科技部補助專題研究計畫報告
Castor 基因在卵巢癌轉移之研究(第3年)
報 告 類 別 : 成果報告 計 畫 類 別 : 個別型計畫
計 畫 編 號 : MOST 106-2314-B-006-060-MY3 執 行 期 間 : 108年08月01日至109年07月31日 執 行 單 位 : 國立成功大學醫學系婦產科
計 畫 主 持 人 : 許耿福 共 同 主 持 人 : 洪澤民
計畫參與人員: 碩士級-專任助理:鍾雯如
碩士班研究生-兼任助理:張文齊
本研究具有政策應用參考價值:■否 □是,建議提供機關
(勾選「是」者,請列舉建議可提供施政參考之業務主管機關)
本研究具影響公共利益之重大發現:□否 □是
中 華 民 國 109 年 10 月 18 日
中 文 摘 要 : 卵巢癌是一種高度惡性、極具組織侵犯性的婦女癌症。卵巢癌高死 亡率的原因在於,大部分病人被診斷時已是癌症晚期,同時也常常 在治療的過程中對化療藥物產生抗藥性。因此,探求卵巢癌腫瘤的 發生機轉並發展有效的治療方式極具必要性。之前我們的研究發現 CASZ1是一個可能導致卵巢癌轉移的重要因子。但是其分子調控機轉 仍然不清楚。
在第一年與第二年的研究中,我們發現漿液性卵巢癌病人高度 表現CASZ1蛋白時會有較差的存活率。顯示CASZ1蛋白在漿液性卵巢 癌的高表現可能與腫瘤的轉移有相關性。但是CASZ1不僅在漿液性卵 巢癌具有高表現,我們也發現其在黏液性卵巢癌中具有高表現相較 於其他類型卵巢癌。所以,我們利用34例黏液性卵巢癌臨床檢體進 行組織化學染色分析,發現CASZ1低表現與較差預後相關。接下來
,我們利用基因微陣列分析,發現黏液性卵巢癌細胞經由
lentivirus感染穩定抑制CASZ1後,MMP1基因可以受到CASZ1的調控
。故推論CASZ1低表現的黏液性卵巢癌具有較差的預後,可能是受到 MMP1基因上調所導致。MMP1是MMPs家族成員中最常表達的分子。
MMP1的過表達與多種惡性腫瘤有關,並發現與早期轉移和不良預後 密切相關。已證明MMP1激活PAR1,這是卵巢癌腹膜轉移小鼠模型中 血管生成和轉移的重要分子。而抑制MMP1-PAR1軸也被證明可能是卵 巢癌侵襲和轉移的治療靶標。此外,MMP1也被報導與乳癌的多重抗 藥性相關。因此,第三年我們著重於黏液性卵巢癌中CASZ1表現與 MMP1調控途徑的探討。
由基因微陣列分析結果發現,RMUGS細胞抑制CASZ1基因表現
,可增加抗藥性基因(ABCC5, ABCF1)、癌幹細胞基因(CD44)與抗細 胞凋亡基因(BCL9)表現。且經由connectivity map (CMap)網路軟體 分析,篩選出Emetine可能為CASZ1基因調控相關的藥物。體外實驗 證實,抑制CASZ1基因表現確實可以增加癌幹細胞與抗細胞凋亡特性
,而Emetine治療可減少因CASZ1低表現而增加的癌幹細胞與抗細胞 凋亡特性。我們證明黏液性卵巢癌細胞中的CASZ1低表現可調控 MMP1訊息路徑,並增加癌幹細胞與抗細胞凋亡特性,使病人癒後較 差。因此,CASZ1可能成為黏液性卵巢癌的癒後標誌,且Emetine可 能是未來黏液性卵巢癌治療的潛力藥物。
中 文 關 鍵 詞 : 卵巢癌,轉移,CASZ1,MMP1,Emetine
英 文 摘 要 : Ovarian cancer is a highly malignant and aggressive gynecological malignancy. Reasons why ovarian cancer is such lethal is that most patients with ovarian cancer are diagnosed at later stages and frequently develop chemo- resistance after therapy. Consequently, it is necessary to understand the underlying mechanism of cancer progression and develop better therapeutic strategies. In previous report, we demonstrated CASZ1 is an important molecule for ovarian cancer metastasis, but the molecular mechanism of CASZ1 in ovarian cancer metastasis is still unclear.
In the first and second years of this project, we found
the CASZ1 high expression in patients with serous type ovarian cancer have poor survival rate. The results suggest that CASZ1 high expression in serous type ovarian cancer may be associated with metastasis. However, CASZ1 high expression is not only in serous type ovarian cancer cells, but also present in mucinous type ovarian cancer cells. So, we used 34 mucinous type ovarian cancer specimens to
execute immunohischemistry stain to validate the CASZ1 expression whether associated with outcome. After statistical analyzed, we found low CASZ1 expression in mucinous type ovarian cancer is associated with poor prognosis. Next, we used the cDNA microarray analysis to screening the candidates of CASZ1 gene knocked down in mucinous type ovarian cancer cells, and found the MMP1 gene is most obvious up regulation. Other words, MMP1 signal activation may be involved in the CASZ1 low expression causing poor prognosis of mucinous type ovarian cancer.
MMP1 is the most commonly expressed molecule of the MMPs family members. Overexpression of MMP1 is related with various type of malignant tumors, and closely related to early metastasis and poor prognosis. MMP1 activate PAR1 has been demonstrated, which is an important molecule for
angiogenesis and metastasis in a mouse model of ovarian cancer peritoneal metastasis. Moreover, MMP1 has been reported associated with multi-drugs resistance in breast cancer. Therefore, we focus on the role of CASZ1 and MMP1 regulation in mucinous type ovarian cancer in the third years of this study.
