1Department of Laboratory Medicine, National Taiwan University Hospital, National Taiwan University College of Medicine, Taipei; 2Institute of Epidemiology, National Taiwan University College of Public Health, Taipei; 3Department of Internal Medicine, National Taiwan University Hospital, National Taiwan University College of Medicine, Taipei; 4Institute of Occupational Medicine and Industrial Hygiene, National Taiwan University College of Public Health, Taipei, Taiwan.
Received: 28 August 2003 Revised: 15 October 2003 Accepted: 9 December 2003
Reprint requests and correspondence to: Dr. Sow-Hsong Kuo, Department of Laboratory Medicine, National Taiwan University Hospital, No. 7, Chung-Shan South Road, Taipei 100, Taiwan.
ORIGINAL ARTICLES
P
REVALENCE
OF
AND
M
AJOR
R
ISK
F
ACTORS
FOR
A
DULT
B
RONCHIAL
A
STHMA
IN
T
AIPEI
C
ITY
I-Shiow Jan,1 Wei-Hui Chou,2 Jung-Der Wang,3,4 and Sow-Hsong Kuo1,3
Background and Purpose: The prevalence of bronchial asthma has been on the rise worldwide, but the prevalence of adult asthma in Taiwan has not been reported. The objective of this study was to determine the current 1-year and lifetime asthma prevalence rates, and to identify major risk factors for adult asthma in Taiwan.
Methods: A cluster sampling was conducted in 1999, where 21 clusters and 4549 adults (age ≥ 18 years) were selected randomly. Face-to-face interviews were conducted with a total of 2076 adults (45.6%; men/women, 987/1089) using a questionnaire designed to assess asthma and asthma-like symptoms adapted from the American Thoracic Society with minor modifications to include information about current asthma status.
Results: The results showed that 50 cases had a previous diagnosis of asthma and 94 had been classified as probably having asthma with intermittently audible wheezing. The lifetime prevalence rate of asthma in adults in Taipei City was 7.8%. Seventy three out of 144 patients had asthmatic symptoms or wheezing in the past 12 months. The 1-year prevalence of asthma was 4.1%. A multiple logistic regression model showed the odds ratio (95% confidence interval) of a history of maternal asthma to be 5.8 (2.77 to 12.18), that of allergic rhinitis to be 3.2 (2.03 to 5.16), that of paternal asthma to be 2.2 (0.91 to 5.21), that of older age (≥ 50 years) to be 2.0 (1.25 to 3.19), and that of smoking habit to be 1.7 (1.02 to 2.72).
Conclusions: The lifetime prevalence rate of adult bronchial asthma in Taipei City was 7.8% and related to both genetic and environmental factors, which included maternal or paternal history of asthma, history of allergic rhinitis, older age (≥ 50 years), and smoking habits.
Key words: Adult; Asthma; Prevalence; Risk factors; Taiwan
J Formos Med Assoc 2004;103:259-63
The prevalence of bronchial asthma has been on the rise worldwide during the last several decades.1–8 The worldwide 12-month prevalence of self-reported asthma symptoms was between 1.6% and 36.8% in children aged 13 to 14 years.9 In the European Community Respiratory Health Survey (ECRHS), the prevalence of asthma diagnosed over the previous 12 months was between 2.0% and 11.9% among adults aged 20 to 44 years old.10,11 Asthma has become a very important issue in public health. Furthermore, uncontrolled asthma, which results in demands on emergency services, hospitalization, work loss, and early retirement, is a significant financial burden on health care systems.12
Taiwan, an island country with more than 22 million people, has recently become a developed country. Per capita gross national production13 in-creased from US$3646 in 1986 to US$14,216 in 2000. Population density is 617 per square kilometer, which is the second highest in the world, the figure being even higher in the metropolitan areas. Hsieh and Shen14 and Wang et al15 showed a steady increase in the pre-valence of childhood asthma in Taiwan over the past 2 decades. However, thus far, there have been no reports about the prevalence of adult asthma in Taiwan.
