Greater Risk of Hip Fracture in Hemodialysis than in Peritoneal DialysisIncreased Risk of Hip Fracture in End-Stage Renal Disease Patients Treated with Hemodialysis: A Nationwide 11-Year Population-Based Cohort
Study in Taiwan Yen-Jen Chen, MD1,2,3 Pei-Tseng Kung, Sc.D 4 Yueh-Hsin Wang, MS1 Chiu-Chin Huang, MD5 Shih-Chang Hsu, MS6 Wen-Chen Tsai, Dr.PH 1 Horng-Chaung Hsu, MD2,3
1. Department of Health Services Administration, China Medical University, Taiwan 2. Department of Orthopedic Surgery, China Medical University Hospital, Taiwan 3. School of Medicine, China Medical University, Taichung, Taiwan
4. Department of Health Administration, Asia University, Taiwan. 5. Division of Nephrology, China Medical University Hospital, Taiwan 6. Landseed Hospital, TaoYuan, Taiwan
Corresponding Author: Dr. Wen-Chen Tsai, Professor
Address: 91 Hsueh-Shih Road, Taichung, Taiwan 40402, R.O.C. Tel.: +886-422073070; Fax: +886-422028895
Abstract
Context Patients on peritoneal dialysis (PD) had higher risks of 25-hydroxyvitamin D deficiency than hemodialysis (HD). Will patients treated with PD have an increased risk of hip fracture?
Objectives To examine the relationship between dialysis modality and risk of hip fracture, and evaluate the risk factors of hip fracture in dialysis patients.
Design, Setting, and Participants The data in this study were extracted from the National Health Insurance Research Database in Taiwan (NHIRD). Incident end-stage renal disease (ESRD) patients who underwent dialysis for more than 3 months and were older than 50 years were selected from January 1998 to December 2008. Patients with a history of previous hip fracture before dialysis and medication with
anti-osteoporotic drugs were excluded. The study cohorts were matched with propensity scores, and 8 HD patients were randomly matched for each identified PD patient. A total of 31 554 patients including 28 048 HD and 3506 PD patients were included in the study. We conducted Cox proportional hazards regression to examine the effects of dialysis modality and other variables on hip fracture risk.
Main outcome measure The hazard ratio (HR) was used to assess various effects on hip fracture risk.
98.49% (2548/2587) of these hip fractures were among patients treated with HD. The incidence of hip fracture in HD patients was 4.29% (2548/59 457), and 0.84% (39/4667) in PD patients; the overall incidence of hip fracture in dialysis patients was 4.03% (2587/64 124). Dialysis modality, sex, age, presence of cardiovascular disease, diabetics, cancer, medication with antiepileptic drugs, diuretics, steroids, and vitamin D had statistically significant associations with hip fracture. Patients on HD had an increased risk of hip fracture compared to patients on PD; the HR was 1.52 (95% CI: 1.09-2.12, P = .02).
Conclusion In this population-based cohort study, HD had a greater hip fracture risk compared to PD; the HR was 1.52 (95% CI: 1.09–2.12, P = .02). We should focus more on patients treated with HD, by improving health education, medication for osteoporosis, and fall prevention, to reduce the risk of hip fractures.
Introduction
Among osteoporotic fractures, hip fractures are associated with the highest morbidity and mortality; over 50% of patients are institutionalized within the first year after a fracture.1 The prevalence of osteoporotic hip fractures among dialysis patients is higher than that of the general population.2 A retrospective study reported that the incidence of hip fractures among hemodialysis (HD) patients was 17.4 times higher than that of the general population and occurred at a younger age.3
Approximately 90% of patients with end-stage renal disease (ESRD) worldwide are maintained on HD and 10% are maintained on peritoneal dialysis (PD).4 In a study of 242 patients with ESRD, patients on PD had the highest risk of 25-hydroxyvitamin D deficiency. Abnormalities in vitamin D metabolism and parathyroid hormone (PTH) secretion result in a change of the trabecular microarchitecture, thinning, and
increased porosity of the cortical bone;5,6 thus, whether patients treated with PD have an increased risk of hip fracture must be assessed.
We examine the incidence of hip fracture in dialysis patients in Taiwan and compare the incidence and hazard ratio (HR) between HD and PD patients.
