Diabetes Mellitus and Cerebrovascular Disease as Independent Determinants for
Increased Hospital Costs and Length of Stay in Open Appendectomy in Comparison
with Laparoscopic Appendectomy: A Nationwide Cohort Study
--ManuscriptDraft--Manuscript Number:
Full Title: Diabetes Mellitus and Cerebrovascular Disease as Independent Determinants for Increased Hospital Costs and Length of Stay in Open Appendectomy in Comparison with Laparoscopic Appendectomy: A Nationwide Cohort Study
Article Type: Regular Manuscript
Keywords: laparoscopic appendectomy; cost; length of stay Corresponding Author: Tsai-Chung Li, Ph.D.
China Medical University Taichung, Taiwan TAIWAN Corresponding Author Secondary
Information:
Corresponding Author's Institution: China Medical University Corresponding Author's Secondary
Institution:
First Author: Chun-Chieh Yeh, M.D. First Author Secondary Information:
All Authors: Chun-Chieh Yeh, M.D. Chi-Hsun Hsieh, M.D. Chien-Chang Liao, Ph.D. Li-Ting Su, M.S.
Yu-Chun Wang, M.D. Tsai-Chung Li, Ph.D. All Authors Secondary Information:
Abstract: Background: Comorbidity has been proven to increase hospital costs and length of hospital stays in patients receiving appendectomy for the treatment of acute
appendicitis. But, the specific comorbidities that independently influence discrepancy of hospital costs and length of stay between open appendectomy and laparoscopic appendectomy still need to be elucidated.
Method: Using multivariate linear analysis, administrative claims data was obtained from Taiwan's National Health Institute Research Database to compare difference of hospitalization costs and length of stay between open appendectomy and laparoscopic appendectomy, categorized by various comorbidities defined in Charlson comorbidity score.
RESULTS: Of 103,653 patients, 81,479 open appendectomy and 22,174 laparoscopic appendectomy were performed for the treatment of acute appendicitis in Taiwan between 2004 and 2008. In multi-linear regression models, the adjusted costs and length of stay for open appendectomy in patients with cerebrovascular diseases or diabetes mellitus were significantly higher than that for laparoscopic appendectomy.
CONCLUSION: To reduce costs and length of stay, patients with cerebrovascular diseases or diabetes mellitus should be particularly recommended to receive laparoscopic approach rather than open approach for the treatment of acute appendicitis.
[First Authors Last Name] Page 1
1
Diabetes Mellitus and Cerebrovascular Disease as Independent Determinants for Increased Hospital Costs and Length of Stay in Open Appendectomy in
Comparison with Laparoscopic Appendectomy: A Nationwide Cohort Study
Introduction
Acute appendicitis is a common surgical disease, with an incidence of 10 per 10,000 persons per year.1 Open appendectomy had been a standard treatment for acute appendicitis for more than a century. In the early 1980’s, laparoscopic appendectomy was introduced as an alternative procedure for the treatment of appendicitis.2 The safety of laparoscopic appendectomy in patients with acute appendicitis has been proven already.3,4 However, the benefits of laparoscopic appendectomy in cost-savings in comparison to open appendectomy are still inconclusive, particularly in patients with comorbidities.3,5,6
Improvement in health care brings longer life expectancy, which subsequently leads to an increased number of elderly patients with acute appendicitis.7 The elderly patients not only have less physiological reserve but also more comorbidities, which could cause higher morbidity and mortality rates while treating their acute appendicitis.8,9 Comorbidity has been proven as an independent determinant of costs and length of stay in surgical patients.10 However, limited studies investigated which comorbidities are independent determinants to influence costs and length of stay in open appendectomy and laparoscopic appendectomy patients.
The Charlson comorbidity score, adapted by Deyo, R.A., is a well-accepted age-comorbidity combined risk score and is a useful index to predict postoperative complication rates, mortality, length of stay, and hospital charges in elective surgery.11,12 To determine which comorbidities as independent determinants on costs
2
and length of stay of laparoscopic appendectomy and open appendectomy, we conducted a nation-wide cohort study to compare differences of costs and length of stay between laparoscopic appendectomy and open appendectomy stratified according to the comorbidities defined by Charlson scores.
Patients and methods
Data source
This study was a nation-wide, population-based analysis of insurance claims data from the 23 million insured people of Taiwan’s National Health Insurance program, which is almost the entire Taiwanese population. We acquired all claims data obtained from the National Health Institute Research Database (NHIRD). The National Health Insurance program in Taiwan is a universal insurance system organized by the Bureau of National Health Insurance in the Department of Health. The insurance program was carried out in March 1995, and by 1996 it included more than 96% of the population.13 The patient information that was recorded included all medical services received in 1996-2008, personal characteristics of patients and characteristics of hospitals. The patient identification numbers linked to their identities were scrambled to ensure patient confidentiality. For this study, we utilized information including date of birth, sex, main diagnosis and procedure at admissions, hospital charges, length of stay, coexisting illness, urbanization of admitting hospitals, admission hospital level and patients’ discharge status.
