j o u r n a l h o m e p a g e : w w w . i n t l . e l s e v i e r h e a l t h . c o m / j o u r n a l s / i j m i
Online detection of potential duplicate medications and changes of physician behavior for outpatients visiting multiple hospitals using national health insurance smart cards in Taiwan
Min-Huei Hsu
a,b, Yu-Ting Yeh
c, Chien-Yuan Chen
d, Chien-Hsiang Liu
e, Chien-Tsai Liu
a,∗aGraduate Institute of Biomedical Informatics, Taipei Medical University, Taipei, Taiwan
bDivision of Neurosurgery, Taipei Medical University-Wan Fang Hospital, Taipei, Taiwan
cGraduate Institute of Medical Sciences, Taipei Medical University, Taiwan
dDepartment of Information Management, Wan-Fang Hospital, Taipei Medical University, Taipei, Taiwan
eDepartment of Healthcare Administration, Asia University, Taichung, Taiwan
a r t i c l e i n f o
Article history:
Received 5 July 2010 Received in revised form 3 November 2010
Accepted 3 November 2010
Keywords:
Duplicate medications Health smart cards CPOE systems Change Logs analysis
Anatomical Therapeutic Chemical (ATC) classification system
a b s t r a c t
Objectives: Doctor shopping (or hospital shopping), which means changing doctors (or hos- pitals) without professional referral for the same or similar illness conditions, is common in Hong Kong, Taiwan and Japan. Due to the lack of infrastructure for sharing health infor- mation and medication history among hospitals, doctor-shopping patients are more likely to receive duplicate medications and suffer adverse drug reactions. The Bureau of National Health Insurance (BNHI) adopted smart cards (or NHI-IC cards) as health cards in Taiwan.
With their NHI-IC cards, patients can freely access different medical institutions. Because an NHI-IC card carries information about a patient’s prescribed medications received from different hospitals nationwide, we used this system to address the problem of duplicate medications for outpatients visiting multiple hospitals.
Methods: A computerized physician order entry (CPOE) system was enhanced with the capa- bility of accessing NHI-IC cards and providing alerts to physicians when the system detects potential duplicate medications at the time of prescribing. Physician responses to the alerts were also collected to analyze changes in physicians’ behavior. Chi-square tests and two- sided z-tests with Bonferroni adjustments for multiple comparisons were used to assess statistical significance of differences in actions taken by physicians over the three months.
Results: The enhanced CPOE system for outpatient services was implemented and installed at the Pediatric and Urology Departments of Taipei Medical University Wan-Fang Hospital in March 2007. The “Change Log” that recorded physician behavior was activated during a 3-month study period from April to June 2007. In 67.93% of patient visits, the physicians read patient NHI-IC cards, and in 16.76% of the reads, the NHI-IC card contained at least one prescribed medication that was taken by the patient. Among the prescriptions issued
∗Corresponding author at: Tel.: +886 2 27361661x3342; mobile: +886 912556039; fax: +886 2 27339049.
E-mail address:ctliu@tmu.edu.tw(C.-T. Liu).
1386-5056/$ – see front matter © 2010 Elsevier Ireland Ltd. All rights reserved.
doi:10.1016/j.ijmedinf.2010.11.003
by physicians, on average, there were 2.36% prescriptions containing at least one medica- tion that might be duplicative to the prior prescriptions stored in NHI-IC cards. The rate of potential duplicate medication alerts for the Pediatric Department was higher than that for the Urology Department (2.78% versus 1.67%). However, the rate of revisions to prescrip- tions was higher in the Urology Department than the Pediatric Department. Overall, the rate of physicians reviewing and revising their prescriptions was 29.25%; the rate of physicians reviewing without revising their prescriptions was 43.62%; the rate of physicians turning off the alert screens right after the screens popped up (overridden) was 27.13%. Thus, physi- cians accepted alerts to review their prescriptions with patients in most situations (72.87%).
Moreover, over the study period, the rate of total revisions made to prescriptions increased and the “overridden” rate decreased. Our approach enhances the capability of CPOE sys- tems using NHI-IC cards as a nationwide infrastructure to provide more complete patient health information and medication history sharing among hospitals in Taiwan. Thus, our system can provide a better prescribing tool to help physicians detect potential duplicate medications for frequent doctor-shopping patients and hence enhance patient safety across hospital boundaries. However, the effectiveness of detecting duplicate medications with our approach is very much dependent on the completeness of NHI-IC cards, which in turn primarily depends on physician use of the cards when prescribing.
© 2010 Elsevier Ireland Ltd. All rights reserved.
1. Introduction
Doctor shopping (or hospital shopping), which means chang- ing doctors (or hospitals) without professional referral for the same or similar illness conditions, is common in East Asian countries. The prevalence of doctor shopping was nearly 40% among patients attending government outpatient depart- ments in Hong Kong[1], 23% among primary care patients in Japan[2–4], and 23.5% among outpatients in Taiwan[5–7].
Evidence shows that patients who receive medical care from multiple health care providers, particularly from different hos- pitals, are more likely to receive duplicate medications and suffer adverse drug reactions[8–11].
