APAMI 2006
Proceedings
亞太醫學資訊研討會論文集
亞太醫學資訊研討會論文集
APAMI 2006 in conjunction with MIST 2006
Towards Global Interoperability for
Electronic Health Records
October 27-29, 2006
Grand Hyatt Taipei
Taipei,Taiwan
2006 APAMI Triennial Conference
Published by Taiwan Association for Medical Informatics
Copyright © 2006 by Asia Pacific Association for Medical Informatics & Taiwan Association for Medical Informatics
Printed in Taipei, Taiwan
Copyright and Reprint Permissions: Abstracting is permitted with credit to the source. Libraries are permitted to photocopy beyond the limits of copyright law for private use of patrons those articles in this volume. Instructors are permitted to photocopy isolated articles for noncommercial classroom use.
ISBN:
Contents
APAMI 2006 Committee & Information ...i
Oral Paper Presentation Schedule ...iv
Special Contributions & Asia-Pacific Regional Reports
...S1~S45
R01
U-Health Approach to the National Health Information Systems in
Korea (
KOREA)
S1
Young Moon Chae
R02
National Health Information Network Development in Korea
(
KOREA)
S9
Yoon Kim
R03 HIS Application status and trend in China. (
CHINA)
S14
Li Baoluo, Shen Tao, Chen Gi, Meng Xiaoyang
R04 Medical Informatics development in Taiwan. (
TAIWAN)
S15
Jack Li
R05
Development of Medical Informatics in Singapore -- Keeping
Pace with Healthcare Challenges. (SINGAPORE)
S16
Walter T.L. Lim
R06 EHR in Japan, -Recent Government Activities. (
JAPAN)S20
Michio Kimura
R07 eHealth trends in Pacific Islands 2006. (
JAPAN)
S22
R08 Health Informatics in the Philippines. (
PHILIPPINES)
S25
Alvin B. Marcelo
R09
Thai Medical Informatics Association and
medical informatics activity in Thailand. (
THAILAND)
S29
Wansa Paoin
R10
Health Information Management: Malaysian Experience.
(
MALAYSIA)
S31
Datin Dr.S.Selvaraju
R11
Recent Development of Health Informatics in Hong Kong. (
HONGKONG
)
S39
CP Wong
R12
Hospital-Wide Implementation of a Multi-Platform
Pharmacological Decision Support System at the Point-of-Care.
(SINGAPORE)
S41
Hui Nar Quek, Yuen Ho Chow Full Papers ... 1~265
A01
Genomic Sequence Variation Markup Language (GSVML) for
Global Interoperability of Clinical Genomics Data. (JAPAN)
1
Jun Nakaya, Michio KimuraA02
Design a pathway/genome expert system using a prolog machine
incorporated with a parallel hardware searcher. (TAIWAN)
9
Wenlung ShuA03
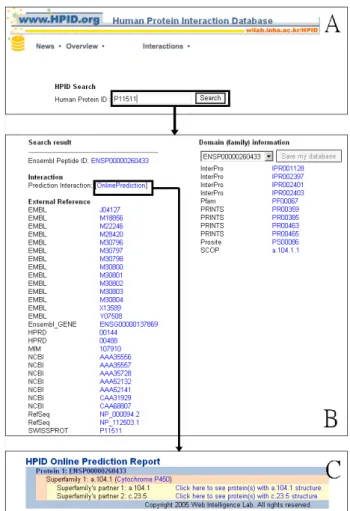
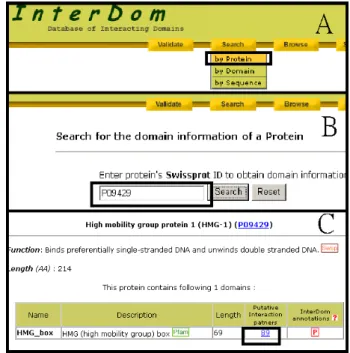
Reconstructing protein-protein interaction networks from
domain-domain interactions. (TAIWAN)
15
Ka-Lok Ng
A04 Establishment of Disease Pathway Discovery System. (
TAIWAN)
19
A05
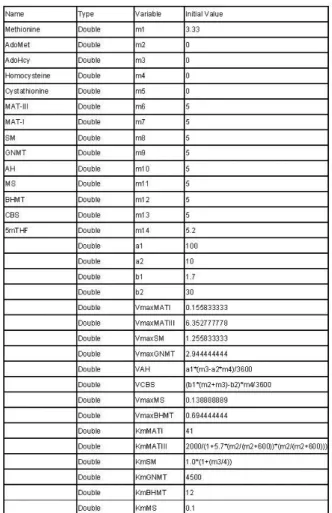
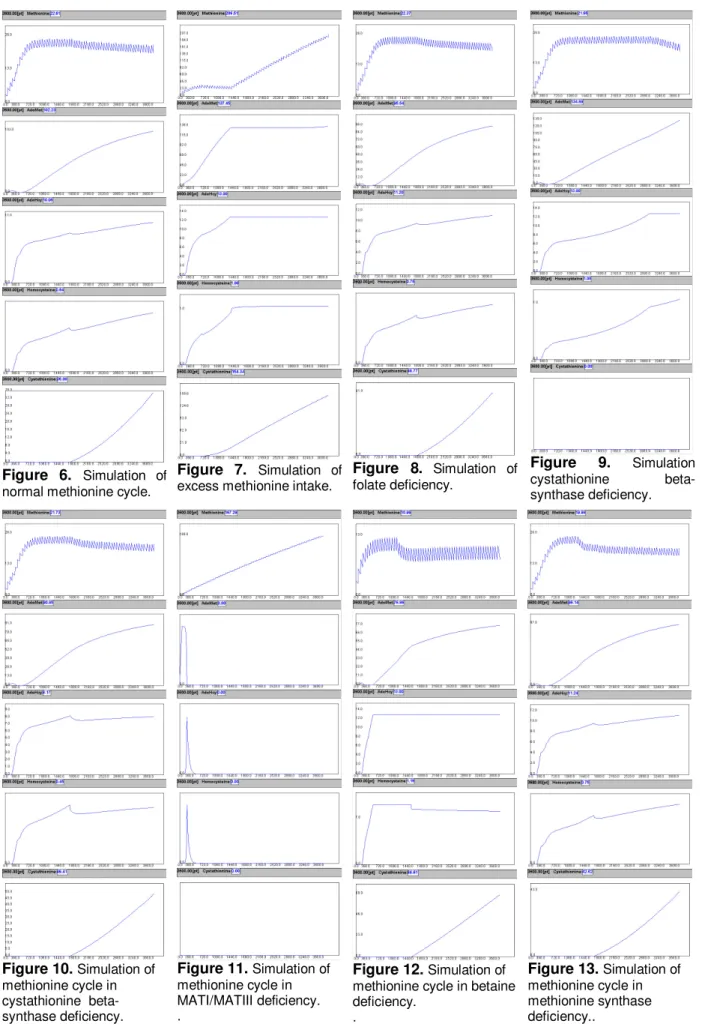
Constructing the Methionine Cycle and Its Related Disease Model
with Hybrid Functional Petri Nets. (TAIWAN)
24
Austin H Chen, Zhi En Chen
A06
Computational Methods to Uncover the Protein-Protein
Interactions. (TAIWAN)
31
Fei-Hung Hung, Hung-Wen Chiu
A07
Mutual Information correction for eddy current-induced Geometric
artefacts In Diffusion-Tensor Tractography. (TAIWAN)
36
Kao-Lun Wang, Shiou-Ping Lee, Jack Li, Wen-Yih Tseng
A08
A Virtual Bronchoscopy with Color-mapped Wall Thickness.
