DOI: 10.1016/j.athoracsur.2009.06.002
http://ats.ctsnetjournals.org/cgi/content/full/88/4/1124
located on the World Wide Web at:
The online version of this article, along with updated information and services, is
Print ISSN: 0003-4975; eISSN: 1552-6259.
Southern Thoracic Surgical Association. Copyright © 2009 by The Society of Thoracic Surgeons.
is the official journal of The Society of Thoracic Surgeons and the
Risk Factors for 24-Hour Mortality After Traumatic
Rib Fractures Owing to Motor Vehicle Accidents:
A Nationwide Population-Based Study
Yung-Chang Lien,
MD,
Chao-Hung Chen,
MD, MPH,
and Herng-Ching Lin,
PhD
Division of Thoracic Surgery, Department of Surgery, Taipei Medical University and Hospital, Department of Thoracic Surgery, Mackay Memorial Hospital, Mackay Medicine, Nursing, and Management College, and School of Health Care Administration, Taipei Medical University, Taipei, Taiwan
Background. Accurate identification of patients at
high risk of death as a result of major chest trauma is essential within a trauma system. We used 3-year population-based data in Taiwan to evaluate risk fac-tors associated with 24-hour mortality among adults with obvious rib fractures and needing hospitalization after traffic accidents.
Methods. Pooled data from Taiwan’s National Health
Insurance Research Database for the years 2002 through 2004 were used. A total of 18,856 patients hospitalized with rib fractures after traffic accidents were included. Multivariate logistic regression using generalized esti-mating equations was performed to explore the relation-ship between 24-hour mortality and patients’ age, sex, and comorbid conditions, as well as hospital characteris-tics, adjusting for social factors and any clustering of the sampled patients by hospital.
Results. Of patients in the sample, 459 (2.4%) died
within 24 hours of admission. Patients who had six or
more rib fractures were three times more likely to die within 24 hours of admission compared with patients with only one rib fracture (odds ratio [OR], 3.16; p < 0.001). The adjusted odds of death within 24 hours were higher for patients who had hemopneumothorax (OR, 3.15; p < 0.001), extremity fractures (OR, 1.74; p < 0.001), pelvic fractures (OR, 2.92; p < 0.001), head injuries (OR, 4.29; p < 0.001), spleen injury (OR, 1.83; p < 0.05), hepatic injury (OR, 4.39; p < 0.001), heart injury (OR, 4.48; p < 0.001), and diaphragm injury (OR, 3.16; p < 0.05) com-pared with patients who had none of these injuries.
Conclusions. We concluded that more than six ribs
fractured, heart injuries, hepatic injuries, head inju-ries, and advanced age are the most important deter-minants of 24-hour mortality after thoracic trauma from traffic accidents.
(Ann Thorac Surg 2009;88:1124 –30) © 2009 by The Society of Thoracic Surgeons
T
rauma is the leading cause of death in the first four decades of life[1]. Thoracic traumas constitute 10% to 15% of all traumas and are the cause of death in 25% of all fatalities attributable to trauma[2]. Blunt chest inju-ries particularly attract attention because of the increas-ing incidence of traffic accidents. Although most chest wall injuries are benign and can be followed up without hospitalization, trauma associated with the thoracic cage may cause profound, sometimes fatal pathophysiologic changes[3].Blunt trauma from motor vehicle crashes accounts for 70% to 80% of thoracic injuries[4]. Thoracic trauma may include injury to the chest wall, pleura, tracheobronchial tree, lungs, diaphragm, esophagus, heart, and major blood vessels, and may be associated with other major organ injuries. Initially these patients are usually trans-ported from the accident site to the nearest available hospital. According to a study by Acosta and colleagues
[5], 70% of trauma victims die within the first 24 hours of
admission. It is essential for any trauma system to accu-rately identify patients at highest risk of mortality as a result of major chest trauma.