In Japan, a study on outpatients of a corporate health insurance society who received prescriptions from multiple medical institutes found that 8.8% of patients were prescribed duplicative medications, and the cost of the duplicated drugs was approximately 0.5–0.7% of the total drug cost in Japan [4]. In Taiwan, the incidences of duplicate medications across multiple hospitals or clinics were 6.15% for diabetic patients and 6.21% for hypertensive patients [12]. About 2% of total medications are duplicated yearly in Taiwan[12,13]. Duplicate medications may result not only in health impairment but also in increased overall cost of medical expenditure.
There have been various approaches proposed to reduce potential duplicate medications, dosing problems and drug interactions. Some suggested that patients work together with their physicians or pharmacists to review their medi- cations[14–17], while others suggested assisting physicians with prescriptions via computerized physician order entry (CPOE) systems or electronic prescription systems [18–23].
However, due to the lack of infrastructure for sharing health information and medication history across different hospitals [24,25], the proposed approaches were unlikely to be effec- tive for doctor-shopping patients. In Taiwan, the Bureau of National Health Insurance (BNHI) has adopted smart cards (or NHI-IC cards) as health cards since November 1999[26].
The infrastructure has been fully operational since the begin- ning of 2004[26–28]. Currently, there are about 23 million NHI-IC cards in use. With their NHI-IC cards, patients can freely access more than 18,000 medical institutes, including about 700 acute care hospitals and 17,000 primary care clinics nationwide. Because patient NHI-IC cards carry information about his/her prescribed medications received from different hospitals nationwide, we have used this system and imple- mented online detection of potential duplicate medications for outpatients visiting multiple hospitals. More specifically, in this study, we enhanced the capability of the CPOE system so that it can access NHI-IC cards and provide alerts to physicians when it detects a potential duplicate medication at the time of prescribing.
2. The framework of an enhanced CPOE system
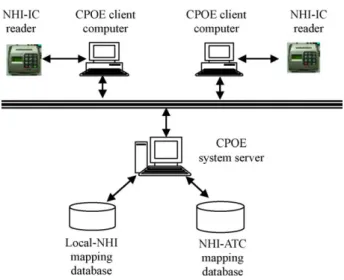
A CPOE system usually assists physicians with prescriptions, orders and results management. In our approach, the CPOE system (Fig. 1) consists of several client computers directly interacting with physicians and a system server for han- dling client requests and performing database transactions.
Currently, most CPOE systems can support the functions of detecting potential duplicate medications and drug inter- actions at a specific hospital setting. To detect potential duplicate medications for outpatients visiting multiple hospi- tals, we connected an NHI-IC card reader to a client computer and enhanced semantic interoperability between the CPOE system and NHI-IC cards.
2.1. NHI-IC cards and card readers
An NHI-IC card consists of four segments to store patient medical information. These segments are basic data, health insurance data, public health administration data (PHAD) and
Fig. 1 – An enhanced CPOE system to detect potential duplicate medications across hospital boundaries.
medical data[26,27]. The basic data segment stores the iden- tification information of the cardholder and the card itself.
The health insurance data segment is comprised of the card- holder’s insurance information and the summary of service data for insurance claims. The public health administration data segment consists of the personal health data pertain- ing to public health such as vaccination records and organ donation status. The medical data segment stores informa- tion including outpatient prescriptions, long-term (over 14 days) prescriptions, important tests and drug allergies. There are up to 60 entries for outpatient and long-term prescrip- tions. Each prescription entry consists of five fields, prescribed date, drug item (represented by an NHI code), number of days (to be taken), dosage and frequency of use. This informa- tion can be used for detecting potential duplicate medications and drug interactions when patients visit multiple hospi- tals.
The data in the NHI-IC card can be accessed and manipu- lated by a card reader, which is usually controlled by a host computer through a set of application programming inter- faces (APIs). The specifications of the card readers and APIs are open to the public, and the APIs are distributed by the BNHI at no cost. Through the common APIs and the format of the card data, the CPOE system can control the card read- ers to read/write data from/to NHI-IC cards. That is, the CPOE system can access up to 60 of the most recently prescribed medications stored in a patient’s NHI-IC card by the hospitals the patient most recently visited.
2.2. Enhancement of semantic interoperability between a CPOE system and NHI-IC cards
The prescribed medications stored in a NHI-IC card are recorded using NHI drug codes (or NHI codes for short). How- ever, a CPOE system adopted by a hospital usually contains drug codes defined by the hospital itself (or hospital codes for short). The CPOE systems may not correctly interpret the pre- scribed drugs recorded in the NHI-IC cards. Our approach to enhance the semantic interoperability is to adopt the Anatom-
ical Therapeutic Chemical (ATC) classification system as a common model for cross-mapping between NHI codes and hospital codes.
The ATC classification system is recommended by the World Health Organization (WHO) for drug utilization studies. In the ATC classification system, drugs are clas- sified in groups at five levels (from first to fifth levels) based on the organ or system on which they act and their chemical, pharmacological and therapeutic proper- ties [29]. The first level consists of fourteen anatomical main groups that are coded with one alphabetical letter.