(KOREA)
39
Sang-joon Park, Jong Hyo Kim, Jin Mo Goo, Kwang Gi Kim, Sang Ho Lee
A09
K-means clustering approach for kinetic pattern analysis of
dynamic contrast enhancement breast MRI. (
KOREA)
45
Sang Ho Lee, Jong Hyo Kim, Kwang Gi Kim, Sang-joon Park, Woo Kyung Moon
A10 A study on the merits of Biometrics to perform e-Health. (
JAPAN)
49
Yasumitsu Tomioka, Toshihiko Kitano, Naoki Aida, Kei Kakehi, Athar SadiqMuhammad, Hiroshi Juzoji, Isao Nakajima
A11
Development of Portable Real-time Instrument for
Three-Dimensional Measurement of Scoliosis. (
TAIWAN)
54
Chung Pao Lin
A12
Diagnoses and Surgical Planning of Lung Cancer in
Color-Enhanced 3D Visualization System. (
TAIWAN)
60
Horng-Shyang Liao
A13
The use of geographic information systems(GIS) for rapid
assessment of health facilities following tsunami disaster in Aceh
province. (
INDONESIA)
68
A14
Dynamic PubMed: Automating bibliometric research using
PubMed. (
AUSTRALIA)
72
Kumara Mendis, Rasika Amarasiri
A15
Visualizing the Health Resources of Taiwan: The application of
Web_GIS. (
TAIWAN)
78
Po-Huang Chiang, Chi-Pang Wen, Yaw-Tang Shih
A16
A FORECAST MODLING AND DECSICION SUPPORT SYSTEM
FOR VACCINE DEMAND DECISION MAKING. (TAIWAN)
83
Chen k. Feng, Ruey k. Chiu
A17
Rasch Analysis Assists BNHI with Revealing Most Misfitting
Strings of Hospital Medical Service Information. (
TAIWAN)
90
Tsair Wei Chien
B01
The Design and Development of a Physician-Oriented Information
Infrastructure for the Enhancement of e-Hospital Facilities.
(
TAIWAN)
94
Hsu-Hua Ho, Tzu-Yi Yu, Hung-Pin Hou, Wen-Yung WuB02
Economic Evaluation of Japanese e-Health Systems: A
Cost-Benefit Analysis. (
JAPAN)
102
Masatsugu - Tsuji, Masaaki Teshima, Fumio Taoka
B03
Health Information on Cellphones over Wireless Application
Protocol (WAP): Issues, Obstacles, and Strategies for the
Philippines. (
PHILIPPINES)
110
Alvin B. MarceloB04
A design of ubiquitous environment for medical problem-based
learning with Web-technology. (
KOREA)
118
Cho Hune
B05
Virtual Site Visit Abroad for EMR/PACS system by Broad Banded
Teleconference system. (
JAPAN)
123
B06 A Collaborative Workspace for Telemedicine System. (
TAIWAN)
128
Hung-Wen Tung, Augustine Tsai
B07
Using TAMIS Hospital Information System to Construct a Base for
Clinical Decision Support in Schizophrenia Patients. (TAIWAN)
132
CHIUNG HSU CHENB08
Problems on a Transborder EHR System in a Disaster in
Asia-Pacific Region. (JAPAN)
138
Tanaka Takeshi
B09 Exercise Delivery Program for elder people in home. (
JAPAN)
142
Nobuyuki Ashida, Taemi Hirai, Terumasa Higasi, Makoto Fukui, Youko Ohashi
B10 Integral Medical Information Interchange with HL7 CDA. (
TAIWAN)146
Kuan Chih Lin, Ruey k. Chiu, Kuo Chin Tsai, Chia Ching HuangB11
Electronic Health Record System Evaluation Based on Patient
Safety. (
AUSTRALIA)
154
Yung-Yu Su, Khin Than Win, John FULCHER
B12
Construction and Evaluation of EHR which Supports Team
Practice. (
JAPAN)
160
Hidehiko Tsukuma
B13
System Interoperability Study for Healthcare Information System
with Web Services. (
UNITED KINGDOM)
165
Jing Kai Zhang, Wei Xu
B14
Features of Standardized Nursing Terminology Sets in Japan.
(
JAPAN)
171
Hiromi itoh Ozaku, Kaoru Sagara, Akinori Abe, Futoshi Naya, Noriaki Kuwahara, Kiyoshi Kogure
B15
Context-Based Retrieval System for Similar Medical Documents.
(
JAPAN)
177
B16
The Influence that Person's Sensibility Receives from
Mixed-Reality based on a Tanka (a traditional Japanese poem of
31 syllables). (
JAPAN)
184
Hiroshi Juzoji, Athar Sadiq Muhammad, Isao Nakajima, Yasumitsu Tomioka
B17
Evidence-Based Medicine Study between Bicycle Helmet and
Head injury. (
TAIWAN)
188
LungWen Tsai, Ten Fang Yang
B18
The effect of different height of posterior walker on gait
parameters in children with spastic diplegic cerebral palsy.
(TAIWAN)
194
Yu Ju ChihC01
Adaptable Access Control for Electronic Medical Records.
(TAIWAN)
200
Kung Chen, Yuan-Chun Chang, Da-Wei Wang
C02
MAC Address-Based Position Detection of Illegal Access
Terminals on Private Network for Hospital Asset Management.
(
JAPAN)
208
Tomohiro Kuroda, Hiroyuki Yoshihara, Naoto Kume
C03
Safeguarding clinical software – A managerial case study about
project management and oversight. (
GERMANY)
214
Wetter Thomas
C05
Expanding the role of Universal Access Fund to Rural
Telemedicine in Developing Countries. (
JAPAN)
220
Athar Sadiq Muhammad
C06
Safety Management and Crime Prevention by IC Tags–Cases of
practical use of IC tag in medical and welfare fields (JAPAN)
224
Nobuyuki Ashida, Yoshie AshidaC07
Applying Grid Computation for Evaluating Potentially
Inappropriate Medication Use in Elderly Patients. (
TAIWAN)
227
C08
Survey on Medical Error Reporting Systems in Korean Hospitals.