We therefore used 3-year population-based data in Taiwan to evaluate the possible risk factors for 24-hour mortality in adults who had experienced traffic accidents and had obvious rib fractures and needed hospitaliza-tion. In addition to thoracic trauma and associated inju-ries, our study examined the association between hospi-tal characteristics and 24-hour morhospi-tality for adults with blunt chest injuries attributable to traffic accidents.
Material and Methods
Database
This study uses pooled data for the years 2002, 2003, and 2004 obtained from the National Health Insurance Re-search Database published by Taiwan’s National Health Research Institute. The National Health Insurance Re-search Database covers all medical benefit claims for approximately 98% of the entire Taiwan population. The National Health Insurance Research Database also in-cludes a registry of contracted medical facilities, a regis-try of board-certified surgeons, and details of orders and Accepted for publication June 1, 2009.
Address correspondence to Dr Lin, School of Health Care Administration, Taipei Medical University, 250 Wu-Hsing St, Taipei, 110, Taiwan; e-mail: henry11111@tmu.edu.tw.
expenditures on prescriptions dispensed at contracted pharmacies. It also provides principal procedure codes along with one principal diagnosis code, and up to four secondary diagnosis codes for each patient, using the International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM). The validity of diag-noses is usually a concern with claims data sets. Thus, the Bureau of National Health Insurance carries out routine sampling of patient charts to crosscheck with each hos-pital’s claims, followed by punitive measures for fraud-ulent coding. This deterrent is further boosted by the National Health Insurance’s reimbursement system, which ties a hospital’s reimbursement rate to its patient severity profile. It is generally believed that the National Health Insurance’s checks and balances promote accu-rate coding.
In our data set, all personal identifiers were encrypted before release for public access for research purposes by the Bureau of National Health Insurance. After consult-ing the institutional review board director of our univer-sity, the study was exempt from full review by the institutional review board board, as only unidentified secondary data were used.
Study Sample
The study sample was identified by a diagnosis of rib fracture (ICD-9-CM code 807, 807.0, or 807.1). Of more