The second and third levels are pharmacological/therapeutic subgroups coded with two digit numbers and one alpha- betical letter, respectively. The fourth level is a chemi- cal/pharmacological/therapeutic subgroup that is coded with one alphabetical, and the fifth level is the chemical substance subgroup that is coded with two digit numbers. Assign- ment of drugs to the same ATC code indicates that they are assigned to the same chemical/pharmacological/therapeutic subgroup.
Each NHI code can be assigned to a code in the ATC classi- fication system[30]. The NHI-ATC mapping database (shown inFig. 1) is used to map a NHI code to the corresponding ATC code[31]. The Local-NHI mapping database is used to map a hospital code to the corresponding NHI code. Through the Local-NHI and NHI-ATC databases, both hospital codes and NHI codes can be mapped to the corresponding ATC codes. Thus, the medications stored in NHI-IC cards can be integrated as a part of the patient’s medication history for a CPOE system to detect duplicate medications across hospital boundaries.
2.3. Online detection on potential duplicate medications using NHI-IC cards
The workflow of outpatient service for detecting potential duplicate medications across hospital boundaries is shown in Fig. 2. When acquiring an outpatient service, a patient presents his/her NHI-IC card to the doctor. The doctor operates an enhanced CPOE system to read the prescribed medications from the patient’s NHI-IC card. If medications are currently taken by the patient, then they are read and stored into a tem- porary database called CTM DB. Recall that the medications are represented by NHI codes. After making diagnosis for the patient, the doctor may prescribe medications for the patient using the CPOE system. The medications to be prescribed (if any) are stored in a database called TBPM DB, and they are represented by the hospital codes. Thus, both medications in the CTM and TBPM databases are eventually mapped to their respective ATC codes through NHI-ATC mapping and Local- NHI mapping databases, respectively, before performing the checks for duplicate medications.
Based on the ATC system, potential duplicate medications can be defined as follows:
Two medications are said to be possibly duplicative if they are in the same therapeutic/pharmacological class (i.e., their ATC codes have the same first four digits).
The algorithm to detect potential duplicate medications can be developed as shown below:
NHI-IC card
CTM DB Currently taken
medications
Begin
Any prescribed medications ?
Yes
No Diagnosis & prescription
Detection of potential duplicate medications
Prescription review & revision
Write back
Read currently taken medications from a NHI-IC card
End Any potential risks
?
Changes to prescriptions ?
NHI-IC card TBPM DB Medications to
be prescribed
Change logs Yes
No No
Yes
Fig. 2 – Online detection of potential duplicate medications across hospital boundaries.
For each medication x∈ TBPM DB, do For each medication y∈ CTM DB, do
If x and y ATC codes are the same for the first four digits, then
marked (x, y) as a potential duplicate medication pair.
End End
If there are potential duplicate medication pairs, the CPOE system signals the doctor and opens a screen for each pair displaying the drug’s brand name, the date it was ordered, the dose, and route of administration, as shown inFig. 3. The doc- tor can then review the prescription with the patient and take an appropriate action from the following:
(1) ignored, the patient did not take the medication, or ignored (not taken) for short;
(2) ignored, due to the need of patients’ conditions even though he/she is taking a potentially duplicative medica- tion, or ignored but needed for short;
(3) accepted, go back to revise the prescription, or revised for short.
However, a doctor may directly turn off the screen by click- ing the icon ( ) at the rightmost upper corner of the screen.
In this case, the action is recorded as “ignored without override reasons” or “overridden” for short. The actions taken by the doctor and the changes to the prescription are then recorded into a table called “Change Log”. Finally, all prescribed med- ications for this visit are written into the patient’s NHI-IC card.
3. Evaluating the impact of the enhanced CPOE system on physician behavior
In order to evaluate whether the alerts provided by the enhanced CPOE system for potential duplicate medication across hospitals were helpful to doctors, we implemented the system with a Change Log to record the actions taken by doctors. Each time the system signaled a potential duplicate medication alert, the prescribing physician, the department
Fig. 3 – A popup screen (translated from Chinese) showing potential duplicate medications when prescribing.