(
KOREA)
235
Jeongeun Kim, Sukwha Kim, David W Bates
C09 Applying Contextual Analysis on Investigating Potential. (
TAIWAN)
236
Wei Yi Fan, Chien-Yeh Hsu
C10
Handheld RFID Patient Safety Improvement – Case Study in Wan
Fang Hospital. (
TAIWAN)
241
Li Xin Xu
C11
The Requirement of Health Record to Satisfy the Patients’ Safety
Management. (
JAPAN)
249
Kiyomu Ishikawa
C12
A Study on a Nationwide Ambulance Communication System via
HEOs to Support Telemedicine. (
JAPAN)
257
Isao NAKAJIMA
C13
A Pilot Learning/Learning/Teaching System of Mammography
Screening for Radiologists. (
TAIWAN)
260
Mann-Li Chang
Supplements: Poster Abstracts ...266~279
P01
Artificial Neural Networks: A Supporting Role
In Improving Prediction Of Benign Prostatic
Obstruction Evaluated By The International
Prostate Symptom Score
Chih-Cheng Lu Jinsheng Roan Yu-jen Lee
TAIWAN
P02
A study on the Metaheuristics - apply
biologically inspired dynamic formation to
telecommunication network -
Isao NAKAJIMA JAPAN
P03
The Application and the Realization Of XML
Transform Middleware in Electronic Medical
Record
Yi Chen
Yong Feng Huang Si Fa Zhang
P04 Development of Teleconsultation System
Yuichi Ishibashi Isao NAKAJIMA Atsuko Hara
JAPAN
P05
Correlation of EEG power ratio and severity
of Alzheimer's disease
Chih-Chung Chen Chien-Yeh Hsu Hung-Wen Chiu TAIWANP06
Development of the Home-Based Multimedia
System for Mental Health Management in
adolescents via Information Superhighway
Jeongyee Bae KOREA
P07
Validating the role of “Mobile Telemedicine
Package” in Marine Time Teleconsultations.
Athar Sadiq Muhammad
JAPAN
P08
A Rough Set-Based Prediction Approach on
Medical Application
PEI CHUN Jia-Yuarn Guo Yu-Tung Dai Chung-hsiu Kuo TAIWANP09
Practical operation of a document delivery
system for medicine information, which used
a hospital web-based system in risk
management side
Hirohiko Mishima JAPAN
P10
A study of formation and storage of laboratory
results based on HL7 Clinical Document
Architecture Standard
Cho Hune KOREA
P11
The development of additional automatic
mapping protocols for local LIS system which
do not make one-to-one correspondence with
LOINC code set
Cho Hune KOREA
P12*
Design an assistive device for Parkinson's
patients with impaired balance to improve the
stride length
Tz Hau Tsuei TAIWAN
P13*
Development of Active Gait Trainer : System
Verification
Che Wen Yu TAIWANP14*
An epidemiological study on psychiatric
disorders based on the medical records of a
tertiary care hospital
Sabu K M INDIA
P15*
Building and Implementing a Comprehensive
Care Healthcare Information System –for
Mackay Memorial Hospital Medical Center
Chang Po-Ren Hsu Shih-Xin Liu Chien-Tsai
TAIWAN
APAMI2006 Organizers
Asia-Pacific Association for Medical Informatics (APAMI) Taiwan Association for Medical Informatics (TAMI)
Graduate Institute of Medical Informatics, Taipei Medical University (GIMI, TMU) Center for Biomedical Informatics, Taipei Medical University (CBI, TMU)
Health Level 7, Taiwan (HL7 Taiwan)
APAMI2006 Organizing Committee
Honorary Presidents
Conference President
Program Director
Exhibition Director
Website Director
Tour Director
Secretariat
Secretary General CIS Designer Treasurers Yun-Sik Kwak Sheng-Mou Hou Henry Chang Chung Yi Hsu Yu-Chuan (Jack) Li Ken N. Kuo Charng-Er Shyu CP Wong (HK) Ronlon TsaiHsien Ming Goh (MY) Yen-Cheng Chen
Wen-Shan Jian
Hsu-Tien (Marian) Wan Mei-Ling Huang
APAMI2006 Science Program Committee
Chair
Co-Chair
Young Moon Chae (KR) Da-Wei Wang (TW)
Chun-Por Wong (HK) Michio Kimura (JP) Steven Chu (NZ) Jin-Shin Lai (TW) Chien Yeh Hsu (TW) JiaJie Zhang(US)
Members
Klaus D Veil (AU) Yang Zhong (CN) Andre Greyling (HK) Chun-Por Wong (HK) Ngai-Tseung Cheung (HK) Saroj K. Mishra (IN) Michio Kimura (JP) Jeongeun Kim (KR) Sukwha Kim (KR) Young Moon Chae (KR) Yun Sik Kwak (KR) Hsien Ming Goh (MA) Jai Mohan (MA) Stephen Chu (NZ) Alvin B. Marcelo (PH) Herman Tolentino (PH) Rommel Palma Feria (PH)Hui Nar Quek (SG) Kwok Chan Lun (SG) Tin Wee Tan (SG) Tze Yun Leong (SG) Yuen Ho Chow (SG) Chamaree Chuapetcharasopon (TH) Nipit Pirawej (TH) Wansa Paoin (TH) Da-Dan Tang (TW) Da-Wei Wang (TW) Der-Ming Liou (TW) Ean-Wen Huang (TW) Jin-Shin Lai (TW) Li Liou (TW) Phei-Lang Chang (TW) Polun Chang (TW) Shien-Young Chang (TW) Wan-Hsuan Lin (TW) Yu-Chuan Li (TW)
APAMI Executive Committee
President
Vice-President
Secretary-General
Treasurer
Member Society
Prof. Yun Sik Kwak (KR)
Prof. Yu-Chuan (Jack) Li (TW) Dr. HM Goh (MY)
Dr. CP Wong (HK)
Australia, China (PR), Hong Kong SAR, Japan, Korea, Malaysia, New Zealand, Philippines, Singapore, Sri Lanka, Thailand, Taiwan
NPO/Government Sponsors (Taiwan)
Department of Health, Executive Yuan National Science Council
National Health Research Institutes (NHRI) Centers for Disease Control
Institute of Information Science, Academia Sinica Ministry of Foreign Affairs
Taipei City Government
Corporate Sponsors
。Phillips Taiwan (台灣飛利浦)
。FlySheet Group (飛資得資訊有限公司)
。Hewlett-Packard Development Company (台灣惠普) 。Maya International (瑪雅資訊)
。Northrop Grumman Corp.
。HaBook Information Technology INC (網奕資訊) 。Data Systems Consulting Co., Ltd (鼎新電腦) 。Lenovo
。TMT Project
Timetable of APAMI2006 Parallel Programs
**
Starting Time
Room A
Room B
Room C
Room D
(MIST)
Room E
Parallel Paper Sessions (I)
13:10 A1
B1
13:25 A2
B2
C1
M1
13:40 A3
B3
C2
M2
14:55 A4
B4
C3
M3
14:10 A5
B5
C5
M4
14:25 A6
B6
C6
M5
AP
Regional
Reports
(I)
R03~06, R10~1114:40-15:00 Coffee
Break
Parallel Paper Sessions (II)
15:00 A7
B7
C7
M6
15:15 A8
B8
C8
M7
15:30 A9
B9
C9
M8
15:45 A10
B10
C10
M9
16:00 A11
B11
C11
M10
16:15 A12
B12
C12
2006/10/28 (Sat.)
