Intelligent Healthcare Support System
– A Patient-Centric Model for Safety and Protection Using Stroke as Example
Shao-Chun Chena, Pao-Cheng Leeb, Pei-Shun Hoc, Shin-Yu Jengd , P. Pete Chongd, Ronlon Tsaid aDepartment of Medicine, College of Medicine, Chang Gung University, Taoyuan.
bFarnet
Technologies co.,Ltd.
cAvances Economiques et Technologies
dDepartment and Graduate Institute
of Information Management, College of Management, Chang Gung University, Taoyuan.
B9002075@stmail.cgu.edu.tw , Jason@avectec.com.tw, mwliu@farnet.com.tw, B9144027@stmail.cgu.edu.tw, chong@mail.cgu.edu.tw , rtsai@mail.cgu.edu.tw
ABSTRACT
Background: In recent years, the focus of public health
and healthcare organizations has changed from primary critical care to prevention and caring for diseases. The proportion of senior citizens in Taiwan had reached 9.7% at 2005, and this change in the population composition has driven the bureau of national health insurance to look closer at geriatric medicine. Although there currently are quite a collection of integrated healthcare delivery systems/networks, none of them contains components of risk assessment and decision support system. This study designs a comprehensive model and provides the said components to these integrated systems.
Methods: The physiological data – which encompass
general, cardiology, and pulmonary fields -- are gathered through noninvasive procedures and devices. Information on commercial devices are gathered through www.gehealthcare.com. RFID is used to integrate wireless communication between devices and data input/output. The intelligent healthcare support system contains a database for physiological data and some diseases data, especially those in acute onset with multiple complications or life threatening conditions. This system can reduce the need of manual processing even with increased information demand.
Results: The system has been put into practice for stroke
patients. The alert for stroke-onset will be automatically sent based on patient high blood pressure, absent blood pulse, abnormal electrocardiogram, hypoventilation, fever,
obesity, and high blood glucose concentration. The information on abnormalities will be forwarded to primary caring physicians if the system deems it necessary. The physicians can then use these data to decide the next step – for example, for the patient to be admitted to the hospital for further tests – for reducing the probability of serious complications and abbreviating the length of hospital stays.
Conclusions: This system has been able to improve the
clinical and administrative efficiency. Through RFID and our intelligent support system, all physiological information can be continuously monitored to reach the goal of “ubiquitous health information environment”. This system may also be used in LTC to provide the safest and most convince service.
Key words: intelligent healthcare support system, stroke, IDSs
INTRODUCTION
During recent years, the changes in the environmental climate have led to a redefinition of the mission of a healthcare organization. The missions and goals of bureau of national health insurance have shifted from emphasizing on individual, independent illness treatments to focusing on the continuum of care, population-based wellness, and providing the appropriate care in the most efficient way. Also, from the management perspective, healthcare providers try to stretch their views to manage services across organizational boundaries, and to be responsible for continuously improving the quality of care
not only through treatment but also prevention and caring.[1] The formation of integrated healthcare delivery systems/networks (IDSs) began with hospitals reinventing themselves in order to increase their market and financial positions, enhance cost effectiveness, improve continuity of care, and respond to changing consumer preferences.[2] Under the influence of managed care, many hospitals, physicians, and outpatient facilities have consolidated their operations through integration. The number of hospital-based IDSs increased 34% from April 1995 to October 1997.[3] The current status of long-term care market (LTC) in Taiwan, at the end of 1998, the senior citizens (age≧65) reached 8.4% of the total population. It is even higher in Taipei city consisting up to 9.2%, of which, 56% are suffering from chronic illnesses, and 5.43% are unable to take care of their own daily living. In other words, almost one out of ten persons needs nursing care from others. Under the current Medicare Prospective Payment System method and the ever-changing managed care environment, the LTC information system is vital to providing quality care and to surviving in business system selection process should be an interdisciplinary effort involving all necessary stakeholders for the proposed system.[4] In the real world, however, researchers have noted that many of the “integrated systems” are systems in name only and just function as information delivery in an integrated fashion, but lack for primarily risk assessment.[5] Viewing IDSs in general, managerial experts have suggested ways to implement integration mechanisms to achieve organizational effectiveness from the viewpoint of organizational design; the recommendations included internet structure, integrated information systems, care coordination, and integrated financing.[6] Although there currently are quite a collection of integrated healthcare delivery systems/networks, none of them contains components of risk assessment and decision support system. This study designs a comprehensive model and provides the said components to these integrated systems.