Participants
Because laparoscopic appendectomy became popular in Taiwan after 2004, the data base between 2004 and 2008 were used in this study. All diagnosis and
3
Ninth Edition, Clinical Modification (ICD-9-CM). Patients who were diagnosed with acute appendicitis and received appendectomies were identified through patient claims data of NHIRD, using ICD-9-CM codes. Inclusion criteria included ICD-9-CM diagnosis codes 540.0, 540.1, 540.9, 541, and 542 combined with ICD-9-CM
procedure codes 47.01, and 47.09. Exclusion criteria were those appendiceal diseases other than appendicitis (ICD-9-CM 543.9 and 127.4) and those patients who received incidental appendectomy (ICD-9-CM 47.1, 47.11 and 47.19). In addition, we also excluded outlier patients with extremely high hospital costs (the top 1% of patients with highest hospital costs).
Outcome of measurement
Length of stay
The duration between admission and discharge dates were calculated as length of stay (measured in days). Length of stay was recorded as “1” if patients were discharged on the same day of admission.
Hospital costs
The hospital costs were calculated by summing fees for all medical supplies and expanses in the hospital. Costs expressed in this study were in US dollars ($1 U.S. was approximately $31.52 in Taiwanese currency in 2008).
Covariates
The covariates included age, gender, severity of appendicitis (complicated vs. uncomplicated appendicitis), and comorbidities as well as hospital level (medical center vs. regional hospital vs. district hospital), and urbanization of hospital (low vs.
4
moderate vs. high). Complicated appendicitis was defined as appendicitis with perforation, abscess formation or peritonitis (ICD-9-CM 540.0, and 540.1). On the other hand, patients ICD-9-CM codes of 540.9, 541 and 542 were defined as uncomplicated appendicitis. In order to evaluate the concerted influence of age and comorbidities, we used the Charlson comorbidity score as a substitute for age and comorbidities. The comorbidities we considered were total coexisting illnesses defined by Charlson comorbidity scores and ICD-9-CM codes were used to identify those comorbidities defined in Charlson scoring system.11,12 There were 319 city districts and townships in Taiwan and the population density were defined by dividing population with residence area (person/Km2). The 1st quartile and the 4th quartile of population density were categorized as areas of low and high urbanization respectively while the 2nd and the 3rd quartiles of population density were considered as moderate urbanization. The urbanization of hospitals was defined in corresponding to the urbanization level of their locations.
Data analysis
First, to compare characteristics of patients receiving either open appendectomy or laparoscopic appendectomy, the distributions of the sociodemographic status, severity of appendicitis, Charlson comorbidity score and comorbidities defined in Charlson scoring system were demonstrated. Second, after adjusting for gender, hospital level, urbanization of hospital and severity of appendicitis, we compared the adjusted hospital costs and length of stay between open appendectomy and laparoscopic appendectomy and tested the linear trends of the discrepancy among subpopulations of patients with different Charlson comorbidity scores. Subsequently, we used univariate analysis to verify specific comorbidities defined in Charlson score
5
that had significant impact on costs and length of stay for laparoscopic appendectomy and open appendectomy. We also compared the difference of adjusted costs and length of stay between laparoscopic appendectomy and open appendectomy by each comorbidity. Multiple linear regression models were used to evaluate the difference of adjusted costs and length of stay between open appendectomy and laparoscopic appendectomy in patients with various comorbidities. Because comorbidity defined in the Charlson comorbidity score often coexists in the same patient, after adjusting for gender, severity of appendicitis, hospital level and urbanization of hospital, Charlson comorbidity scores were also used as a covariate for adjustment in each regression model. All analyses used SAS software version 9.1 (by SAS Institute Inc. Carey, North Carolina, and U.S.A.). The statistically significant level was set at 0.05 by a two-tailed test.
