Contents lists available atScienceDirect
Archives of Gerontology and Geriatrics
journal homepage:www.elsevier.com/locate/archger
Synergistic e ffect of low handgrip strength and malnutrition on 4-year all- cause mortality in older males: A prospective longitudinal cohort study
Yu-Chun Wang
a,b, Chih-Kuang Liang
a,c,d,e, Ying-Hsin Hsu
a, Li-Ning Peng
c,d,f, Che-Sheng Chu
a,g, Mei-Chen Liao
a, Hsiu-Chu Shen
a,e, Ming-Yueh Chou
a,b,c,d,⁎, Yu-Te Lin
a,eaCenter for Geriatrics and Gerontology, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan
bChia Nan University of Pharmacy and Science, Taiwan
cAging and Health Research Center, National Yang Ming University, Taipei, Taiwan
dDepartment of Geriatric Medicine, National Yang Ming University School of Medicine, Taipei, Taiwan
eDivision of Neurology, Department of Medicine, Kaohsiung Veterans General, Taiwan
fCenter for Geriatrics and Gerontology, Taipei Veterans General Hospital, Taipei, Taiwan
gDepartment of Psychiatry, Kaohsiung Veterans General Hospital Kaohsiung, Taiwan
A R T I C L E I N F O
Keywords:
Older adults Malnutrition Handgrip strength Mortality
A B S T R A C T
Background: No studies have yet examined the interrelationship of malnutrition and low handgrip strength in terms of mortality. The aim of the present study was to evaluate the potential synergistic effects of malnutrition and low handgrip strength on mortality among older adults living in a retirement community.
Methods: This prospective longitudinal cohort study recruited subjects aged 65 years and over from a veterans care home in Taiwan in 2013. Nutritional status was assessed using the Mini-Nutritional Assessment-Short Form (MNA-SF, malnutrition was MNA-SF < 12); muscle strength was measured by handgrip strength (low handgrip strength was handgrip strength < 26 kg). The Kaplan-Meier method with the log-rank test was used to estimate survival differences between groups and Cox proportional regression model was used to estimate the adjusted difference in 4-year all-cause mortality between groups.
Results: Recruited for the present study were 333 male participants (mean age 85.4 ± 5.7 years). Of these, 50.2% had malnutrition and 54.7% had low handgrip strength. Compared with subjects with no malnutrition and low handgrip strength, those with malnutrition had significantly greater risk of 4-year all-cause mortality (adjusted hazards ratio: 2.05, 95% confident interval [CI]: 1.04–4.01); hazard ratio increased to 3.41 (95% CI 1.93–6.04) for those with both malnutrition and low handgrip strength.
Conclusions: Malnutrition was an independent risk factor for 4-year all-cause mortality and low handgrip strength with malnutrition synergistically increased the mortality risk. Further study is needed to confirm the effectiveness of integrated programs to assist those at risk.
1. Introduction
Malnutrition is highly prevalent and significantly associated with geriatric syndromes in community-dwelling older adults (Verlaan et al., 2017; Wei, Nyunt, Gao, Wee, & Ng, 2017). The prevalence of mal- nutrition is generally above 30% in independent community-dwelling older adults and is up to 50% in those with poor physical function (Cereda et al., 2016;Kaiser et al., 2010). Risk of malnutrition in older adults is related to old age, chronic diseases, frailty, loss of interest in life, impaired efficacy in swallowing, polypharmacy, and in- stitutionalization (Chapman, 2006;Favaro-Moreira et al., 2016). The
adverse health outcomes associated with malnutrition include in- creasing severity of disability (Sharkey, 2002), more function decline (Chu et al., 2017), higher prevalence of comorbidities (e.g., delirium) (Chu et al., 2016), longer hospital stays (Ruiz et al., 2018), higher readmission rates (Chu et al., 2017), significant economic burden (Ruiz et al., 2018), decreased quality of life (Keller, Ostbye, & Goy, 2004), and higher mortality rates (Wei et al., 2018).
Handgrip strength, suggested by the Academy of Nutrition and Dietetics and the American Society for Parenteral and Enteral Nutrition (ASPEN) to screen functional status, is reported to be associated with decline in cognitive function, falls, postsurgical complications,
https://doi.org/10.1016/j.archger.2019.05.007
Received 26 April 2019; Received in revised form 6 May 2019; Accepted 7 May 2019
⁎Corresponding author at: Center for Geriatrics and Gerontology, Kaohsiung Veterans General Hospital, 386, Ta-Chung 1st RD., Zuoying District 813, Kaohsiung, Taiwan.
E-mail address:mychou@vghks.gov.tw(M.-Y. Chou).