METHODS
Physiological Data
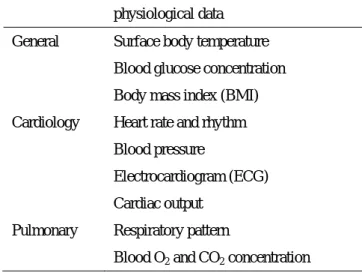
The physiological data – which encompass general, cardiology, and pulmonary fields -- are gathered through noninvasive procedures and devices. Information on commercial devices is gathered through www.gehealthcare.com. We choose some basic physiological data as our data set, including surface body temperature, blood glucose concentration, etc.[table 1] We choose these items as our minimum data set for their physiological importance and informative role.[7]
Table 1 Noninvasive physiological data in systems
physiological data
General Surface body temperature Blood glucose concentration Body mass index (BMI) Cardiology Heart rate and rhythm
Blood pressure
Electrocardiogram (ECG) Cardiac output
Pulmonary Respiratory pattern Blood O
Radio Frequency Identification (RFID)
Because the meaningful data must be continuous, the devices have to be carried by people all the time. We want these devices bother the usual life as less as possible. RFID is used to integrate wireless communication between devices and data input/output. Also, the RFID has the advantage of accuracy for long time and stable efficiency; resistance to foul environment and endurable for millions times data input/output. The most important is the small size and light weight which make them more convenience for people to carry all the time.
Intelligent Healthcare Support System
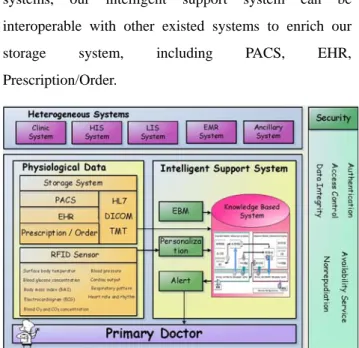
There are different types of specific physiological data expressing early in some cases of important diseases. These diseases usually have lots of complications if doctors ignore them in the early stage or life-threatening at onset.[table2] [8,9] The intelligent healthcare support system contains a database for physiological data and some diseases data, especially those in acute onset with
multiple complications or life threatening conditions. The most significant is it can remind primary doctors for the alarming data. This system can reduce the need of manual processing even with increased information demand. To get the past health record and integrate with other systems, our intelligent support system can be interoperable with other existed systems to enrich our storage system, including PACS, EHR, Prescription/Order.
Figure 1. Architecture of intelligent support system
These data communicate between these systems in the public standards, such as HL7, DICOM, and TMT. Also, the RFID sensors can detect the physiological information and send to the intelligent support system. After that, the system can personalize and customize these data with each person’s health record. In addition, the expansion of our database can combine with the evidence-based medicine database to supply the latest research data. Finally, the knowledge based system uses all above data to sum up the diseases’ risk probability. Once the system confirms the risk probability, it will send the alarm messages to the primary doctors for further following up. To secure patient privacy, we also use different types of secure mechanisms to protect the whole system.[Figure 1.]
RESULTS
We use stroke-onset as a practice in our model. The symptoms of stroke may be transient or persist for long period. Symptoms and signs remain indefinitely if the brain becomes irreversibly damaged. Unfortunately, neurologic symptoms do not accurately reflect the
presence of stroke.[10] Sudden loss of focal brain function is the core feature of the onset of stroke. In addition, people who have a stroke may present with other serious medical conditions. It is important to assess and optimize vital physiologic function before sending for an intensive study. Also, people with established coronary heart disease (CHD) have a high risk of stroke. Risk factor modification can decrease morbidity and mortality, including hypertension, body weight, and glycemic control in diabetes.[11] In people with CHD, these measures are referred to as "secondary prevention," or prevention of complications due to established disease. However, equally intensive risk factor modification is recommended in patients with a CHD risk equivalent.
Blood Pressure
The seventh Joint National Committee (JNC) report proposed the following definitions:[12]
• Normal blood pressure: systolic <120 mmHg and diastolic <80 mmHg
• Prehypertension: systolic 120-139 mmHg or diastolic 80-89 mmHg
• Hypertension: systolic 140 mmHg or diastolic 90 mmHg
People with prehypertension have higher rates of cardiovascular mortality and of progression to overt hypertension.[13] Hypertension is the most common and most important stroke risk factor. The mean arterial blood pressure is usually elevated in people with an acute stroke. An acute elevation in blood pressure often represents an appropriate response to maintain brain perfusion and a possible decline in neurologic functioning when blood pressure is lowered.
The goal blood pressure in JNC was <140/<90 mmHg, including those with cardiovascular disease alone. A lower goal (<130/<80 mmHg) was recommended only in people with diabetes and proteinuric chronic renal failure.
Heart Rate and Rhythm
Absent pulses favors a diagnosis of embolism.