According to the results of cDNA microarray analysis, the drug resistance genes (ABCC5, ABCF1), cancer stemness gene (CD44) and anti-apoptosis gene (BCL9) up regulation in RMUGS cells that stable knock down CASZ1 gene. And we also noticed Emetine that had screened by the connectivity map (CMap) network software maybe the potential drug to block CASZ1 low expression induced MMP1 signal transduction. We confirmed the mucinous type ovarian cancer cells with CASZ1 knocked down can increase character of cancer stemness and anti-apoptosis, and the Emetine treatment can reverse this phenomena. Here, we prove that the low expression of CASZ1 in mucinous ovarian cancer cells can regulate the MMP1 signaling pathway, and then increase characters of cancer stemness and anti-apoptosis to cause poor prognosis. Thus, CASZ1 may be act a prognostic biomarker of mucinous ovarian cancer, and the Emetine may be the potential therapeutic drug in future.
英 文 關 鍵 詞 : ovarian cancer, metastasis, CASZ1, MMP1, Emetine
1
科技部補助專題研究計畫成果報告
(
□期中進度報告/█期末報告)Castor 基因在卵巢癌轉移之研究
計畫類別: █個別型計畫 □整合型計畫
計畫編號:MOST 106-2314-B-006-060-MY3 執行期間:106 年 08 月 01 日至 109 年 07 月 31 日
執行機構及系所:國立成功大學 醫學系婦產科
計畫主持人:許耿福 共同主持人:洪澤民
計畫參與人員:林長霓、鍾雯如
本計畫除繳交成果報告外,另含下列出國報告,共 0 份:
□執行國際合作與移地研究心得報告
□出席國際學術會議心得報告
□出國參訪及考察心得報告
中 華 民 國 109 年 09 月 30 日
2
中文摘要
卵巢癌是一種高度惡性、極具組織侵犯性的婦女癌症。卵巢癌高死亡率的原因在於,大部分病人 被診斷時已是癌症晚期,同時也常常在治療的過程中對化療藥物產生抗藥性。因此,探求卵巢癌腫瘤 的發生機轉並發展有效的治療方式極具必要性。之前我們的研究發現CASZ1是一個可能導致卵巢癌轉 移的重要因子。但是其分子調控機轉仍然不清楚。
在第一年與第二年的研究中,我們發現漿液性卵巢癌病人高度表現CASZ1蛋白時會有較差的存活 率。顯示CASZ1蛋白在漿液性卵巢癌的高表現可能與腫瘤的轉移有相關性。但是CASZ1不僅在漿液性 卵巢癌具有高表現,我們也發現其在黏液性卵巢癌中具有高表現相較於其他類型卵巢癌。所以,我們 利用34例黏液性卵巢癌臨床檢體進行組織化學染色分析,發現CASZ1低表現與較差預後相關。接下來,
我們利用基因微陣列分析,發現黏液性卵巢癌細胞經由lentivirus感染穩定抑制CASZ1後,MMP1基因可 以受到CASZ1的調控。故推論CASZ1低表現的黏液性卵巢癌具有較差的預後,可能是受到MMP1基因上 調所導致。MMP1是MMPs家族成員中最常表達的分子。MMP1的過表達與多種惡性腫瘤有關,並發現 與早期轉移和不良預後密切相關。已證明MMP1激活PAR1,這是卵巢癌腹膜轉移小鼠模型中血管生成 和轉移的重要分子。而抑制MMP1-PAR1軸也被證明可能是卵巢癌侵襲和轉移的治療靶標。此外,MMP1 也被報導與乳癌的多重抗藥性相關。因此,第三年我們著重於黏液性卵巢癌中CASZ1表現與MMP1調控 途徑的探討。
由基因微陣列分析結果發現,RMUGS細胞抑制CASZ1基因表現,可增加抗藥性基因(ABCC5, ABCF1)、癌幹細胞基因(CD44)與抗細胞凋亡基因(BCL9)表現。且經由connectivity map (CMap)網路軟體 分析,篩選出Emetine可能為CASZ1基因調控相關的藥物。體外實驗證實,抑制CASZ1基因表現確實可 以增加癌幹細胞與抗細胞凋亡特性,而Emetine治療可減少因CASZ1低表現而增加的癌幹細胞與抗細胞 凋亡特性。我們證明黏液性卵巢癌細胞中的CASZ1低表現可調控MMP1訊息路徑,並增加癌幹細胞與 抗細胞凋亡特性,使病人癒後較差。因此,CASZ1可能成為黏液性卵巢癌的癒後標誌,且Emetine可能 是未來黏液性卵巢癌治療的潛力藥物。
關鍵詞: 卵巢癌,轉移,CASZ1,MMP1,Emetine
3
Abstract
Ovarian cancer is a highly malignant and aggressive gynecological malignancy. Reasons why ovarian cancer is such lethal is that most patients with ovarian cancer are diagnosed at later stages and frequently develop chemo-resistance after therapy. Consequently, it is necessary to understand the underlying mechanism of cancer progression and develop better therapeutic strategies. In previous report, we demonstrated CASZ1 is an important molecule for ovarian cancer metastasis, but the molecular mechanism of CASZ1 in ovarian cancer metastasis is still unclear.
In the first and second years of this project, we found the CASZ1 high expression in patients with serous type ovarian cancer have poor survival rate. The results suggest that CASZ1 high expression in serous type ovarian cancer may be associated with metastasis. However, CASZ1 high expression is not only in serous type ovarian cancer cells, but also present in mucinous type ovarian cancer cells. So, we used 34 mucinous type ovarian cancer specimens to execute immunohischemistry stain to validate the CASZ1 expression whether associated with outcome. After statistical analyzed, we found low CASZ1 expression in mucinous type ovarian cancer is associated with poor prognosis. Next, we used the cDNA microarray analysis to screening the candidates of CASZ1 gene knocked down in mucinous type ovarian cancer cells, and found the MMP1 gene is most obvious up regulation. Other words, MMP1 signal activation may be involved in the CASZ1 low expression causing poor prognosis of mucinous type ovarian cancer. MMP1 is the most commonly expressed molecule of the MMPs family members. Overexpression of MMP1 is related with various type of malignant tumors, and closely related to early metastasis and poor prognosis. MMP1 activate PAR1 has been demonstrated, which is an important molecule for angiogenesis and metastasis in a mouse model of ovarian cancer peritoneal metastasis.
Moreover, MMP1 has been reported associated with multi-drugs resistance in breast cancer. Therefore, we focus on the role of CASZ1 and MMP1 regulation in mucinous type ovarian cancer in the third years of this study.