16:30-18:00 Poster
Session
Parallel Paper Sessions (III)
09:00 A13
B13
M11
09:15 A14
B14
M12
09:30 A15
B15
M13
09:45 A16
B16
M14
10:00 A17
B17
M15
10:15 A18
B18
AP
Regional
Reports (II)
R01, R02, R07~092006/10/29 (Sun.)
10:30-10:40 Coffee
Break
**Timetable shown here is subjected to change without notice, please see Conference Directory for the most accurate information.
U-Health Approach to the National Health
Information Systems in Korea
Young Moon Chae, Ph.D.
Graduate School of Public Health, Yonsei University, Seoul, Korea
Email: ymchae@yumc.yonsei.ac.kr
Abstract
This study describes the current status of computerization for hospitals and makes various recommendations to improve the level of computerization and information sharing between hospitals in order to strengthen the National Health Information System (NHIS). According to a survey of 314 out of 1,289 hospitals in August 2005, the computerization level was higher for the specialty tertiary hospitals and general hospitals than for smaller hospitals. The computerization rate by applications was 75.6% for outpatient CPOE (Computerized Physician Order Entry System), 70.6% for inpatient CPOE, 47.1% for PACS (Picture Archiving and Communication System), and 20.7% for outpatient EMR (Electronic Medical Record).
In addition, this paper also presents the NHIS plan in Korea and the survey results that examined to identify the user requirements for the electronic health record (EHR), which is a core element of NHIS. According to a survey
conducted in May 2005 of 317 people, ranging from community residents, health workers, and information systems people, most people responded that development of EHR was necessary and that they were willing to use it actively. With regard to key information included in EHR, they made the following recommendations in order: test results, health program, medical examination, immunization, allergy, information about medication and medical treatment, health behavior, genetic information, cause of death, and medical charge information. Most of the respondents wanted to apply EHR to the management of chronic diseases, but they were concerned about the security of private medical information. Based on the results, recommendations for development and implementation strategies were presented.
Keyword: national health information system,
standards, electronic health records
1. Introduction
As information technologies (IT) are rapidly improved, healthcare institutions in Korea are increasingly introducing information systems in order to improve quality of care and reduce administrative costs. There are several factors related to the increasing trends in computerization of health institutions and the increasing demand for the national health information system (NHIS). First, the proportion of the elderly population has been rapidly increasing for the last several years. The elderly population has been increasing at an annual rate of 5% and the elderly population is expected to reach about 23.9% of the total population in 2030 [1]. This rate of increase is higher than that of most OECD countries. Since elderly people place greater demand on healthcare services and resources, there is a need for information systems to support these health services and improve the efficiency in administrative activities at healthcare institutions.
Second, the legal system in Korea has been instrumental in the rapid computerization of the healthcare sector. Three application areas on e-health have been legalized in 2003: telemedicine, electronic medical record (EMR), and e-prescription system for pharmacies, which is a computerized physician order entry (CPOE) system between hospitals and
pharmacies.
Third, a major change in national hospital policy has also affected the information trend. Under the DDA (Doha Development Agenda), the Korean hospital market will be opened to foreign countries in 2007. Many Korean hospitals fear that world-class U.S. hospitals will enter the Korean market by targeting rich patients and using advanced information systems such as telemedicine and EMR. In a response to this, many Korean hospitals are developing more specialized medical services and strengthening their information systems.
Finally, advanced internet infrastructure and other IT in Korea have been a driving force for the rapid growth in computerization. The broadband uptake rate is in the top level in the world (Figure 1). In addition, Korea is also one of the top countries in the manufacture and export of PCs, computer monitors, hard disks, and other hardware.
Figure 1. Number of subscribers of high-speed internet users in Korea
Many developed countries are actively developing their NHIS according to their health delivery systems. Most countries are developing electronic health record (EHR) as the core element of their national systems [2]. EHR has been defined as a systematic and continuous aggregation of computerized information about medical treatment and individual health. The EHR system includes the information about medical treatment and health collected throughout life from birth to death, as well as family genetic information and personal information on health wellness. In the United States, hospitals at the state level are integrated to form the Local Health Information Infrastructure (LHII), which is further integrated at the national level to form the National Health Information Infrastructure (NHII). Through NHII, an integrated EHR system was developed incorporating public and private insurance. This system was managed by a committee comprised of government officials, health providers, and consumers. The EHR system is being applied to patient care, electronic prescription service, and review of insurance claims [3]. In England, the public health system was divided into 5 regions and the nationwide, unified EHR system was developed and used in all regions to support e-medical treatment reservation service, telephone consultation service, and clinic research, etc.
The Korean government developed its first
10-year national ISP (Information Strategy Plan) for NHIS in 1990, followed by the second version in 2001. The scope of the ISP was broad covering almost all activities of the Ministry of Health and Welfare (MOHW): community health information system for health centers and subcenters, hospital information systems for emergency care and blood management, national health insurance system for processing insurance claims data with a focus on EDI (Electronic Data Interchange) for data transmission, national pension system, quarantine system for imported foods, pharmaceutical information system for processing administrative drug data for KFDA (Korea Food and Drug Administration), infectious disease surveillance system and vaccination system for CDC (Center for Disease Control), national registration system for the handicapped people, and national health statistics system.
The national ISP has been a driving force for upgrading information systems for MOHW. While these information systems have greatly contributed to achieving our national goals of reducing health care costs and improving quality of healthcare, our national systems are still years behind some western countries with respect to standards, e-health related laws, EHR, and telemedicine. This paper presents some key infrastructure (standards, law, and organization), national ISP, and the survey results on EHR.
2. Current Status of
Computerization in Korean
Healthcare Institutions
2.1 Subjects
Chae et al. [4] have conducted a nationwide survey on the computerization of healthcare institutions. 314 out of 1,289 hospitals were surveyed in August 2005.
2.2 Results
2.2.1 Hospitals
As seen in Table 1, almost all specialty tertiary hospitals implement both outpatient and inpatient CPOE, PACS (Picture Archiving and Communication System), insurance claims processing, including transmitting claims data by EDI, and ADT (Admission, Discharge, and Transfer). However, only about 20% of hospitals were implementing EMR, perhaps because EMR was legalized only in 2003. It is expected that most tertiary hospitals will implement EMR by the end of 2007.
2.2.2 Clinics and Pharmacies
Most private clinics and pharmacies are implementing some form of information system. Over 90% of all clinics and pharmacies are transmitting their insurance claims via EDI network. Even before the government legalized EMR, many clinics had introduced EMR and about 85% of clinics
were implementing EMR in 2005.