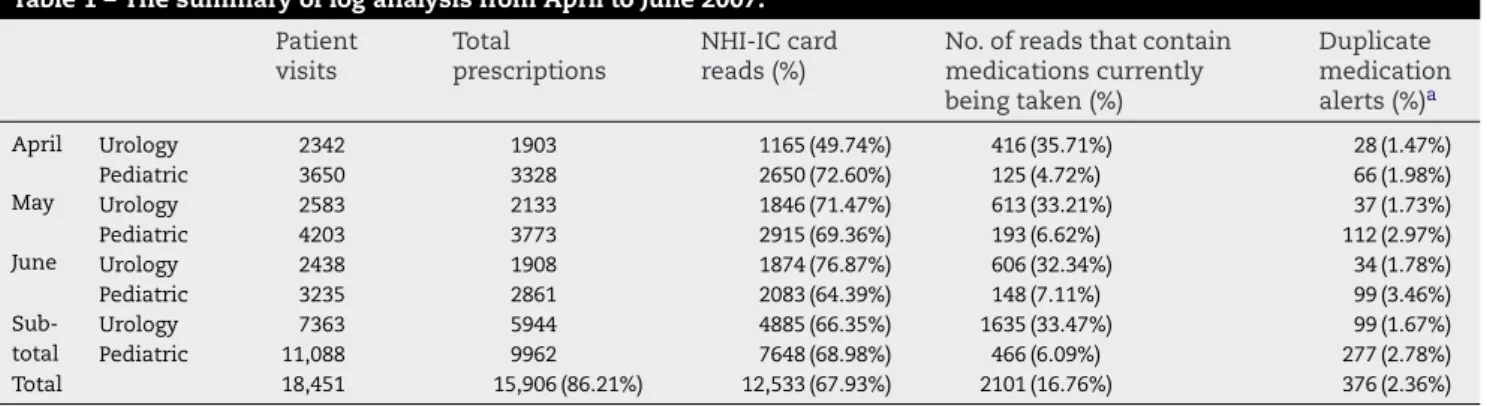
Table 1 – The summary of log analysis from April to June 2007.
Patient visits
Total prescriptions
NHI-IC card reads (%)
No. of reads that contain medications currently being taken (%)
Duplicate medication alerts (%)a
April Urology 2342 1903 1165 (49.74%) 416 (35.71%) 28 (1.47%)
Pediatric 3650 3328 2650 (72.60%) 125 (4.72%) 66 (1.98%)
May Urology 2583 2133 1846 (71.47%) 613 (33.21%) 37 (1.73%)
Pediatric 4203 3773 2915 (69.36%) 193 (6.62%) 112 (2.97%)
June Urology 2438 1908 1874 (76.87%) 606 (32.34%) 34 (1.78%)
Pediatric 3235 2861 2083 (64.39%) 148 (7.11%) 99 (3.46%)
Sub- total
Urology 7363 5944 4885 (66.35%) 1635 (33.47%) 99 (1.67%)
Pediatric 11,088 9962 7648 (68.98%) 466 (6.09%) 277 (2.78%)
Total 18,451 15,906 (86.21%) 12,533 (67.93%) 2101 (16.76%) 376 (2.36%)
a Alerts (%): the number of prescriptions containing duplicate medications÷ the total number of prescriptions issued × 100.
to which the physician belongs, the taken action, the patient, the medication order and the date and time were saved to the Change Log. The system was installed at Taipei Medical Uni- versity Wan-Fang Hospital, a teaching affiliate hospital with 750 beds, for outpatient services in March 2007. The hospi- tal has been using CPOE systems for outpatient service since 1999.
We recruited the Pediatric and Urology Departments of the hospital for the pilot study based on the fact that the physi- cians of the two departments used NHI-IC cards more often and that the two departments had a higher possibility for duplicate medications than other departments. There were three and five physicians in Pediatric and Urology Depart- ments at the time of the study, respectively. Among eight physicians, seven were male and one was female. Their aver- age age was 47.88(±10.3), and average experience in using CPOE systems was 9.13(±2.3) years.
In the first month (March) after the system was operational, we assisted each physician with becoming familiar with the new system functions. After the first month, we activated the Change Log to record physician behavior over the next three months (April to June). If the alerts were helpful, the physicians would reexamine their prescriptions and take an appropriate action, instead of closing the popup screen right after it showed up. Thus, the null hypothesis was that the physicians’ behavior in choosing their actions in responding to alerts would remain unchanged over study period (April to June.)
We used Chi-square test and two-sided z-tests with Bon- ferroni adjustments for multiple comparisons to assess the statistical significance of differences in actions taken by physicians over the three months. Level of significance was considered when p value <0.05. The statistics software used in the analysis was SPSSTM 13.0 edition (SAS Inc., Chicago, IL). This pilot study was approved by the Institutional Review Board at Wan-Fang Hospital.
4. Evaluation results
The Change Log (from April to June) was analyzed and is sum- marized inTable 1. In total, there were 18,415 patient visits over the three months, consisting of 7363 and 11,088 vis- its to Pediatric and Urology Departments, respectively. The total number of prescriptions issued by the physicians was 15,906, consisting of 5944 and 9962 prescriptions issued by Pediatric and Urology Departments, respectively. In 67.93%
(12,533) of the visits, the physicians read the patient NHI-IC cards, and in 16.76% (2101) of the reads, the NHI-IC card con- tained at least one prescribed medication that was currently being taken by the patient. Among the prescriptions issued by the physicians, there were 376 (2.36%) prescriptions con- taining at least one medication that might be duplicative to current prescriptions stored in NHI-IC cards. Thus, 376 alerts were signaled by the system for the physicians to review with their patients. The percentage of NHI-IC card reads made by the Urology Department (66.35%) was very close to that for the Pediatric Department (68.98%), but the rate of poten- tial duplicate medication alerts for the Pediatric Department (2.78%) was much higher than that for the Urology Department (1.67%).