According to the results of cDNA microarray analysis, the drug resistance genes (ABCC5, ABCF1), cancer stemness gene (CD44) and anti-apoptosis gene (BCL9) up regulation in RMUGS cells that stable knock down CASZ1 gene. And we also noticed Emetine that had screened by the connectivity map (CMap) network software maybe the potential drug to block CASZ1 low expression induced MMP1 signal transduction. We confirmed the mucinous type ovarian cancer cells with CASZ1 knocked down can increase character of cancer stemness and anti-apoptosis, and the Emetine treatment can reverse this phenomena. Here, we prove that the low expression of CASZ1 in mucinous ovarian cancer cells can regulate the MMP1 signaling pathway, and then increase characters of cancer stemness and anti-apoptosis to cause poor prognosis. Thus, CASZ1 may be act a prognostic biomarker of mucinous ovarian cancer, and the Emetine may be the potential therapeutic drug in future.
Keywords: ovarian cancer, metastasis, CASZ1, MMP1, Emetine
4
Introduction
Epithelial ovarian cancer (EOC) is the leading cause of cancer-related deaths among women. Despite its relatively low incidence rate, it has the highest fatality in gynecological cancers [1, 2]. This high lethality is attributed to the fact that the early stage of the disease is mostly asymptomatic. Therefore, the disease often remains undiagnosed until the cancer has already disseminated throughout the peritoneal cavity [3]. As mortality in EOC is directly associated with metastatic disease, ovarian cancer metastasis merits further investigation.
Among these, mucinous ovarian cancer is a rare tumor, probably accounting for 3% of all epithelial ovarian cancers, but its biologic features have shown that it is a unique disease [4, 5]. Different with serous type ovarian cancer, mucinous type ovarian cancer is characteristically diagnosed in younger patients, and appear to evolve in stepwise fashion from benign epithelium to a preinvasive lesion to carcinoma [4, 6-8]. In our preliminary results, mucinous type ovarian cancer cell lines (RMUGS and MCAS) and serous type ovarian cancer cell lines (OVCAR3 and OVCAR4) were highly expressed CASZ1 gene as compared with other subtypes (Supplemental Figure 1), imply CASZ1 plays important role in mucinous type ovarian cancer progression.
CASZ1, which localizes to chromosome 1p36.22, is the human homolog of the Drosophila zinc finger transcription factor Castor (dCas) [9]. dCas regulates neuronal differentiation and neural fate [10, 11]. CASZ1 was recognized as a tumor suppressor in neuroblastoma due to its ability to induce cell differentiation and inhibit tumor cell migration and growth in vitro and in vivo [12, 13]. Recent studies have shown that low expression of CASZ1 is associated with poor prognosis in clear cell renal cell carcinoma [14]. Previously, we have identified that CASZ1 may be a novel promoter of metastasis in ovarian cancer [15]. CASZ1 may play an important role in ovarian cancer. In the previous two years, we focused on serous type ovarian cancer patients and its correlation with CASZ1 expression. However, we found out that CASZ1 is highly expressed in mucinous ovarian carcinoma cell lines compared to others. Thus in the third year, we aim to clarify the role of CASZ1 in mucinous ovarian carcinoma progression.
In clinical specimens, we observed CASZ1 low expression in mucinous type ovarian cancer is associated with poor survival. And according to the results of cDNA microarray, we noticed MMP1 gene significantly up regulation in RMUGS cells that knock down CASZ1 gene via lentivirus infection. Other words, MMP1 signal maybe the regulator in mucinous type ovarian cancer with CASZ1 low expression to causing poor outcome.
MMP1 is the most commonly expressed molecule of the MMPs family members. Overexpression of MMP1 is
5
related with various type of malignant tumors, and closely related to early metastasis and poor prognosis [16].
MMP1 activate PAR1 has been demonstrated, which is an important molecule for angiogenesis and metastasis in a mouse model of ovarian cancer peritoneal metastasis [17]. Moreover, MMP1 has been reported associated with multi-drugs resistance in breast cancer [18, 19]. While drug resistance also a risk factor for ovarian cancer poor outcome. A study conducted that MMP1 mRNA was wrapped in the ovarian cacner cell-derived extracellular vesicles to induce apoptosis in mesothelial cells [20]. Importantly, MMP1 expression in ovarian cancer is tightly correlated with a poor prognosis. Thus, we presume that MMP1 signal activation involved in the CASZ1 low expression mucinous type ovarian cancer progression. Here, we aim to clarify the molecular mechanism of CASZ1 in mucinous type ovarian cancer.
Objective
In the third years of this project, we aim to demonstrate the role of CASZ1 in ovarian carcinoma and validate its association with clinical outcome in mucinous ovarian cancer patients, and the molecular mechanism of CASZ1 in mucinous tumor progression.
Materials and methods Immunohistochemistry
For immunohistochemistry, paraffin-embedded samples of 34 mucinous-type ovarian cancer patients were immunostained with the anti-human CASZ1 antibody (1:100; B-11; Santa Cruz Biotechnology, Inc.). After horseradish peroxidase (HRP)-conjugated immunoglobulin G (IgG) antibody was added for 1 hour, the specimens were analyzed by using avidin and biotinylated enzyme complex (ABC) detection. IHC imaging was observed under the ZEISS Axio Imager D2 microscope and quantitation of CASZ1 level was determined by using the Nuance imaging software (version 3.0.2, PerkinElmer, Inc.). This study was approved by Human Experimental and Ethics Committee of NCKUH (under an IRB number of A-ER-103-248). The written informed consent for participation in the study was obtained from participants.
Cell culture and transfection
The human mucinous type ovarian cancer cell lines, MCAS and RUMGS. The MCAS cell line was purchased
6
from the Human Science Research Resources Bank (HSRRB) (Osaka, Japan) and RUMGS cell line was obtained from the American Type Culture Collection (ATCC) (Manassas, VA). All of the cell lines were incubated in a humidified atmosphere with 5% CO2 at 37°C. The transient expression of CASZ1 was achieved by transfecting cells with CASZ1-expressing plasmids, using Lipofectamine reagent (Invitrogen). The transfection procedures were performed according to the manufacturer’s protocol. The CASZ1-shRNA- expressing lentiviral vectors were obtained from the National RNAi Core Facility (Academia Sinica, Taipei, Taiwan). 1 × 106 cells were inoculated in 10 cm dish for one day. Virus was put on the ice one hour before cells infection. We replaced cell culture medium and added 8 μg / ml polybrene in the dish plus virus (MOI = 3, cell number/virus titer × MOI). After 24 hours, we replaced culture medium and added puromycin to select Casz1- silenced cells.