This survey was conducted to evaluate the pre-valence of adult asthma by questionnaire in Taipei
City. In addition, the magnitudes of effect of major risk factors for asthma were also evaluated, including gender, age, family history, education, occupation, smoking, and other environmental factors.
M
ethods
Taipei, the capital of Taiwan, is located in the northern part of the island. The average temperature in January, the coldest month, is 15.3°C; in July, the hottest month, it is 29.0°C. The relative humidity ranges from 83% (February) to 77% (July).16 The population of Taipei City in 1999 was 2,646,474, including 876,063 house-holds and 9950 “lins” (the smallest administrative unit in Taiwan — within each “lin” is a geographic cluster of 20 to 100 households). We conducted a single-stage cluster sampling with probability proportional to size.17 Twenty one clusters of lins were selected randomly under the assumption that each household has an equal number of adults.
This study was conducted using a questionnaire, which was a Chinese language version translated and modified from a questionnaire of the American Thoracic Society and the Division of Lung Diseases (ATS-DLD-78) designed to assess asthma and asthma-like symptoms.18,19 To make the questionnaire suitable for an asthma study, some questions about current asthma status were adapted from a questionnaire of the International Union against Tuberculosis and Lung Disease.20 The validity of this revised question-naire was evaluated by a pulmonologist and 2 epidemiologists before this study was conducted.
Twenty college students were recruited as inter-viewers. Training courses and a handbook of standard operating procedures were prepared for the inter-viewers. Every item on the questionnaire was standard-ized and repeatedly practiced at least 30 times before actual interviews were performed. All interviews were carried out in either Mandarin or Taiwanese, depend-ing on the language background of the sampled subjects. Every adult 18 years of age or older in each
selected household was interviewed. Each completed questionnaire was reviewed and verified by a researcher for quality control. A subject with a diagnosis of bron-chial asthma made by a physician was categorized as having definite asthma. If a respondent answered, “yes,” on one or both of the following questions, he/she was classified as having probable asthma: “Does your chest sound wheezy or whistling when you have a cold?” and “Does your chest sound wheezy or whistling occasionally apart from when you have a cold?”
Statistical analysis
Data were stored in Microsoft Excel 2000 format and statistical analysis was conducted using SAS 6.12 statistical software. The association between asthma and each risk factor was first examined by chi-squared test. Then, a logistic regression model was constructed using definite and probable asthma as the dependent variables, and gender, age, education, allergic rhinitis, smoking, maternal and paternal asthma, occupational dust, vapor and/or fume exposure, pets in the house-hold, indoor fungi, and indoor incense burning as independent variables. The significance level was set at p ≤ 0.05.
R
esults
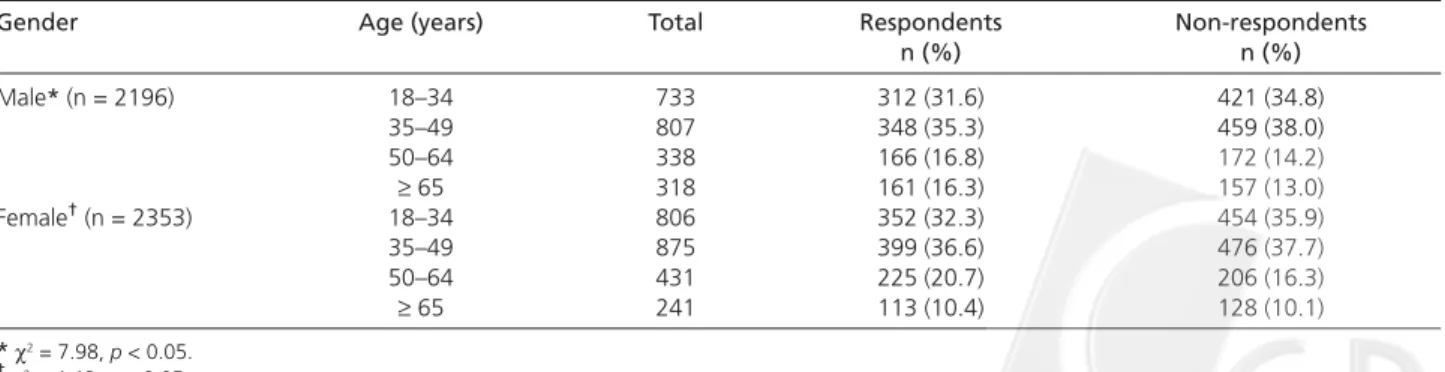
A total of 4549 adults living in 21 lins in Taipei City were interviewed between November 1999 and October 2000. Finally, 2076 (45.6%) adults, including 987 men and 1089 women, were interviewed. The distribution in age for the respondents and non-respondents was similar (Table 1) except that non-respondents were slightly younger than respondents, as shown in Table 1.