Available online 08 May 2019
0167-4943/ © 2019 Published by Elsevier B.V.
T
functional decline, and even death (Alfaro-Acha et al., 2006;Bohannon, 2001; McLean et al., 2014; Rantanen et al., 1999, 2003; Stessman, Rottenberg, Fischer, Hammerman-Rozenberg, & Jacobs, 2017; Xue, Walston, Fried, & Beamer, 2011). In addition to handgrip strength, muscle mass and gait speed are the compartments of sarcopenia.
However, handgrip strength is considered as a key characteristic of sarcopenia, by the European Working Group on Sarcopenia in Older People (EWGSOP) (Cruz-Jentoft et al., 2019), and was reported as a more practical measure of nutrition assessment than the 5-meter walk by McNicholl et al., due to its higher complete rate (McNicholl et al., 2018). Most previous studies have focused on independent correlations of malnutrition or low handgrip strength with mortality, but the effect on mortality of the two together remains unclear. An association be- tween malnutrition and low handgrip strength in older adults was re- cently reported (Kim, Jeon, & Jeong, 2019), implying a possible sy- nergistic effect on all-cause mortality in older adults. Thus, the aim of the present study was to evaluate the potential synergistic effect of malnutrition and low handgrip strength on mortality among older adults living in a retirement community in Taiwan.
2. Materials and methods 2.1. Participant recruitment
Residents of a Veteran’s Care Home (VCH) were invited to partici- pate in this prospective longitudinal cohort study in 2013 [43]. VCH is a veteran’s retirement community and is similar to assisted living in the United States. All participants aged 65 years and over were enrolled when they provided signed informed consent. Subjects with the fol- lowing conditions were excluded: (1) inability to communicate with research nurses, (2) inability or unwillingness to provide informed consent, (3) diagnosed with moderate or advanced dementia, and (4) inability to perform the physical measurement, such as handgrip strength. The study protocol was reviewed and approved by the Institutional Review Board of Kaohsiung Veterans General Hospital (IRB19-1234).
2.2. Comprehensive geriatric assessments
Comprehensive geriatric assessments were performed in all parti- cipants by well-trained research nurses who collected demographic data, including age, educational level, marital status, smoking status, body mass index (BMI, kg/m2), Charlson’s Comorbidity Index (CCI) (Charlson, Pompei, Ales, & MacKenzie, 1987), polypharmacy (defined as currently using more than 4 drugs for over 2 weeks), cognitive im- pairment (defined as scores < 24 on the Chinese version of the Mini- Mental State Examination, MMSE) (Folstein, Folstein, & McHugh, 1975), depressive symptoms (defined by scores > 5 on the 15-item Chinese Geriatric Depression Scale, GDS-15) (Nyunt, Fones, Niti, & Ng, 2009), malnutrition (defined by scores < 12 on the Mini-Nutritional Assessment-Short Form, MNA-SF) (Kaiser et al., 2009), pain severity (assessed by visual analogue scale, VAS score) (Huskisson, 1974), and baseline Activities of Daily Living (ADLs, assessed by Barthel Index, BI) (Collin, Wade, Davies, & Horne, 1988). The mortality dates were re- corded until December 2017 from the VCH medical records.
2.3. Definition and assessment of handgrip strength and gait speed
Muscle strength was measured by handgrip strength using a digital dynamometer (TTM-YD, Tokyo, Japan). The best measurement of three trials using the dominant hand was recorded. Usual gait speed was measured by using a timed 6-meter walking test (with or without walking aids) with a static start throughout the hallway without de- celeration. Low handgrip strength was defined as handgrip strength < 26 kg and low gait speed was defined as < 0.8 m/s ac- cording to the definition of the Asian Working Group for Sarcopenia
(Chen et al., 2014).
2.4. Statistical analysis
All continuous variables were presented as mean ± standard de- viation (SD), and categorical data were presented as numbers (per- centage). Student’s t-test was used to compare continuous variables between groups and the chi-squared test or Fisher exact test was used to compare categorical variables between groups, as appropriate. To evaluate the synergistic effect of malnutrition and low handgrip strength on 4-year all-cause mortality, participants were classified into one of four groups: good nutrition with good handgrip strength (Group 1), good nutrition with low handgrip strength (Group 2), malnutrition with good handgrip strength (Group 3), and malnutrition with low handgrip strength (Group 4). The Kaplan-Meier method with the log- rank test was used to estimate the survival difference between groups and Cox proportional regression model was used to estimate the dif- ference in 4-year all-cause mortality between groups after adjusting for the covariates of age, CCI, polypharmacy, cognitive impairment, BI, slow gait speed, depressive symptoms, and hearing impairment. All statistical analyses were performed using IBM SPSS Statistics for Windows, Version 21.0 IBM Corp., Armonk, NY). P < 0.05 was used to indicated statistical significance.