Western blot assay
30 μg of protein were subjected to electrophoresis with 10% SDS-PAGE and transferred onto polyvinylidene fluoride (PVDF) membranes (IPVH00010; Millipore). Primary antibodies (Abs) was CASZ1 (1:1000; B-11;
Santa Cruz Biotechnology, Inc.). Secondary antibodies was anti-mouse HRP conjugates (1:10000 dilution;
A9044; Sigma). The blocking/dilution reagent was 5% skim milk in a mixture of tris-buffered saline plus 0.05%
Tween 20 (TBST). The proteins were visualized using an X-ray film and an enhanced chemiluminescence system (Millipore).
Immunocytochemistry
MCAS and RMUGS cells were fixed in 4% paraformaldehyde for 15 min at room temperature (RT). They were then incubated in 0.25% Triton X-100 in phosphate buffered saline (PBS) for 10 min after wash with ice cold PBS. 1% bovine serum albumin (BSA) in phosphate buffered saline with Tween 20 (PBST) was then used for 30 min to execute blocking, and then CASZ1 (1:100; B-11; Santa Cruz Biotechnology, Inc.) antibody was added and stored overnight at 4℃. After wash with PBS, samples were treated with secondary antibody with fluorescence conjugate in 1% BSA for 1 hour at RT in dark. The results of immunocytochemistry stain were observed through a confocal microscope.
7
Total RNA extraction and RT-qPCR to detect Casz1 and MMP1 expression
Cells were lysed with Trizol reagent (Invitrogen) according to the standard protocol. Then, a conventional two-step RT-PCR was performed using the M-MLV reverse transcriptase and GoTaq Master mix (Promega) as described in the manufacturer's instructions. Total RNA (1 μg) and 18mer oligo-dT (1 mM) was denatured by heating mixtures at 70°C for 5 min, followed by the addition of RT (50 U) and RNase inhibitor (20 U). RT was done at 42 °C for 1 h, followed by heating to 75°C for 15 min to inactivate the enzymes. After chilling on ice, the tubes were added with 180 μl d.d. H2O. To detect CASZ1 and MMP1 expression, 1 μl cDNA was added with GoTaq Master mix and indicated primer. The reaction was performed in StepOne Real-Time PCR System (Thermo Fisher Scientific).
Flow cytometry
For analyzing the cell apoptosis phenomena, Annexin V and PI were stained in MCAS or RMUGS cells and further analyzed by fluorescence-activated cell sorter (FACS; BD Biosciences). Moreover, anti-human CD44 conjugated with FITC () was used to detect activated cancer stem cell amount. Geometric mean fluorescence intensity (MFI) was determined by the FCSalyzer 0-5 software.
Statistical analysis
Statistical significance will be determined by Student’s t test in the in vitro study, with P < 0.05 considered to be statistically significant. Analyses of the data were performed using the GraphPad Software (Version 4.0, San Diego, CA). For clinical analysis, clinical variables will be compared using the Chi-square test or Student t test when appropriate. Survival curves will be constructed using the Kaplan–Meier method. A p value of <
0.05 is considered statistically significant. All statistical analyses were conducted with SPSS 16.0 statistical software.
Results
CASZ1 low expression on mucinous type ovarian cancer is associated with poor outcome.
To explore the role of CASZ1 expression in mucinous type ovarian cancer, we used 34 mucinous type ovarian cancer specimens to execute immunohistochemistry experiment. IHC imaging was observed under the ZEISS
8
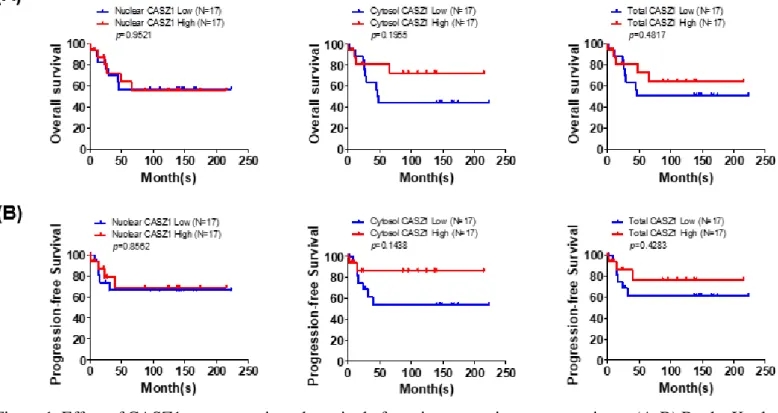
Axio Imager D2 microscope and quantitation of CASZ1 level was determined by using the Nuance imaging software (version 3.0.2, PerkinElmer, Inc.). According to quantitation of CASZ1 level (nuclear CASZ1 median=1.52; cytosol CASZ1 median=24.09; total CASZ1 median=28.69) to distingue into high CASZ1 high expression and CASZ1 low expression. After immunohistochemistry and statistical analyzed, we noticed cytosol CASZ1 and total CASZ1 low expression have a trend for poor prognosis (Figure 1).
Figure 1. Effect of CASZ1 on prognosis and survival of mucinous ovarian cancer patients. (A-B) By the Kaplan- Meier survival analysis, we found that patients with lower expression of cytosol and total CASZ1 had poorer overall and progression-free survival. However, expression of nuclear CASZ1 showed no correlation with overall and progression-free survival. This represents that low expression of cytosol CASZ1 in ovarian cancer patients may be a certain risk factor of disease progression.