Results
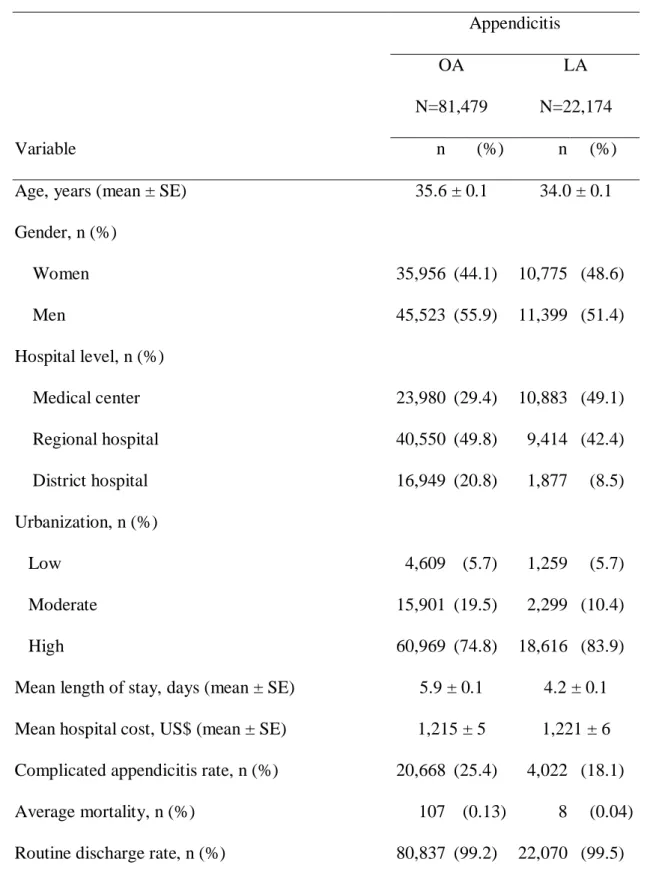
Basal demographic results (Table1)
Difference of adjusted hospital costs and length of stay between laparoscopic
appendectomy and open appendectomy at each Charlson comorbidity score in
population with appendicitis (Fig.1a, b)
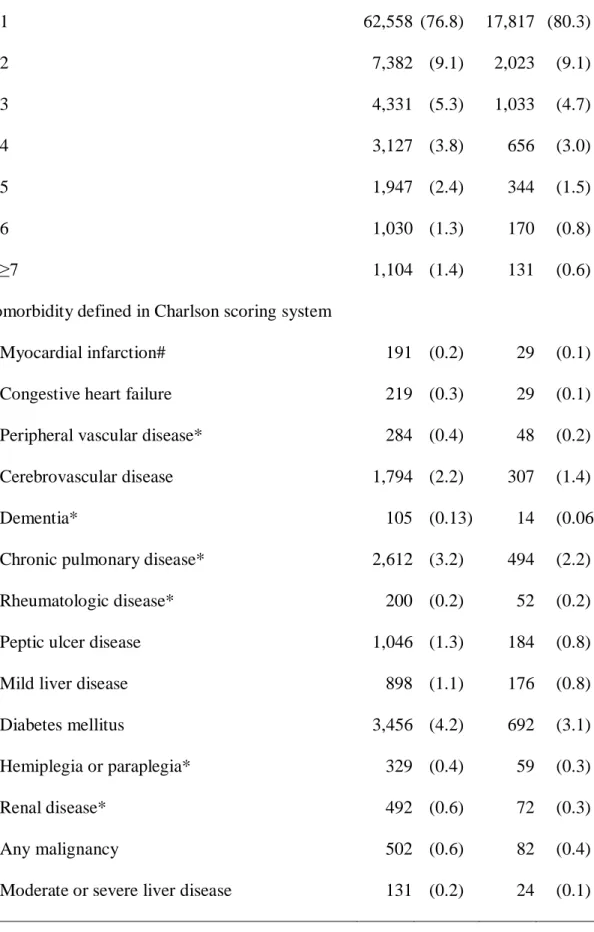
Univariate analysis for hospital costs and length of stay of laparoscopic
appendectomy and open appendectomy at various comorbidities (Table 2)
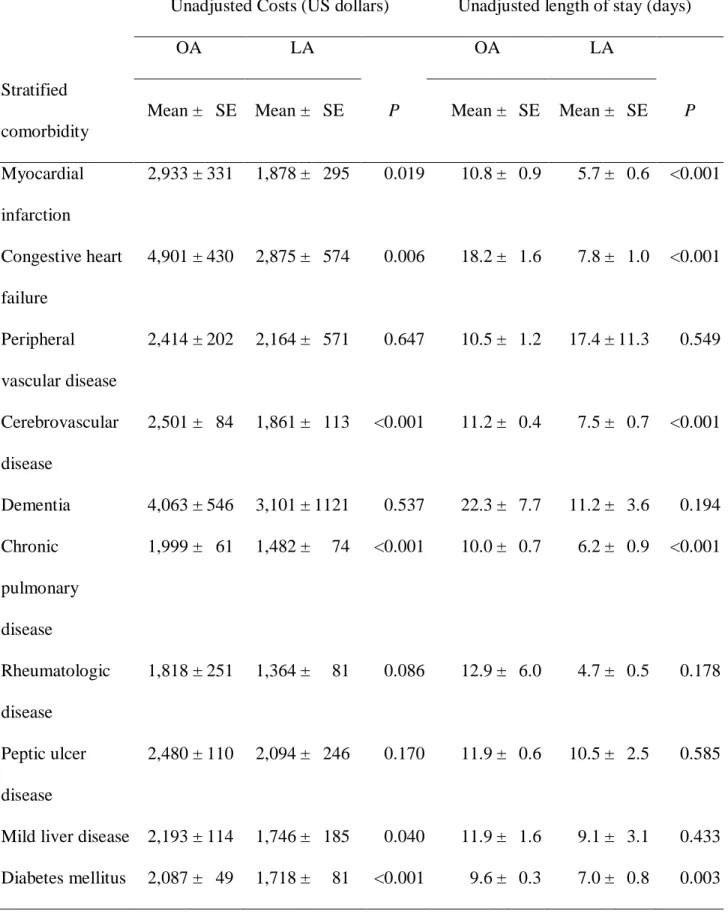
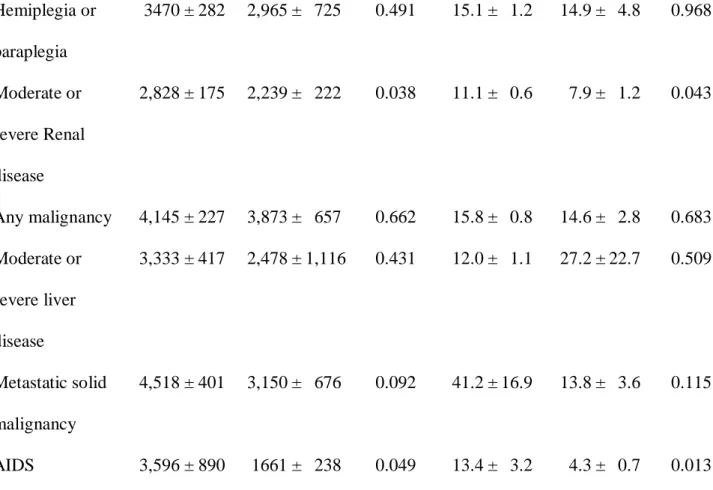
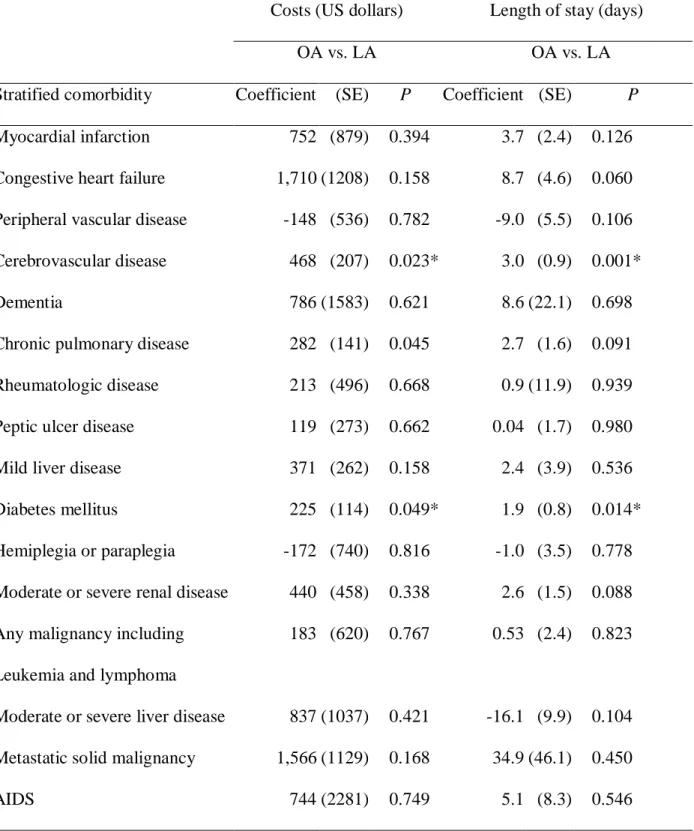
Multiple linear regression analysis for hospital costs and length of stay of
laparoscopic appendectomy and open appendectomy at various comorbidities
6
Between 2004-2008, 103,653 patients underwent appendectomy and 45% of them were women. Among these patients, 81,479 of them received open
appendectomy and 22,174 by laparoscopic appendectomy (Table 1). In comparison with open appendectomy patients, more laparoscopic appendectomy patients lived in highly urbanized areas (83.9% vs. 74.8%, p<0.001) and was treated in medical centers (49.1% vs. 29.4%, p<0.001). The mean length of stay was higher in open
appendectomy patients than laparoscopic appendectomy patients (5.90.1 vs. 4.20.1 days, p<0.001). However, average hospital costs were slightly higher in laparoscopic appendectomy patients than in open appendectomy patients (12216 vs. 1215 5 US dollars, p<0.001).
The differences of adjusted hospital costs between open appendectomy and laparoscopic appendectomy also increased in patients with higher Charlson comorbidity scores (p for linear trend=0.003) (Fig.1a). In addition, there was a significant interaction between types of operation and Charlson comorbidity score (p for interaction <0.001). Adjusted costs of open appendectomy were significantly less than laparoscopic appendectomy in populations with Charlson comorbidity scores of 1. In patients with Charlson comorbidity scores of 2 to 4, the adjusted costs for open appendectomy and laparoscopic appendectomy was similar. Furthermore, in patients with Charlson comorbidity scores of 5 and beyond, adjusted costs of open
appendectomy became significantly higher than laparoscopic appendectomy. Nonetheless, adjusted length of stay of open appendectomy was universally longer than laparoscopic appendectomy in each group of patients with different Charlson comorbidity scores. The discrepancy of adjusted length of stay between open appendectomy and laparoscopic appendectomy became larger as Charlson comorbidity scores increased (p for linear trend < 0.05); while there is also an
7
interaction between operative types and Charlson comorbidity scores on adjusted length of stay (p for interaction <0.05) (Fig. 1b).