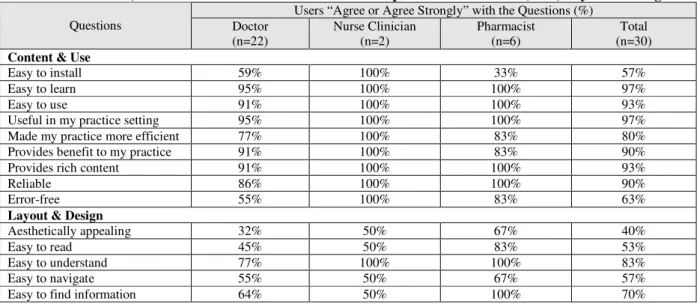
Table 1. Status of Computerization in Hospitals ( ): percentages
2.2.3 Public Healthcare Institutions
Similarly, most public healthcare institutions were implementing information systems. All community health centers were implementing CPOE and the reporting systems on infectious diseases and vaccination. The Korean government is in the process of changing client-server based public health information to web-based systems using the ASP (Application Service Provider) approach.
2.2.4 National Health Information System
This survey also included items on government policies on NHIS. Most hospitals did not introduce any form of standards on clinical terminology, perhaps due to the absence of both national standards and incentives for using international standards. Despite the government policy on information sharing among health institutions, only 15% of institutions were exchanging information for the purpose of patient referrals. Over 80% of clinics expressed negative opinion on telemedicine due to the high risk of misdiagnosis and loss of patients to large tertiary hospitals. These results have significant implications for developing and disseminating the NHIS.
3. National Health Information
Systems (NHIS ) in Korea
3.1 Information Strategy Plan (ISP)
In 2004, MOHW revised its ISP, which was comprised of three phases. In Phase 1 (2004-2005), ISP for NHIS was developed and standards and e-health related laws were developed. In Phase 2 (2006-2007), EHR and public health information systems are being developed using new standards. In Phase 3 (2008-2009), standards and EHR for health centers will be redeveloped to meet the needs
for the private health institutions.
3.2 Organization
In order to effectively carry out ISP, the MOHW created the organization. Several advisory committees were created for providing policy directions and expert opinions. Two centers were created for carrying out system development and the related researches: Center for NHIS Development and R & D Center for EHR. In addition, several working groups were created for developing the detailed activity plans for each application: telemedicine, consumer health information, and so on.
3.3 Standards
Standard is an important infrastructure for the NHIS because it allows hospitals to exchange and share patient information. In order to develop the national standards, 14 subcommittees were created in 2004: clinical terminology, dental terminology, healthcare terminology, herbal medicine terminology, medical devices, image processing, security, etc.
The committees chose the UMLS (Unified Medical Language System) developed by the NLM (National Library of Medicine) in the United States as a framework for building the Korean standards because it is internationally
accepted standards and there is no charge, which can be a big financial burden for the small hospitals in the future. Matching tables for clinical and other terminologies were created under the UMLS framework in order to develop the Korean national standards.
3.4 e-Health Law
Three revisions in the medical law enacted in 2003 greatly upgraded healthcare information systems in Korea: legalizing telemedicine, legalizing electronic medical record, and legalizing e-prescription system for outside pharmacies. However, there are needs for revising this law again. First, there is a need for providing a legal ground for NHIS. Second, there is a need for strengthening security and confidentiality of patient information. Third, there is a need for modifying some clauses related to telemedicine in order to increase its use in healthcare institutions.
Accordingly, government developed a draft of new e-Health law that includes the following elements: authorizing a creation of the Center for NHIS, including a separate Act for security and confidentiality of patient information, authorizing maintenance of EMR outside of the hospital that holds the ownership in order to allow ASP for public health information systems, and allowing tele-homecare for revisit patients.
3.5 Public Health Information Systems
The public health system in Korea is comprised of a three tier system: 250 community health centers, 1200 health subcenters, and 2000 health posts. They provide primary health services and vaccinations to community residents and collect health statistics at the grass-root level. In an effort to improve their operation and quality of services, health centers started to introduce information systems in the early 90s and now entire health centers are implementing information systems. According to the evaluation survey [5], health center information systems were effective in improving patient satisfaction and increasing the productivity of health workers.
However, updating software and providing timely hardware maintenance have been serious problems for health centers because most health centers are located in remote rural areas and suffer a lack of skilled maintenance people. Since the public health information systems are the backbone of the NHIS, the government decided to strengthen the system by converting current client-server based systems to a web-based system using the ASP approach. In addition, newly developed national standards will be applied to develop community EHR for the new public health information system.
3.6 Telemedicine
First pilot project on telemedicine was carried out from 1995 to 1998 between the Wooljin Health center and the Kyungbook University hospital using a high speed T1 telecommunication network. While this project demonstrated a possibility of providing medical consultation from a distance through network, it was not widely used as much as people anticipated because of inadequate telecommunication network and lack of financial incentives for medical doctors. While several pilot telemedicine projects have been carried out mainly at community health centers since then, most of them had a limited success in community acceptance even after telemedicine was legally allowed in 2003.
3.7 Survey on EHR
According to a survey conducted in May 2005 of 317 people, ranging from community residents, health workers, and information system people, most people responded that development of EHR was necessary and that they were willing to use it actively [6]. As a prerequisite for the development of EHR, the respondents recommended the development of a security system, standards, budgets, restructuring the legal system, obtaining community support, and telecommunication network (Table 2).
Table 2. Prerequisites for Developing EHR ( ): percentage Item Health
worker
Gov Aca Bus Res Tot Security 67 (42) 11 (31) 10 (37) 9 (26) 20 (48) 117 (39) Standard 62 (39) 20 (57) 10 (37) 17 (50) 16 (38) 125 (42) Budget 67 (42) 10 (29) 6 (22) 15 (44) 18 (43) 116 (39) Legal 50 (31) 15 (43) 12 (44) 17 (50) 14 (33) 108 (36) Support 39 (26) 10 (29) 10 (37) 7 (21) 10 (24) 76 (26) Network 28 (18) 4 (11) 4 (15) 3 (9) 6 (14) 45 (15) Total 159 35 27 34 42 297 (Gov: Government employee, Aca: Academics,
Bus: Business, Res: Community residents)
The degree of participation was the highest for those in business, followed in order by government employees, academics, health workers, community residents, and health providers. With regard to key information included in EHR, they made the following recommendations in order: test results, health program, medical examination, immunization, allergy, information about medication and medical treatment, health behavior, genetic information, cause of death, and medical charge information. Most of the respondents wanted to apply EHR to the management of
chronic diseases, but they were concerned about the security of private medical information. The majority wanted to access their own personal information through Internet after security validation.
In conclusion, the unified England EHR model was proposed for the EHR system for public health institutions in Korea based on the similarities in the public health delivery system in the two countries and the Korean nationwide registration system. In order to protect the security of private health information, we recommend using an IC security card to access EHR. In addition, we recommend organizing an EHR committee, similar to that of the United States, in order to protect against an infringement of personal information due to the monopoly of information by a single organization.
4. Conclusion
The Korean government is pushing hard with its ambitious plan for the NHIS. The factors which are critical for the success of the plan may include reliable and cost-effective IT, user-friendly application systems, standards, law, budgets, and strong support from various affected groups such as the Korean Medical Association, citizen’s group, etc. Of these, the latter four factors are rather weak areas in
Korea, compared with the technical factors, and therefore they need to be strengthened. Especially, getting support from medical community is very important factor for the success of telemedicine.