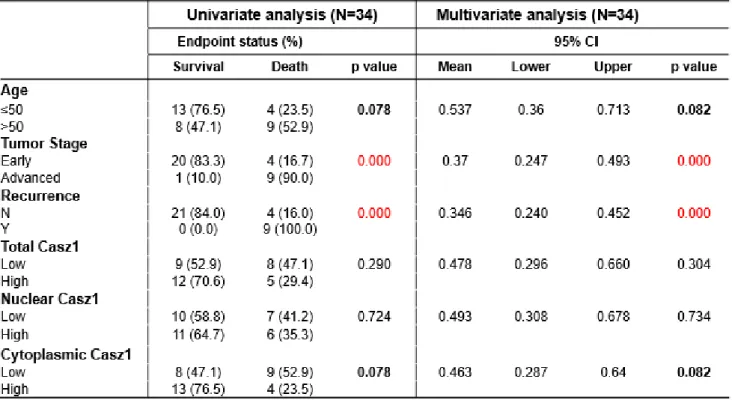
The age range of these 34 patients with mucinous type ovarian cancer is 27 to 70, median is 50. In these 34 patients, 24 patients who were diagnosed early stage, among these, 4 patients were appearing recurrence. In univariate and multivariate analysis, the tumor stage and recurrence were significantly associated with overall survival of patients with mucinous type ovarian cancer (Table 1). Notably, the cytoplasmic CASZ1 has a trend for significantly associated with overall survival. The results demonstrated that the low cytoplasmic CASZ1 expression maybe a potential prognosis marker of mucinous type ovarian cancer.
9
Table 1. Clinical characteristics of patients with mucinous ovarian cancer
CASZ1 gene knock down in mucinous type ovarian cancer cells causing the MMP1 gene up regulation.
To clarify the molecular mechanism of CASZ1 in mucinous type ovarian cancer cells, we first established the CASZ1-overexpressed (pCMV-1b-MCAS #mock, #08 and #11) and CASZ1-knock down (shCASZ1- RMUGS #Luc, #21 and #88) stable cell lines. Next, the CASZ1 protein expression levels were determined using western blot assay and immunofluorescence (Figure 2). The results show that CASZ1 does increased in MCAS cells and does decreased in RMUGS cells.
Figure 2. CASZ1 protein expression in mucinous cell lines with CASZ1-overexpression and CASZ1-knock down. (A) CASZ1 expression levels in MCAS and RMUGS mucinous cell lines were determined by western blotting assays. The molecular weight of CASZ1 is more than 120 kDa. β-actin was used as the internal control.
Two clones of pCMV-1b-MCAS (#08 and #11) showed CASZ1 slightly increased as compare with vector
10
control (Mock). And in shCasz1-RMUGS, #21 and #88 clones showed lower CASZ1 expression than vector control (Luc). (B) The expression and localization of CASZ1 in pCMV-1b-MCAS and shCasz1-RMUGS cell lines are shown respectively by immunofluorescence staining. The immunofluorescence microscopy image of 400× field show that CASZ1 mostly expressed in nucleus.
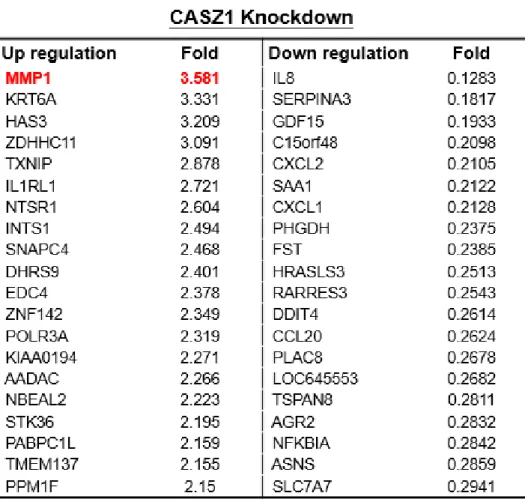
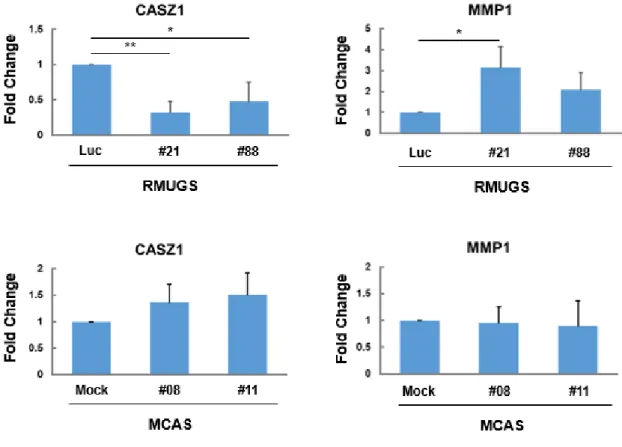
We next analyzed the cDNA microarray data and noticed the MMP1 gene significant up regulated (Fold=3.5806) in the shCASZ1-RMUGS cells (Table 2). qPCR data also showed MMP1 gene expression significantly reduce in shCASZ1-RUMGS cells. But MMP1 gene expression not significantly increased in pCMV-1b-MCAS cells (Figure 3). Known the CASZ1 low expression in mucinous type ovarian cancer is associated with poor outcome. And the MMP1 gene up regulated in RMUGS cells by the CASZ1 knocked down. The results suggest that CASZ1 low expression promote mucinous type ovarian cancer progression is mediated by MMP1 signal activation.
Table 2. MMP-1 is significant up regulation in RMUGS cells with CASZ1 knock down.
11
Figure 3. Real-time PCR results show that MMP1 gene expression regulated by CASZ1 in mucinous type ovarian cancer cells.
MMP1 up regulation enhance drug resistance, cancer stem cell and anti-apoptosis genes expression in mucinous type ovarian cancer cells, but no effect epithelial–mesenchymal transition (EMT).
To explore the molecular mechanism of CASZ1 low expression promote mucinous type ovarian cancer progression, we next analyzed the cDNA microarray data to find out the possible candidates. Reports indicated that MMP1 signal activation promote tumorigenesis, such as contribution in a proliferative/migratory and anti- apoptotic phenotype, drug resistance increasing and enhance cancer stemness features. Therefore, we analyzed these related genes change in shCASZ1-RUMGS cells through the cDNA microarray, and we noticed drug resistance genes (ABCC5 and ABCF1), cancer stemness gene (CD44) and anti-apoptosis gene (BCL9) were up regulated in shCASZ1-RUMGS cells (Table 3). But the EMT related genes (CDH1 and FN1) no differences in shCASZ1-RUMGS cells, imply CASZ1 low expression not effect cell migration. So, we next focus on the charactates of drug resistance, cancer stemness and anti-apoptosis to investigate the mechanism and functions of CSAZ1-MMP1 axis in mucinous type ovarian cancer.