Materials and methods
Database and study population
The data in this study were obtained from the National Health Insurance Research Database (NHIRD) of the Taiwanese National Health Insurance (NHI) program, which is an electronic medical claims database. This database includes the medical records of all patients insured by the NHI in Taiwan. Approximately 99.59% of Taiwan’s population was insured by the end of 2009. All dialysis patients in Taiwan were registered in this database. This study was approved by the Institutional Review Board (IRB) of China Medical University.
Incident ESRD patients who underwent dialysis for more than 3 months and who were older than 50 years were selected from January 1998 to December 2008. Patients with missing data (376 patients), a history of previous hip fractures before dialysis (2361 patients), and medicated with anti-osteoporotic drugs before dialysis or hip fracture (311 patients) were excluded.
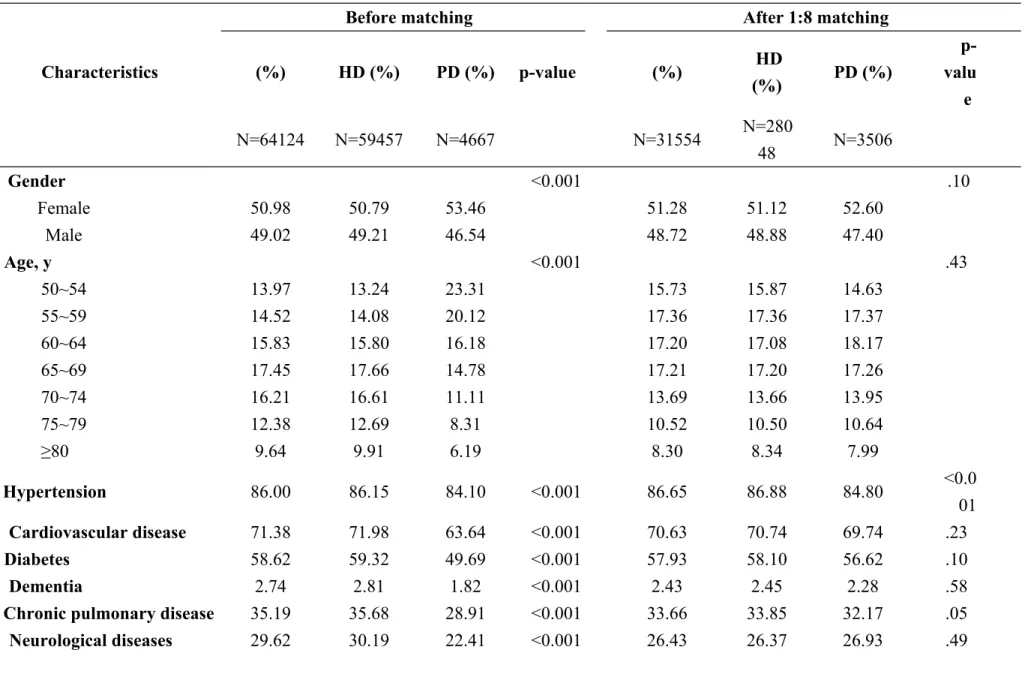
A total of 64 124 incident ESRD patients comprised the unmatched cohort: 59 457 (92.72%) HD and 4667 (7.28%) PD patients (Table 1).
Ascertainment of dialysis modality
PD patients may initially receive temporary HD. Thus, dialysis modality was defined as the modality at Day 90 after the first dialysis (intent-to-treat).
The number of hip fractures that occurred during follow-up was determined using information in the NHIRD hospitalization files, which include data on inpatient hospital stays. Hospitalization data were considered fromJanuary 1, 1998 to December 31, 2008 for the current analysis. Hip fractures were identified using International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes indicating cervical, intertrochanteric, or subtrochanteric hip fractures.
Propensity Score Matching
The proportion of PD patients is only 7.28% (4667/64 124), and patients treated with PD were different compared to patients treated with HD, for age, health status, and especially comorbidities, which are important covariates associated with hip fracture risk. Therefore, we established study cohorts who were matched with propensity scores; 8 HD patients were randomly matched for each identified PD patient. The propensity score was estimated using a logistic regression model including covariates that are generally considered important factors associated with hip fractures.These covariates included sociodemographic variables andbaseline comorbidities (Table 2). The sociodemographic variables used in this study included sex, age, premium-based monthly salary, and urbanization of the residence area. The premium-based monthly salary was divided into 8 levels. Urbanization of the
residence area was divided into 7 levels. The baseline comorbidity history included hypertension, cardiovascular disease (CVD), diabetes, dementia, chronic pulmonary disease, neurological disease, rheumatic disease, and cancer. All illnesses were identified using the ICD-9-CM.