The percentage of alerts for the Pediatric Department was 1.98% in April, increasing to 2.97% in May and 3.98% in June. On average, 2.78% of the issued prescriptions poten- tially contained at least one medication currently being taken by patients. In contrast, the percentage of potential duplicate medications for the Urology Department was stable over the three months, comprising approximately 1.7% of total issued prescriptions.
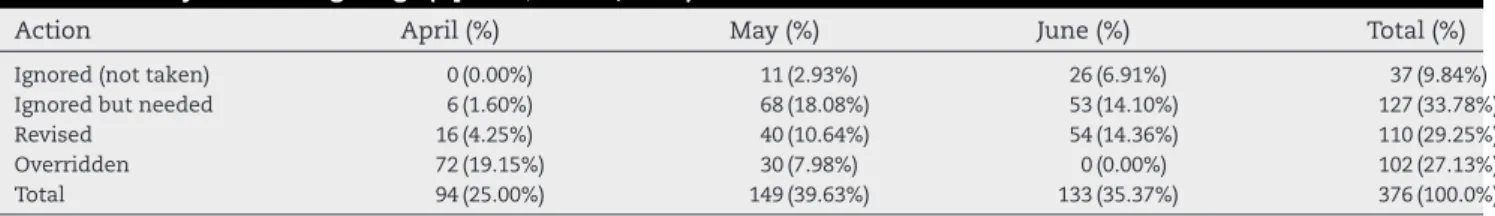
The detailed analysis of the Change Log, which recorded the actions taken by physicians on popup alert screens, is shown inTable 2. There were 376 alerts in total. 102 (27.13%) of the popup screens were overridden (ignored without override
Table 2 – Analysis of Change Logs (April 1–June 30, 1997) based on departments.
Dept. Ignored (not taken) Ignored but needed Revised Overridden Total
Pediatric 37 (13.36%) 87 (31.41%) 61 (22.02%) 92 (33.21%) 277 (100%)
Urology 0 (0.00%) 40 (40.41%) 49 (49.49%) 10 (10.10%) 99 (100%)
Total 37 (9.84%) 127 (33.78%) 110 (29.25%) 102 (27.13%) 376 (100%)
Table 3 – Analysis of Change Logs (April 1–June 30, 1997) based on months.
Action April (%) May (%) June (%) Total (%)
Ignored (not taken) 0 (0.00%) 11 (2.93%) 26 (6.91%) 37 (9.84%)
Ignored but needed 6 (1.60%) 68 (18.08%) 53 (14.10%) 127 (33.78%)
Revised 16 (4.25%) 40 (10.64%) 54 (14.36%) 110 (29.25%)
Overridden 72 (19.15%) 30 (7.98%) 0 (0.00%) 102 (27.13%)
Total 94 (25.00%) 149 (39.63%) 133 (35.37%) 376 (100.0%)
reasons) and 274 (72.87%) were reviewed by physicians with their patients before taking the following actions:
(1) 37 (13.5%) ignored the alerts because patients did not take the shown medications;
(2) 127 (46.4%) ignored due to the need of patients’ conditions;
(3) 110 (40.1%) made changes to the prescriptions after the reviews.
The rate of revisions to prescriptions for the Urology department (49.49%) was higher than that for the Pediatric department (22.02%), due to the fact that the medications prescribed by the Pediatric Department were commonly in the forms of mixed powder, liquid or syrup such as anti- histamines, bronchodilators or compound drugs for colds, making it difficult to separate the duplicate ingredient. There- fore, most pediatric physicians advised their patients not to take the previously prescribed medicines rather than to make changes to the prescriptions. During the study period, 27.13%
of alerts were overridden by physicians; 43.62% were ignored and 29.25% were revised after physicians had reviewed the prescriptions with patients. As shown inTable 3, over time, the rate of changes made to prescriptions increased and the overridden rate decreased.
We further performed Chi-Square test inTable 3 to see whether the difference in actions taken over the three months was significant.Table 4shows that Pearson Chi-Square value is 185.9964, and two-Sided asymptotic significance (Asymp. Sig.) value is 0.000 (<0.05). Hence, we can reject the null hypothesis that the physicians’ behavior in choosing actions in respond- ing to alerts would remain unchanged. Thus, we subsequently performed z-tests with Bonferroni adjustments for multiple comparisons which produce pair-wise tests of the equality of column proportions forTable 3.
The results (seeTable 5) revealed that the rate of “Ignored (not taken)” taken in June (C) was significantly greater than those taken in May (B) and in April (the cell marked by hyphen means 0). Similarly, the rate of “Ignored but needed” taken in June or in May was greater than those taken in April (A);
the rate of “Revised” taken in June was greater than those taken in May and April; the rate of “Overridden” taken in April was greater than those taken in May and June. Thus, we
Table 4 – Chi-square tests.
Value df Asymp. sig. (2-sided)
Pearson Chi-square 185.964a 6 0.000
No. of valid cases 376
a 0 cells (.0%) have expected count less than 5. The minimum expected count is 9.25.
can conclude that the physicians did properly respond to the alerts and review their prescriptions because the overridden rate decreased, and the revised rate increased over the three months.