3. Results
3.1. Clinical characteristics of participants
In total, 333 male participants were recruited for the present study.
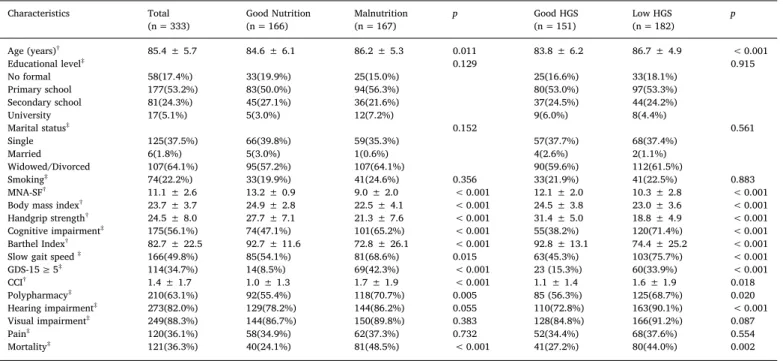
The mean age was 85.4 ± 5.7 years. Among them, 167 (50.2%) were identified as having malnutrition and 54.7% were identified as having low handgrip strength.Table 1shows the difference between groups by malnutrition and handgrip strength status. Compared with the partici- pants with good nutrition, those with malnutrition were older (86.2 ± 5.3 versus 84.6 ± 6.1 years, p = 0.011), had lower BMI (22.5 ± 4.1 versus 24.9 ± 2.8, p < 0.001), lower handgrip strength (21.3 ± 7.6 versus 27.7 ± 7.1 kg, p < 0.001), more cognitive im- pairment (65.2% versus 47.1%, p < 0.001), lower ADL levels (BI 72.8 ± 26.1 versus 92.7 ± 11.6, p < 0.001), lower gait speed (68.6% versus 54.1%, p = 0.015), higher rates of depressive symptoms (42.3% versus 8.5%, p < 0.001), higher CCI scores (1.7 ± 1.9 versus 1.0 ± 1.3, p < 0.001), higher rates of polypharmacy (70.7% versus 55.4%, p = 0.005), and a higher 4-year all-cause mortality rate (48.5%
versus 24.1%, p < 0.001) (Table 1).
Compared with those classified with good handgrip strength, those with low handgrip strength were older (86.7 ± 4.9 versus 83.8 ± 6.2 years, p < 0.001) and had lower BMI (23.0 ± 3.6 versus 24.5 ± 3.8, P < 0.001), more cognitive impairment (71.4% versus 38.2%, p < 0.001), lower ADL scores (74.4 ± 25.2 versus 92.8 ± 13.1, p < 0.001), slower gait speed (75.7% versus 45.3%, p < 0.001), higher rates of depressive symptoms (33.9% versus 15.3%, p < 0.001), higher CCI scores (1.6 ± 1.9 versus 1.1 ± 1.4, p = 0.018), higher rates of polypharmacy (68.7% versus 56.3%, p = 0.020), more hearing impairment (90.1% versus 72.8%, p < 0.001), and higher rates of 4-year all-cause mortality (44.0%
versus 27.2%, p = 0.002) (Table 1).
Fig. 1 shows the survival curve of those with and without mal- nutrition (χ2= 22.03, P < 0.001) or low handgrip strength (χ2= 10.74, P < 0.001) using Kaplan-Meier survival curves along with their respective log-rank tests.