Thereafter, 31 554 patients, of whom 28 048 were HD and 3506 were PD patients, were included in the study.
Study endpoint
All study patient cases were followed to ascertain whether they had subsequent admissions for hip fracture. The follow-up period started from the first dialysis until the first of the following: date of hip fracture diagnosis; date of death; date of
withdrawal from the NHI program, date of renal transplantation, or date of follow-up termination (December 31, 2009).
Statistical analysis
We used the chi-square test to verify the matching efficiency of the sample distributions and differences between PD and HD patients. The incidence density of hip fractures was calculated for the 2 groups.
We conducted the Cox proportional hazards model, estimating the HR and 95% confidence interval (CI) to examine the effects of dialysis modality and other
variables on hip fracture risk. Variables were included in the multivariate model either in an attempt to control for confounding factors or as independent risk factors of
fracture after adjustment for other covariates. Models were adjusted for
sociodemographic variables,baseline comorbidities, and oral medications. The oral medications included in this study were antiepileptic drugs, calcium, diuretics, steroids, and vitamin D.
All analyses were performed using SAS 9.1 statistical software (SAS Institute, Inc., Cary, NC, USA). The results were considered statistically significant when two-tailed P values were less than .05.
Results
Subjects Characteristics
The characteristics of the study population before and after matching are shown on Tables 1 and 2. Over half the patients (50.98%) were women, and 49.02% were men. The incident number of ESRD patients increased yearly, from 4533 patients in 1999 to 7370 patients in 2008. The percentage of patients who underwent PD increased steadily from 3.43% (156/4543) in 1998 to 10.53% (776/7370) in 2008. The peak age group in all dialysis patients was 65–69 years (17.45%), followed by 70–74 years (16.21%) and 60–64 years (15.83%). The peak age group in PD patients was 50–54 years and decreased gradually with increasing age.
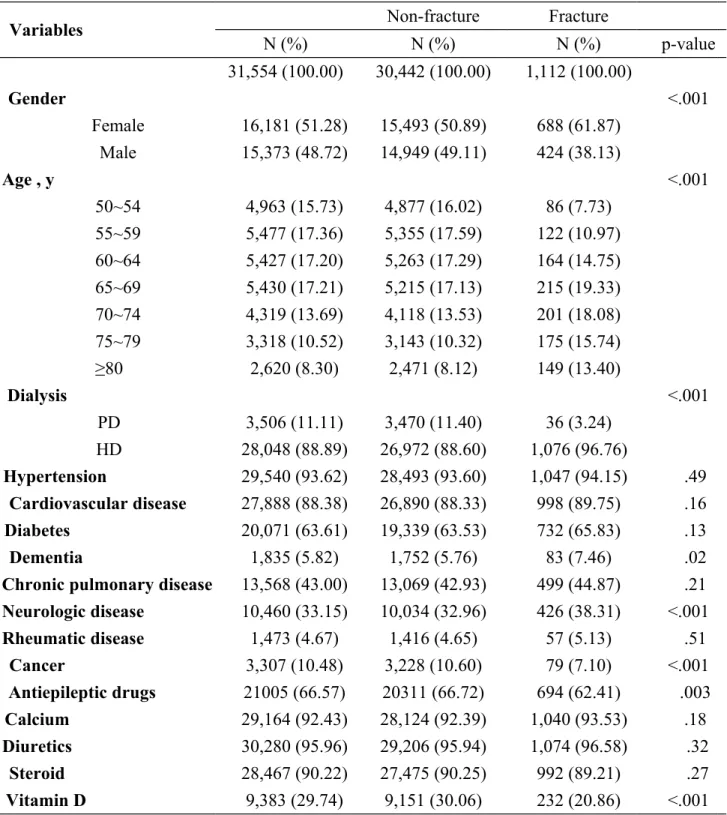
A total of 2587 hip fractures were identified in 64 124 dialysis patients. The overall incidence of hip fractures in dialysis patients was 4.03% (2587/64 124), and 98.49% (2548/2587) of hip fractures were among patients treated with HD. The incidence of hip fracture in HD patients was 4.29% (2548/59 457) and 0.84% (39/4667) in PD patients.
