHI drug benefit plans. The health care data were obtained from the National Health Research Institutes’ records for the year 2000.
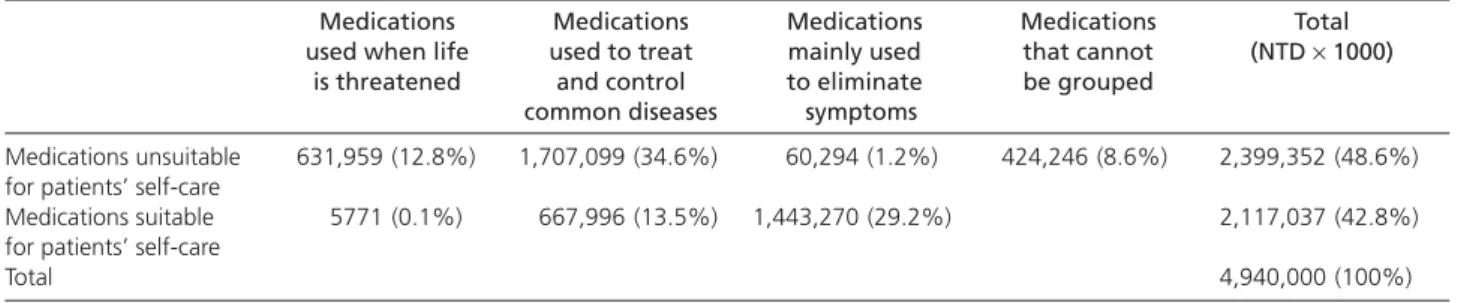
The results in Table 3 show that drug expenditures for acute URI were about 4,940,000,000 NTD, which was 6.0% of total expenditure for drugs. Among the total, medications unsuitable for patients’ self-care accounted for 48.6% (A1 + B1 + C1); medications suit-able for patients’ self-care accounted for 42.8% (A2 + B2 + C2); and medications that could not be grouped accounted for 8.6%. Among medications unsuitable for patients’ self-care, medications used for life-threatening ailments accounted for 12.8% ; medications used to treat and control common diseases accounted for 34.6%; and medications mainly used to eliminate symptoms accounted for only 1.2%. Among medications
suitable for patients’ self-care, medications used to treat and control common diseases (B2) accounted for 13.5% and medications mainly used to eliminate symptoms (C2) accounted for 29.2%.
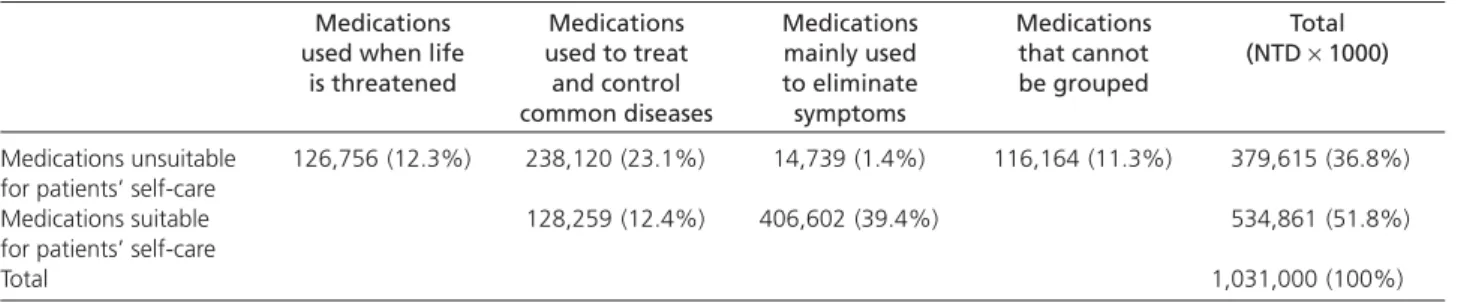
The classification of medications used to treat acute nasopharyngitis (common cold) is shown in Table 4. The total drug expenditure for acute naso-pharyngitis was about 1,031,000,000 NTD, which was 1.25% of total expenditure for drugs. Medications unsuitable for patients’ self-care accounted for 36.8%, medications suitable for patients’ self-care accounted for 51.8%, and medications that could not be grouped accounted for 11.3%. Among medications unsuitable for patients’ self-care, medications used for life-threatening events accounted for 12.3%, medications used to treat and control common diseases accounted for 23.1%, and medications used to eliminate symp-toms only accounted for 1.4%. Among medications suitable for patients’ self-care, medications used to treat and control common diseases accounted for 12.4% and medications mainly used to eliminate symptoms accounted for 39.4%.
Table 3. Classification of medications for acute upper respiratory infections.*
Medications Medications Medications Medications Total
used when life used to treat mainly used that cannot (NTD × 1000)
is threatened and control to eliminate be grouped
common diseases symptoms
Medications unsuitable 631,959 (12.8%) 1,707,099 (34.6%) 60,294 (1.2%) 424,246 (8.6%) 2,399,352 (48.6%)
for patients’ self-care
Medications suitable 5771 (0.1%) 667,996 (13.5%) 1,443,270 (29.2%) 2,117,037 (42.8%)
for patients’ self-care
Total 4,940,000 (100%)
* Values are in New Taiwan Dollars (NTD), where 1 NTD = 33.5 US dollars.