5. Discussion
Research has shown that patients who visit multiple health care providers or hospitals might increase not only their risk of polypharmacy (concurrent use of multiple medications) but also the overall cost of medical expenditure. There have been various approaches proposed to reduce potential adverse drug reactions, specifically for duplicate medications, dosing problems and drug interactions. Early studies proposed for physicians or pharmacists to provide medication reviews to their patients[14–17]. Although comprehensive medication reviews are effective, they are very labor-intensive and costly.
Moreover, patients might forget to bring their prescriptions or fail to memorize all of their current medications. Thus this approach is not sustainable.
As an advancement in information and communication technology, computerized prescribing (ePrescribing) systems or CPOE systems have been developed. These systems allow physicians to prescribe medications and provide information regarding patient demographics, diagnosis, past illnesses and treatment history at the point of care. The systems are usually integrated with other department systems, such as labora- tory information systems, pharmacy information systems, and hospital information management systems, to provide relevant checking and timely feedback to consequently pre- vent prescription errors and reduce inappropriate drug use [18–23]. However, most CPOE systems are designed for use in a single hospital or one managed care organization set- ting and cannot perform checks on duplicate medications or drug interactions beyond the hospital boundaries, thus patient
Table 5 – Z-tests with Bonferroni adjustments for multiple comparisons of action categories.
Months
April May June
(A) (B) (C)
Options Ignored (not taken) – B
Ignored but needed A A
Revised A B
Overridden B –
Results are based on two-sided tests with significance level 0.05. For each significant pair, the key of the category with the smaller col- umn proportion appears under the category with the larger column proportion.
medication histories and health information cannot be shared across hospital boundaries.
Our approach enhances the capability of CPOE systems using NHI-IC cards as a nationwide infrastructure to share patient health information and medication histories among hospitals. In this way, our system can access a more com- plete patient medication history through the NHI-IC cards and can help physicians detect potential duplicate medications for frequent doctor-shopping patients. Our approach provides a better prescribing tool and hence enhances patient safety across hospital boundaries.
Because our approach only focused on detection of dupli- cate medications involving multiple hospitals, we did not include duplicate medications that might occur within a hos- pital setting, which are usually caught by a CPOE system. Thus, it is not surprising that the rate of potential duplicate medi- cations in our approach was 2.36%, lower than that found in other studies[4,12].
Our approach to detecting duplicate medications very much depends on the completeness of NHI-IC cards, which in turn primarily depends on physician use of the cards when prescribing. As indicated in Ref.[27], most hospitals in Taiwan are characterized by a large volume of medical services. Inclu- sion of NHI-IC cards into the medical services increases service time, and BNHI allows patients to receive medical services without their NHI-IC cards in some cases such as patient forgetting to bring NHI-IC cards or in cases of power out- age. In other words, physicians do not always use NHI-IC cards when prescribing. In fact, based on our study, physi- cians read patient NHI-IC cards in only 67.93% of patient visits (Table 1). The completeness of NHI-IC cards also depends on the medications covered by the NHI program. Based on the NHI reimbursement policy, only the medications covered by the insurance program must be written into NHI-IC cards. Self- paid medicines are not recorded on NHI-IC cards. Currently, very few medications (<5%) are not covered by the NHI pro- gram. The impact on the completeness of NHI-IC cards caused by this problem is much less important compared to physician use of NHI-IC cards.
Although about one third of the physicians did not use the enhanced CPOE system for their routine outpatient ser- vice, the system has shown its capability in detecting potential duplicate medications across hospitals. Currently, the system has been expanded to all departments of the hospital for out- patient service. In order to meet each physician’s model of service, the system was customized to allow a physician to turn on or off the function at the first time use.
6. Conclusions
Our approach enhances the capability of CPOE systems using the NHI-IC cards as a nationwide infrastructure to share patient health information and medication histories among hospitals in Taiwan so that the systems can detect potential duplicate medications for frequent doctor-shopping patients.
Thus, our approach provides a better prescribing tool to enhance patient safety across hospital boundaries. However, the effectiveness of detecting duplicate medications in our approach is very much dependent on the completeness of
Summary points
What was already known on the topic:
• Frequent doctor-shopping patients are more likely to receive duplicate medications and adverse drug reac- tions due to the lack of infrastructure for sharing health information and medication history among hospitals.
• A CPOE system usually assists physicians with pre- scriptions, orders and results management, and can provide relevant and timely checks and feedbacks to prevent prescription errors and reduce inappropriate drug use in a single hospital or one managed care orga- nization setting.
• In Taiwan, the BNHI adopted smart cards (or NHI-IC cards) as health cards in November 1999. An NHI-IC card carries information about a patient’s prescribed medications received from different hospitals nation- wide.
What this study added to our knowledge:
• Our approach enhances the capability of a CPOE sys- tem using NHI-IC cards as a nationwide infrastructure to provide more complete patient health information and medication history sharing among hospitals in Taiwan. The system can access NHI-IC cards and pro- vide alerts to physicians when it detects potential duplicate medications at the time of prescribing.