The results of bivariate analysis are shown in Table 3. Sex, age, premium-based monthly salary, dialysis modality, presence of dementia, neurological disease, cancer, medication with antiepileptic drugs, diuretics, and vitamin D had statistically
significant associations with hip fracture (P < .05). Urbanization of the residence area, presence of hypertension, CVD, diabetes, chronic pulmonary disease, rheumatic
disease, medication with calcium, and steroids had no statistically significant association with hip fracture.
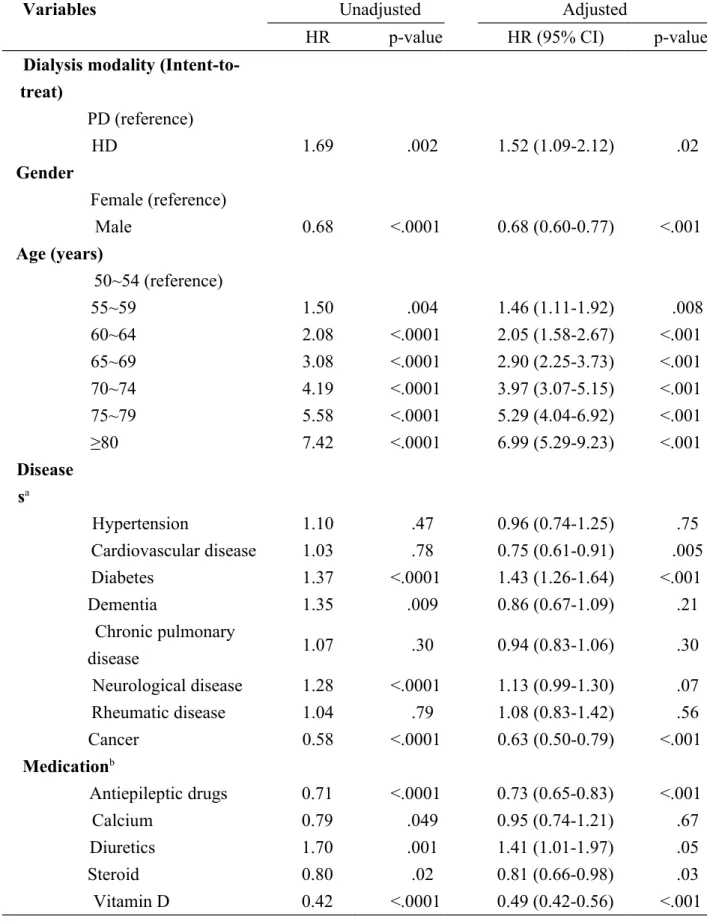
The results of the multivariate Cox proportional hazards model analysis are shown in Table 4. Dialysis modality, sex, age, presence of CVD, diabetes, cancer,
medication with antiepileptic drugs, diuretics, steroids, and vitamin D had a statistically significant association with hip fracture. However, premium-based monthly salary, urbanization of the residence area, presence of hypertension, dementia, neurological disease, chronic pulmonary disease, rheumatic disease, and medication with calcium had no statistically significant association with hip fracture. Factors that were independently associated with an increased risk of hip fracture included HD, increasing age, female sex, presence of diabetes, and medication with diuretics. Conversely, patients with CVD, cancer, medication with antiepileptic drugs, steroids, and vitamin D were independently associated with a decreased risk of hip fracture. Patients on HD had an increased risk of hip fracture compared to patients on PD; HR was 1.52 (95% CI: 1.09–2.12, P = .02).
More PD patients switched between PD and HD compared to HD patients in this study. Therefore, several biases may exist in the group of PD patients. Three models (intent-to-treat, as-treated, and PD combined HD vs. PD or HD only) were analyzed to solve this issue. HD patients had an increased risk of hip fracture in all 3 models
(Table 5).