3.2. Synergistic effects of low handgrip strength and malnutrition on 4-year all-cause mortality
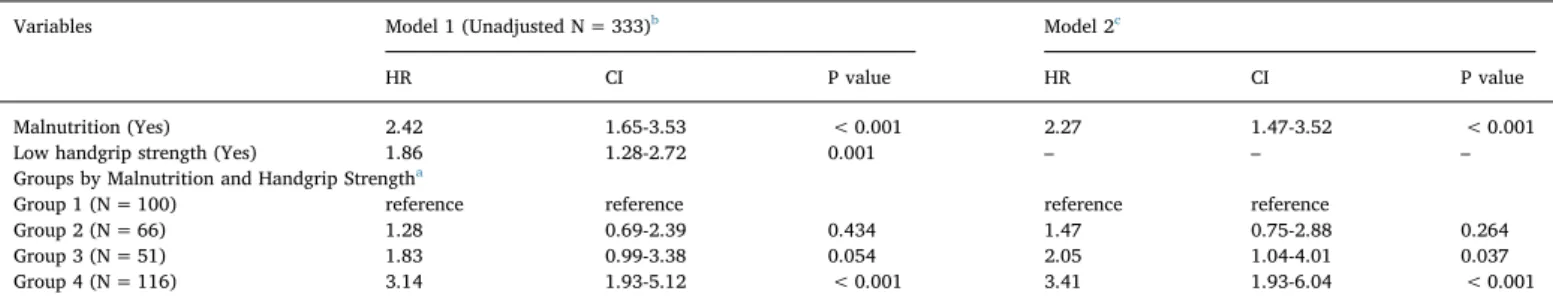
Overall, participants with malnutrition and low handgrip strength were at significantly higher risk for 4-year all-cause mortality [Hazard
ratio (HR): 2.42, 95% confident interval (CI): 1.65–3.53 for subjects with malnutrition; HR: 1.86, 95% CI: 1.28–2.72 for those with low handgrip strength] (Table 2). Based on the classifications of malnutri- tion and low handgrip strength, Groups 3 and 4 were at higher risk for 4-year all-cause mortality (HR: 1.83, 95% CI: 0.99–3.38 for Group 3;
HR: 3.14, 95% CI: 1.93–5.12 for Group 4). After adjusting for covari- ates, Group 3 and Group 4 remained significantly associated with 4 year all-cause mortality (adjusted HR: 2.05, 95% CI: 1.04–4.01 for Group 3;
adjusted HR: 3.41, 95% CI: 1.93–6.04 for Group 4). The 4-year survival curves of the four groups based on nutritional status and handgrip strength are shown inFig. 2(χ2= 28.64, p < 0.001).
4. Discussion 4.1. Overall results
This prospective longitudinal cohort study evaluated the synergistic effects of malnutrition and low handgrip strength on the prediction of 4-year all-cause mortality among male older adults living at the VCH.
Results of the present study showed that 50.2% of the participants were classified as having malnutrition, a rate similar to those in previous studies (Cereda et al., 2016; Kaiser et al., 2010). The present study showed that participants with malnutrition were at significantly higher Table 1
Sociodemographic Characteristics of Participants by Nutritional Status and Handgrip Strength (HGS).
Characteristics Total Good Nutrition Malnutrition p Good HGS Low HGS p
(n = 333) (n = 166) (n = 167) (n = 151) (n = 182)
Age (years)† 85.4 ± 5.7 84.6 ± 6.1 86.2 ± 5.3 0.011 83.8 ± 6.2 86.7 ± 4.9 < 0.001
Educational level‡ 0.129 0.915
No formal 58(17.4%) 33(19.9%) 25(15.0%) 25(16.6%) 33(18.1%)
Primary school 177(53.2%) 83(50.0%) 94(56.3%) 80(53.0%) 97(53.3%)
Secondary school 81(24.3%) 45(27.1%) 36(21.6%) 37(24.5%) 44(24.2%)
University 17(5.1%) 5(3.0%) 12(7.2%) 9(6.0%) 8(4.4%)
Marital status‡ 0.152 0.561
Single 125(37.5%) 66(39.8%) 59(35.3%) 57(37.7%) 68(37.4%)
Married 6(1.8%) 5(3.0%) 1(0.6%) 4(2.6%) 2(1.1%)
Widowed/Divorced 107(64.1%) 95(57.2%) 107(64.1%) 90(59.6%) 112(61.5%)
Smoking‡ 74(22.2%) 33(19.9%) 41(24.6%) 0.356 33(21.9%) 41(22.5%) 0.883
MNA-SF† 11.1 ± 2.6 13.2 ± 0.9 9.0 ± 2.0 < 0.001 12.1 ± 2.0 10.3 ± 2.8 < 0.001
Body mass index† 23.7 ± 3.7 24.9 ± 2.8 22.5 ± 4.1 < 0.001 24.5 ± 3.8 23.0 ± 3.6 < 0.001
Handgrip strength† 24.5 ± 8.0 27.7 ± 7.1 21.3 ± 7.6 < 0.001 31.4 ± 5.0 18.8 ± 4.9 < 0.001
Cognitive impairment‡ 175(56.1%) 74(47.1%) 101(65.2%) < 0.001 55(38.2%) 120(71.4%) < 0.001
Barthel Index† 82.7 ± 22.5 92.7 ± 11.6 72.8 ± 26.1 < 0.001 92.8 ± 13.1 74.4 ± 25.2 < 0.001
Slow gait speed‡ 166(49.8%) 85(54.1%) 81(68.6%) 0.015 63(45.3%) 103(75.7%) < 0.001
GDS-15≥ 5‡ 114(34.7%) 14(8.5%) 69(42.3%) < 0.001 23 (15.3%) 60(33.9%) < 0.001
CCI† 1.4 ± 1.7 1.0 ± 1.3 1.7 ± 1.9 < 0.001 1.1 ± 1.4 1.6 ± 1.9 0.018
Polypharmacy‡ 210(63.1%) 92(55.4%) 118(70.7%) 0.005 85 (56.3%) 125(68.7%) 0.020
Hearing impairment‡ 273(82.0%) 129(78.2%) 144(86.2%) 0.055 110(72.8%) 163(90.1%) < 0.001
Visual impairment‡ 249(88.3%) 144(86.7%) 150(89.8%) 0.383 128(84.8%) 166(91.2%) 0.087
Pain‡ 120(36.1%) 58(34.9%) 62(37.3%) 0.732 52(34.4%) 68(37.6%) 0.554
Mortality‡ 121(36.3%) 40(24.1%) 81(48.5%) < 0.001 41(27.2%) 80(44.0%) 0.002
Values presented as†mean ± standard deviation;‡number (%).