Among the 2076 subjects, 50 had a diagnosis of bronchial asthma by physicians and were classified as having definite asthma. Within this group, 28 subjects had suffered from asthmatic symptoms in the past 12 months. According to the criteria, 94 subjects who noted wheezing on the questionnaire were grouped as having probable asthma. Forty five out of these 94
Table 1. Comparison of age distribution between respondents and non-respondents.
Gender Age (years) Total Respondents Non-respondents n (%) n (%) Male* (n = 2196) 18–34 733 312 (31.6) 421 (34.8) 35–49 807 348 (35.3) 459 (38.0) 50–64 338 166 (16.8) 172 (14.2) ≥ 65 318 161 (16.3) 157 (13.0) Female† (n = 2353) 18–34 806 352 (32.3) 454 (35.9) 35–49 875 399 (36.6) 476 (37.7) 50–64 431 225 (20.7) 206 (16.3) ≥ 65 241 113 (10.4) 128 (10.1) *χ2 = 7.98, p < 0.05. †χ2 = 4.48, p < 0.05.
subjects had wheezing in the past 12 months. We excluded subjects with chronic bronchitis using items in the same questionnaire for patient history and symptoms of chronic bronchitis. Subjects with chronic bronchitis and emphysema were excluded from the probable asthma group. A total of 144 subjects either had a diagnosis of bronchial asthma by physicians or reported suffering from wheezing on the question-naire. The prevalence of lifetime asthma was 7.8%. Seventy three of the 144 subjects had asthma attacks or wheezing in the past 12 months. Therefore, the 1-year prevalence of asthma was 4.1%.
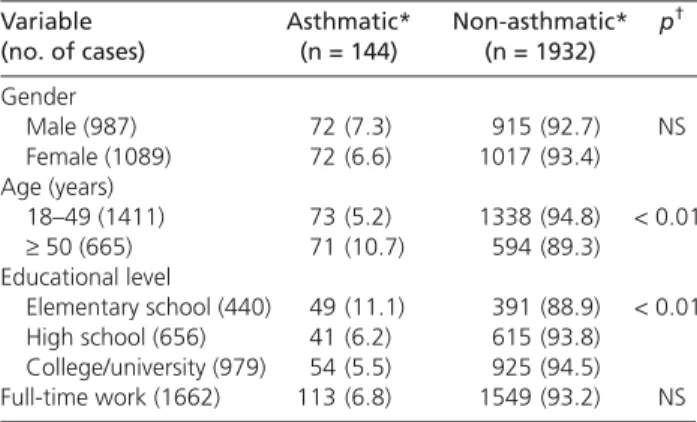
As shown in Table 2 there were more elderly persons and those with lower education levels in the asthmatic group than in the non-asthmatic group (p < 0.01). More retired subjects (25.7% vs 11.7%) and more people without work (11.1% vs 6.0%) were also found in the asthmatic group than in the non-asthmatic group. Allergic rhinitis, paternal and/or maternal asthma, paternal and/or maternal allergic rhinitis and smoking were significantly associated with asthma by chi-squared analysis (Tables 3 and 4).
