Original Article
Introduction
Estrogen deficiency may be associated with the development of urinary incontinence in women.
There is evidence that estrogen applied locally in the form of vaginal cream improves urinary incontinence [1]. The physiological effects of estrogenic compounds are modulated by estrogen receptor subtypes alpha (ERα) and beta (ERβ) [2]. Lang et al. reported a positive correlation
between estrogen receptors and the number of postmenopausal years in women with stress urinary incontinence (SUI) [3]. In another study, ERα score and number of blood vessels were significantly higher in premenopausal group when compared with postmenopausal group with pelvic organ prolapse [4]. ERβ was first discovered in 1996. Since then, the traditional estrogen receptor has been denoted ERα [5]. ERβ has wide tissue distribution and ERβ- selective agonist is a potential target for treatment of various diseases. Chen et al. detected ERβ-mRNA in vaginal wall tissue samples of premenopausal women but not in vaginal wall tissue samples of postmenopausal women [6].
Since estrogen deficiency is one of the etiologies
Estrogen receptor expression and vascularization of anterior vaginal wall after local estrogen supplement in postmenopausal women with urinary incontinence
Soo-Cheen Ng
1,2,3, Yi-Ju Lee
2,4, Hsien‐Yu Peng
5, Jeng-Dong Hsu
2,4, Gin-Den Chen
1,3*Department of Obstetrics and Gynecology, Chung Shan Medical University Hospital, Taichung, Taiwan School of Medicine, Chung Shan Medical University, Taichung, Taiwan.
Institute of Medicine, Chung Shan Medical University, Taichung, Taiwan.
Department of Pathology, Chung Shan Medical University Hospital, Taichung, Taiwan.
Department of Medicine, Mackay Medical College, New Taipei City, Taiwan.
* Corresponding Author: Gin-Den Chen
Address: No.110, Section 1, Chien-Kuo N. Road, Taichung, 40201, Taiwan, R.O.C
Tel: +886-4-24789595 ext. 21721
Purpose: To evaluate the effects of local vaginal estrogen supplement on estrogen receptor expression and vascularization of anterior vaginal wall in post-menopausal women with stress urinary incontinence.
Methods: Twenty-five post-menopausal women who were to receive anti-incontinence surgery were invited to participate. Women in the estrogen supplement group applied topical estrogen cream vaginally at a dose of 1g every two days. Immunohistochemical staining for estrogen receptor β and CD34 (endothelial cell marker of blood vessels) was performed on anterior vaginal wall tissue samples.
Data was compared between the estrogen supplement group and the control group.
Results: There were no significant differences in ERβ ratio or number of CD34 stained blood vessels between the groups.
Conclusion: ERβ expression and vascularization did not increase after vaginal estrogen supplement in postmenopausal women with stress urinary incontinence.
Keywords: postmenopausal, stress urinary incontinence, vaginal estrogen supplement, estrogen receptor, vascularization
of pelvic floor dysfunction, it is important to investigate whether estrogen replacement affects estrogen receptors, especially Erβ, in female urogenital organs. The aim of this study was to evaluate the effects of vaginal estrogen replacement on ERβ expression and vascularization (CD34 expression) in post-menopausal women with SUI.
Materials and Methods
From January 2016 to June 2016, 25 post-menopausal women who were to receive anti-incontinence surgery due to SUI were invited to participate in this study.
All subjects were asked to sign a written informed consent form and received pelvic examination for the evaluation of the severity of SUI and pelvic organ prolapse (POP-Q ordinal stage). Urodynamic study was performed to evaluate bladder function before operation. Patients were assigned to vaginal estrogen replacement group or control group. The vaginal estrogen replacement group received estrogen cream (0.625mg conjugated equine estrogens per 1g vaginal cream) to apply vaginally every two days in the evening for at least 2 weeks. Women with breast cancer or high risk for breast cancer were excluded.
