The impacts of smart cards on hospital
information systems—–An investigation of the first
phase of the national health insurance smart card
project in Taiwan
Chien-Tsai Liu
a,∗, Pei-Tun Yang
a,b, Yu-Ting Yeh
a, Bin-Long Wang
baGraduate Institute of Medical Informatics, Taipei Medical University, 250 Wu-Xing Street, Taipei 107, Taiwan
bDepartment of Information Management, Tri-Services General Hospital, Taiwan
Received 6 September 2004 ; received in revised form 6 April 2005; accepted 11 July 2005
KEYWORDS
Smart cards;
Health insurance cards; Patient data cards; Hospital information systems
Summary
Purpose: To investigate the impacts of the first phase of Taiwan’s Bureau of National
Health Insurance (TBNHI) smart card project on existing hospital information sys-tems.
Setting: TBNHI has launched a nationwide project for replacement of its paper-based
health insurance cards by smart cards (or NHI-IC cards) since November 1999. The NHI-IC cards have been used since 1 July 2003, and they have fully replaced the paper-based cards since 1 January 2004. Hospitals must support the cards in order to provide medical services for insured patients.
Methods: We made a comprehensive study of the current phase of the NHI-IC card
system, and conducted a questionnaire survey (from 1 October to 30 November, 2003) to investigate the impacts of NHI-IC cards on the existing hospital informa-tion systems. A quesinforma-tionnaire was distributed by mail to 479 hospitals, including 23 medical centers, 71 regional hospitals, and 355 district hospitals. The returned questionnaires were also collected by prepaid mail.
Results: The questionnaire return rates of the medical centers, regional hospitals
and district hospitals were 39.1, 29.6 and 20.9%, respectively. In phase 1 of the project, the average number of card readers purchased per medical center, regional hospital, and district hospital were 202, 45 and 10, respectively. The average person-days for the enhancement of existing information systems of a medical center, regional hospital and district hospital were 175, 74 and 58, respectively. Three months after using the NHI-IC cards most hospitals (60.6%) experienced prolonged
∗Corresponding author. Tel.: +886 2 23776730x202; fax: +886 2 27339049. E-mail address: ctliu@tmu.edu.tw (C.-T. Liu).
1386-5056/$ — see front matter © 2005 Elsevier Ireland Ltd. All rights reserved. doi:10.1016/j.ijmedinf.2005.07.022
service time for their patients due to more interruptions caused mainly by: (1) impair-ment of the NHI-IC cards (31.2%), (2) failure in authentication of the SAMs (17.0%), (3) malfunction in card readers (15.3%) and (4) problems with interfaces between the card readers and hospital information systems (15.8%). The overall hospital satisfac-tion on the 5-point Likert scale was 2.86. Although most hospitals were OK with the project, there was about 22% dissatisfied and strongly dissatisfied, that is twice as many hospitals with satisfied (about 10%).
Conclusions: Our recommendations for those who are planning to implement similar
projects are: (1) provide public-awareness programs or campaigns across the country for elucidating the smart card policy and educate the public on the proper usage and storage of the cards, (2) improve the quality of the NHI-IC cards, (3) conduct com-prehensive tests in software and hardware components associated with NHI-IC cards before operating the systems and (4) perform further investigations in authentication approaches and develop tools that can quickly identify where and what the problems are.
© 2005 Elsevier Ireland Ltd. All rights reserved.
1. Introduction
A smart card is a credit-card sized plastic card with an embedded computer chip that can be memory or also include a microprocessor[1,2]. A micropro-cessor chip can add, delete and otherwise manip-ulate information in its memory and hence offer complex data security schemes[3—6]. Smart cards have been in use as health cards for more than 10 years[7—11]. Several large-scale projects have demonstrated the practical use of smart cards in healthcare in Europe such as The Health Cover-age’s (Mutualit´es Belges) Social Identity System (SIS) cards in Belgium, versicherten-karte (Insur-ance cards) in Germany, carte vitale (vitale card) in France, health insurance cards in Slovenia[12], and so on. The European council of Barcelona of March 2002 decided to launch an European health insur-ance card on 1 June 2004. The card will replace all the current paper forms needed for health treat-ment in European union (EU) member state by 31 December 2005[13,14].