Abbreviations: MNA-SF, Mini Nutritional Assessment-Short Form, scores < 12 indicate risk of malnutrition; MMSE, Mini-Mental State Examination, scores < 24 indicate cognitive impairment; slow gait speed defined as < 0.8 m/s; GDS-15, 15-item Geriatric Depression Scale, scores ≥5 indicate depressive symptoms; CCI, Charlson’s Comorbidity Index.
Fig. 1. Kaplan-Meier survival curves of older adults (A) with or without malnutrition and (B) low handgrip strength (HGS).
risk for 4-year all-cause mortality than those without. Furthermore, the synergistic effect of low handgrip strength with malnutrition increased the adjusted hazard ratio of 4-year all-cause mortality from 2.05 to 3.41. This study is thefirst to report this significant synergistic effect of low handgrip strength and malnutrition with this design.
4.2. Adverse outcomes associated with malnutrition
Older age increases the risk of malnutrition, multimorbidity, and disability. Aging also places people at risk of accumulating chronic diseases and impairments—such as cognitive and physical decline, depressive symptoms, socioeconomic decline, and poor oral health—all of which can contribute to the development of malnutrition and its adverse outcomes (Favaro-Moreira et al., 2016). Malnutrition has been reported to be significantly associated with older age, polypharmacy, physical and cognitive decline, constipation, dementia, eating depen- dence, poor appetite, institutionalization, and frailty (Favaro-Moreira et al., 2016). In our present study, malnutrition was related to older age, lower BMI, lower handgrip strength, higher physical and cognitive impairment, lower gait speed, more depressive symptoms, more co- morbidity, and polypharmacy, and which could also predict mortality.
Understanding the risk factors for malnutrition in male older adults can
help with the development of integrated intervention programs to im- prove outcomes in those at risk of malnutrition (Kang et al., 2019;
Ngandu et al., 2015).
4.3. The relationship of low handgrip strength and malnutrition
Much evidence shows that lower physical function, as indicated by lower handgrip strength or slower gait speed, frailty, and sarcopenia, is more prevalent in older adults with malnutrition (Wei et al., 2017). In addition, there is increasing awareness of the overlap between physical dysfunction and malnutrition, as well as the common interventions for both (Laur, McNicholl, Valaitis, & Keller, 2017). Currently, no uni- versally accepted definition of malnutrition exists, despite the many consensus statements and assessment tools available. These assessment tools were developed based on the definition of malnutrition by White et al. as an overall“decline in lean body mass, with the potential for functional impairment” (White, Guenter, Jensen, Malone, & Schofield, 2012). The Academy of Nutrition and Dietetics and ASPEN re- commendations include diminished functional status as one of their six criteria to identify malnutrition. This recommendation acknowledges that individual clinical markers of body composition and physical dysfunction characterize malnutrition; however, it failed to address the interaction between malnutrition and physical dysfunction in terms of clinical outcome. Recent research found malnutrition associated with the need for more complex care among the oldest old male residents of long-term care facilities with mobility-type prefrailty or frailty, a cor- relation not found among those with good physical function. This result reinforces the relationship between nutritional status and physical function (Chou et al., 2019).