Electrocardiogram
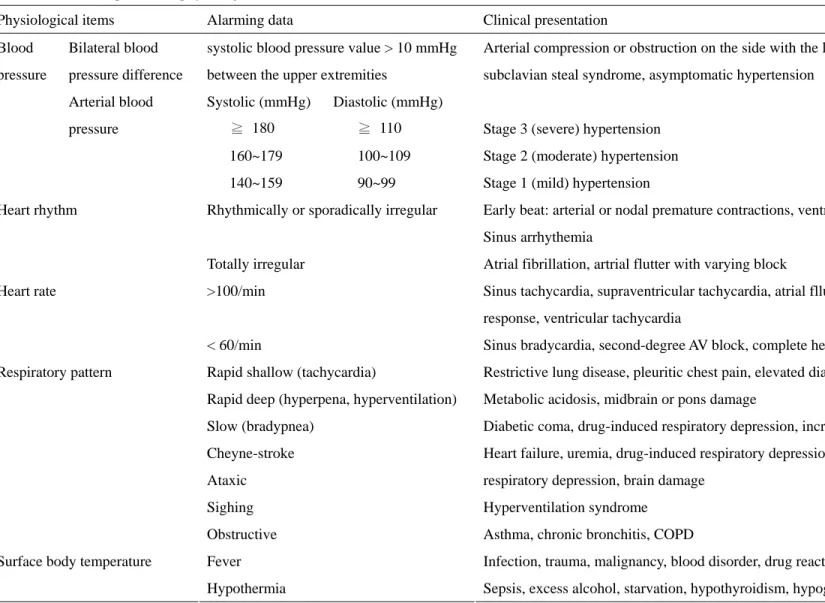
Table 2 Relationship between physiological data and diseases
Physiological items Alarming data Clinical presentation
Bilateral blood pressure difference
systolic blood pressure value > 10 mmHg between the upper extremities
Arterial compression or obstruction on the side with the lower pressure, severity of subclavian steal syndrome, asymptomatic hypertension
Blood pressure Arterial blood pressure Systolic (mmHg) Diastolic (mmHg) ≧ 180 ≧ 110 160~179 100~109 140~159 90~99
Stage 3 (severe) hypertension Stage 2 (moderate) hypertension Stage 1 (mild) hypertension
Rhythmically or sporadically irregular Early beat: arterial or nodal premature contractions, ventricular premature contractions Sinus arrhythemia
Heart rhythm
Totally irregular Atrial fibrillation, artrial flutter with varying block
>100/min Sinus tachycardia, supraventricular tachycardia, atrial flluter with a regular ventricular response, ventricular tachycardia
Heart rate
< 60/min Sinus bradycardia, second-degree AV block, complete heart block
Rapid shallow (tachycardia) Restrictive lung disease, pleuritic chest pain, elevated diaphragm Rapid deep (hyperpena, hyperventilation) Metabolic acidosis, midbrain or pons damage
Slow (bradypnea) Diabetic coma, drug-induced respiratory depression, increased intracranial pressure
Cheyne-stroke Heart failure, uremia, drug-induced respiratory depression, brain damage
Ataxic respiratory depression, brain damage
Sighing Hyperventilation syndrome
Respiratory pattern
Obstructive Asthma, chronic bronchitis, COPD
Fever Infection, trauma, malignancy, blood disorder, drug reaction, immune disorder
Surface body temperature
Hypothermia Sepsis, excess alcohol, starvation, hypothyroidism, hypoglycemia
including cardiac valvular disease, prior myocardial infarction, atrial fibrillation, and endocarditis, which increase the probability of a stroke due to embolism, earlier to decrease the complications of stroke.
Respiratory Pattern and Blood O2, CO2 Concentration
People with increased intracranial pressure (ICP) due to stroke can present with a decreased respiratory drive or muscular airway obstruction. Hypoventilation, with a resulting increase in the partial pressure of CO2, may lead to cerebral vasodilation which further elevates ICP.[14]
Surface Body Temperature
Fever may occur in people with an acute stroke and can worsen brain ischemia.[15] Normothermia should be maintained for at least the first several days after an acute stroke. Also, fever raises the suspicion of endocarditis and resulting embolic stroke
Body Mass Index
Obesity is a risk factor for CHD in both men and women.[16] Using a BMI < 21 kg/m2 as a reference, the adjusted relative risk for CHD was 1.19 at a BMI of 21 to 22.9 kg/m2, 1.46 at 23 to 24.9 kg/m2, 2.06 at 25 to 28.9 kg/m2, and 3.56 at a BMI 29 kg/m2.The relative risk of dying from cardiovascular disease at 16 years was 4.1 in women with a BMI 32 compared with <19 kg/m2.