An univariate analysis (table 2) revealed that myocardial infarction, congestive heart failure, cerebrovascular disease, chronic pulmonary disease, mild liver disease, diabetes mellitus, moderate or severe renal disease and acquired immune deficiency syndrome (AIDS) were determinants for differences of unadjusted costs between Open appendectomy and laparoscopic appendectomy. In patients who had any one of these comorbidities, unadjusted costs for open appendectomy were significantly higher than laparoscopic appendectomy. Similarly, these comorbidities -- except mild liver disease -- were also determinants of differences of unadjusted length of stay between open appendectomy and laparoscopic appendectomy. The unadjusted length of stay of open appendectomy was significantly longer than that of laparoscopic appendectomy if patients had certain comorbidities.
After adjusting for gender, severity of appendicitis, Charlson comorbidity score, hospital level and urbanization of hospital, the results of multiple linear regression models (table 3) demonstrated that cerebrovascular disease, chronic pulmonary disease, and diabetes mellitus were independent determinants for difference of adjusted costs between open appendectomy and laparoscopic appendectomy. Likewise, cerebrovascular disease and diabetes mellitus were independent
determinants for differences of adjusted length of stay between open appendectomy and laparoscopic appendectomy.
Discussion
With a longer life expectancy in modern times, comorbid conditions become important determinants of clinical and economic outcomes in health care systems.10
8
By using a nation-wide dataset, our results indicated that patients with diabetes mellitus and cerebrovascular disease benefited from laparoscopic appendectomy rather than open appendectomy in the treatment of acute appendicitis in terms of reduced hospital costs and length of stay.
Comorbidities, such as cerebrovascular disease, chronic pulmonary disease and diabetes mellitus, have been reported as determinants of increased postoperative complications and length of stay in laparoscopic surgeries.10,14-16 Following statistical adjustment for the severity of appendicitis and Charlson comorbidity scores between groups, we found that cerebrovascular disease and diabetes mellitus were independent determinants for the increased costs and length of stay following open appendectomy than that of laparoscopic appendectomy. These results were consistent with previous studies reported by Cho10, Cheng14, Kim15 and Ming16, et al. In addition, the reason to use Charlson comorbidity score instead of specifying comorbidities for regression analysis was to avoid too many parameters in regression models that may lead to wrong statistic calculation. Furthermore, we found that some comorbidities such as myocardial infarction, congestive heart failure, moderate to severe renal disease and AIDS were modifiers in univariate analysis but not in multivariate analysis. A possible explanation was that the prevalence of these comorbidities was too low to achieve adequate statistic power. Thus, if we could collect more cases with these specific comorbidities, we may be able to draw more positive conclusions regarding these comorbidities as significant modifiers for discrepancy of costs and length of stay between open appendectomy and laparoscopic appendectomy.
There were limitations in our study. First, inaccurate coding is possible in such a large, population-based database. However, inaccurate coding theoretically appeared with similar frequency in both open appendectomy and laparoscopic appendectomy
9
groups; therefore, the discrepancy of costs and length of stay between laparoscopic appendectomy and open appendectomy can be minimized but cannot be biased. In addition, data on postoperative complications and recovery time were not collected in this database and could not be analyzed. With the limitations of this database, we focused our study on the analysis of costs and length of stay following open appendectomy or laparoscopic appendectomy without answering other clinically relevant questions such as whether laparoscopic appendectomy rather than open appendectomy were associated with lower incidence of postoperative complications, and reduced postoperative recovery time as well as time of returning to work.
In conclusion, this is a nation-wide cohort study to evaluate which comorbidities could influence economic outcomes between open appendectomy and laparoscopic appendectomy for acute appendicitis. In terms of reducing hospital costs and length of stay, patients with diabetes mellitus and cerebrovascular disease should be recommended to receive laparoscopic appendectomy as the treatment of choice for acute appendicitis.
Acknowledgements
This study was supported partly by the Executive Yuan National Science Council in Taiwan, Republic of China (grant number NSC 97-2625-M-039-003), the China Medical University Hospital (grant number 1MS1), and the Taiwan Department of Health Clinical Trials and Research Centre for Excellence (grant number
OH100-TD-B-111-004) and Cancer Research Centre of Excellence (grant number DOH100-TD-C-111-005).
10
References
1. Ohmann C, Franke C, Kraemer M, Yang Q. Status report on epidemiology of acute appendicitis. Chirurg 2002; 73: 769-76.
2. Semm K. Endoscopic appendectomy. Endoscopy 1983; 15: 59-64.
3. Harrell AG, Lincourt AE, Novitsky YW, et al. Advantages of laparoscopic appendectomy in the elderly. Am Surg 2006; 72: 474-80.
4. Kirshtein B, Perry ZH, Mizrahi S, Lantsberg L. Value of laparoscopic appendectomy in the elderly patient. World J Surg 2009; 33: 918-22.
5. Nakhamiyayev V, Galldin L, Chiarello M, et al. Laparoscopic appendectomy is the preferred approach for appendicitis: a retrospective review of two practice patterns. Surg Endosc 2010; 24: 859-64
6. Wei HB, Huang JL, Zheng ZH, et al. Laparoscopic versus open appendectomy: a prospective randomized comparison. Surg Endosc 2010; 24: 266-9.
7. Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 1990; 132: 910-25.