Taiwan’s bureau of national health insurance (TBNHI) has implemented National health insurance (NHI) program since 1 March 1995. All people in Tai-wan must be enrolled in the NHI program. Based on the results of a survey on NHI program in terms of adequacy and accessibility of medical care, 75% of the insured persons were satisfied with the program
[15]. However, in order to provide better quality of services and to improve the effective use of medi-cal resources, TBNHI therefore launched a project for implementing smart cards as the health insur-ance cards since November 1999. The smart cards, known as ‘‘NHI-IC’’ cards in Taiwan, allow patients to access medical services electronically, and carry a certain amount of critical patient information.
Because of its electronic nature, the NHI-IC cards also allow TBNHI to timely discover the inappro-priate use of medical resources and to investigate medical frauds.
The NHI-IC cards have been used since 1 July 2003, and they have fully replaced the paper-based cards since 1 January 2004. Currently more than 22 millions NHI-IC cards have been issued, and more than 17,000 hospitals, primary care providers and health care institutions are involved in this project. Incorporation of NHI-IC cards into hospital medical services demands both information technology and financial support for building up the information infrastructure and enhancing the existing hospital information systems.
In this paper, we will describe the current status of the project, the NHI-IC card system, and present the results of a questionnaire survey investigating the impact of the cards on hospital information sys-tems. These results reveal the problems and poten-tial issues that might be useful for those who are planning to implement similar projects.
2. The NHI-IC card system
The NHI-IC card system consists of the following major components: NHI-IC cards, the card readers for manipulation of the NHI-IC cards, the hospital information systems that controls the operations of the card readers and the communication networks that make the entire system work properly for med-ical services.
2.1. NHI-IC cards
Similar to a bank IC card, a NHI-IC card has an IC chip consisting of a CPU and 32 KB (103 bytes) of
mem-ory. The visible information on the NHI-IC card con-tains the cardholder’s name, identification number, date of birth, photo (optional), and the card serial number (an unique number assigned to each NHI-IC card). The content inside a NHI-NHI-IC card can be divided into four segments: basic data, health insur-ance data, medical data and public health admin-istration data[16].
The basic data segment stores the identification information for both the cardholder and the card itself. The health insurance data segment is com-prised of the cardholder’s insurance information and service data for insurance claims. The medical data segment contains 4 KB of memory, and is used to record important physician orders, prescriptions and drug allergies. The public health administra-tion data segment contains 2 KB of memory, and is used for recording personal data pertaining to public health such as vaccination records and organ donation notes.
2.2. NHI-IC card readers
A NHI-IC card can be accessed and manipulated through a card reader. However, for access to sensitive data the cardholder’s password may be required. The card reader can read/write the data from/into the NHI-IC card in accordance with the operations initiated by a host computer, which is usually a client of a hospital information system or a standalone computer. The host computer can invoke a set of predefined application programming interfaces (or so-called control software) to oper-ate the reader and to manipuloper-ate the data in the NHI-IC cards. The control software is free, and can be downloaded from TBNHI website[17].
Each card reader is equipped with a unique secu-rity access module (SAM) distributed by TBNHI. When a card reader is powered on, it must perform an authentication test on its SAM against TBNHI database. Only after successfully passing the test, can the card reader work properly.
2.3. Hospital information systems
A hospital information system in general refers to a computer system that handles the workflows of daily medical services, facilitates the management of financial, administrative and clinical data, and processes healthcare insurance claims. Most hospi-tals in Taiwan have developed their hospital infor-mation systems. The changes to the workflows of medical services due to the introduction of NHI-IC cards will likely affect their information flows, and hence may result in changes to their information systems.
The hospitals are ranked based on their capac-ity and capabilcapac-ity in providing the qualcapac-ity of health care [18]. They are, from the highest to the low-est, medical centers, regional hospitals, district hospitals and primary care clinics. Hospitals with higher rank usually have more sophisticated work-flows of medical services, resulting in sophisticated information systems in those hospitals. The hospi-tal information systems in primary care clinics are relatively simple since workflows there are straight-forward. Thus, in this study we focused on medical centers, regional hospitals and district hospitals. We use ‘‘hospital’’ to refer to those three cate-gories of the hospitals later in this paper.