Discussions
The causes of renal osteodystrophy among ESRD patients are multiple, including secondary hyperparathyroidism, abnormal
vitamin D metabolism, relative immobility, hypogonadism, β2- microglobulin-associated amyloidosis, chronic acidosis, aluminum deposition, osteomalacia, steroid therapy, and other disorders.7
Age-associated osteoporosis should also be considered. As renal failure progresses, ensuing abnormalities in vitamin D metabolism and PTH secretion result in a change of the trabecular microarchitecture, thinning, and an increased porosity of the cortical bone5; thus, hip fracture rates are significantly increased in dialysis patients and transplant recipients.6
The data from the US Renal Data System (USRDS) demonstrated a 4-fold increase of hip fracture risk among ESRD patients,8 and the mortality rate of dialysis patients
after hip fracture was 2.7 times higher than of patients without a hip fracture.9 In this
study, the incidence of hip fracture was 4.03% in 64 124 dialysis patients, which is significantly higher than the incidence (0.58%) in the general population of Taiwan.10
The Cox proportional hazards model demonstrated that increasing age, female sex, presence of diabetes, and medication with diuretics were independently associated with increased hip fracture risk; medication with vitamin D was associated with decreased hip fracture risk. These findings were consistent with those of previous studies.11–16
with a decreased risk of hip fracture. This finding was inconsistent with those of previous studies. Sennerby et al studied 31 936 Swedish twins and demonstrated that a diagnosis of CVD was significantly associated with a risk of subsequent hip
fracture.17 However, their study did not target ESRD patients, and their CVD
subdiagnosis included stroke; stroke was demonstrated to increase hip fracture risk 2-fold.18 If stroke had been excluded from CVD diagnosis in their study, the result may
have been different. In a study of ESRD patients, a USRDS Dialysis Morbidity and Mortality Study Wave 1 (DMMS-1) demonstrated that the presence of peripheral vascular disease (PVD) was independently associated with an increased risk of hip fracture, but the presence of coronary artery disease (CAD) was not. In this study, the HR of CVD before adjustment was 1.03 (P = .77), and the HR after adjustment was 0.79 (P = .03). Further studies are required to confirm this finding and improve the understanding of the impact of CVD on the risk of hip fracture in dialysis patients.
Other risk factors that were inconsistent with previous studies included the presence of dementia, neurological disease, chronic pulmonary disease, and
medications with steroids and antiepileptic drugs. However, several differences may exist because the populations targeted by previous studies were osteoporotic patients, and not ESRD patients. Further studies are required to improve the understanding of risk factors associated with hip fractures of dialysis patients.
Numerous debates on which dialysis modality is “superior” have taken place in recent decades. However, most debates focused on which modality was associated with a better survival rate or better quality of life for patients with ESRD. Only one study group has compared the risk of hip fracture between PD and HD patients.9 Stehman-Breen et al used the data from USRDS DMMS-1 to analyze the risk factors of hip fracture among ESRD patients and indicated that dialysis modality was not an important predictor of hip fracture. The incidence rate was 7.91 per 1000 patient-years in the HD group and 3.47 in the PD group. However, the adjusted relative risk of PD was 0.52, and there was no statistically significance (P = .52). Because their study population numbered 4952, the mean follow-up time was 2.86 years, and only 1 patient in the PD group had a hip fracture; thus, the statistical non-significance may have been caused by the small sample. The authors acknowledged that they had limited power in addressing the impact of dialysis modality on hip fracture risk.
Several differences may have existed between patients treated with PD and HD because of the difference in dialysis modality. HD patients showed a higher incidence of delayed graft function and primary allograft failure, had elevated erythrocyte superoxide dismutase, lower glutathione peroxidase and catalase activities, decreased levels of Se, Zn, and Fe, and attenuation of serum antioxidant capacity.19-21 However, the most important difference of PD and HD that may influence the risk of hip
fracture is vitamin D. Elder et al examined 242 patients with renal failure, and found that patients on PD had lower levels of 25-hydroxyvitamin D than those on HD.22 Furthermore, they identified positive associations between 25-hydroxyvitamin D levels and the Z score of bone mineral density (BMD), and an association between femoral neck BMD with a fracture at any site.22
These studies indicate that patients with lower vitamin D levels have a lower BMD and a higher risk of fracture. Patients on PD had lower vitamin D levels and
potentially have a higher risk of hip fracture than patients on HD. Conversely, this study demonstrated that patients on HD had a higher risk of hip fracture; the HR was 1.52. This result cannot be explained with the theory of vitamin D and BMD.