• Over the study period, physicians accepted alerts to review their prescriptions with patients in most sit- uations even though the alerts might interrupt and slow down clinical services. Moreover, the rate of total revisions made to prescriptions increased and the
“overridden” rate decreased. Thus, our approach pro- vides a better prescribing tool and hence enhances patient safety across hospital boundaries.
NHI-IC cards, which in turn primarily depends on physician use of the cards when prescribing. It is expected that a posi- tive incentive and education plan that encourages physicians to use NHI-IC cards will improve the completeness of patient NHI-IC cards. Although we did not provide the online check for adverse drug reactions[32,33], which are also potential risks for frequent doctor-shopping patients, our system can be easily extended to serve that function by including rele- vant rules and knowledge bases because the NHI-IC cards and the infrastructure are already available in Taiwan.
Author contributions
Min-Huei Hsu contributed to design of clinical workflows, sys- tem development, data collection, and manuscript writing.
Yu-Ting Yeh contributed to data analysis and interpretation, and assisted in manuscript preparation. Chien-Yuan Chen contributed to literature review, carried out programming, and
assisted in data collection and analysis. Chien-Hsiang Liu con- tributed to NHI code analysis and mapping, and coordination of research activities. Chien-Tsai Liu contributed to obtaining funding for the study, design of research methods, oversight of the study, and critical revision and final approval of the manuscript.
Competing interests
The authors report no conflict of interest.
Acknowledgements
This research was partially supported by Taipei Medi- cal University Wan-Fang Hospital under the grant number 95TMU-WFH-16. The authors express their thanks to the CPOE team of the Department of Information Systems at Wan-Fang Hospital for their technical support and thank Dr. Denis J.
Protti, Professor of Health Information Science, University of Victoria, Canada, for reviewing the paper and valuable com- ments. We also thank the anonymous reviewers and the Chief Editor Dr. Jan Talmon for their comments on earlier versions of this manuscript.
r e f e r e n c e s
[1] A.Y. Lo, A.J. Hedley, G.K. Pei, S.G. Ong, L.M. Ho, R. Fielding, et al., Doctor-shopping in Hong Kong: implications for quality of care, Int. J. Qual. Health Care 6 (4) (1994) 371–381.
[2] T. Sato, M. Takeichi, M. Shirahama, T. Fukui, J.K. Gude, Doctor-shopping patients and users of alternative medicine among Japanese primary care patients, Gen. Hosp.
Psychiatry 17 (2) (1995) 115–125.
[3] T. Sato, M. Takeichi, T. Hara, S. Koizumi, Second opinion behaviour among Japanese primary care patients, Br. J. Gen.
Pract. 49 (444) (1999) 546–550.
[4] H. Kinoshita, Y. Kobayashi, T. Fukuda, Duplicative medications in patients who visit multiple medical institutions among the insured of a corporate health insurance society in Japan, Health Policy 85 (1) (2008) 114–123.
[5] T.J. Chen, L.F. Chou, S.J. Hwang, Patterns of ambulatory care utilization in Taiwan, BMC Health Serv. Res. 6 (2006) 54–61.
[6] W.I. Lee, B.Y. Shih, Y.S. Chung, The exploration of
consumers’ behavior in choosing hospital by the application of neural network, Expert Syst. Appl. 34 (2) (2008) 806–816.
[7] M.J. Wang, S.P. Lin, Study on doctor shopping behavior:
insight from patients with upper respiratory tract infection in Taiwan, Health Policy 94 (1) (2010) 61–67.
[8] K. Schmader, J.T. Hanlon, M. Weinberger, P.B. Landsman, G.P.
Samsa, I. Lewis, et al., Appropriateness of medication prescribing in ambulatory elderly patients, J. Am. Geriatr.
Soc. 42 (12) (1994) 1241–1247.
[9] D.W. Bates, D.J. Cullen, N. Laird, L.A. Petersen, S.D. Small, D.
Servi, et al., Incidence of adverse drug events and potential adverse drug events: implications for prevention, JAMA 274 (1) (1995) 29–34.
[10] R.M. Tamblyn, P.J. McLeod, M. Abrahamowicz, R. Laprise, Do too many cooks spoil the broth? Multiple physician
involvement in medical management of elderly patients and potentially inappropriate drug combinations, CMAJ 154 (8) (1996) 1177–1184.
[11] R.P. Riechelmann, I.F. Tannock, L. Wang, E.D. Saad, N.A.
Taback, M.K. Krzyzanowsk, Potential drug interactions and duplicate prescriptions among cancer patients, J. Natl.
Cancer Inst. 99 (8) (2007) 592–600.
[12] J.T. Lai, T.W. Hou, C.L. Yeh, C.M. Chao, Using Healthcare IC Cards to manage the drug doses of chronic disease patients, Comput. Biol. Med. 37 (2) (2007) 206–213.
[13] Medications Waste and Promotion Campaigns for Returns of Expired Drugs, Health
& Medicine, United Daily News, March 6, 2008, Taipei, Taiwan.
http://mag.udn.com/mag/life/printpage.jsp?f ART ID=113990 (accessed 01.06.10).