The hospitals are characterized by the large vol-ume of medical services and extensive use of com-puters [19]. It is crucial to integrate NHI-IC card readers into their hospital information systems so that the workflows of the medical services can be streamlined and the service time for a patient can be optimized. That is, the data required to be recorded in a NHI-IC card can be collected and made ready for transferral to TBNHI with as little human intervention as possible.
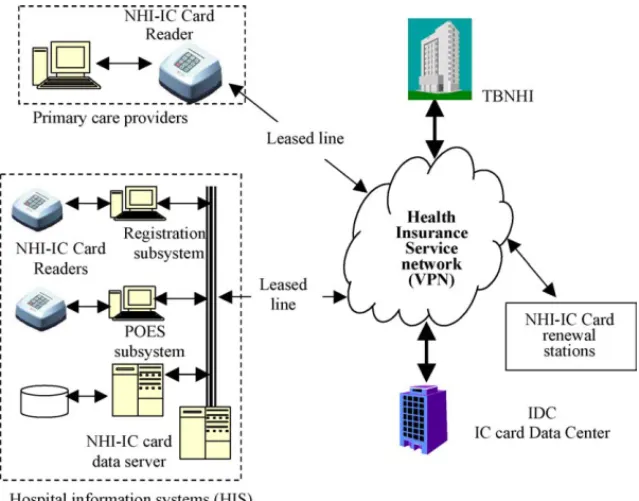
2.4. Interconnection networks
In order to facilitate the operation of the NHI-IC cards, TBNHI has established a NHI-IC card data cen-ter (IDC) to manage and maintain the card database and a high bandwidth health insurance service net-work (HISN) for connecting the card readers and data servers installed in hospitals or healthcare providers nationwide to the IDC. The hospitals must purchase NHI-IC card readers, and establish connec-tions (e.g., leased lines or phone lines) to the IDC as shown inFig. 1.
2.5. The current status of the NHI-IC
project
There are three phases in the implementation of the NHI-IC card project. The information involved in phase 1 includes the basic data segment and the information essential for insurance reimbursement claims in the health insurance data segment. In phase 2, in addition to the information involved in phase 1, the information including the medical data segment would be included. In phase 3 all the infor-mation including health insurance data, medical data and public health administration data would be included. The ultimate goal is to record as much patient care information in the NHI-IC card as pos-sible.
Fig. 1 The framework of the NHI-IC card system.
The current status of the project is in phase 1 now, with data involving identification informa-tion and insurance claims informainforma-tion. One of the key information for insurance claims is the service-sequence number, which is stored in each individ-ual card. For each medical service, a healthcare provider must read the number from the card, and then update the number for next use. When the ser-vice number reaches a predefined number (now 6, reflecting the six blocks of time stamps in a paper-based card), the patient is responsible for renewal of his/her card at any public service terminal or at a card reader in a hospital.
TBNHI establishes and maintains the HISN net-work and the NHI-IC card database for hospitals and the public. As indicated above, the healthcare providers who provide medical services for their patients are responsible for updating the service-sequence number into the patients’ NHI-IC card and transferring both the number and patient identifi-cation information to the IDC within 24 h, so that TBNHI can keep track of every insured’s consump-tion of the medical resources.
A hospital is highly recommended to enhance the existing hospital information systems to support NHI-IC cards to facilitate patient services. However, there is great diversity in hospitals, stemming from the individual hospitals own financial and technical problems in adopting NHI-IC cards to their service workflows.
TBNHI realize that the NHI-IC card project influ-ences not only the medical care providers but also
the way ordinary people access medical facilities. Consequently, TBNHI conducted a series of public-awareness programs or seminars nationwide for educating people on the government NHI-IC card policy and explaining how to use the cards. BNHI also created technical teams to provide hospitals (healthcare providers) consultations on NHI-IC card related matters.
3. Methods for evaluating the impacts of
NHI-IC cards
There are exceptions not related to NHI-IC cards such as patients seeking medical services without their NHI-IC cards or in case of power outage, which cannot be controlled by hospitals. TBNHI allows a hospital to make reimbursement claims for their medical services for the exceptions. The exception claims can be verified later as needed.