4.4. Interaction and synergistic effect of malnutrition and handgrip strength
In the present study, we found that malnutrition was significantly associated with low handgrip strength and slow gait speed, compatible with a previous study (Akbar & Setiati, 2018). Malnutrition is a widely known key mechanism in the pathogenesis of sarcopenia. Sarcopenia, in addition to the negative result of malnutrition, is also a negative consequence of physical inactivity, chronic diseases, or hormonal, cy- tokine, or metabolic imbalances (Campins et al., 2017; Jeejeebhoy, 2012), and is well known to lead to such adverse health outcomes as falls, institutionalization, functional dependence, and even mortality (Chen et al., 2014). A recent population-based cross-sectional study reported that excessive carbohydrate and inadequate protein intake could lead to malnutrition and was associated with low handgrip strength in community-dwelling older adults (Kim et al., 2019). An- other study reported that low handgrip strength could independently predict nutritional status (Flood, Chung, Parker, Kearns, & O’Sullivan, Table 2
The interrelationship between malnutrition, handgrip strength and 4-year all-cause mortality based on Cox regression analysis.
Variables Model 1 (Unadjusted N = 333)b Model 2c
HR CI P value HR CI P value
Malnutrition (Yes) 2.42 1.65-3.53 < 0.001 2.27 1.47-3.52 < 0.001
Low handgrip strength (Yes) 1.86 1.28-2.72 0.001 – – –
Groups by Malnutrition and Handgrip Strengtha
Group 1 (N = 100) reference reference reference reference
Group 2 (N = 66) 1.28 0.69-2.39 0.434 1.47 0.75-2.88 0.264
Group 3 (N = 51) 1.83 0.99-3.38 0.054 2.05 1.04-4.01 0.037
Group 4 (N = 116) 3.14 1.93-5.12 < 0.001 3.41 1.93-6.04 < 0.001
HR, hazard ratio; CI, confidence interval; MMSE, Mini-Mental State Evaluation; GDS-15, Geriatric Depression Scale.
a Group 1: good nutrition with good handgrip strength, Group 2: good nutrition with low handgrip strength, Group 3: malnutrition with good handgrip strength, Group 4: malnutrition with low handgrip strength.
b Model 1: unadjusted.
c Model 2: Adjusted by age, cognitive impairment (MMSE < 24), polypharmacy, Barthel Index, slow gait speed (< 0.8 m/s), depressive symptoms (GDS-15≥ 5), hearing impairment, Charlson’s Comorbidity Index score.
Fig. 2. Kaplan-Meier survival curves of older adults by malnutrition and handgrip strength (HGS) status.
2014). In the present study, participants with malnutrition or low handgrip strength were at higher risk for 4-year all-cause mortality.
Fully one-third of those with malnutrition also had low handgrip strength, which increased the hazard ratio of mortality from 2.05 to 3.41. The potential interactive mechanism between malnutrition and muscle strength may be a closed-loop cyclical association. Certain bio- psycho-social factors may also affect appetite and food consumption, such as loss of taste sensation, chewing difficulties, and impairment in digestion function (Murphy, 2008;Nieuwenhuizen, Weenen, Rigby, &
Hetherington, 2010). The negative consequence of these conditions are usually compounded by physical function impairments in the ability to prepare food and psychological or cognitive impairment such as de- pression and dementia (Favaro-Moreira et al., 2016), which may in- crease the risk of co-existing malnutrition and physical decline.
4.5. Limitations
Despite our best efforts, this study still has some limitations. First, the participants were all retired male veterans living in one facility, VCH. Their characteristics were homogenous and all were male. The results of the present study might not apply to the general population.
Second, nutritional status was assessed by using MNA-SF, which might not be sensitive enough. However, Kaiser et al. didfind that MNA-SF could detect the precise nutritional condition of older adults (Kaiser et al., 2009). Third, the present study did not measure nutritional status or handgrip strength repeatedly, so that any dynamic changes in nu- tritional status or handgrip strength could not be estimated. Long- itudinal studies may yield more robustfindings.
4.6. Conclusions
Malnutrition was an independent risk factor for 4-year all-cause mortality and low handgrip strength had the synergistic effect of in- creasing the risk of mortality. A further intervention study is needed to determine the effectiveness of integrated programs for those at risk for both malnutrition and low handgrip strength, to lower the risk of ad- verse health outcomes in these older adults.
Conflict of interest
All authors declared no conflict of interest.
References
Akbar, F., & Setiati, S. (2018). Correlation between hand grip strength and nutritional status in elderly patients. Journal of Physics.
Alfaro-Acha, A., Al Snih, S., Raji, M. A., Kuo, Y. F., Markides, K. S., & Ottenbacher, K. J.
(2006). Handgrip strength and cognitive decline in older Mexican Americans. The Journals of Gerontology Series A, Biological Sciences and Medical Sciences, 61, 859–865.
Bohannon, R. W. (2001). Dynamometer measurements of hand-grip strength predict multiple outcomes. Perceptual and Motor Skills, 93, 323–328.
Campins, L., Camps, M., Riera, A., Pleguezuelos, E., Yebenes, J. C., & Serra-Prat, M.