Multiple logistic regression analysis indicated some factors to be significantly associated with asthma, namely
age ≥ 50 years, allergic rhinitis, smoking, and maternal asthma (Table 5). Paternal asthma had a borderline significant association with asthma (p < 0.08). Gender, education, exposure to dust, vapors or fumes in the workplace, passive smoking, pet or fungi in the household, and family incense burning were not entered in the final logistic model.
D
iscussion
This survey was conducted with a single-stage cluster sampling with probability proportional to size assum-ing each household had an equal number of adults. Then, all those ≥ 18 years old in each household were interviewed. This sampling method could estimate the true prevalence rate given the budget constraint.
The age distribution was younger in the non-respondent group than in the non-respondent group. The reasons for lack of complete interview data were as follows: the interviewers were unable to meet sampled subjects after 4 attempted visits (45.1%); the sampled subjects moved to other areas or could not be located (32.8%); or the request for an interview was rejected (17.6%). Among the 434 non-respondents who rejected the interview, 188 stated that they were not interested in the asthma survey. Healthy people were much more likely to refuse participation in the survey. This may have resulted in overestimating the prevalence rate. The fact that non-respondents were slightly younger than respondents was also an indication of such a tendency, as age ≥ 50 years was associated with a 2-fold increased risk of asthma.
Table 3. Comparison of frequency distribution of allergic
history between asthmatic and non-asthmatic groups. Variable Asthmatic Non-asthmatic p*
(no. of cases) (%) (%)
Allergic rhinitis (190) 31 (16.3) 159 (83.7) < 0.01 Paternal asthma (48) 8 (16.7) 40 (83.3) < 0.01 Maternal asthma (42) 12 (28.6) 30 (71.4) < 0.01 Paternal allergic rhinitis (54) 11 (20.4) 43 (79.6) < 0.01 Maternal allergic rhinitis (61) 11 (18.0) 50 (82.0) < 0.01 Atopic dermatitis (9) 1 (11.1) 8 (88.9) NS Paternal atopic dermatitis (2) 0 (0) 2 (100) NS Maternal atopic dermatitis (1) 1 (100) 0 (0) NS * Chi-squared test, α = 0.05.
NS = not significant.
Table 4. Comparison of frequency distribution of indoor
environmental risk factors between asthmatic and non-asthmatic groups.
Variable Asthmatic Non-asthmatic p*
(no. of cases) (%) (%)
Smoking (459) 44 (9.6) 415 (90.4) 0.01 Passive smoking (796) 53 (6.7) 743 (93.3) NS Pet in household (477) 42 (8.8) 435 (91.2) NS Fungi in household (606) 44 (7.3) 562 (92.7) NS Family incense burning (1204) 86 (7.1) 1118 (92.9) NS * Chi-squared test, α = 0.05.
NS = not significant.
Table 5. Multivariate analysis of risk factors associated with
definite and probable asthma.
Risk factor OR 95% CI p Maternal asthma 5.8 2.77–12.18 < 0.01 Allergic rhinitis 3.2 2.03–5.16 < 0.01 Age ≥ 50 years 2.0 1.25–3.19 < 0.01 Smoking 1.7 1.02–2.72 0.04 Paternal asthma 2.2 0.91–5.21 0.08
OR = odds ratio; CI = confidence interval.