than eight million inpatient records within the data set covering the period of this study, 34,081 were admitted because of rib fractures. We then excluded sampled patients whose rib fractures were not caused by traffic accidents (n ⫽ 15,093). We also excluded all 30-day readmissions for the treatment of rib fractures, regarding these as the same episode as the first-time admission
(n⫽ 4). In addition, children’s ribs are more flexible in
nature compared with those of adults, which may lead to different consequences after thoracic trauma. For exam-ple, children experiencing simple trauma may have inju-ries to the intrathoracic viscera rather than rib fractures
[6]. Therefore, all patients younger than 18 years of age (n⫽ 122) were excluded from the data set. Ultimately, our study sample consisted of 18,856 patients.
Key Variables of Interest
The primary study outcome was dichotomous: whether or not a patient was dead within 24 hours after admis-sion. For this study, the National Health Insurance Re-search Database was linked to the “cause of death” data file by the patient’s national identification number with the assistance of the Department of Health in Taiwan. Because the registration of all deaths is mandatory, the data are considered to be very accurate and comprehen-sive. This linkage allowed us to identify all deaths occur-ring within 24 hours of hospitalization. The independent
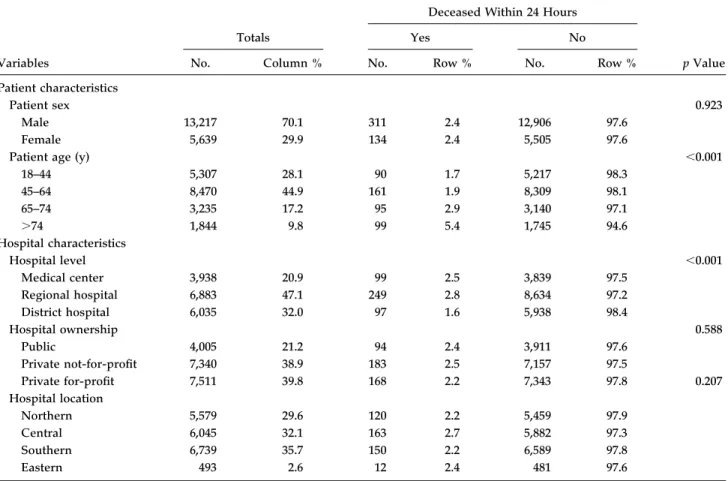
Table 1. Distribution of Patient and Hospital Characteristics for Cases With Traumatic Rib Fractures After Traffic Accidents in Taiwan, 2002–2004 (n⫽ 18,856)
Variables
Totals
Deceased Within 24 Hours
p Value
Yes No
No. Column % No. Row % No. Row %
Patient characteristics
Patient sex 0.923
Male 13,217 70.1 311 2.4 12,906 97.6
Female 5,639 29.9 134 2.4 5,505 97.6
Patient age (y) ⬍0.001
18–44 5,307 28.1 90 1.7 5,217 98.3 45–64 8,470 44.9 161 1.9 8,309 98.1 65–74 3,235 17.2 95 2.9 3,140 97.1 ⬎74 1,844 9.8 99 5.4 1,745 94.6 Hospital characteristics Hospital level ⬍0.001 Medical center 3,938 20.9 99 2.5 3,839 97.5 Regional hospital 6,883 47.1 249 2.8 8,634 97.2 District hospital 6,035 32.0 97 1.6 5,938 98.4 Hospital ownership 0.588 Public 4,005 21.2 94 2.4 3,911 97.6 Private not-for-profit 7,340 38.9 183 2.5 7,157 97.5 Private for-profit 7,511 39.8 168 2.2 7,343 97.8 0.207 Hospital location Northern 5,579 29.6 120 2.2 5,459 97.9 Central 6,045 32.1 163 2.7 5,882 97.3 Southern 6,739 35.7 150 2.2 6,589 97.8 Eastern 493 2.6 12 2.4 481 97.6 GENERAL THORACIC
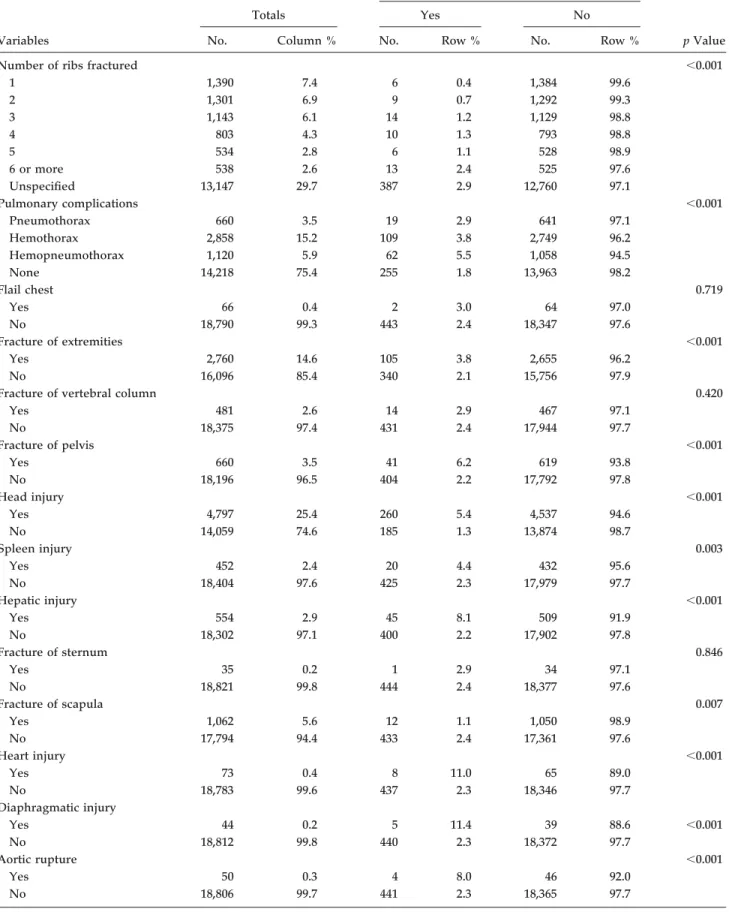