(2017). Oral drugs related with muscle wasting and Sarcopenia. A review.
Pharmacology, 99, 1–8.
Cereda, E., Pedrolli, C., Klersy, C., Bonardi, C., Quarleri, L., Cappello, S., et al. (2016).
Nutritional status in older persons according to healthcare setting: A systematic re- view and meta-analysis of prevalence data using MNA((R)). Clinical, 35, 1282–1290.
Chapman, I. M. (2006). Nutritional disorders in the elderly. The Medical Clinics of North America, 90, 887–907.
Charlson, M. E., Pompei, P., Ales, K. L., & MacKenzie, C. R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: Development and valida- tion. Journal of Chronic Diseases, 40, 373–383.
Chen, L. K., Liu, L. K., Woo, J., Assantachai, P., Auyeung, T. W., Bahyah, K. S., et al.
(2014). Sarcopenia in Asia: Consensus report of the Asian working group for sarco- penia. Journal of the American Medical Directors Association, 15, 95–101.
Chou, M. Y., Shen, H. C., Peng, L. N., Hsu, Y. H., Liang, C. K., Liao, M. C., et al. (2019).
Underweight mobility-type pre-frailty/ frailty was associated with complex care needs of long-term care facilities residents: Results using MDS RAP triggers. Aging Medicine and Healthcare, 10, 18–23.
Chu, C.-S., Liang, C.-K., Chou, M.-Y., Lin, Y.-T., Hsu, C.-J., Chou, P.-H., et al. (2016).
Short-Form Mini Nutritional Assessment as a useful method of predicting the de- velopment of postoperative delirium in elderly patients undergoing orthopedic
surgery. General Hospital Psychiatry, 38, 15–20.
Chu, C. S., Liang, C. K., Chou, M. Y., Lu, T., Lin, Y. T., & Chu, C. L. (2017).
Mini‐Nutritional Assessment Short‐Form as a useful method of predicting poor 1‐year outcome in elderly patients undergoing orthopedic surgery. Geriatrics & Gerontology International, 17, 2361–2368.
Collin, C., Wade, D. T., Davies, S., & Horne, V. (1988). The Barthel ADL Index: A relia- bility study. International Disability Studies, 10, 61–63.
Cruz-Jentoft, A. J., Bahat, G., Bauer, J., Boirie, Y., Bruyere, O., Cederholm, T., et al.
(2019). Sarcopenia: Revised European consensus on definition and diagnosis. Age and Ageing, 48, 16–31.
Favaro-Moreira, N. C., Krausch-Hofmann, S., Matthys, C., Vereecken, C., Vanhauwaert, E., Declercq, A., et al. (2016). Risk factors for malnutrition in older adults: A sys- tematic review of the literature based on longitudinal data. Advances in Nutrition, 7, 507–522.
Flood, A., Chung, A., Parker, H., Kearns, V., & O’Sullivan, T. A. (2014). The use of hand grip strength as a predictor of nutrition status in hospital patients. Clinical Nutrition, 33, 106–114.
Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189–198.
Huskisson, E. C. (1974). Measurement of pain. The Lancet, 304, 1127–1131.
Jeejeebhoy, K. N. (2012). Malnutrition, fatigue, frailty, vulnerability, sarcopenia and cachexia: Overlap of clinical features. Current Opinion in Clinical Nutrition and Metabolic Care, 15, 213–219.
Kaiser, M. J., Bauer, J. M., Ramsch, C., Uter, W., Guigoz, Y., Cederholm, T., et al. (2009).
Validation of the Mini Nutritional Assessment short-form (MNA-SF): A practical tool for identification of nutritional status. The Journal of Nutrition, Health & Aging, 13, 782–788.
Kaiser, M. J., Bauer, J. M., Ramsch, C., Uter, W., Guigoz, Y., Cederholm, T., et al. (2010).
Frequency of malnutrition in older adults: A multinational perspective using the mini nutritional assessment. Journal of the American Geriatrics Society, 58, 1734–1738.
Kang, L., Gao, Y., Liu, X., Liang, Y., Chen, Y., Liang, Y., et al. (2019). Effects of whey protein nutritional supplement on muscle function among community-dwelling frail older people: A multicenter study in China. Archives of Gerontology and Geriatrics, 83, 7–12.
Keller, H. H., Ostbye, T., & Goy, R. (2004). Nutritional risk predicts quality of life in elderly community-living Canadians. The Journals of Gerontology Series A, Biological Sciences and Medical Sciences, 59, 68–74.
Kim, C. R., Jeon, Y. J., & Jeong, T. (2019). Risk factors associated with low handgrip strength in the older Korean population. PloS One, 14, e0214612.