5. Reference
[1] Ministry of Health and Welfare. “National Demographic and Health Statistics”, 2003.12 [2] E. Middleton, E. Hammond, P.F. Brennan,
“Accelerating U.S. Adoption”, JAMIA, 2005; 12, pp. 13-19
[3] W.A. Yasnoff, B.L. Humphry, D.E. Detmer, “A Consensus Action Agenda for Achieving the National Health Information Infrastructure”,
JAMIA, 2004; 11, pp. 332-338
[4] Y.M. Chae, et al. Status of Computerization in Korean Health Institutions”, Health Insurance Review Agency, 2005.12
[5] Y.M. Chae, S.I. Kim, S.H. Choi, I.S. Kim, “Implementing Health Information System: Measuring Success in Korea’s Health Centers”,
International Journal of Health Planning and Management, 1994; 9, pp. 341-348
[6] G.H. Kim, Y.M. Chae, S.I. Kim, Y.E. Kim, “Study on the Korean Model for Community-based EHR”, Journal of Korea Society of
National Health Information Network Development in Korea
Yoon Kim MD, Ph.D., MS
(1)Department of Health Policy and Management,
Seoul National University College of Medicine, Seoul, Korea
(1)yoonkim@snu.ac.kr
Abstract
National level efforts have been made to adopt information and communication technologies in health care to improve the quality and safety and to reduce the costs and errors of health care in many countries. A national strategic plan, National Health Information Network, is prepared for the successful implementation of the interoperable health information technology in health care by the Ministry of Health and Welfare, Korea.
The purpose of this study is to describe how the National Health Information Network programs are developed and working in Korea. To ensure the anywhere, anytime access for anyone who wants to the lifetime electronic health record (EHR) and decision supports in secure way to improve the quality, safety and efficiency of health care by 2010, national health information standards, national health information infrastructure, lifetime electronic health record, public health information system, building consensus were the selected as NHIN programs. And the challenges faced in the process of NHIN development are discussed later.
1. Introduction
Recently the national effort is going underway to adopt information and communication technologies to improve the quality and efficiency of health care and to reduce the cost of health care in all over the world. Ever since the series of IOM reports [1, 2] were published, many countries have made an effort to improve patient safety and quality of healthcare and to reduce the healthcare costs using information technology. According to the experience of countries including UK, US, Australia and Canada, which are leading the adoption of information technology in health care, a roadmap developed with a national consensus is the most necessary work to start for the successful health information technology (HIT) adoption.
Improving quality and safety of health care and reducing the health care costs are issues in Korea as well as in others. Since the Korean government felt needs for the HIT adoption and its efficient implementation, a national strategic plan for National Health Information Network (NHIN) has been prepared by the Ministry of Health and Welfare (MOHW), Korea. The health system of Korea is required to be more efficient and effective due to the consumer needs for the good quality, safe
health care and the burden of the increasing cost of health care.
According to the recent national survey for health care consumers, 13% of people had experienced the needs for health information sharing of the past medical tests [3]. Another study showed that almost 20% of people experienced the need for laboratory information sharing from other healthcare institutions [4]. Health information sharing improves the quality of health care from the continuity of care as well as causes the decrease of cost from the tests duplications. Lab tests duplications, prescription errors, and preventable medical errors cause the high cost and low quality of health care. Another noticeable factor requiring the modernization of Korea health system is the rapidly aging society and the increasing health care costs. Aging society means the increase of chronic diseases, which are known that preventable services and self management are important.
The increasing cost of health care due to poor quality and safety, performance of health care system, and aging society are not the only problems for Korea. The benefit of national HIT adoption is estimated about 5% of national health expenditure savings and expected more [4]. The benefits of national HIT adoption may only be the estimation; however, many studies and reports prove the improvement of the performance and the quality of health care and many countries pursues the HIT adoption. National HIT adoption started already, now we are at the point to find the key factors to drive the national HIT adoption successfully.
2. National Health Information Network
Framework [5]
In 2005, the MOHW announced the vision of future healthcare, “anywhere, anytime access to electronic health records and decision supports in secure way to improve the quality, safety and efficiency of health care by 2010”. For the sake of the vision achievement, the Korean government developed a 5-year national plan for NHIN and started to carry into action. The 5-year, NHIN plan includes implementing interoperable EMRs for public hospitals and public centers and facilitating EMR adoption among private health care organizations, developing national services through the infrastructure for health information sharing, and developing the infrastructure and governing structure for NHIN as shown in Figure 1.
Figure 1 Korean NHIN Model
2.1. NHIN Programs
The development of NHIN programs is meant to be as flexible and comprehensive as possible allowing for the future changes of techniques and circumstances. The developed standards for NHIN programs define the functions enabling health care institutions following the national standards to exchange the health information and .be part of NHIN.
2.1.1. HIT adoption of public hospitals. The public
hospital covers only 10% of the total number of beds in Korea. The performance and the quality of care in public hospitals are far behind the private hospitals. The HIT adoption in public hospitals is slow and inefficient. The utilization and satisfaction rate of public hospitals and health centers is low. According to the national plan for strengthening public health system, HIT adoption in public hospitals is considered as a way for the modernization of the public health care system.
Many public hospitals are planning to adopt HIT by their own; however, most of public hospitals are faced with the lack of budget, experience and expert personnel. Not only the HIT adoption effort of public hospitals costs high, but its implementation of individual institution makes it difficult the health information share. HIT adoption effort of public hospitals will be pursued according to the national NHIN plan for the efficient and effective implementation and investment.
The one of the NHIN program for public hospital HIT adoption is to develop and deploy a standardized hospital information system, which is flexible and standardized interoperable component-based hospital information system. Standardized hospital information system will be developed following the functions enabling health information share between health institutions following the national standards. A well developed standardized hospital information system and its core technologies will be provided to private hospitals and we are expecting that HIT adoption of public hospitals and standardized hospital information implementation can boost the HIT adoption in nation wide.
2.1.2. National health information share model
Neither the data sets for health information sharing, nor the NHIN data sharing model did not earn the consensus of the public yet. However, a data share model is necessary and inevitable to support the information exchange between health systems. The national health information share model plays the role for any health care institutions to be connected to the national services and to exchange the health information only if they follow the national standards. Though the public health system is taking up only 10% of total health care system, the national health information share model is not only aimed for the information exchange of public health care systems. At the present time Center for interoperable Electronic Health Record (CiEHR) is responsible for the development of the national health information share model and to get the public consensus on the model.
Figure 2 National health information share model 2.1.3. National health information services
If the national health information share model is the technical information exchange model such as networks, national health information services are made of the services enabling the health information sharing at the national level beyond only one health care institution such as e-prescriptions. The national health information service are e-prescriptions, lifetime health records, Telehealth, image information sharing, public health, data warehouse, e-procurement, and medical knowledge base sharing. E-prescription is known effective for improving the convenience of patients and reducing errors from the handwriting prescriptions; lifetime health records for the quality of care with the continuity of care, and the self management of chronic diseases; data warehouse for health care researchers; medical knowledge database enabling the data sharing for evidence based practice; e-procurement for efficient management of health care organizations, and so on. The development of national health information services is still undergoing and need to earn the consensus from stakeholders.