8. Lau WY, Fan ST, Yiu TF, et al. Acute appendicitis in the elderly. Surg Gynecol Obstet 1985; 161:157-60.
9. Podnos YD, Jimenez JC, Wilson SE. Intra-abdominal Sepsis in Elderly Persons. Clin Infect Dis 2002; 35: 62-8.
10. Cho JY, Han HS, Yoon YS, Ahn KS. Risk factors for acute cholecystitis and a complicated clinical course in patients with symptomatic cholelithiasis. Arch Surg 2010; 145: 329-33.
11. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992; 45: 613-9.
11
12. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373-83.
13. Chiang TL. Taiwan's 1995 health care reform. Health Policy 1997; 39: 225-39. 14. Cheng SP, Chang YC, Liu CL, et al. Factors associated with prolonged stay after laparoscopic cholecystectomy in elderly patients. Surg Endosc 2008; 22: 1283-9. 15. Kim W, Song KY, Lee HJ, et al. The impact of comorbidity on surgical outcomes in laparoscopy-assisted distal gastrectomy: a retrospective analysis of multicenter results. Ann Surg 2008; 248: 793-9.
16. Ming PC, Yan TY, Tat LH. Risk factors of postoperative infections in adults with complicated appendicitis. Surg Laparosc Endosc Percutan Tech 2009; 19: 244-8.
12
Figure Legends
Fig 1a. Comparison of costs between OA and LA for acute appendicitis. Adjusting for gender, hospital level, urbanization of hospital and severity of acute appendicitis. P for linear trend<0.01. P for interaction <0.001;*: OA vs. LA, p<0.05. Significance established at multiple linear regression models.
Fig 1b. Comparison of LOS between OA and LA for acute appendicitis. Adjusting for gender, hospital level, urbanization of hospital and severity of acute appendicitis. P for linear trend<0.05; P for interaction <0.05; *: OA vs. LA, p<0.05. Significance established at multiple linear regression models.
[First Authors Last Name] Page 1
1
Diabetes Mellitus and Cerebrovascular Disease as Independent Determinants for
Increased Hospital Costs and Length of Stay in Open Appendectomy in
Comparison with Laparoscopic Appendectomy: A Nationwide Cohort Study
1-3
Chun-Chieh Yeh, M.D. , 2Chi-Hsun Hsieh, M.D.,4,5Chien-Chang Liao, Ph.D., 2,4
Li-Ting Su, M.S., 2 Yu-Chun Wang, M.D.,6-10 Tsai-Chung Li, PhD, Professor
1
Graduate institute of Clinical Medical Science, China Medical University, Taichung
404, Taiwan
2
Trauma and Emergency Center, China Medical University Hospital, China Medical
University, Taichung 404, Taiwan
3
Department of Surgery, China Medical University Hospital, Taichung 404, Taiwan
4
Management Office for Health Data, China Medical University Hospital, Taichung
404, Taiwan
5
Department of Anesthesiology, Taipei Medical University Hospital, Taipei 110,
2
6
Graduate Institute of Biostatistics, College of Public Health, China Medical
University, Taichung 404, Taiwan
7
Graduate Institute of Chinese Medicine Science, College of Chinese Medicine,
China Medical University, Taichung 404, Taiwan
8
Biostatistics Center, China Medical University, Taichung 404, Taiwan
9
Department of Medical Research, China Medical University Hospital, Taichung 404,
Taiwan
10
Institute of Health Care Administration, College of Health Science, Asia University,
Taichung 404, Taiwan
Authors:
Chun-Chieh Yeh, MD: b8202034@gmail.com
Chi-Hsun Hsieh, MD: chihsun@mail.cmuh.org.tw
Chien-Chang Liao, Ph.D.: jacky48863027@yahoo.com.tw
Li-Ting Su, M.S.: sweety@mail.cmu.edu.tw
Yu-Chun Wang, M.D.: traumawang@yahoo.com.tw
3
All authors worked together and contributed the manuscript in 1) substantial
contributions to conception and design, or acquisition of data, or analysis and
interpretation of data; 2) drafting the article or revising it critically for important
intellectual content; and 3) final approval of the version to be published.
Reprints and correspondence to:
Tsai-Chung Li, PhD, Professor
China Medical University Graduate Institute of Biostatistics
91 Hsueh-Shih Road 15F, Taichung 404, Taiwan
Telephone number: 886-4-2205-3366 ext. 6605, Fax number: 886-4-2207-8539
E-mail address: tcli@mail.cmu.edu.tw
Word count: 180 in abstract, 2048 in text, 3 tables, 2 figures and 16 references
All the authors do not have any conflict of interest.
[First Authors Last Name] Page 1
[Insert Running title of <72 characters]
Tsai-Chung Li, PhD, Professor China Medical University
graduate Institute of Biostatistics 91 Hsueh-Shih Road 15F,
Taichung 404, Taiwan
Aug. 16, 2011 Editors in Chief
Re: “Diabetes Mellitus and Cerebrovascular Disease as Independent Determinants for Increased Hospital Costs and Length of Stay in Open Appendectomy in Comparison with Laparoscopic Appendectomy: A Nationwide Cohort Study
”.
Dear editor:
This paper is an original report and particularly designed to investigate economic influence of different operative strategies to treat acute appendicitis in populations with specific comorbidity.