Laur, C. V., McNicholl, T., Valaitis, R., & Keller, H. H. (2017). Malnutrition or frailty?
Overlap and evidence gaps in the diagnosis and treatment of frailty and malnutrition.
Applied Physiology, Nutrition, and Metabolism = Physiologie Appliquee, Nutrition et Metabolisme, 42, 449–458.
McLean, R. R., Shardell, M. D., Alley, D. E., Cawthon, P. M., Fragala, M. S., Harris, T. B., et al. (2014). Criteria for clinically relevant weakness and low lean mass and their longitudinal association with incident mobility impairment and mortality: The foundation for the National Institutes of Health (FNIH) sarcopenia project. The Journals of Gerontology Series A, Biological Sciences and Medical Sciences, 69, 576–583.
McNicholl, T., Dubin, J. A., Curtis, L., Mourtzakis, M., Nasser, R., Laporte, M., et al.
(2018). Handgrip strength, but not 5-Meter walk, adds value to a clinical nutrition assessment. Nutrition in Clinical Practice: Official Publication of the American Society for Parenteral and Enteral Nutrition.
Murphy, C. (2008). The chemical senses and nutrition in older adults. Journal of Nutrition for the Elderly, 27, 247–265.
Ngandu, T., Lehtisalo, J., Solomon, A., Levalahti, E., Ahtiluoto, S., Antikainen, R., et al.
(2015). A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. Lancet, 385, 2255–2263.
Nieuwenhuizen, W. F., Weenen, H., Rigby, P., & Hetherington, M. M. (2010). Older adults and patients in need of nutritional support: Review of current treatment options and factors influencing nutritional intake. Clinical Nutrition, 29, 160–169.
Nyunt, M. S., Fones, C., Niti, M., & Ng, T. P. (2009). Criterion-based validity and relia- bility of the Geriatric Depression Screening Scale (GDS-15) in a large validation sample of community-living Asian older adults. Aging & Mental Health, 13, 376–382.
Rantanen, T., Guralnik, J. M., Foley, D., Masaki, K., Leveille, S., Curb, J. D., et al. (1999).
Midlife hand grip strength as a predictor of old age disability. JAMA, 281, 558–560.
Rantanen, T., Volpato, S., Ferrucci, L., Heikkinen, E., Fried, L. P., & Guralnik, J. M.
(2003). Handgrip strength and cause-specific and total mortality in older disabled women: Exploring the mechanism. Journal of the American Geriatrics Society, 51, 636–641.
Ruiz, A. J., Buitrago, G., Rodriguez, N., Gomez, G., Sulo, S., Gomez, C., et al. (2018).
Clinical and economic outcomes associated with malnutrition in hospitalized pa- tients. Clinical Nutrition.
Sharkey, J. R. (2002). The interrelationship of nutritional risk factors, indicators of nu- tritional risk, and severity of disability among home-delivered meal participants. The Gerontologist, 42, 373–380.
Stessman, J., Rottenberg, Y., Fischer, M., Hammerman-Rozenberg, A., & Jacobs, J. M.
(2017). Handgrip strength in old and very old adults: Mood, cognition, function, and mortality. Journal of the American Geriatrics Society, 65, 526–532.
Verlaan, S., Ligthart-Melis, G. C., Wijers, S. L. J., Cederholm, T., Maier, A. B., & de van der Schueren, M. A. E. (2017). High prevalence of physical frailty among community- dwelling malnourished older adults-A systematic review and meta-analysis. Journal of the American Medical Directors Association, 18, 374–382.
Wei, K., Nyunt, M. S., Gao, Q., Wee, S. L., Yap, K. B., & Ng, T. P. (2018). Association of frailty and malnutrition with long-term functional and mortality outcomes among
community-dwelling older adults: Results from the Singapore longitudinal aging study 1. JAMA Network Open, 1, e180650.
Wei, K., Nyunt, M. S. Z., Gao, Q., Wee, S. L., & Ng, T. P. (2017). Frailty and malnutrition:
Related and distinct syndrome prevalence and association among community- dwelling older adults: Singapore longitudinal ageing studies. Journal of the American Medical Directors Association, 18, 1019–1028.
White, J. V., Guenter, P., Jensen, G., Malone, A., & Schofield, M. (2012). Consensus
statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: Characteristics recommended for the identification and doc- umentation of adult malnutrition (undernutrition). Journal of the Academy of Nutrition and Dietetics, 112, 730–738.
Xue, Q. L., Walston, J. D., Fried, L. P., & Beamer, B. A. (2011). Prediction of risk of falling, physical disability, and frailty by rate of decline in grip strength: The women’s health and aging study. Archives of Internal Medicine, 171, 1119–1121.