From this perspective, the impacts of NHI-IC cards on the existing hospital information systems can be divided into two components namely, • the effect of changes to the existing workflow of
the medical services, and
• the adoption capability of existing hospital infor-mation systems.
The impacts were evaluated by using a question-naire survey consisting of three parts: the basic information of the hospitals and respondents who
answered the questionnaire, the financial burden of changes to the existing information systems, and the effects of the changes to medical services.
The questionnaire was reviewed by an expert committee. The reliability test, Cronbach’s alpha (␣) was 0.76. The survey was conducted from 1 October to 30 November 2003. A questionnaire was distributed by mail to all 479 hospitals, including 23 medical centers, 71 regional hospitals, and 355 dis-trict hospitals. The returned questionnaires were also collected by prepaid mail.
4. Evaluation results
4.1. Basic data of respondents and their
hospitals
One hundred and four hospitals returned their ques-tionnaires: 9 medical centers, 21 regional hospitals and 74 district hospitals. The questionnaire return rates of the medical centers, regional hospitals and district hospitals were 39.1, 29.6 and 20.9%, respectively. The average return rate was 21.7%. The hospital with higher rank was higher than those with lower rank.
The volume of medical services of the responding hospitals, measured by inpatient beds and outpa-tient visits, is shown inTable 1. The average number of beds for medical centers, regional hospitals and district hospitals were 1187, 560 and 103, respec-tively, and the average outpatient visit per day was 4950 for medical centers, 1536 for regional hos-pitals and 466 for district hoshos-pitals. The results
reflected the fact that the service volume of a medical center is usually greater than a regional hospital, and in turn greater than a district hospi-tal.
The respondents’ roles, as shown in Table 2, were largely IT professionals (64.4%), the adminis-tration or medical record management profession-als (31.5%), and nurses (3.7%). The results show that most hospital top-level managers considered the NHI-IC project mainly related to hospital informa-tion systems, and assigned IT professionals or the like to complete the survey questionnaires.
4.2. The financial impacts
The financial burden to enhance the existing hospi-tal information systems is divided into three parts: the number of card readers purchased, the cost of communication bandwidth and the person-days for enhancement of hospital information systems. The total number of card readers purchased by medi-cal centers, regional hospitals and district hospitals were 1817, 947 and 768, respectively, as shown in
Table 3. On average a medical center, a regional hospital and a district hospital purchased 202, 45 and 10 card readers, respectively, during phase 1 of the project. It is reasonable that the higher ranked the hospital, the larger the service volume, and thus the more card readers needed.
The bandwidth of the communication lines con-necting between a hospital and the IDC usually depends on the amount of data to be transferred and on the cost of communication bandwidth. As shown in Table 4, most hospitals (48.1%)
sub-Table 1 The number of outpatient visits and the number of beds on an average in fiscal year 2002 Hospital category Number of hospitals Number of average