National health information standards. A national
health information standard is the most critical factor for the interoperable national health information system and the health information exchange. Since National health information standards committee was organized first in 2004, now the phase three of national health information standards development has been started. 10 subcommittees started at the phase one and became 14 subcommittees at the phase three now. 14 health domains were selected for the national health information standards development and the domain experts including physicians, nurses, health information administrators, medical informaticians, etc have been participating in the standards development process. National health information standards committee adopted the Unified Medical Language System (UMLS) to create, to process, to retrieve and to integrate the national health data and information in Korea. All health data concepts collected in the first and second phases were mapped into UMLS concept. The basic principles of the health information standardization in Korea were to localize the international standards, to add the required local concepts, and to take a gradual approach. Besides the National Health Information Standards Committee, Korea Standard Organization (KSO), ISO/TC215 working groups, and other international health information standard organizations are working. The cooperation and coordination effort among health information standards organizations has been made for the efficient and successful NHIN implementation. The Figure 3 described the relationship of health information standards organizations and the strategy of collaboration.
Figure 2 Health Information standard organizations NHIN architecture. NHIN architecture is a business
and technical framework of NHIN, and the specification of functions enabling to exchange health information such as the Blueprint of Canada. NHIN architecture describes how NHIN programs are collaborating and working for the health information exchange and electronic health records. Health care organizations, health information system vendors following NHIN architecture will be able to join NHIN and to access the national health information services. This effort is made for the successful HIT adoption in Korea with the government will to provide fair opportunities to any
organizations who want to participate and to foster the many health information system vendors.
Privacy and Security. Privacy and security is the most
critical issues not only in building consensus, also in operating NHIN in real. When NHIN plan was announced by the government, privacy and security was the first concern from the public, and many organizations. Privacy and security standards are developed with a great concern by many privacy and security experts in the subcommittee of a national health information committee.
2.1.5. Governing structure
The governing structure of NHIN is developed for the purpose of efficient and effective implementation of NHIN plan. Strategic planning, law, regulation and policies, standard authentication process, organizations, and incentives and strategic investment are considered for the management purpose of NHIN. Governing structure is important as much as other components of NHIN. Currently legislations including the hospital information management, individual consent on the health information use are prepared and undergoing. National strategic plan for NHIN is prepared by the government. However, standard management process and incentives and strategic investment plans are sill remained for the further considerations.
2.2. Organizations
There are several organizations engaged in the NHIN plan to translate into action: MOHW, Health Industry Development Commission under the Office of Prime Minister, e-Health committee, Health Information Working Groups, National Health Information Standards Committees, the Center for Interoperable EHR, and etc. Some are newly established and others are to be. The coordination and cooperation among organizations are important for the efficient NHIN implementation. These are the key organizations to be described for the successful implementation of NHIN in near future.
Figure 4 Organizations for NHIN development 2.2.1. The center for interoperable EHR (CiEHR).
development and dissemination of the national architecture of NHIN and the core technologies of the standard based health information systems. It is established in the late 2005, and now actively engaged in planning NHIN and developing core technologies of standard based health information systems.
2.2.2. National health information standard committee. The national health information standard
committee was established in 2004 and has been responsible for the development, maintenance of the national health information standards. 14 domains of the vocabulary, document and technology standards were selected for the development of health information standards. The standard development process will be belonging to National health information center, and the evaluation, verification and authentication process will be the responsibilities of the National health information standards committee.
2.2.3. National health information center (NHIC).
National health information task force team, now, is the former self of NHIC. NHIC is tentative to be the main body to promote the NHIN plan and to be responsible for the development, maintenance and management, and deployment of national health information standards, and the training of skilled personnel. NHIC is in charge of all the technical supports of NHIN implementation.
3. Challenges
To build consensus. The one of the biggest
challenges for NHIN development and implementation is to build public consensus by clearing up the common misunderstandings and explaining the benefit of NHIN. There have been several projects proposed for national health information implementation for the past decade. The main reason for the program failure was again, the lack of consensus by public, health care providers, payers, policy makers, health information industries and etc. Not much difference can be found in the former projects or in the concept of health information exchange, but the circumstances shown in a global trend and the strong government will for health information technology adoption at the national level have been changed. It is the very critical time for Korea to drive strongly forward the health information technology adoption at the national level to ensure the more efficient and higher level of health care system facing the aging society. We need to focus on the development of strategies for building consensus of the society.
To increase the needs for health information standards. Another difficulty in adopting the national
health information technologies is to make people realize the needs for a national health information standard. Most of people are not aware of the importance of the standard adoption in implementing interoperable life-time electronic health records. One of
the NHIN programs, national health information standards development is not evaluated and verified the usability and feasibility of them. The pilot programs are needed to be tried as soon as possible to apply them in real life system.
To encourage the participations of consumers and health professions. The engagement of health
professions is another key factor for the successful NHIN implementation. However, the channel of participation to NHIN plan is limited to the few who are actively engaging already from the lack of general awareness. Besides the lack of health professions’ participation will, public indifference for the idea of having EHR for their convenience and consumer rights causes the ignorance of healthcare providers. There are many communication channels including public relations, seminars, public hearings, workshops, etc. Better engagement of physicians and other health professions working in real system and the public interests will lead the NHIN program to be more successful by reducing the resistance of the system users and increasing the compliance of the program.
To assure the evidence of NHIN benefits. The
evidence which NHIN implementation could bring benefits to not only for the public also for the healthcare providers is the most effective way to persuade them. The analysis of cost and benefit of NHIN implementation are rarely reported in the past. Again, the most effective method to increase the participation rate of stakeholders is to show the benefits what they can expect. More evidence studies of NHIN implementation at the national level, EMR adoptions, health information standard adoptions, and lifetime electronic health records use are required in near future.
4. Conclusion
A national strategic plan for the HIT adoption has been developed by the government initiations. With the advanced information and communication technologies of Korea and the flexible attitudes toward new technology, we can expect the synergy effect from promoting the HIT adoption by the government for health care markets.
The value of the health information exchange could be much higher than we can estimate at the current status since there are many factors we hadn’t had counted yet. However, the value of NHIN could be achieved only with the high level of HIT adoption. In addition, a nation-wide effort for the health information technology adoption is even necessary than partial or local effort by individuals. The successful HIT adoption can only be achieved when the various needs of stakeholders are considered with a comprehensive national strategic plan of NHIN and the benefit of NHIN is agreed.
[1] L.T. Kohn, J.M. Corrigan, M.S. Donaldson, and Editors, To error is human: Building a safer health
system, National Academy of Sciences, Washington,
D.C., 1999
[2] Institute of Medicine, Crossing the quality chasm: A
new health system for the 21st century, National
Academy of Sciences, Washington, D.C., 2001
[3] J. Kim, 2006 National Consumer Survey for NHIN, Seoul, Korea, 2006.