Table 2. Distribution of Comorbidities Among Patients With Traumatic Rib Fractures After Traffic Accidents in Taiwan, 2002– 2004 (n⫽ 18,856)
Variables
Totals
Deceased Within 24 Hours
p Value
Yes No
No. Column % No. Row % No. Row %
Number of ribs fractured ⬍0.001
1 1,390 7.4 6 0.4 1,384 99.6 2 1,301 6.9 9 0.7 1,292 99.3 3 1,143 6.1 14 1.2 1,129 98.8 4 803 4.3 10 1.3 793 98.8 5 534 2.8 6 1.1 528 98.9 6 or more 538 2.6 13 2.4 525 97.6 Unspecified 13,147 29.7 387 2.9 12,760 97.1 Pulmonary complications ⬍0.001 Pneumothorax 660 3.5 19 2.9 641 97.1 Hemothorax 2,858 15.2 109 3.8 2,749 96.2 Hemopneumothorax 1,120 5.9 62 5.5 1,058 94.5 None 14,218 75.4 255 1.8 13,963 98.2 Flail chest 0.719 Yes 66 0.4 2 3.0 64 97.0 No 18,790 99.3 443 2.4 18,347 97.6 Fracture of extremities ⬍0.001 Yes 2,760 14.6 105 3.8 2,655 96.2 No 16,096 85.4 340 2.1 15,756 97.9
Fracture of vertebral column 0.420
Yes 481 2.6 14 2.9 467 97.1 No 18,375 97.4 431 2.4 17,944 97.7 Fracture of pelvis ⬍0.001 Yes 660 3.5 41 6.2 619 93.8 No 18,196 96.5 404 2.2 17,792 97.8 Head injury ⬍0.001 Yes 4,797 25.4 260 5.4 4,537 94.6 No 14,059 74.6 185 1.3 13,874 98.7 Spleen injury 0.003 Yes 452 2.4 20 4.4 432 95.6 No 18,404 97.6 425 2.3 17,979 97.7 Hepatic injury ⬍0.001 Yes 554 2.9 45 8.1 509 91.9 No 18,302 97.1 400 2.2 17,902 97.8 Fracture of sternum 0.846 Yes 35 0.2 1 2.9 34 97.1 No 18,821 99.8 444 2.4 18,377 97.6 Fracture of scapula 0.007 Yes 1,062 5.6 12 1.1 1,050 98.9 No 17,794 94.4 433 2.4 17,361 97.6 Heart injury ⬍0.001 Yes 73 0.4 8 11.0 65 89.0 No 18,783 99.6 437 2.3 18,346 97.7 Diaphragmatic injury Yes 44 0.2 5 11.4 39 88.6 ⬍0.001 No 18,812 99.8 440 2.3 18,372 97.7 Aortic rupture ⬍0.001 Yes 50 0.3 4 8.0 46 92.0 No 18,806 99.7 441 2.3 18,365 97.7 THORACIC
variables of interest were patient’s age (18 to 44, 45 to 64, 65 to 74, and ⬎74 years), sex, and comorbidities, and hospital characteristics. Comorbidities included pulmo-nary complications (pneumothorax [ICD-9-CM code 860.0 or 860.1], hemothorax [ICD-9-CM code 860.2 or 860.3], pneumohemothorax [ICD-9-CM code 860.4 or 960.5]), flail chest (ICD-9-CM code 807.4), extremity frac-ture (ICD-9-CM codes 812 through 828), vertebral col-umn fracture (ICD-9-CM codes 805 through 806), pelvis fracture 9-CM code 808), sternum fracture 9-CM codes 807.2 through 807.3), scapula fracture (ICD-9-CM code 811), head injury (ICD-(ICD-9-CM codes 800 through 804 or 851 through 854), spleen injury (ICD-9-CM code 865), hepatic injury (ICD-(ICD-9-CM code 864), heart injury (ICD-9-CM codes 861.0 through 861.1), and diaphragmatic injury (ICD-9-CM codes 862.0 through 862.1).