outpatients/per day Number of beds Medical center 9 4950 1187 Regional hospital 21 1536 560 District hospital 74 466 103 Total/average 104 874 289
Table 2 Which of the following best describes your role within your hospital
Medical centers Regional hospitals District hospitals Total
Physicians 0 0 0 0 Nurses 0 0 4 4 (3.9%) IT professionals 9 20 38 67 (64.4%) Administration or medical record professionals 0 1 32 33 (31.7%) Others 0 0 0 0 Total 9 21 74 104
Table 3 The number of NHI-IC card readers your hospital purchased
N Mean 95% confidence interval
Medical center 9 201.89 110.23—293.55
Regional hospital 21 45.10 34.36—55.83
District hospital 74 10.38 6.62—14.14
Total 104 33.96 21.23—46.70
Table 4 What type of communication lines between your hospital and the IDC
Medical center Regional hospital District hospital Total
512K/64K ADSL 3 3 38 44 (42.3%)
768K/128K ADSL 0 0 0 0 (0.0%)
1.5M/384K ADSL 0 1 2 3 (2.9%)
512K/512K ADSL 4 17 29 50 (48.1%)
T1/E1 leased line 2 0 5 7 (6.7%)
56K dial-up 0 0 0 0 (0.0%)
Total 9 21 74 104
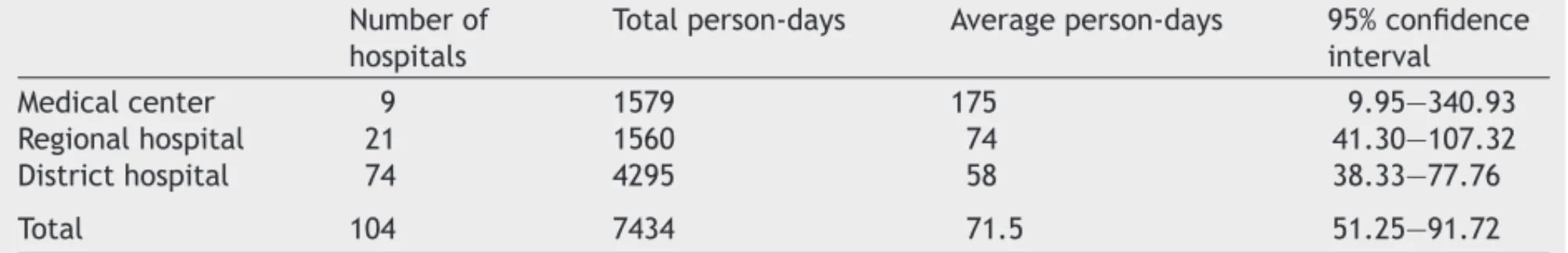
Table 5 The number of person-days took to enhance the information systems of your hospital (N = 104) Number of
hospitals
Total person-days Average person-days 95% confidence interval
Medical center 9 1579 175 9.95—340.93
Regional hospital 21 1560 74 41.30—107.32
District hospital 74 4295 58 38.33—77.76
Total 104 7434 71.5 51.25—91.72
scribed 512K (downstream rate)/512K (upstream rate) ADSL (asymmetric digital subscriber line)
[20,21], and 42.3% subscribed the 512K/64K ADSL, and 6.7% subscribed T1/E1 leased lines [20,21]. There was little relationship between the ranks of hospitals and their leased communication lines because there was little data to be transferred in the phase 1 of the project.
The enhancement of existing information sys-tems was measured in person-days.Table 5shows that the average person-days for a medical center, regional hospital and district hospital to enhance its hospital information systems were 175, 74 and 58, respectively. The results reflect the complexity of hospital information systems in different rank of hospitals.
4.3. The impact on medical services
The impact on hospital medical services can be identified by observing whether the service time for a patient visit takes longer after inclusion of the NHI-IC cards into the workflows. As shown in
Table 6, 60.6% of responding hospitals felt that the time for an outpatient service was prolonged, 34.6%
remain unchanged and few (4.8%) became shorter. Thus, for most of hospitals, inclusion of NHI-IC cards into medical services tended to make the service time longer because the workflows become more complicated, and may even cause problems in their hospital information systems.
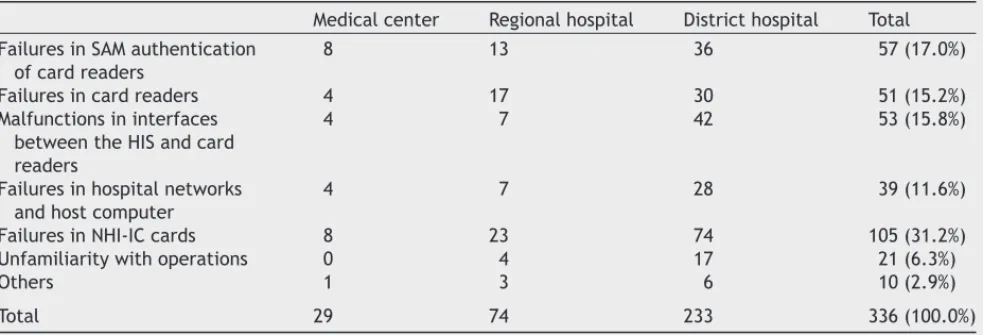
After inclusion of NHI-IC cards in medical ser-vices the problems that resulted in interruptions of the services were shown in Table 7. The major causes of the problems were (1) NHI-IC cards them-selves (31.2%), (2) the failures in SAM authenti-cation (17.0%), (3) the malfunctions in interfaces between the hospital information systems and card readers (15.8%), and (4) the failures in card readers (15.3%). It is noteworthy that about 5.6 and 2.9% of the problems were introduced by unfamiliarity with the operations of the NHI-IC card systems and oth-ers, respectively.