Table 2. Total costs and drug costs distributions for acute upper respiratory infections and common cold.*
Acute upper respiratory infections (ICD-9: 460) Common cold (ICD-9: 465)
Total cost (NTD) Drug cost (NTD) Total cost (NTD) Drug cost (NTD)
Mean SD p value Mean SD p value Mean SD p value Mean SD p value
Hospital level
Medical center 564 306 < 0.0001 247 219 < 0.0001 605 574 < 0.0001 230 369 < 0.0001
Area hospital 503 425 170 186 514 493 163 273
Local hospital 366 133 112 96 382 187 119 151
Primary care (clinics) 319 54 91 32 316 56 91 33
Others 332 68 92 59 345 125 96 60 Department General medicine 320 50 < 0.0001 88 36 < 0.0001 319 63 < 0.0001 91 35 < 0.0001 Family medicine 319 58 93 40 323 73 92 53 Internal medicine 335 82 94 57 347 133 100 74 Pediatrics 324 141 99 44 320 117 98 46 Others 335 123 100 69 331 184 100 125 Age ≤ 14 years 320 93 < 0.0001 96 37 0.0003 318 77 < 0.0001 95 37 < 0.0001 15–39 years 332 105 94 62 327 115 93 71 40–64 years 331 80 92 51 333 137 96 83 ≥ 65 years 339 115 97 82 343 197 102 134
* Values are in New Taiwan Dollars (NTD), where 1 NTD = 33.5 US dollars. ICD-9 = International Classification of Diseases, 9th edition.
D
iscussion
Hospital level, department, and patient age are important factors determining the cost of treatment for acute URIs and the common cold. There is no enforced referral system in Taiwan. This study provides information which may be useful in determining whether different classes of drugs should be covered by insurance, or whether different classes of drugs should differ in their coinsurance or copayments.
In many countries, health care drugs are divided into prescription drugs and OTC drugs. For example, in the United States, early in 1951, the Durham-Humphrey Amendment12 set forth the basis for
distin-guishing between prescription and OTC medications. The amendment specified that 3 classes of drugs be available by prescription: habit-forming drugs; drugs that were unsafe for use except under expert super-vision because of toxicity or other possible harmful effects; and drugs limited to prescription under a manufacturer’s new drug application.13
Approval of OTC status for a drug requires an assessment by the Food and Drug Administration that the drug is safe and effective. Unfortunately, the information needed to evaluate how drugs will actually be used by consumers if approved for OTC status is not always available.14 The decision to make
a drug available OTC and, in particular, to change the status of a drug from prescription-only to OTC raises questions relevant to the quality of health care, patients’ access to drugs, patients’ autonomy, and the costs of health care.
Using our classification method, in terms of acute URIs, non-payment for C2 medications (used to eliminate symptoms and suitable for patients’ self-care) had the least influence on patients’ health. In terms of efficiency of resource distribution, this type of medication has the least importance. Therefore, this study suggests that C2 drugs can be listed as non-prescription drugs, and that insurance should not cover these drugs. In this way, nearly 30% (NTD 1,443,270, 000) of the total drug expenditure for acute URIs would be saved per year. If payment for
B2 medications (used to treat and control common diseases and suitable for patients’ self-care) is not granted, 43% (NTD 2,117,200,037) of the total drug expenditure for acute URIs would be saved per year. In terms of acute nasopharyngitis (common cold), if the payment for C2 medications is refused, about 39.5% (NTD 406,602,000) of the total expenditure for treatment of common cold could be saved, and if payments for C2 and B2 medications are not covered, 53% (NTD 534,861,000) of the total expenditure for the common cold could be saved.
In addition, in terms of prescription drugs in categories B1 and C1, different payment rates can be adopted. Most previous studies that have looked at the impact of cost-sharing for prescription drugs have reported a decline in the use of such medications. The impact tended to be greater for the use of non-essential medications than for non-essential drugs.15–18
Tamblyn et al19 recently examined the impact of the
reform of the Quebec drug policy on elderly patients and welfare recipients affected by the changes. They found that use of both essential and non-essential drugs decreased after the policy reform. In addition, they found that the decline in the use of essential drugs was associated with an increase in serious health events and visits to the emergency department.