The study protocol was approved by the Chung Shan Medical University Hospital Institutional Review Board (CSMUH No.CS15117)
Sampling and tissue preparation
Anterior vaginal wall tissue samples (full layers, 10 x 20mm) were obtained from the cut edge of mid- urethral sling insertion incision about 1.5cm below the urethral meatus after the surgical procedure and before closure of the anterior vaginal wall incision.
The extracted tissue was divided into several tissue blocks and frozen for subsequent use.
Immunohistochemical staining for ERβ and CD34 (endothelial cell marker of blood vessels) was performed on Benchmark XT autostainer (Ventana Medical Systems, AZ, USA). Paraffin sections of 3 µm thickness were baked at 75 °C for 30 minutes and deparaffinized in the instrument with EZ prep solution (Ventana Benchmark XT platform). Heat Induced Epitope Retrieval (HIER) was performed in Tris-EDTA buffer pH 7.8 at 95°C for 30 min (mild CC1) on Ventana Benchmark XT.
To block endogenous peroxides and proteins, these steps were conducted using UltraView Universal DAB Inhibitor. Next, primary antibodies ERβ (dilution 1:50, Santa Cruz, USA) and CD34 (dilution 1:50, Santa Cruz, USA) were applied to the tissue sections, followed by incubation with dilution antibody at 37 °C for 60 min (ERβ) or 32 min (CD34).
Reactions were detected using the UltraView Universal DAB Detection kit. Finally, the slides were counterstained with Hematoxylin for 1 min and washed for 10 min. EVG staining was performed using a standard protocol in our laboratory. The paraffin sections were deparaffinized in xylene and rehydrated through a descending series of alcohol to water. Slides were returned to 70% alcohol solution for 3 sec and stained in Wiegert’s resorcin-fuchsin solution for 60 min. The sections were rinsed in 100% alcohol solution for 5 sec followed by staining with Wiegert’s iron hematoxylin for 30 sec, rinsed in running water for 5 sec, and stained with van Gieson's solution for 5 min. Finally, the slides were rinsed quickly in 95% alcohol solution, cleared, and mounted.
Calculations
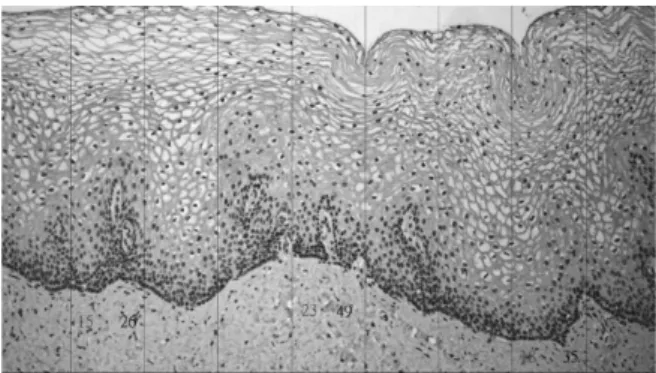
Figure 1 illustrates the method of calculation of Erβ expression. Totally, 3 areas were selected and coded ERβ-1, ERβ-2 and ERβ-3, respectively.
ERβ ratio was defined as the number of cell nuclei positively stained divided by all the nuclei counted in the selected area. Vessel counting was performed by CD34 staining on the lamina propria of the anterior vaginal wall.
Figure 1. ERβ immunohistochemical staining. Each section was divided into 9 areas with 3 areas selected for calculation. Numbers of positively stained and unstained cell nuclei were determined.
Statistics
SPSS software version 20.0 (SPSS Inc., Chicago, IL, USA) was used for data analysis. Mann- Whitney U test was applied to the evaluation of the median of continuous variables between groups and Fisher’s exact test to the evaluation of two nominal variables. A P value of less than 0.05 was considered significantly different.