Blood Glucose Concentration
The benefits of glycemic control on microvascular disease type 1 and type 2 diabetes were demonstrated in the Diabetes Control and Complications Trial (DCCT) and the United Kingdom Prospective Diabetes Study (UKPDS).[17]
• The DCCT trial found a nonsignificant trend toward fewer cardiovascular events with intensive therapy (3.2 versus 5.4 percent, p = 0.08).
• The primary analysis in UKPDS found no difference in macrovascular disease in the intensive and conventional therapy groups.
The information on abnormalities will be forwarded to primary caring physicians if the system deems it necessary. The physicians can use these data to decide what the next step – for example, for the patient to be
admitted to the hospital for further tests – for reducing the probability of serious complications and abbreviating the length of hospital stays.
Conclusions
Several studies have drawn on economic and organizational theories to discuss the potential benefits of an integrated system.[18] Improved clinical and administrative efficiency and fewer unneeded services; higher profits; increased market power, negotiation power and environmental acceptance; enhanced relationships with customers; and improved quality of care are the benefits commonly cited. Because of these presumed benefits from IDSs, their formation has been considered necessary to adapt to our ever-increasing healthcare costs, aging demographics, rapid advances in technology, limited human resources, and shifts of responsibility.[20] However, the quality of care in LTC facilities continues to be a national concern. Also, inadequate nurse staffing has long been blamed as the reason for quality care concerns. The solution proposed by nursing and consumer advocates is to mandate minimum staffing standards. The premise is that staffing standards will lead to quality care in LTC facilities.
Figure 2 Ubiquitous patient-centric premium healthcare
environment
No matter where you are, these devices combining with RFID can monitor your physiological information all the time to reach the goal of “ubiquitous health information environment”. Through these informative data, our intelligent support system can personalize/ customize and
integrate all your health record to establish a premium patient-centric healthcare information environment. In the future, this system can also apply in long term care of different types of chronic diseases to prevent complications happened and cost more efficiently in the national health insurance. Also, it can apply to the living-alone aged people for remote monitoring, so that their family will be at ease even not beside them.[table2]
Reference
1. Stahl, D. A., Integrated delivery system: An opportunity or a dilemma. Nurs. Manag. 26:20–23, 1995.
2. American Psychological Association, Developing an integrated delivery system, In American Psychological
Association Practice Directorate With Coopers & Lybrand, L. L. P., American Psychological Association,
Washington, DC, 1996.
3. Integrated Health care Network Top 100 Directory, SMG Market Group, and John Hancock Center, Chicago, IL, 1998.
4. Nahm ES, Mills ME, Feege B., Long-term care information systems: and overview of the selection process. J. Gerontol Nurs. Jun;32(6):32-8
5. Kuder, J. M., Belue, R., Wysong, J., and Nauenberg, E., The value of decision-making autonomy in hospital managers and its influence on contracts regarding network development and system integration. Abstr.
Book Assoc. Health Serv. Res. 15:122–123, 1998.
6. Nilson, J. T., Integration challenges: What you can do to smooth the transition. Health care Exec. 13:21–24, 1998.
7. Del Rio RA, Goldman M., Kapella BK., Sulit L., Murry PK. The accuracy of minimum data set diagnoses in describing recent hospitalization at acute care facilities. J Am Med Dri Assoc. 2006 may,7(4)212-8
8. Bickley, Lynm S. Bates’ guide to physical examination and history taking. 8th ed. 2003
9. Dennis L. Kasper, et al. Harrison’s principles of internal medicine. 16th ed.
10. Caplan, LR. Terms describing brain ischemia by tempo are no longer useful: A polemic (with apologies to Shakespeare). Surg Neurol 1993; 40:91.
11. Antman, EM, Anbe, DT, Armstrong, PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). Circulation 2004; 110:588.
12. Chobanian, AV, Bakris, GL, Black, HR, Cushman, WC. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report.
JAMA 2003; 289:2560.
13. Pastor-Barriuso, R, Banegas, JR, Damian, J, Appel, LJ. Systolic blood pressure, diastolic blood pressure, and pulse pressure: An evaluation of their joint effect on mortality. Ann Intern Med 2003; 139:731.
14. Krauss, RM, Winston, M. Obesity: Impact on cardiovascular disease. Circulation 1998; 98:1472. 15. Ginsberg, MD, Busto, R. Combating hyperthermia in
acute stroke: A significant clinical concern. Stroke 1998; 29:529.
16. Willett, WC, Manson, JE, Stampfer, MJ, et al. Weight, weight change, and coronary heart disease in women. Risk within the 'normal' weight range. JAMA 1995; 273:461.
17. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993; 329:977.
18. Conrad,D. A., and Shortell, S. M., Integrated health systems: Promise and performance. Front. Health Serv.