The desire to control health care costs has led to considerable variation in how employers and health insurance providers structure formularies, design benefits, and provide incentives to both physicians and patients. It was found that many of the tools used to influence pharmaceutical use were effective in re-ducing drug expenditures for working-age enrollees with employer-provided drug coverage. Adding an additional level of copayment and increasing existing copayments or coinsurance rates significantly reduced health insurance plan payments. Doubling patient copayments lowered average drug spending by as much as one-third, reducing both the likelihood of having a claim and the level of spending conditional upon use of the drug.20
From the point of view of medical resource distribution, improper use of drugs for URIs is a waste of resources, and theoretically, payment should not
Table 4. Classification of medications for acute nasopharyngitis (common cold).*
Medications Medications Medications Medications Total
used when life used to treat mainly used that cannot (NTD × 1000)
is threatened and control to eliminate be grouped
common diseases symptoms
Medications unsuitable 126,756 (12.3%) 238,120 (23.1%) 14,739 (1.4%) 116,164 (11.3%) 379,615 (36.8%)
for patients’ self-care
Medications suitable 128,259 (12.4%) 406,602 (39.4%) 534,861 (51.8%)
for patients’ self-care
Total 1,031,000 (100%)
be granted. However, because the public does not have a good understanding of URIs, sudden refusal to pay may have negative effects. In addition, the issue of medical access for disadvantaged patients and the possibility of untreated illnesses becoming more severe if left untreated must be addressed.
Taking the above factors into consideration, the NHI policy for drug benefit might benefit by first working to increase the public’s understanding of respiratory diseases, and then gradually reducing the scope of drugs paid for by health insurance. Using the benefit plan for prescribed drugs in the OPD as proposed in this study, our results suggest that the excessive use of drugs in the OPD could be reduced, the clinic medical utilization rate for acute URIs and the common cold could be improved, and that medi-cal resources could be distributed more efficiently. However, a limitation of this plan includes the fact that beginning a new classification system requires resources and is time-consuming. Senior experts’ assistance and common understanding are needed, and with the advancement of science and technology, constant adjustment will be needed. Due to data limitations, our study did not explore the impact of different copayments or coinsurance rates. Further analyses are needed for policy decision-making.
R
eferences
1. Department of Health, the Executive Yuan, Republic of China:
National Health Insurance Annual Statistical Report, 2001. Taipei:
Bureau of National Health Insurance; June 2002: 314-5. 2. Organization for Economic Co-operation and Development:
OECD Health Data 2002: A Comparative Analysis of 30 Countries. 4th edition, 2002. Washington, DC: OECD, 2002.
3. West JV: Acute upper airway infections. Br Med Bull 2002; 61: 215-30.
4. English JA, Bauman KA: Evidence-based management of upper respiratory infection in a family practice teaching clinic. Fam Med 1997; 29: 38-41.
5. Tylenol cold tablets (acetaminophen, chlorpheniramine,
pseudoephedrine): Physicians’ Desk Reference. 54th ed.
Montvale, NJ: Medical Economics Company; 2000: 1676-7. 6. Gaedigk A: Interethnic differences of drug-metabolizing
enzymes. Int J Clin Pharmacol Ther 2000;38:61-8.
7. Snow V, Mottur-Pilson C, Gonzales R: Principles of appropriate antibiotic use for treatment of nonspecific upper respiratory tract infections in adults. Ann Intern Med 2001;143:487-9. 8. Fahey T, Stocks N, Thomas T: Systematic review of the treatment of
upper respiratory tract infection. Arch Dis Child 1998;79:225-30. 9. Huang SM: URI outpatient utilization. Technical Report of Second
Generation National Health Insurance Conference, 2002. 10. Chen GT, Tam YH: The Benefit Plan for NHI Drugs. Report of
Second Generation National Health Insurance. Taipei: Executive Yuan; 2003: 197-202.
11. Covington TR: Ed. Handbook of nonprescription drugs. 11th ed. Washington, DC: American Pharmaceutical Association. The National Professional Society of Pharmacists, 1996.
12. Humphrey-Durham Drug Prescription Act, Pub L No. 82-215. 65 Stat 648-649 (October 26, 1951).
13. Gossel EA: Implications of reclassification of drugs from prescription-only to over-the-counter status. Clin Ther 1991;13: 200-15.
14. Stuart B, Zacker C: Who bears the burden of Medicaid drug copayment policies? Health Aff 1999;18:201-12.
15. Soumerai SB, Ross-Degnan D, Avorn J, et al: Effects of Medicaid drug-payment limits on admission to hospitals and nursing homes. N Engl J Med 1991;325:1072-7.
16. Johnson RE, Goodman MJ, Hornbrook MC, et al: The effect of increased prescription drug cost-sharing on medical care utilization and expenses of elderly health maintenance organization members. Med Care 1997;35:1119-31.
17. Harris BL, Stergachis A, Ried LD: The effect of drug co-payments on utilization and cost of pharmaceuticals in a health maintenance organization. Med Care 1990;28:907-1017. 18. Joyce GF, Escarce JJ, Solomon MD, et al: Employer drug benefit
plans and spending on prescription drugs. JAMA 2002;288: 1733–9.
19. Tamblyn R, Laprise R, Hanley JA, et al: Adverse events associated with prescription drug cost-sharing among poor and elderly persons. JAMA 2001;285:421-9.
20. Brass EP: Changing the status of drugs from prescription to over-the-counter availability. N Engl J Med 2001;345:810-6.