A clinical and economical influence of laparoscopic appendectomy for appendicitis is still inconclusive, particularly for specific subpopulations with coexisting illness. However, with an increasing aged population in modern society, comorbidity became important issues in determining clinical and economic outcomes in surgical disease, such as acute appendicitis.
In order to determine the influence of specific comorbidity on costs and length of stay at laparoscopic appendectomy and open appendectomy, we conducted a nation-wide, population-based study to compare differences of costs and length of stay between laparoscopic appendectomy and open appendectomy in patients with different comorbidities defined in Charlson scores. In multi-linear regression models, the adjusted costs and length of stay for open appendectomy in patients with cerebrovascular diseases and diabetes mellitus were significantly higher than that for laparoscopic appendectomy.
In summary, to reduce hospital costs and length of stay, laparoscopic appendectomy is the procedure of choice for patients with cerebrovascular disease and diabetes mellitus.
The manuscript and material within the manuscript have not been published and are not being considered for publication elsewhere in whole or in part in any language, websites or
e-[Insert Running title of <72 characters]
print servers. Part of the data has been presented at conference. The manuscript is being submitted only to The American Surgeon and it will not be submitted elsewhere while under consideration. All authors certify that any work in preparation, submitted, in press, or published that is potentially overlapping either in the actual data presented or in the conceptual approach is enclosed along with the original submission. Any material within the manuscript that has appeared elsewhere is cross-referenced. All authors have participated in the concept development and design; analysis and interpretation of data; drafting or revising of the manuscript, and have approved the manuscript as submitted.
No conflict in financial interest is involved in this study. Thank you for your review and consideration of publication for this paper.
Sincerely,
Tsai-Chung Li, PhD, Professor
China Medical University Graduate Institute of Biostatistics 91 Hsueh-Shih Road 15F, Taichung 404, Taiwan
Telephone number: 886-4-2205-3366 ext. 6605 Fax number: 886-4-2207-8539
[First Authors Last Name] Page 1
Table 1. Socio-demographic characteristics of patients with appendicitis and receiving appendectomy between 2004-2008 Variable Appendicitis OA N=81,479 LA N=22,174 n (%) n (%)
Age, years (mean ± SE) 35.6 ± 0.1 34.0 ± 0.1
Gender, n (%) Women 35,956 (44.1) 10,775 (48.6) Men 45,523 (55.9) 11,399 (51.4) Hospital level, n (%) Medical center 23,980 (29.4) 10,883 (49.1) Regional hospital 40,550 (49.8) 9,414 (42.4) District hospital 16,949 (20.8) 1,877 (8.5) Urbanization, n (%) Low 4,609 (5.7) 1,259 (5.7) Moderate 15,901 (19.5) 2,299 (10.4) High 60,969 (74.8) 18,616 (83.9)
Mean length of stay, days (mean ± SE) 5.9 ± 0.1 4.2 ± 0.1 Mean hospital cost, US$ (mean ± SE) 1,215 ± 5 1,221 ± 6 Complicated appendicitis rate, n (%) 20,668 (25.4) 4,022 (18.1)
Average mortality, n (%) 107 (0.13) 8 (0.04)
Table 1. Socio-demographic characteristics of patients with appendicitis and receiving appendectomy between 2004-2008 (cont.)
Charlson comorbidity score
1 62,558 (76.8) 17,817 (80.3) 2 7,382 (9.1) 2,023 (9.1) 3 4,331 (5.3) 1,033 (4.7) 4 3,127 (3.8) 656 (3.0) 5 1,947 (2.4) 344 (1.5) 6 1,030 (1.3) 170 (0.8) ≥7 1,104 (1.4) 131 (0.6)
Comorbidity defined in Charlson scoring system
Myocardial infarction# 191 (0.2) 29 (0.1)
Congestive heart failure 219 (0.3) 29 (0.1)
Peripheral vascular disease* 284 (0.4) 48 (0.2)
Cerebrovascular disease 1,794 (2.2) 307 (1.4)
Dementia* 105 (0.13) 14 (0.06)
Chronic pulmonary disease* 2,612 (3.2) 494 (2.2)
Rheumatologic disease* 200 (0.2) 52 (0.2)
Peptic ulcer disease 1,046 (1.3) 184 (0.8)
Mild liver disease 898 (1.1) 176 (0.8)
Diabetes mellitus 3,456 (4.2) 692 (3.1)
Hemiplegia or paraplegia* 329 (0.4) 59 (0.3)
Renal disease* 492 (0.6) 72 (0.3)
Any malignancy 502 (0.6) 82 (0.4)
Table 1. Socio-demographic characteristics of patients with appendicitis and receiving appendectomy between 2004-2008 (cont.)
Metastatic solid tumor 128 (0.2) 18 (0.1)
AIDS 19 (0.02) 3 (0.01)
OA: Open appendectomy; LA: Laparoscopic appendectomy; AIDS: acquired immunodeficiency syndrome
# Myocardial infarction included both acute and old myocardial infarction. Acute myocardial infarction (ICD-9-CM 410-410.9) was only included if recorded prior to the index admission. In contrast, old myocardial infarction (ICD-9-CM 412) was included if listed during the index or prior admission.