Table 3. Listed are genes regulated by MMP-1. The data showed that ABCC5, ABCF1, CD44 and BCL9 are
12
upregulated in shCasz1-RMUGS cell lines. This indicates that CASZ1 is associated with drug resistance, stemness and anti-apoptosis.
CASZ1 knock down in RUMGS cells enhance the features of cancer stemness and anti-apoptosis through MMP1 signal activation.
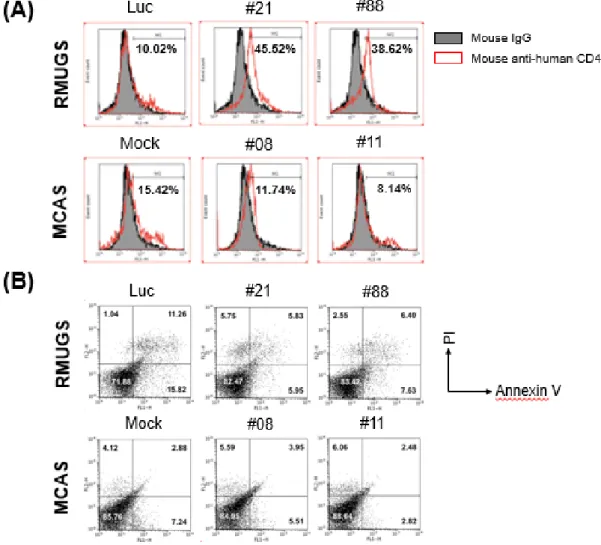
To validate the cancer stemness feature and anti-apoptosis function change of CASZ1 low expression and high expression, we use the shCASZ1-RMUGS and pCMV-1b-MCAS cell lines to experiments through immunofluoresence stain and flow cytometry. The data showed that CD44 increasing in the RMUGS cells with CASZ1 stable knocked down (shCASZ1-RMUGS, clone #21 and #88) as compare with vector control (Luc). In converse, the CD44 decreased in MCAS cells with CASZ1 overexpression (pCMV-1b-MCAS, clone #08 and
#11) as compare with vector control (Mock) (Figure 4A). In the meantime, the apoptotic cells reduced in RMUGS cells with CASZ1 stable knocked down (Figure 4B), imply CASZ1 low expression in mucinous type ovarian cancer occurring poor prognosis is because the cancer stemness and anti-apoptosis features increase.
And the result was due to the MMP1 signal activation. Hence, the CASZ1-MMP1 axis may be the potential target for future mucinous type ovarian cancer therapy.
13
Figure 4. CASZ1 expression can regulate cancer stemness and anti-apoptosis features in mucinous type ovarian cancer cell. (A) CD44 (cancer stem cell marker) expression increased in shCASZ1-RUMGS cells, and decreased in pCMV-1b-MCAS cells. (B) After Annexin V and PI staining and flow cytometry analyzed, the apoptotic cells decreased in shCASZ1-RUMGS cells, but not significant change in pCMV-1b-MCAS cells.
Emetine treatment inhibits the cancer stemness and anti-apoptosis features in mucinous type ovarian cancer cells with CASZ1 low expression.
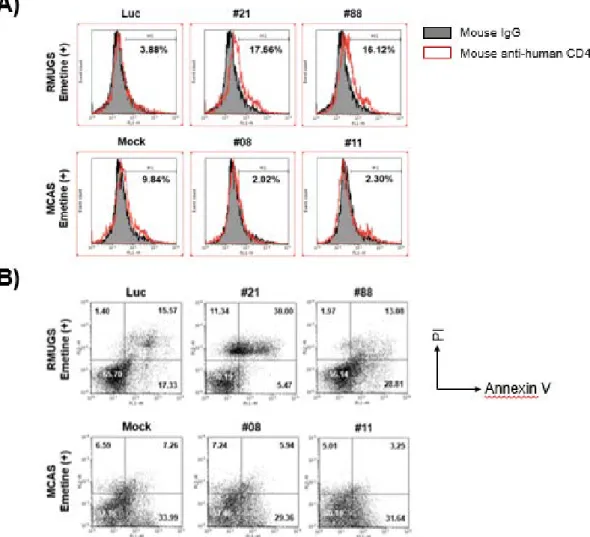
According to the results of connectivity map (CMap) network software, Emetine may have the therapeutic effect in the CASZ1 low expression type mucinous ovarian cancer. We next used the Emetine (purchased from BioVision Inc.) 5 μM to treat shCASZ1-RMUGS and pCMV-1b-MCAS cell lines. After 72 hours, the cells were executed immunofluorescence staining and flow cytometry analysis. The results showed that CD44 expression reduce and apoptotic cells increase in shCASZ1-RMUGS and pCMV-1b-MCAS cell lines after Emetine treatment (Figure 5). But the shCASZ1-RMUGS cell line is more obvious than pCMV-1b-MCAS cell line. Other words, Emetine maybe act the therapeutic drug for future mucinous type ovarian cancer treatment, especially the CASZ1 low expression mucinous carcinoma.
14
Figure 5. Emetine plays a therapeutic role in mucinous carcinoma. (A-B) After Emetine treatment (5μM for 72 hrs), the shCASZ1-RMUGS and pCMV-1b-MCAS cells were executed immunofluorescence staining and flow cytometry analysis to validate the therapeutic effect. The results suggest that CD44 decrease and apoptotic cell increase after Emetine treatment.
Discussion
Mucinous type ovarian cancer is a separate entity as compared with other epithelial ovarian cancers because it has a distinct natural history, molecular profile, chemo-sensitivity, and prognosis [21]. Mucinous type ovarian cacner is the most frequent histological subtype in women under the age of 40, while it is diagnosed as stage 1 in 80% of the cases [22, 23]. But the chemoresistance is still the major reason for poor outcome [24, 25].
Therefore, finding an effective treatment is an urgent issue.