Furthermore, several other factors may influence the risk of hip fracture, including age, sex, race, a history of systemic diseases or fractures or falls, physical activity, limitations in activities or decreased mobility in daily living, tobacco or alcohol consumption, use of medicine (including calcium and vitamin D), vision status, age of menopause, body mass index, and muscle strength.23–26 Lan et al indicated that low
milk intake, peak expiratory flow rate, hand grip strength in women, and low mini-mental state examination scores in men were independently associated with an increased risk of hip fracture for elderly people in Taiwan.25 Additional risk factors for fracture among dialysis patients included peripheral vascular disease9 and either
low or high PTH levels.27,28Patients on HD should present themselves at a hospital 3 times per week, but patients on PD are not. Patients on HD may have intradialytic hypotension, which may raise the risk of falling and increase the risk of fracture.
Therefore, other factors may influence HD toward higher hip fracture risk. This study was not designed to elucidate the pathophysiological mechanism of dialysis and hip fracture. Further studies are required to confirm our results and improve the
understanding of risk factors for hip fractures in dialysis patients.
The 1-year mortality rate after hip fracture was higher than that without hip fracture in dialysis patients; thus, we should focus more on patients treated with HD, by improving health education, medication for osteoporosis, and fall prevention, to reduce the risk of hip fractures.
Limitations
This study has several limitations. First, a retrospective study was used to ascertain the information regarding causes and effects from existing claims data. Other
information that may influence the risk of hip fracture, such as laboratory data, BMD, health behavior, and patient lifestyles, were unavailable in the claims data.
However, this study represented the experience of the entire incident dialysis population spanning an 11-year period in Taiwan, and the available sample size was
clinically relevant indications and may assist in dialysis modality choices for ESRD patients in Taiwan.
Conclusion
In this population-based cohort study, HD patients had a higher risk of hip fracture compared to PD patients, and the HR was 1.52 (95% CI: 1.09–2.12, P = .02). We should focus more on patients treated with HD, by improving health education, medication for osteoporosis, and fall prevention, to reduce the risk of hip fractures.
Acknowledgements
The authors are grateful for financial support from China Medical University and Asia University (grant numbers: CMU998-ASIA-183, DOH100-TD-B-111-004) as well as the National Science Council (grant number: NSC98-2410-H-468-015-MY2) in Taiwan.
References
1. Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet 2002;359:1761-7.
Disease, Prospective Testing Under Real World Environments (FRACTURE): a prospective study. BMC Nephrol;11:17.
3. Coco M, Rush H. Increased incidence of hip fractures in dialysis patients with low serum parathyroid hormone. Am J Kidney Dis 2000;36:1115-21.
4. Grassmann A, Gioberge S, Moeller S, Brown G. ESRD patients in 2004: global overview of patient numbers, treatment modalities and associated trends. Nephrol Dial Transplant 2005;20:2587-93.
5. Parfitt AM. A structural approach to renal bone disease. J Bone Miner Res 1998;13:1213-20.
6. Leonard MB. A structural approach to skeletal fragility in chronic kidney disease. Semin Nephrol 2009;29:133-43.
7. Leinau L, Perazella MA. Hip fractures in end-stage renal disease patients: incidence, risk factors, and prevention. Semin Dial 2006;19:75-9.
8. Alem AM, Sherrard DJ, Gillen DL, et al. Increased risk of hip fracture among patients with end-stage renal disease. Kidney Int 2000;58:396-9.
9. Stehman-Breen CO, Sherrard DJ, Alem AM, et al. Risk factors for hip fracture among patients with end-stage renal disease. Kidney Int 2000;58:2200-5.
10. Shao CJ, Hsieh YH, Tsai CH, Lai KA. A nationwide seven-year trend of hip fractures in the elderly population of Taiwan. Bone 2009;44:125-9.
an urban tertiary care hospital with osteoporotic fractures: correlations with risk factors, fracture type, gender and ethnicity. Osteoporos Int 2006;17:410-6. 12. Brown JP, Josse RG. 2002 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada. CMAJ 2002;167:S1-34.
13. Chen HF, Ho CA, Li CY. Increased risks of hip fracture in diabetic patients of Taiwan: a population-based study. Diabetes Care 2008;31:75-80.
14. Nguyen ND, Pongchaiyakul C, Center JR, Eisman JA, Nguyen TV.
Identification of high-risk individuals for hip fracture: a 14-year prospective study. J Bone Miner Res 2005;20:1921-8.