[4] Center for Information Technology Leadership, The
value of healthcare information exchange and interoperability, HIMSS, MA, US, 2004
[5] The center of interoperable EHR, The National
health information network development in Korea,
HIS Application status and trend in China
-- Summary Analyses Report based on the 2005 Survey
Li Baoluo, Shen tao,Chen qi, Meng Xiaoyang
Abstract:
Healthcare providing system reforming is puzzling the Chinese
healthcare stockholder. HIS is a powerful tool to solve the “High cost of
medication and low accessibility of healthcare” problem complained by
public.
Chinese Hospital Information Management Association (CHIMA)
launched a national survey project from February to September 2006 in
order to analyses HIS application status and trend in China. They already
collected 512 eligible responses provided by chief information officers
(CIOs)/directors of information systems at healthcare facilities who were
invited to participate via meeting, phone call and e-mail across the China.
This presentation will describe the Chinese general situation of
healthcare system, the survey purpose, methodology and several analysis
profiles: Description Statistics, Survey Respondents, IT Priorities, IT
Barriers, IT Applications, Technology Adoption, IT Budget and Staff.
This summary report should be very helpful for both the domestic
healthcare administrative officers/venders and oversea HIT vender to
understand the Chinese HIS current status, future trends, to make their
stratagem development plan and to master the HIT market requirements.
The Health Smart Cards and the National Health Informatics
Project in Taiwan
Yu-Chuan (Jack) Li, M.D., Ph.D.
1,21. Vice President, Asia Pacific Assoc for Med Info (APAMI)
2. President Emeritus, Taiwan Association for Medical Informatics (TAMI)
2. Professor and Chair, Institute of Biomedical Informatics
National Yang-Ming University, Taipei, Taiwan
Correspondence:
jackli@ym.edu.tw
The issuance of the first Health Smart Cards (HSC) from the Bureau of National Health Insurance (NHI) in the July of 2002 started a new era for personal health information exchange in Taiwan. Connected by a ubiquitous "Health Information Virtual Private Network", all the 600 hospitals, 5000 pharmacies and 17,000 clinics in Taiwan are now submitting health information to the IDC (Internet Data Center) of NHI from 40,000 card readers everyday. The HSCs are swiped through the readers 360,000,000 times a year. With visits and hospitalization information like vaccinations, diagnoses, medications and major procedures registered, the HSC has become a precursor for a nation-wide health information infrastructure.
In the end of 2005, the Department of Health initiated a 5-year plan called the National Health Informatics Project (NHIP). The NHIP is formulated in a three-layer structure, namely, the Core Architecture, the Key Applications and the Value-Added Applications.
In the Core Architecture layer, infrastructure and common platforms are laid out in 5 different component projects:
1. Information standards for Electronic Health Record and Personal Health Record
2. Ethics, legal and social impact 3. Standard platforms for health
information exchange
4. Incentives and Innovations for the Health Information Technology (HIT) industry.
5. Training and education of HIT for health professionals.
The 2nd layer of the NHIP is for the Key Applications. There are four key applications planned in this layer:
1. Evidence-based medicine and clinical decision support systems for patient safety and quality of care
2. Personal health information management system for the public 3. Integrated public health information
systems
4. Consumer health knowledge repository The 3rd layer of the NHIP is for the Value-Added Applications. There are two value-added applications planned in this layer:
1. Tele-care and U-care for chronic and home care patients
2. Establishing value-added secondary medical databases from de-identified electronic health records and national health insurance research databases With its goals set on population health, personal health, patient safety, quality of care and HIT industry, this 5-year National Health Informatics Project will hopefully become a foundation for a future health care system with better efficiency, efficacy, safety, patient-centerness, timeliness and equitability.
Development of Medical Informatics in Singapore
-- Keeping Pace with Healthcare Challenges
Walter T.L. Lim, MBBS
Association for Medical and Bio-Informatics, Singapore Correspondence: walter.t.l.lim@singhealth.com.sg
Abstract
The development of Medical Informatics in Singapore is closely intertwined with that of the overall healthcare system and has moved in concert with changing healthcare needs. This paper provides an overview of Medical informatics development in relation to key strategic directions in Singapore healthcare.
1. Introduction
In recent years, the Singapore healthcare system has had to react rapidly to the changing needs of the nation and its population. There have been several key drivers of change: fundamental shifts in national demographics and the burden of disease, the threat of emerging infectious diseases and the globalization of healthcare services.
The development of Medical Informatics in Singapore is closely intertwined with that of the overall healthcare system, and thus far has moved in concert with changing healthcare needs.
This paper provides an overview of Medical Informatics in Singapore and its development in relation to some of the key strategic directions in Singapore healthcare.
2. Overview of Singapore Health System
As with most other developed countries, the burden of disease has shifted towards non-communicable chronic illnesses: Cancer, stroke and cardiovascular diseases together account for approximately 65% of the total causes of death.
In Singapore, there is a dual system of healthcare delivery. The public system is managed by the Government while the private system is provided by the private hospitals and general practitioners. The majority of primary healthcare is provided by private practitioners, whereas the reverse is true for hospital care. Public healthcare delivery is structured into two vertically integrated healthcare clusters, namely Singapore Health Services (SHS) and National Healthcare Group (NHG).
Medical savings accounts are the cornerstone of healthcare financing. These are supplemented by Government as well as private insurance schemes. Until recently, use of funds in medical savings accounts was restricted to in-patient stays.
3. Electronic Medical Records Development 3.1. First Steps
The first hospital information systems in
Singapore were primarily administrative systems
supporting admissions/discharge and billing processes. Users of these systems were largely administrative staff and nurses.
The process of growing these systems into comprehensive electronic medical records (EMRs) has been an organic one. Initial functionality was a reflection of the system’s administrative origins: patient demographics, medical alerts and electronic discharge summaries.
In para-clinical areas, pockets of computerization have arisen independently. The implementation of such para-clinical systems (Laboratory Information Systems, Radiology Information Systems) have been facilitated by the relatively compartmentalized nature and specific scope of their related work-processes. This has provided avenues for organic growth of core EMR systems, by providing additional sources of electronic clinical data.
As such, current hospital-based EMRs have grown into the role of umbrella systems that aggregate clinically relevant electronic data from various sources.
3.2. Beyond Organic Growth
The organic model still offers room for expansion. New systems such as operating theatre management systems, e-Archival for paper-based records, web-based radiological image and ECG repositories continue to emerge, and can be integrated under the EMR umbrella.
However, with regards to clinical documentation, functionality has been relatively slow in developing. Fully electronic clinical documentation has been limited to specific clinical scenarios i.e. Emergency Medicine Departments, Armed Forces Outpatient Services.
To address this, the two healthcare clusters have taken steps to engage commercial vendors in the development of the next generation of EMRs. The distinguishing feature of these next generation systems is a ground-up attempt to incorporate clinical workflows such as computerized physician order entry (CPOE), clinical results tracking and nursing records. This has necessitated deeper involvement on the part of healthcare users, which could be seen as a co-development role.