Cisplatin is the first-line chemotherapeutic agents in the treatment of ovarian cancer. However, chemoresistance is the leading cause of therapeutic failure and is responsible for the poor overall survival rate.
A study conducted that Emetine treatment enhance the sensitivity of ovarian carcinoma cells to cisplatin through downregulation of bcl-xL [26]. In the meantime, we used the connectivity map (CMap) network software to
15
screening the candidates of ovarian cancer therapy under CASZ1 low expression situation, Emetine has the highest score. In in vitro experiments, we observed that Emetine treatment reversed cancer stemness and anti- apoptosis features in mucinous type ovarian cancer cells with CASZ1 low expression. Emetine may act the therapeutic drug in mucinous type ovarian cancer, especially the CASZ1 low expression.
In 2014, the World Health Organization (WHO) introduced a new diagnostic classification of mucinous ovarian carcinoma, with two categories according to the growth pattern: the expansile subtype (back-to-back glands without stromal invasion) and the infiltrative subtype (malignant cells or cell clusters with destructive stromal invasion). Expansile subtype mucinous ovarian cancer have a lower metastatic potential and low risk of relapse. In contrast, infiltrative subtype mucinous ovarian cancer is more aggressive and high risk of relapse [27-30]. CASZ1 whether correlated with mucinous ovarian cancer subtype needs more experiments to validate in future. Here, we observed CASZ1 low expression occur poor prognosis in mucinous type ovarian cancer, while it may be induced by MMP1 signal activation to causing cancer stemness and anti-apoptosis features increase. However, the Emetine treatment sufficient to rescute the phenomena. These results imply Emetine may have therapeutic effect in mucinous type ovarian cancer, and it is targeting on the CASZ1-MMP1 axis.
Reference
1. Benedet JL, Bender H, Jones H, 3rd, Ngan HY and Pecorelli S. FIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. FIGO Committee on Gynecologic Oncology.
Int J Gynaecol Obstet 2000; 70: 209-262.
2. Siegel R, Ma J, Zou Z and Jemal A. Cancer statistics, 2014. CA Cancer J Clin 2014; 64: 9-29.
3. Clarke-Pearson DL. Clinical practice. Screening for ovarian cancer. N Engl J Med 2009; 361: 170-177.
4. Seidman JD, Horkayne-Szakaly I, Haiba M, Boice CR, Kurman RJ, Ronnett BM. The histologic type and stage distribution of ovarian carcinomas of surface epithelial origin. Int J Gynecol Pathol. 2004;23(1):41-4.
5. Cheasley D, Wakefield MJ, Ryland GL, Allan PE, Alsop K, Amarasinghe KC, et al. The molecular origin and taxonomy of mucinous ovarian carcinoma. Nat Commun. 2019;10(1):3935.
6. Peres LC, Cushing-Haugen KL, Köbel M, Harris HR, Berchuck A, Rossing MA, et al. Invasive Epithelial Ovarian Cancer Survival by Histotype and Disease Stage. J Natl Cancer Inst. 2019;111(1):60-68.
7. Prat J, D'Angelo E, Espinosa I. Ovarian carcinomas: at least five different diseases with distinct histological features and molecular genetics. Hum Pathol. 2018;80:11-27.
8. Jordan SJ, Green AC, Whiteman DC, Webb PM; Australian Ovarian Cancer Study Group. Risk factors for benign, borderline and invasive mucinous ovarian tumors: epidemiological evidence of a neoplastic continuum?
Gynecol Oncol. 2007;107(2):223-30.
9. Liu Z, Yang X, Tan F, Cullion K, Thiele CJ. Molecular cloning and characterization of human Castor, a novel human gene upregulated during cell differentiation. Biochem Biophys Res Commun. 2006;344:834–844.
16
10. Hitier R, Chaminade M, Preat T. The Drosophila castor gene is involved in postembryonic brain development. Mech Dev. 2001;103:3–11.
11. Mellerick DM, Kassis JA, Zhang SD, Odenwald WF. castor encodes a novel zinc finger protein required for the development of a subset of CNS neurons in Drosophila. Neuron. 1992;9:789–803.
12. Liu Z, Naranjo A, Thiele CJ. CASZ1b, the short isoform of CASZ1 gene, coexpresses with CASZ1a during neurogenesis and suppresses neuroblastoma cell growth. PLoS One. 2011;6:e18557.
13. Liu Z, Yang X, Li Z, McMahon C, Sizer C, Barenboim-Stapleton L, Bliskovsky V, Mock B, Ried T, London WB, Maris J, Khan J, Thiele CJ. CASZ1, a candidate tumor-suppressor gene, suppresses neuroblastoma tumor growth through reprogramming gene expression. Cell Death Differ. 2011;18:1174–1183.
14. Kim B, Jung M, Moon KC. The Prognostic Significance of Protein Expression of CASZ1 in Clear Cell Renal Cell Carcinoma. Dis Markers. 2019;2019:1342161.
15. Wu YY, Chang CL, Chuang YJ, Wu JE, Tung CH, Chen YC, Chen YL, Hong TM, Hsu KF. CASZ1 is a novel promoter of metastasis in ovarian cancer. Am J Cancer Res. 2016;6(6):1253-70.
16. Zhang Y, Chen Q. Relationship between matrix metalloproteinases and the occurrence and development of ovarian cancer. Braz J Med Biol Res. 2017;50(6):e6104.
17. Agarwal A, Tressel SL, Kaimal R, Balla M, Lam FH, Covic L, Kuliopulos A. Identification of a metalloprotease-chemokine signaling system in the ovarian cancer microenvironment: implications for antiangiogenic therapy. Cancer Res. 2010;70(14):5880-90.
18. Wang QM, Lv L, Tang Y, Zhang L, Wang LF. MMP-1 is overexpressed in triple-negative breast cancer tissues and the knockdown of MMP-1 expression inhibits tumor cell malignant behaviors in vitro. Oncol Lett.
2019;17(2):1732-1740.
19. Shen CJ, Kuo YL, Chen CC, Chen MJ, Cheng YM. MMP1 expression is activated by Slug and enhances multi-drug resistance (MDR) in breast cancer. PLoS One. 2017 Mar 23;12(3):e0174487.