15. Rejnmark L, Vestergaard P, Mosekilde L. Fracture risk in patients treated with loop diuretics. J Intern Med 2006;259:117-24.
16. Taylor BC, Schreiner PJ, Stone KL, et al. Long-term prediction of incident hip fracture risk in elderly white women: study of osteoporotic fractures. J Am Geriatr Soc 2004;52:1479-86.
17. Sennerby U, Melhus H, Gedeborg R, et al. Cardiovascular diseases and risk of hip fracture. JAMA 2009;302:1666-73.
18. Pouwels S, Lalmohamed A, Leufkens B, et al. Risk of hip/femur fracture after stroke: a population-based case-control study. Stroke 2009;40:3281-5.
19. Freitas C, Fructuoso M, Martins LS, et al. Posttransplant outcomes of peritoneal dialysis versus hemodialysis patients. Transplant Proc;43:113-6.
20. Guo CH, Wang CL, Chen PC, Yang TC. Linkage of Some Trace Elements, Peripheral Blood Lymphocytes, Inflammation, and Oxidative Stress in Patients Undergoing Either Hemodialysis or Peritoneal Dialysis. Perit Dial Int.
21. Rysz J, Stolarek RA, Pedzik A, Nowicki M, Nowak D. Serum antioxidant capacity is preserved in peritoneal dialysis contrary to its robust depletion after hemodialysis and hemodiafiltration sessions. Ther Apher Dial;14:209-17.
22. Elder GJ, Mackun K. 25-Hydroxyvitamin D deficiency and diabetes predict reduced BMD in patients with chronic kidney disease. J Bone Miner Res
2006;21:1778-84.
23. Benetos IS, Babis GC, Zoubos AB, Benetou V, Soucacos PN. Factors affecting the risk of hip fractures. Injury 2007;38:735-44.
24. Dubey A, Koval KJ, Zuckerman JD. Hip fracture epidemiology: a review. Am J Orthop (Belle Mead NJ) 1999;28:497-506.
25. Lan TY, Hou SM, Chen CY, et al. Risk factors for hip fracture in older adults: a case-control study in Taiwan. Osteoporos Int;21:773-84.
26. Wehren LE, Magaziner J. Hip fracture: risk factors and outcomes. Curr Osteoporos Rep 2003;1:78-85.
27. Danese MD, Kim J, Doan QV, et al. PTH and the risks for hip, vertebral, and pelvic fractures among patients on dialysis. Am J Kidney Dis 2006;47:149-56. 28. Kaneko TM, Foley RN, Gilbertson DT, Collins AJ. Clinical epidemiology of
long-bone fractures in patients receiving hemodialysis. Clin Orthop Relat Res 2007;457:188-93.
Table 2. Patient characteristics before and after Propensity Score (PS) Matching
Before matching After 1:8 matching
Characteristics (%) HD (%) PD (%) p-value (%) HD (%) PD (%) p-valu e N=64124 N=59457 N=4667 N=31554 N=280 48 N=3506 Gender <0.001 .10 Female 50.98 50.79 53.46 51.28 51.12 52.60 Male 49.02 49.21 46.54 48.72 48.88 47.40 Age, y <0.001 .43 50~54 13.97 13.24 23.31 15.73 15.87 14.63 55~59 14.52 14.08 20.12 17.36 17.36 17.37 60~64 15.83 15.80 16.18 17.20 17.08 18.17 65~69 17.45 17.66 14.78 17.21 17.20 17.26 70~74 16.21 16.61 11.11 13.69 13.66 13.95 75~79 12.38 12.69 8.31 10.52 10.50 10.64 ≥80 9.64 9.91 6.19 8.30 8.34 7.99 Hypertension 86.00 86.15 84.10 <0.001 86.65 86.88 84.80 <0.0 01 Cardiovascular disease 71.38 71.98 63.64 <0.001 70.63 70.74 69.74 .23 Diabetes 58.62 59.32 49.69 <0.001 57.93 58.10 56.62 .10 Dementia 2.74 2.81 1.82 <0.001 2.43 2.45 2.28 .58