Results
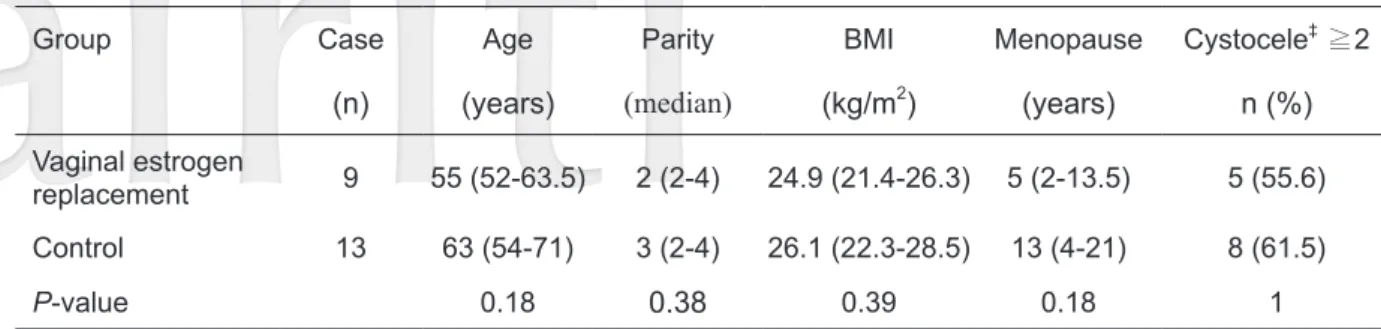
Three patients in the vaginal estrogen replacement group discontinued the estrogen cream due to fear of increased breast cancer risk and were not included in the analysis. The data of the vaginal estrogen replacement group (n=9) and control group (n=13) was analyzed and compared. The characteristics of the study subjects are shown in Table 1. There were no statistically significant differences in
age, parity, BMI, length of menopause, or high stage cystocele between the groups. The mean duration of vaginal estrogen application was 24 days in the replacement group. Table 2 shows no significant difference in the ERβ ratio calculated from 3 separate areas between the vaginal estrogen replacement group and the control group. In terms of anterior vaginal wall vascularization, there were no significant differences between the two groups in the number of CD34-stained blood vessels.
Discussion
In the present study, ERβ expression did not change significantly after vaginal estrogen replacement in postmenopausal women with SUI.
Our results were consistent with those of previous studies. Fuermetz et al. evaluated the changes in estrogen receptors and progesterone receptors in the posterior vaginal wall of postmenopausal women who received intravaginal estrogen therapy (estriol Table 1. Comparisons of two post-menopausal sub-groups with stress urinary incontinence
Group Case Age Parity BMI Menopause Cystocele‡ ≧2
(n) (years) (median) (kg/m2) (years) n (%)
Vaginal estrogen
replacement 9 55 (52-63.5) 2 (2-4) 24.9 (21.4-26.3) 5 (2-13.5) 5 (55.6) Control 13 63 (54-71) 3 (2-4) 26.1 (22.3-28.5) 13 (4-21) 8 (61.5)
P-value 0.18 0.38 0.39 0.18 1
Data presented as median (IQR), mean or number (percentage).
IQR=Interquartile range.
Mann-Whitney U test and ‡Fisher's exact test.
Table 2. Receptor levels in anterior vaginal wall; comparisons of vaginal estrogen replacement group and control group
Variables Control
(n=13) Vaginal estrogen replacement
(n=9) P-value
ERβ-1 0.33 (0.2-0.36) 0.28 (0.22-0.36) 0.78
ERβ-2 0.23 (0.19-0.29) 0.21 (0.15-0.34) 0.76
ERβ-3 0.26 (0.21-0.34) 0.32 (0.19-0.41) 0.97
CD34 5 (3-7) 3 (2-4.5) 0.16
ERβ: estrogen receptor β Mann-Whitney U test
0.5mg) every evening for 6 weeks [7]. Compared to postmenopausal female cadavers, local vaginal estrogen therapy did not increase ERβ expressions in the epithelium, stroma, and connective tissue of the posterior vaginal wall. Fuermetz et al. also evaluated steroid receptor expression by immunohistochemical staining. In another study, steroid receptor changes were assessed via messenger RNA expression [8].