Most hospitals have been involved in the NHI-IC card project. Overall speaking, so far the hospi-tals have taken a passive stance to the NHI-IC card project. As indicated inTable 8, no hospital strongly agreed with it, 10.6% agreed and 67.3% had no comment. However, 19.2 and 2.9% disagreed and strongly disagreed with the project, respectively.
Table 6 The time for an outpatient service in your hospital after implementation of NHI-IC cards (N = 104) The time for an outpatient service in your hospital Total
Longer Shorter Remain unchanged
Medical center 7 1 1 9
Regional hospital 11 1 9 21
District hospital 45 3 26 74
Total 63 (60.6%) 5 (4.8%) 36 (34.6%) 104
Table 7 What were the problems that interrupted medical services after inclusion of NHI-IC cards into the services (multiple choices)
Medical center Regional hospital District hospital Total Failures in SAM authentication
of card readers
8 13 36 57 (17.0%)
Failures in card readers 4 17 30 51 (15.2%)
Malfunctions in interfaces between the HIS and card readers
4 7 42 53 (15.8%)
Failures in hospital networks and host computer
4 7 28 39 (11.6%)
Failures in NHI-IC cards 8 23 74 105 (31.2%)
Unfamiliarity with operations 0 4 17 21 (6.3%)
Others 1 3 6 10 (2.9%)
Total 29 74 233 336 (100.0%)
Table 8 As a whole, from your hospital point of view, you are satisfied with the NHI-IC card project so far (N = 104) Strongly
agree (5)
Agree (4) OK (3) Disagree (2) Strongly disagree (1) Average score Medical centers 0 3 4 1 1 3 Regional hospitals 0 1 15 5 0 2.81 Distrcit hospitals 0 7 51 14 2 2.85 Total 0 11 (10.6%) 70 (67.3%) 20 (19.2%) 3(2.9%) 2.86
The results show that the lower ranked the hospi-tal, the stronger the dissatisfaction with the project because their business scale would not allow them to allocate adequate resources to enhance their hospital information systems and reorganized their workflows as well.
5. Discussion
With the capability of portable and highly secured storage, smart cards have played a major role in the area of healthcare. Most of them provide visually readable information and carry identification data. Some may be used as access keys to the relevant databases, while some may carry patient health information for emergency use. Taiwan’s NHI-IC cards carry not only identification data but also the
data needed for health insurance, medical care and public health administration. Moreover, a health-care provider is responsible for writing the specified data into a card and transferring the data to TBNHI within 24 h. Therefore, hospitals are likely to face more obstacles in adoption of the NHI-IC cards as an integral part of their hospital information systems. As indicated in the survey results, 3 months after inclusion of NHI-IC cards into the medical services, most hospitals experienced longer service time due to more interruptions introduced by the problem in the NHI-IC cards themselves, the malfunctions in card readers, authentication of the SAMs and inter-faces between the card readers and hospital infor-mation systems. It is noteworthy that about 30% of the interruptions were caused by NHI-IC cards. Improvement of the quality of the NHI-IC cards and provision of education on storage and usage of the
cards for the public at the beginning of the project would effectively help reduce the occurrences of the problem.
Another major problem was the failure in the online authentication of card readers. There are too many factors involved in authentication test-ing such as the HISN networktest-ing system, the IDC database system, hospital networking systems and the card readers [22]. The causes cannot be dis-tinguished easily, and hence the problem tends to take longer to fix. Therefore, TBNHI should perform further investigation in alternative authentication approaches, or develop tools that can quickly iden-tify where and what the problems are.
In the beginning of 3 months of the first phase, most problems resulted mainly from ill-designed and incomplete tests in hardware and software components. After TBNHI distributed a new version of the control software, the professionals of the hospitals were familiar with the NHI-IC card system and learned the integration approaches, there have been fewer and fewer such problems reported as the project proceeded. Thus, well-integrated and robust hospital information systems could alleviate the prolonged service time.