20. Yokoi A, Yoshioka Y, Yamamoto Y, Ishikawa M, Ikeda SI, Kato T, et al. Malignant extracellular vesicles carrying MMP1 mRNA facilitate peritoneal dissemination in ovarian cancer. Nat Commun. 2017;8:14470.
21. Cancer Genome Atlas Research Network. Integrated genomic analyses of ovarian carcinoma. Nature.
2011;474(7353):609-15.
22. Yoshikawa N, Kajiyama H, Mizuno M, Shibata K, Kawai M, Nagasaka T, Kikkawa F. Clinicopathologic features of epithelial ovarian carcinoma in younger vs. older patients: analysis in Japanese women. J Gynecol Oncol. 2014;25(2):118-23.
23. Seidman JD, Horkayne-Szakaly I, Haiba M, Boice CR, Kurman RJ, Ronnett BM. The histologic type and stage distribution of ovarian carcinomas of surface epithelial origin. Int J Gynecol Pathol. 2004;23(1):41-4.
24. Xu W, Rush J, Rickett K, Coward JI. Mucinous ovarian cancer: A therapeutic review. Crit Rev Oncol Hematol. 2016;102:26-36.
25. Morice P, Gouy S, Leary A. Mucinous Ovarian Carcinoma. N Engl J Med. 2019;380(13):1256-1266.
26. Sun Q, Yogosawa S, Iizumi Y, Sakai T, Sowa Y. The alkaloid emetine sensitizes ovarian carcinoma cells to cisplatin through downregulation of bcl-xL. Int J Oncol. 2015;46(1):389-94.
27. Lee KR, Scully RE. Mucinous tumors of the ovary: a clinicopathologic study of 196 borderline tumors (of intestinal type) and carcinomas, including an evaluation of 11 cases with 'pseudomyxoma peritonei'. Am J Surg Pathol. 2000;24(11):1447-64.
28. Rodríguez IM, Prat J. Mucinous tumors of the ovary: a clinicopathologic analysis of 75 borderline tumors (of intestinal type) and carcinomas. Am J Surg Pathol. 2002;26(2):139-52.
17
29. Muyldermans K, Moerman P, Amant F, Leunen K, Neven P, Vergote I. Primary invasive mucinous ovarian carcinoma of the intestinal type: importance of the expansile versus infiltrative type in predicting recurrence and lymph node metastases. Eur J Cancer. 2013;49(7):1600-8.
30. Gouy S, Saidani M, Maulard A, et al. Characteristics and Prognosis of Stage I Ovarian Mucinous Tumors According to Expansile or Infiltrative Type. Int J Gynecol Cancer. 2018;28(3):493-499.
18
科技部補助專題研究計畫成果自評表
請就研究內容與原計畫相符程度、達成預期目標情況、研究成果之學術或應用價 值(簡要敘述成果所代表之意義、價值、影響或進一步發展之可能性) 、是否適 合在學術期刊發表或申請專利、主要發現(簡要敘述成果是否具有政策應用參考 價值及具影響公共利益之重大發現)或其他有關價值等,作一綜合評估。
1. 請就研究內容與原計畫相符程度、達成預期目標情況作一綜合評估
█ 達成目標
□ 未達成目標(請說明,以 100 字為限)
□ 實驗失敗
□ 因故實驗中斷
□ 其他原因 說明:
2. 研究成果在學術期刊發表或申請專利等情形(請於其他欄註明專利及技轉之 證號、合約、申請及洽談等詳細資訊)
論文: □已發表□未發表之文稿 □撰寫中 █無 專利: □已獲得□申請中 █無
技轉: □已技轉□洽談中
█無
其他:(以 200 字為限)
3. 請依學術成就、技術創新、社會影響等方面,評估研究成果之學術或應用價 值(簡要敘述成果所代表之意義、價值、影響或進一步發展之可能性,以 500 字為限) 。
在此計畫中,我們證實了 CASZ1-MMP1 axis 可能是黏液性卵巢癌的治療標 靶,而 Emetine 具有治療潛力。除了將此部分研究成果撰寫學術論文,對未來 卵巢癌的治療策略亦有另一個參考價值。一旦提高卵巢癌的治癒率,不僅可 減少病患的焦慮感,亦可減少健保費用在治療癌症用藥的支出。
4. 主要發現
本研究 具有政策應用參考價值: █否 □是,建議提供機關_______
(勾選「是」者,請列舉建議可提供施政參考之業務主管機關) 本研究具影響公共利益之重大發現: █否 □是
說明:(以 150 字為限)
19
Supplemental Figures
Supplemental Figure 1. The mrna expression level in four type epithelial ovarian cancer cells.
106年度專題研究計畫成果彙整表
計畫主持人:許耿福 計畫編號:106-2314-B-006-060-MY3 計畫名稱:Castor 基因在卵巢癌轉移之研究
成果項目 量化 單位
質化
(說明:各成果項目請附佐證資料或細 項說明,如期刊名稱、年份、卷期、起 訖頁數、證號...等)
國
內 學術性論文
期刊論文 0
研討會論文 0 篇
專書 0 本
專書論文 0 章
技術報告 0 篇
其他 0 篇
國
外 學術性論文
期刊論文 0
研討會論文 0 篇
專書 0 本
專書論文 0 章
技術報告 0 篇
其他 0 篇
參 與 計 畫 人 力
本國籍
大專生 0
人次
碩士生 1 碩士生 張文齊參與研究計畫
博士生 0
博士級研究人員 0
專任人員 1 碩士級專案人員 鍾雯如參與研究計畫
非本國籍
大專生 0
碩士生 0
博士生 0
博士級研究人員 0
專任人員 0
其他成果
(無法以量化表達之成果如辦理學術活動
、獲得獎項、重要國際合作、研究成果國 際影響力及其他協助產業技術發展之具體 效益事項等,請以文字敘述填列。)
在此計畫中,我們證實了CASZ1-MMP1 axis可能是黏液性 卵巢癌的治療標靶,而Emetine具有治療潛力。除了將此 部分研究成果撰寫學術論文,對未來卵巢癌的治療策略亦 有另一個參考價值。一旦提高卵巢癌的治癒率,不僅可減 少病患的焦慮感,亦可減少健保費用在治療癌症用藥的支 出。