Hospital characteristics included hospital ownership, accreditation level, and geographic location, with the hospital ownership variable being recorded as one of three types: public, private not-for-profit, and private for-profit hospitals. Within the variable of hospital ac-creditation level, each hospital was classified as a medical center (with a minimum of 500 beds), a regional hospital (minimum 250 beds), or a district hospital (minimum 20 beds); hospital level can therefore be used as a proxy for both hospital size and clinical service capabilities. Hos-pital teaching status was not included in this study as all medical centers and regional hospitals in Taiwan are teaching hospitals.
Statistical Analysis
The SAS statistical package (SAS System for Windows, Version 8.2; SAS Institute Inc, Cary, NC) was used to perform analysis of the data. Descriptive analyses, in-cluding frequency, percentage, mean, and standard de-viation, were performed on the identified variables. Global2
analyses were conducted to examine the rela-tionships between 24-hour death and independent vari-ables of interest. Multivariate logistic regression using generalized estimating equations was also performed to explore the relationship between 24-hour death and patient’s age, sex, and comorbidities, as well as hospital characteristics, after adjusting for other factors and any clustering of the sampled patients among particular hospitals. A two-sided probability value of less than or equal to 0.05 was considered statistically significant.
Results
Table 1describes the distribution of the sampled patients by patient demographics and hospital characteristics. Of the total 18,856 patients hospitalized for rib fractures during the 3-year study period, 70.1% were male, and the mean age of the patients was 53.6 years (standard devi-ation, 15.6 years).
Among the study sample, 459 patients (2.4%) were dead within 24 hours after admission, contributing to 55% of all 30-day mortalities (n ⫽ 827). Table 1 also presents the bivariate analyses of patient and hospital
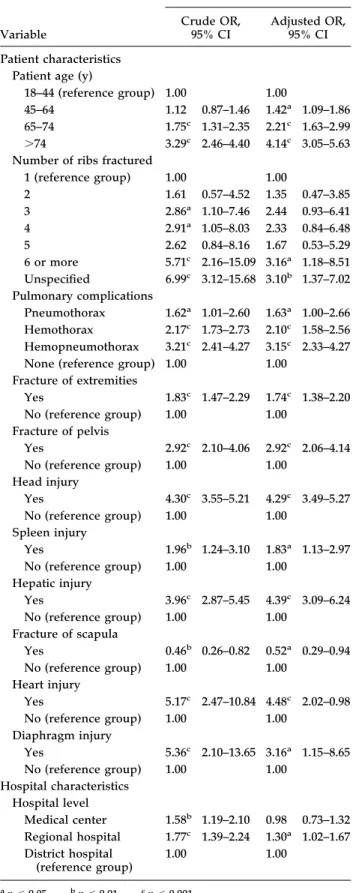
Table 3. Crude and Adjusted Odds Ratios for 24-Hour Death in Taiwan, by Patient and Hospital Characteristics, 2002–2004 (n⫽ 18,856)
Variable
Deceased Within 24 Hours Crude OR,
95% CI
Adjusted OR, 95% CI Patient characteristics
Patient age (y)
18–44 (reference group) 1.00 1.00
45–64 1.12 0.87–1.46 1.42a 1.09–1.86
65–74 1.75c 1.31–2.35 2.21c 1.63–2.99 ⬎74 3.29c 2.46–4.40 4.14c 3.05–5.63
Number of ribs fractured
1 (reference group) 1.00 1.00 2 1.61 0.57–4.52 1.35 0.47–3.85 3 2.86a 1.10–7.46 2.44 0.93–6.41 4 2.91a 1.05–8.03 2.33 0.84–6.48 5 2.62 0.84–8.16 1.67 0.53–5.29 6 or more 5.71c 2.16–15.09 3.16a 1.18–8.51 Unspecified 6.99c 3.12–15.68 3.10b 1.37–7.02 Pulmonary complications Pneumothorax 1.62a 1.01–2.60 1.63a 1.00–2.66 Hemothorax 2.17c 1.73–2.73 2.10c 1.58–2.56 Hemopneumothorax 3.21c 2.41–4.27 3.15c 2.33–4.27