Table 2. Comparison of frequency distribution of
demo-graphic data between asthmatic and non-asthmatic groups. Variable Asthmatic* Non-asthmatic* p†
(no. of cases) (n = 144) (n = 1932) Gender Male (987) 72 (7.3) 915 (92.7) NS Female (1089) 72 (6.6) 1017 (93.4) Age (years) 18–49 (1411) 73 (5.2) 1338 (94.8) < 0.01 ≥ 50 (665) 71 (10.7) 594 (89.3) Educational level Elementary school (440) 49 (11.1) 391 (88.9) < 0.01 High school (656) 41 (6.2) 615 (93.8) College/university (979) 54 (5.5) 925 (94.5) Full-time work (1662) 113 (6.8) 1549 (93.2) NS * Values are number (%).
† Chi-squared test, α = 0.05. NS = not significant.
However, this impact was probably limited because only 7.6% of the non-respondents reported being uninterested in this survey.
There were more retired and jobless people in the asthmatic group than in the non-asthmatic group. Previous study found that asthma is associated with work loss and early retirement.12
In Taiwan, the prevalence of current asthma for school children aged 7 to 15 years increased from 1.30% in 1974 to 5.07% in 1985.14 In 2001, Lin et al reported 8.5% of 1,018,031 students in middle school had a history of asthma and the prevalence of asthma was higher in more urbanized areas (11.2%) than in less urbanized and rural areas (6.5%).21 This study found the lifetime and current asthma prevalence rates for adults above 18 years old were 7.8% and 4.1%, respectively. Although there has been a lack of consistency in the definition of bronchial asthma among different studies, the prevalence of adult asthma in this study was about half of that in the children in Taiwan.15,21 This finding is in accordance with other studies of adults.2,9–11 Using this study’s definition of probable asthma and comparing the rate with that for definite (physician-diagnosed) asthma, there was a ratio of 1.9 untreated and/or undiagnosed cases for each case of treated asthma in this sample. Two-thirds of adults who had wheezing did not visit doctors or were not recognized early by their physi-cians as having bronchial asthma. This finding sug-gests that asthma is under-diagnosed in Taiwan. Taiwan health education in general, and especially for medical professionals, should stress this finding.
Maternal or paternal history of asthma, history of allergic rhinitis, older age (≥ 50 years), and smok-ing habits were found to be major risk factors for asthma in this study. This is consistent with previous studies.22–24 In this study, 21.5% of asthma patients were current smokers, slightly higher than the 18.2% found using the same definition in the USA.25
The subjects who were screened and found to have asthma were recommended to undergo spiro-metry and bronchial provocation tests26 to verify the diagnosis of asthma. However, the percentage of patients who completed further testing was very low. To the best of our knowledge, this is the first pre-valence survey of adult bronchial asthma in Taiwan. Data from this study may serve as baseline data for the comparison of future prevalence surveys of adult asthma in Taiwan. According to the prevalence rates found in this study, approximately 1,700,000 people suffer from asthma in Taiwan. This is a substantial public health problem and socioeconomic burden for the country. Further efforts to improve education of medical staff and the general community about the problem of under-diagnosis of asthma are needed.
ACKNOWLEDGMENT: This survey was sponsored
by a grant from the Department of Health, Executive Yuan (DOH89-46), ROC.
R
eferences
1. Sears MR: Descriptive epidemiology of asthma. Lancet 1997; 350(Suppl II):S1-S4.
2. Ormerod LP, Myers P, Prescott RJ: Prevalence of asthma and 'probable' asthma in the Asian population in Blackburn, U.K.
Respir Med 1999;93:16-20.
3. Christiansen SC, Martin SB, Schleicher NC, et al: Current preva-lence of asthma-related symptoms in San Diego's predominantly Hispanic inner-city children. J Asthma 1996;33:17-26. 4. Kivity S, Shochat Z, Bressler R, et al: The characteristics of
bronchial asthma among a young adult population. Chest 1995; 108:24-7.
5. Hartert TV, Peebles RSJ: Epidemiology of asthma: the year in review. Curr Opin Pulm Med 2000;6:4-9.
6. Schwartz J, Gold D, Dockery DW, et al: Predictors of asthma and persistent wheeze in a national sample of children in the United States. Association with social class, perinatal events, and race. Am Rev Respir Dis 1990;142:555-62.