[First Authors Last Name] Page 1
Table 2. Unadjusted costs and length of stay for either OA or LA, stratified by specific comorbidity defined by Charlson scores
Unadjusted Costs (US dollars) Unadjusted length of stay (days)
OA LA OA LA
Stratified comorbidity
Mean ± SE Mean ± SE P Mean ± SE Mean ± SE P
Myocardial infarction 2,933 ± 331 1,878 ± 295 0.019 10.8 ± 0.9 5.7 ± 0.6 <0.001 Congestive heart failure 4,901 ± 430 2,875 ± 574 0.006 18.2 ± 1.6 7.8 ± 1.0 <0.001 Peripheral vascular disease 2,414 ± 202 2,164 ± 571 0.647 10.5 ± 1.2 17.4 ± 11.3 0.549 Cerebrovascular disease 2,501 ± 84 1,861 ± 113 <0.001 11.2 ± 0.4 7.5 ± 0.7 <0.001 Dementia 4,063 ± 546 3,101 ± 1121 0.537 22.3 ± 7.7 11.2 ± 3.6 0.194 Chronic pulmonary disease 1,999 ± 61 1,482 ± 74 <0.001 10.0 ± 0.7 6.2 ± 0.9 <0.001 Rheumatologic disease 1,818 ± 251 1,364 ± 81 0.086 12.9 ± 6.0 4.7 ± 0.5 0.178 Peptic ulcer disease 2,480 ± 110 2,094 ± 246 0.170 11.9 ± 0.6 10.5 ± 2.5 0.585
Mild liver disease 2,193 ± 114 1,746 ± 185 0.040 11.9 ± 1.6 9.1 ± 3.1 0.433 Diabetes mellitus 2,087 ± 49 1,718 ± 81 <0.001 9.6 ± 0.3 7.0 ± 0.8 0.003
Table 2. Unadjusted costs and length of stay for either OA or LA, stratified by specific comorbidity defined by Charlson scores (cont.)
Hemiplegia or paraplegia 3470 ± 282 2,965 ± 725 0.491 15.1 ± 1.2 14.9 ± 4.8 0.968 Moderate or severe Renal disease 2,828 ± 175 2,239 ± 222 0.038 11.1 ± 0.6 7.9 ± 1.2 0.043 Any malignancy 4,145 ± 227 3,873 ± 657 0.662 15.8 ± 0.8 14.6 ± 2.8 0.683 Moderate or severe liver disease 3,333 ± 417 2,478 ± 1,116 0.431 12.0 ± 1.1 27.2 ± 22.7 0.509 Metastatic solid malignancy 4,518 ± 401 3,150 ± 676 0.092 41.2 ± 16.9 13.8 ± 3.6 0.115 AIDS 3,596 ± 890 1661 ± 238 0.049 13.4 ± 3.2 4.3 ± 0.7 0.013 OA: Open appendectomy; LA: Laparoscopic appendectomy; AIDS: acquired immunodeficiency syndrome; SE: standard error; Two sample Student t test was used to compare costs and LOS between OA and LA in patients with specific comorbidity.
[First Authors Last Name] Page 1
Table 3. Discrepancy of adjusted costs and length of stay between OA or LA, stratified by specific comorbidity defined by Charlson scores
Costs (US dollars) Length of stay (days)
OA vs. LA OA vs. LA
Stratified comorbidity Coefficient (SE) P Coefficient (SE) P
Myocardial infarction 752 (879) 0.394 3.7 (2.4) 0.126 Congestive heart failure 1,710 (1208) 0.158 8.7 (4.6) 0.060 Peripheral vascular disease -148 (536) 0.782 -9.0 (5.5) 0.106 Cerebrovascular disease 468 (207) 0.023* 3.0 (0.9) 0.001*
Dementia 786 (1583) 0.621 8.6 (22.1) 0.698
Chronic pulmonary disease 282 (141) 0.045 2.7 (1.6) 0.091 Rheumatologic disease 213 (496) 0.668 0.9 (11.9) 0.939 Peptic ulcer disease 119 (273) 0.662 0.04 (1.7) 0.980 Mild liver disease 371 (262) 0.158 2.4 (3.9) 0.536 Diabetes mellitus 225 (114) 0.049* 1.9 (0.8) 0.014* Hemiplegia or paraplegia -172 (740) 0.816 -1.0 (3.5) 0.778 Moderate or severe renal disease 440 (458) 0.338 2.6 (1.5) 0.088 Any malignancy including
Leukemia and lymphoma
183 (620) 0.767 0.53 (2.4) 0.823
Moderate or severe liver disease 837 (1037) 0.421 -16.1 (9.9) 0.104 Metastatic solid malignancy 1,566 (1129) 0.168 34.9 (46.1) 0.450
AIDS 744 (2281) 0.749 5.1 (8.3) 0.546
OA: Open appendectomy; LA: Laparoscopic appendectomy; AIDS: acquired immunodeficiency syndrome; SE: standard error; Adjusting for gender, hospital level, urbanization of hospital, severity of acute appendicitis and Charlson scores; analyzed by multiple linear regression