However, the route of estrogen replacement differed from that in this study. In a study by Gebhart et al., postmenopausal women received oral or transdermal estrogen for at least 6 months. ERβ expression was highest in the premenopausal group and lowest in the postmenopausal group with estrogen replacement therapy [8]. In the present study, there were no significant differences in ERβ expression between postmenopausal groups with and without estrogen replacement therapy.
In our previous study, we compared the changes in the extracellular matrix of anterior vaginal wall in women with and without prolapse [9]. Sixty five percent of women with prolapse were menopausal.
In women with anterior vaginal prolapse, there were significantly fewer capillaries surrounding arterioles than in the control group. In the present study, after vaginal estrogen replacement, the anterior vaginal wall of post-menopausal women with SUI did not show increased vascularization as assessed by immunohistochemical staining for CD34 endothelial cell marker.
This study has three main limitations. First, ER immunohistochemical staining is a semiquantitative assessment. Second, we did not examine the expressions of ERβ and CD34 in postmenopausal patients without SUI or compare the differences between postmenopausal patients with SUI. Third, the duration might have been too short and the dose of vaginal estrogen cream supplement might have been too low to cause changes in steroid receptor expression in the vaginal wall. In a study by Long et al. [9], topical estrogen was administered once daily for 3 months with significant increase in the number of vaginal vessels as assessed by introital Doppler velocimetry.
In conclusion, ERβ and CD34 expressions did
not increase after vaginal estrogen replacement in postmenopausal women with SUI. However, the etiology of SUI is complex and multi-factorial.
Further studies are warranted, especially those that include quantitative assessment.
Acknowledgment
Funding source: Chung Shan Medical University Hospital, Taichung, Taiwan (CSH-2016-A-001).
Reference
1. Cody JD, Jacobs ML, Richardson K, Moehrer B, Hextall A Oestrogen therapy for urinary incontinence in post-menopausal women. Cochrane Database Syst Rev. 2012;10:CD001405.
2. Paterni I, Granchi C, Katzenellenbogen JA, Minutolo F. Estrogen receptors alpha (ERα) and beta (ERβ):
subtype-selective ligands and clinical potential.
Steroids. 2014;90:13-29.
3. Lang JH, Zhu L, Sun ZJ, Chen J. Estrogen levels and estrogen receptors in patients with stress urinary incontinence and pelvic organ prolapse. Int J Gynaecol Obstet. 2003 ;80:35-9
4. Lara LA, Ribeiro da Silva A, Rosa-e-Silva JC, Silva-de-Sá MF, Rosa-e-Silva AC Estrogen receptor expression and vessel density in the vagina wall in postmenopausal women with prolapse. Tissue Cell.
2014 ;46:159-64
5. Younes M, Honma N. Estrogen Receptorβ. Arch Pathol Lab Med 2011;135:63-66
6. Chen GD, Oliver RH, Leung BS, Lin LY, Yeh J.
Estrogen receptor alpha and beta expression in the vaginal walls and uterosacral ligaments of premenopausal and postmenopausal women. Fertil Steril. 1999;71:1099-1102.
7. Fuermetz A, Schoenfeld M, Ennemoser S, Muetzel E, Jeschke U, Jundt K. Change of steroid receptor expression in the posterior vaginal wall after local estrogen therapy. Eur J Obstet Gynecol Reprod Biol. 2015; 187:45-50
8. Gebhart JB, Rickard DJ, Barrett TJ, Lesnick TG, Webb MJ, Podratz KC, Spelsberg TC. Expression of estrogen receptor isoforms alpha and beta messenger RNA in vaginal tissue of premenopausal and
postmenopausal women. Am J Obstet Gynecol.
2001 Dec;185(6):1325-1330.
9. Lin SY1, Tee YT, Ng SC, Chang H, Lin PP, Chen GD.
Changes in the extracellular matrix in the anterior vagina of women with or without prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(1):43-8
10. Long CY, Liu CM, Hsu SC, Wu CH, Wang CL, Tsai EM. A randomized comparative study of the effects of oral and topical estrogen therapy on the vaginal vascularization and sexual function in hysterectomized postmenopausal women.
Menopause. 2006;13:737-43