Very few hospitals (2.9%) complained about the interruptions to medical services caused by the other problems (not listed in the question), which mainly refer to non-technical problems such as patients seeking medical services without their NHI-IC cards, in case of power outage, and so on. The outcome might be attributed to TBNHI’s compre-hensive public-awareness programs for the public and healthcare providers before starting use of NHI-IC cards. Likewise, we can reduce or remove 5.6% of problems due to unfamiliarity with the system operations by giving more comprehensive training programs to end users at the very beginning phase. The success of the project is very much depen-dent on the cooperation and support from hospitals. The hospitals can hardly get direct benefits from early adoption of NHI-IC cards in the current phase. In addition, they have to invest their money in enhancement of their hospital information systems. As shown inTable 8, although most hospitals were OK with the project, there was about 22% dissatis-fied or strongly dissatisdissatis-fied, that is twice as many hospitals with satisfied (about 10%). The lower rank of a hospital, the less satisfaction with the project it had because its business scale is rather small and would not allow them to invest money in full computerization their medical services in a short time.
Even with the low satisfaction rate, there are two forces driving the NHI-IC card project ahead. Firstly, there is only one health insurance provider
in Taiwan. The hospitals must make their infor-mation systems compliant with the NHI-IC card requirements in order to get reimbursement for their medical services. Secondly, most people con-sider the NHI-IC cards as simple and convenient for access to medical services and would expect hos-pitals provide such a convenience. Thus, although some hospitals disagreed with TBNHI, the NHI-IC card project has been now survived and continues to approach the initially designed goals.
The overall return rate of this questionnaire sur-vey was low, and the hospitals with higher rank had higher return rate. There might be a sample bias. The results may be over estimated. Therefore, the problems revealed here would be less than as they were.
6. Conclusions
From the survey results, very few hospitals com-plained about the interruptions caused by non-technical problems; instead, the major problems that caused the interruptions of medical services were the impairment of NHI-IC cards and online authentication testing. Therefore, our recommen-dations for those who are planning to implement similar projects are: (1) provide public-awareness programs or campaigns across the country for elu-cidating the health smart card policy and educating how people can use and store the cards, (2) improve the quality of the NHI-IC cards, (3) conduct compre-hensive tests in software and hardware components associated with NHI-IC card systems before oper-ating the system, and (4) perform further investi-gations in authentication approaches and develop tools that can quickly identify where and what the problems are.
Although there was not enough direct incen-tive for hospitals to adopt NHI-IC cards into their medical services, the cards are simple and conve-nient for the public to access medical services. It is expected that the project will gradually move to phase 2 and phase 3. Hence, more and more patient health information can be stored in the cards as well as in the TBNHIs database. The healthcare providers can take the advantages of the availabil-ity of such data to provide better qualavailabil-ity of care, while the TBNHI can keep track of the use of med-ical resources precisely to prevent the potential medical frauds timely.
What was known before the study:
• TBNHI has launched a nationwide project for replacement of its paper-based health insurance cards by NHI-IC cards since November 1999.
Hos-pitals must support the cards in order to provide medical services for insured patients.
• Incorporation of NHI-IC cards into medical ser-vices was critical, but little was known of the cost of building up the systems associated with NHI-IC cards and enhancing the existing information systems.
• Little information was attained on the major problems of the NHI-IC card system after it was in operation nationwide, and most of what was attained was indefinite.
What this study has added to the body of knowl-edge:
• The survey results reveal that the average cost for a hospital to build up the systems associated with NHI-IC cards and to enhance the existing information systems. The cost was proportional to its rank.
• The major problems after the NHI-IC card system was up and running nationwide were (1) impair-ment of the NHI-IC cards, (2) failure in authenti-cation of the SAMs, (3) malfunction in card read-ers and (4) problems in interfaces between the card readers and hospital information systems. • Most hospitals experienced prolonged service
time for their patients in 3 months after start-ing to use the NHI-IC cards.
• We learned from the project, and made recom-mendations to those who are planning to imple-ment similar projects.