[14] I. Schmidt, C.B. Claesson, B. Westerholm, L.G. Nilsson, B.L.
Svarstad, The impact of regular multidisciplinary team interventions on psychotropic prescribing in Swedish nursing homes, J. Am. Geriatr. Soc. 46 (1) (1998) 77–82.
[15] H.M. Fillit, R. Futterman, B.I. Orland, T. Chim, L. Susnow, G.P.
Picariello, et al., Polypharmacy management in Medicare managed care: changes in prescribing by primary care physicians resulting from a program promoting medication reviews, Am. J. Manag. Care 5 (5) (1999) 587–594.
[16] S. Meredith, P. Feldman, D. Frey, L. Giammarco, K. Hall, K.
Arnold, et al., Improving medication use in newly admitted home healthcare patients: a randomized controlled trial, J.
Am. Geriatr. Soc. 50 (9) (2002) 1484–1491.
[17] B.J. Zarowitz, L.A. Stebelsky, B.K. Muma, T.M. Romain, E.L.
Peterson, Reduction of high-risk polypharmacy drug combinations in patients in a managed care setting, Pharmacotherapy 25 (11) (2005) 1636–1645.
[18] D.W. Bates, L.L. Leape, D.J. Cullen, N. Laird, L.A. Petersen, J.M.
Teich, E. Burdick, et al., Effect of computerized provider order entry and a team intervention on prevention of serious medication errors, JAMA 280 (15) (1998) 1311– 1316.
[19] R. Tamblyn, A. Huang, R. Perreault, A. Jacques, D. Roy, J.
Hanley, et al., The medical office of the 21st century (MOXXI): effectiveness of computerized decision-making support in reducing inappropriate prescribing in primary care, CMAJ 169 (6) (2003) 549–556.
[20] R. Kaushal, K.G. Shojania, D.W. Bates, Effects of
computerized physician order entry and clinical decision support systems on medication safety: a systematic review, Arch. Intern. Med. 163 (12) (2003) 1409–1416.
[21] A. Oliven, I. Michalake, D. Zalman, E. Dorman, D. Yeshurun, M. Odeh, Prevention of prescription errors by computerized, on-line surveillance of drug order entry, Int. J. Med. Inform.
74 (5) (2005) 377–386.
[22] D.C. Classen, A.J. Avery, D.W. Bates, Evaluation and certification of computerized provider order entry systems, J. Am. Med. Inform. Assoc. 14 (2007) 48–55.
[23] J.B. Metzger, E. Welebob, F. Turisco, D.C. Classen, Effective use of medication-related decision support in CPOE, Patient Safety Qual. Healthcare 5 (5) (2008) 16–24.
[24] J. Ingenerf, J. Reiner, B. Seik, Standardized terminological services enabling semantic interoperability between distributed and heterogeneous systems, Int. J. Med. Inform.
64 (2) (2001) 223–240.
[25] M.H. Hsu, J.C. Yen, W.T. Chiu, S.L. Tsai, C.T. Liu, Y.C. Li, Using health smart cards to check drug allergy history: the perspective from Taiwan’s experiences, J. Med. Syst. (2009), doi:10.1007/s10916-009-9391-5.
[26] The Bureau of National Health Insurance, Department of Health, Taiwan, National Health Insurance Profiles.http://
www.nhi.gov.tw/english/webdata.asp?menu=11&menu id=
290&webdata id=1884(accessed 01.06.10).
[27] C.T. Liu, P.T. Yang, Y.T. Yeh, B.L. Wang, The impacts of smart cards on hospital information systems – an investigation of the first phase of the national health insurance smart card project in Taiwan, Int. J. Med. Inform. 75 (1) (2006) 173–
181.
[28] J.W. Huang, T.W. Hou, Design and prototype of a mechanism for active on-line emerging/notifiable infectious diseases control, tracking and surveillance, based on a national healthcare card system, Comput. Methods Programs Biomed. 86 (2) (2007) 161–170.
[29] WHO Collaborating Centre for Drug Statistics Methodology, Guidelines for ATC classification and DDD assignment 2008, Oslo, 2007.
[30] K.Y.H. Yang, C.W. Kuo, H.J. Hung, S.W. Jia, Classification of pharmaceutical products reimbursed by National Health Insurance by the ATC system, The Chin. Pharm. J. 54 (4) (2002) 283–290.
[31] The Bureau of Nation Health Insurance, Department of Health, Taiwan, A Query System for National Health Insurance Reimbursed Drugs.http://www.nhi.gov.tw/
inquire/query1.asp?menu=1&menu id=8(accessed 01.06.10).
[32] W. Wongpoowarak, P. Wongpoowarak, Unified algorithm for real-time detection of drug interaction and drug allergy, Comput. Methods Programs Biomed. 68 (1) (2002) 63–72.
[33] S. Bostwick, B.M. Greenwald, Impact of computerized prescriber order entry on the incidence of adverse drug events in pediatric patients, Pediatrics 120 (5) (2007) 1058–1066.