Rheumatic diseases 3.31 3.29 3.56 .34 3.34 3.32 3.48 .65
Cancer 6.19 6.37 3.90 <0.001 4.74 4.75 4.735 .99
Table 3. Bivariate Analysis of non-fracture and fracture
Variables Non-fracture Fracture
N (%) N (%) N (%) p-value 31,554 (100.00) 30,442 (100.00) 1,112 (100.00) Gender <.001 Female 16,181 (51.28) 15,493 (50.89) 688 (61.87) Male 15,373 (48.72) 14,949 (49.11) 424 (38.13) Age , y <.001 50~54 4,963 (15.73) 4,877 (16.02) 86 (7.73) 55~59 5,477 (17.36) 5,355 (17.59) 122 (10.97) 60~64 5,427 (17.20) 5,263 (17.29) 164 (14.75) 65~69 5,430 (17.21) 5,215 (17.13) 215 (19.33) 70~74 4,319 (13.69) 4,118 (13.53) 201 (18.08) 75~79 3,318 (10.52) 3,143 (10.32) 175 (15.74) ≥80 2,620 (8.30) 2,471 (8.12) 149 (13.40) Dialysis <.001 PD 3,506 (11.11) 3,470 (11.40) 36 (3.24) HD 28,048 (88.89) 26,972 (88.60) 1,076 (96.76) Hypertension 29,540 (93.62) 28,493 (93.60) 1,047 (94.15) .49 Cardiovascular disease 27,888 (88.38) 26,890 (88.33) 998 (89.75) .16 Diabetes 20,071 (63.61) 19,339 (63.53) 732 (65.83) .13 Dementia 1,835 (5.82) 1,752 (5.76) 83 (7.46) .02
Chronic pulmonary disease 13,568 (43.00) 13,069 (42.93) 499 (44.87) .21 Neurologic disease 10,460 (33.15) 10,034 (32.96) 426 (38.31) <.001 Rheumatic disease 1,473 (4.67) 1,416 (4.65) 57 (5.13) .51 Cancer 3,307 (10.48) 3,228 (10.60) 79 (7.10) <.001 Antiepileptic drugs 21005 (66.57) 20311 (66.72) 694 (62.41) .003 Calcium 29,164 (92.43) 28,124 (92.39) 1,040 (93.53) .18 Diuretics 30,280 (95.96) 29,206 (95.94) 1,074 (96.58) .32 Steroid 28,467 (90.22) 27,475 (90.25) 992 (89.21) .27 Vitamin D 9,383 (29.74) 9,151 (30.06) 232 (20.86) <.001 Abbreviation: PD, peritoneal dialysis; HD, hemodialysis.
Table 4 Related factors of fracture in the multivariate model
Variables Unadjusted Adjusted
HR p-value HR (95% CI) p-value
Dialysis modality (Intent-to-treat) PD (reference) HD 1.69 .002 1.52 (1.09-2.12) .02 Gender Female (reference) Male 0.68 <.0001 0.68 (0.60-0.77) <.001 Age (years) 50~54 (reference) 55~59 1.50 .004 1.46 (1.11-1.92) .008 60~64 2.08 <.0001 2.05 (1.58-2.67) <.001 65~69 3.08 <.0001 2.90 (2.25-3.73) <.001 70~74 4.19 <.0001 3.97 (3.07-5.15) <.001 75~79 5.58 <.0001 5.29 (4.04-6.92) <.001 ≥80 7.42 <.0001 6.99 (5.29-9.23) <.001 Disease sa Hypertension 1.10 .47 0.96 (0.74-1.25) .75 Cardiovascular disease 1.03 .78 0.75 (0.61-0.91) .005 Diabetes 1.37 <.0001 1.43 (1.26-1.64) <.001 Dementia 1.35 .009 0.86 (0.67-1.09) .21 Chronic pulmonary disease 1.07 .30 0.94 (0.83-1.06) .30 Neurological disease 1.28 <.0001 1.13 (0.99-1.30) .07 Rheumatic disease 1.04 .79 1.08 (0.83-1.42) .56 Cancer 0.58 <.0001 0.63 (0.50-0.79) <.001 Medicationb Antiepileptic drugs 0.71 <.0001 0.73 (0.65-0.83) <.001 Calcium 0.79 .049 0.95 (0.74-1.21) .67 Diuretics 1.70 .001 1.41 (1.01-1.97) .05 Steroid 0.80 .02 0.81 (0.66-0.98) .03 Vitamin D 0.42 <.0001 0.49 (0.42-0.56) <.001 N=31,554
ratio.
aNo disease group was used as reference group. bNo medication group was used as reference group.