Acknowledgments
We thank the reviewers of the journal for the com-ments to clarify issues in the questionnaire survey and make the paper more structural and read-able. This research was partially supported by the grants from the Bureau of National Health Insurance (DOH 90-2511-S-038-002, DOH 91-2511-S-038-002, and DOH 92-2516-S-038-002).
References
[1] W. Rankl, W. Effing, Smart Card Handbook, 3rd ed., John Wiley and Sons, New York, 2004.
[2] K.M. Shelfer, J.D. Procaccino, Smart card evolution, Com-mun. ACM 45 (7) (2002) 83—88.
[3] D. Backman, Smartcards: the intelligent way to security, Network Comput. 9 (9) (1998) 168—171.
[4] S.B. Guthery, Java card: internet computing on a smart card, IEEE Internet Comput. 1 (1) (2001) 57—59.
[5] L.C. Guillou, M. Ugon, J.J. Quisquater, The smart card—–a standardized security device dedicated to public cryptol-ogy in Gustavus Simmons, in: Contemporary Cryptolcryptol-ogy—– The Science of Information Integrity, IEEE Press, 1992, pp. 561—614.
[6] D. McElroy, E. Turban, Using smart cards in electronic com-merce, Int. J. Inform. Manage. 18 (1) (1998) 61—72. [7] A.T.S. Chan, Web-enabled smart card for ubiquitous access
of patient’s medical record, Comput. Networks 31 (11—16) (1999) 1591—1598.
[8] D. Dieng, The keys of success of a health card project—–the lessons learned from 9 health cards project, in: Proceedings of the 10th IEEE Symposium on Computer-Based Medical Systems (CBMS’97), 1997, pp. 227—230.
[9] ˙Inan G¨uler, R. Murat Zengin, Mustafa S¨onmez, Smart cards: a specific application in the hospital, J. Med. Syst. 22 (6) (1998) 405—419.
[10] B. Blobel, The European trusthealth project experiences with implementing a security infrastructure, Int. J. Med. Inform. 60 (2000) 193—201.
[11] J. Mohan, R.R.R. Yaacob, The Malaysian telehealth flagship application: a national approach to health data protection and utilisation and consumer rights, Int. J. Med. Inform. 73 (2004) 217—227.
[12] D. Trˇcek, R. Novak, Slovene smart card and IP based health-care information system infrastructure, Int. J. Med. Inform. 61 (2001) 33—43.
[13] Medical and Engineering Applications (MEDEA), Italy, A European Health Card, European Parliament, Directorate General for Research, Directorate A, The STOA Programme, Workplan Ref.: EP/IV/A/STOA/2000/09/02, March 2001. [14] Commission of the European Communities, Communication
from the commission concerning the introduction of a European health insurance card, Brussels, February 2003,
http://europa.eu.int/comm/employment social/news/ 2003/feb/hicard en.html.
[15] Taiwan’s Bureau of National Health Insurance, accessed on June 1, 2004,http://www.nhi.gov.tw/.
[16] The definitions of content of NHI-IC card and the specifi-cation for daily reporting medical service data, Taiwan’s Bureau of National Health Insurance, December, 2001. [17] Taiwan’s Bureau of National Health Insurance, accessed on
June 15, 2004http://www.nhi.gov.tw/iccard/iccard.htm. [18] The Department of Health, Taiwan,http://www.doh.gov.
tw.
[19] Department of Health (Taiwan), The Survey on Computer-ization of Healthcare Information Systems and their Appli-cations in Taiwan, Technical Reports, Taipei, Taiwan, March 2002,http://www.doh.gov.tw/statistic/data/.
[20] P.J. Kyees, R.C. McConnell, K. Sistanizadeh, ADSL: a new twisted-pair access to the information highway, IEEE Com-mun. Mag. 4 (3) (1995) 52—60.
[21] A.M. Odlyzko, The internet and other networks: utilization rates and their implications, Inform. Econ. Policy 12 (2000) 341—365.
[22] P.T. Yang, The study on the impact of incorporating national health insurance IC card into the hospital information sys-tems in Taiwan, Master Thesis, Graduate Institute of Medi-cal Informatics, Taipei MediMedi-cal University, July 2004.