7. Burney PGJ, Chinn S, Rona RJ: Has the prevalence of asthma increased in children? Evidence from the national study of health and growth 1973-86. BMJ 1990;300:1306-10.
8. Burr ML, Butland BK, King S, et al: Changes in asthma prevalence: two surveys 15 years apart. Arch Dis Child 1989;64:1452-6. 9. Beasley R, Keil U, Mutius EV, et al: Worldwide variation in
prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. Lancet 1998;351:1225-32. 10. Burney PGJ, Luczynska C, Chinn S, et al: The European
community respiratory health survey. Eur Respir J 1994;7: 954-60.
11. Burney P, Chinn S, Jarvis D, et al: Variations in the prevalence of respiratory symptoms, self-reported asthma attacks, and use of asthma medication in the European Community Respiratory Health Survey (ECRHS). Eur Respir J 1996;9:687-95.
12. Barnes PJ, Jonsson B, Klim JB: The costs of asthma. Eur Respir J 1996;9:636-42.
13. Directorate-General of Budget Accounting and Statistics, Executive Yuan, R.O.C. Key economic and social indicators. Taipei: Directorate-General of Budget Accounting and Statistics, Executive Yuan; 2001 [cited 2001 July 11]:[1 screen]. Available from URL: http://www.dgbasey.gov.tw/english/dgbas_e3.htm 14. Hsieh KH, Shen JJ: Prevalence of childhood asthma in Taipei,
Taiwan, and other Asian Pacific countries. J Asthma 1988;25: 73-82.
15. Wang WC, Lue KH, Sheu JN: Allergic diseases in preschool children in Taichung city. Acta Paed Sin 1998;39:314-8. 16. Central Weather Bureau. CWB’s observatory monthly mean
temperature. Taipei: The Bureau; [cited 2001 July 11]:[1 screen]. Available from: URL: http://www.cwb.gov.tw/V3.0/climate/ twn_station/sta03.htm
17. Cochran WG: Single-stage cluster sampling: clusters of un-equal sizes. In: Cochran WG, ed. Sampling techniques. 3rd ed. New York: John Wiley & Sons, 1977:249-73.
18. Torén K, Brisman J, Järvholm B: Asthma and asthma-like symptoms in adults assessed by questionnaires. Chest 1993; 104:600-8.
19. Ferris BG: Epidemiology standardization project. II. Recom-mended respiratory disease questionnaires for use with adults and children in epidemiologic research. Am Rev Respir Dis 1978; 118(Suppl):S7-S53.
20. Burney PGJ, Laitinen LA, Perdrizet S, et al: Validity and repeatability of the IUATLD (1984) bronchial symptoms questionnaire: an international comparison. Eur Respir J 1989; 2:940-5.
21. Lin RS, Sung FC, Huang SL, et al: Role of urbanization and air pollution in adolescent asthma: a mass screening in Taiwan. J
Formos Med Assoc 2001;100:649-55.
22. Newman-Taylor A: Environmental determinants of asthma.
Lancet 1995;345:296-9.
23. Cookson WOC: Asthma genetics. Chest 2002;121(Suppl):S7-S13.
24. Chowgule RV, Shetye VM, Parmar JR, et al: Prevalence of respiratory symptoms, bronchial hyperreactivity, and asthma in a Megacity – results of the European Community Respiratory Health Survey in Mumbai (Bombay). Am J Respir Crit Care Med 1998;158:547-54.
25. Fuhlbrigge AL, Adams RJ, Guilbert TW, et al: The burden of asthma in the United States. Am J Respir Crit Care Med 2002; 166:1044-9.
26. Juniper EF, Frith PA, Dunnett C, et al: Reproducibility and com-parison of responses to inhaled histamine and methacholine.