None (reference group) 1.00 1.00 Fracture of extremities Yes 1.83c 1.47–2.29 1.74c 1.38–2.20 No (reference group) 1.00 1.00 Fracture of pelvis Yes 2.92c 2.10–4.06 2.92c 2.06–4.14 No (reference group) 1.00 1.00 Head injury Yes 4.30c 3.55–5.21 4.29c 3.49–5.27 No (reference group) 1.00 1.00 Spleen injury Yes 1.96b 1.24–3.10 1.83a 1.13–2.97 No (reference group) 1.00 1.00 Hepatic injury Yes 3.96c 2.87–5.45 4.39c 3.09–6.24 No (reference group) 1.00 1.00 Fracture of scapula Yes 0.46b 0.26–0.82 0.52a 0.29–0.94 No (reference group) 1.00 1.00 Heart injury Yes 5.17c 2.47–10.84 4.48c 2.02–0.98 No (reference group) 1.00 1.00 Diaphragm injury Yes 5.36c 2.10–13.65 3.16a 1.15–8.65 No (reference group) 1.00 1.00 Hospital characteristics Hospital level Medical center 1.58b 1.19–2.10 0.98 0.73–1.32 Regional hospital 1.77c 1.39–2.24 1.30a 1.02–1.67 District hospital (reference group) 1.00 1.00 ap⬍ 0.05. bp⬍ 0.01. cp⬍ 0.001. CI⫽ confidence interval; OR⫽ odds ratio.
GENERAL
characteristics in relation to 24-hour death, indicating significant relationships between 24-hour death and pa-tient age (p⬍ 0.001) and hospital accreditation level (p ⬍ 0.001).
Table 2 describes the distribution of the sampled patients by patient comorbidities. A total of 25.4%, 15.2%, 14.6%, and 5.6% had comorbidities of head injury, hemo-thorax, extremity fractures, and scapula fractures, respec-tively. Of 3,978 patients with hemothorax or hemopneu-mothorax, 26 patients (0.65%) had ruptured aorta. Twenty-four hour mortality was further associated with number of rib fractures (p ⬍ 0.001), pulmonary compli-cations (p⬍ 0.001), extremity fractures (p ⬍ 0.001), pelvis fractures (p ⬍ 0.001), head injury (p ⬍ 0.001), spleen injury (p ⫽ 0.003), hepatic injury (p ⬍ 0.001), scapula fractures (p⫽ 0.007), heart injury (p ⬍ 0.001), diaphrag-matic injury (p⬍ 0.001), and aortic rupture (p ⬍ 0.001).
Table 3provides the crude odds ratio (OR) estimates of the likelihood of 24-hour death, by patient and hospital characteristics. As expected, the odds of 24-hour death increased with patient age. Patients with pulmonary complications, extremity fractures, pelvis fractures, head injuries, spleen injury, hepatic injury, heart injury, and diaphragmatic injury had higher odds of 24-hour death than patients who did not.
Table 3also shows adjusted OR of 24-hour death by patient and hospital characteristics. The adjusted OR of 24-hour deaths increased with increasing patient age. Patients with six or more rib fractures were three times more likely to die within 24 hours after admission than patients with only 1 rib fracture (OR, 3.16; 95% confi-dence interval [CI], 1.18 to 8.51). The odds of 24-hour death for those patients experiencing hemopneumotho-rax (OR, 3.15; 95% CI, 2.33 to 4.27), extremity fractures (OR, 1.74; 95% CI, 1.38 to 2.20), pelvis fractures (OR, 2.92; 95% CI, 2.06 to 4.14), head injuries (OR, 4.29; 95% CI, 3.49 to 5.27), spleen injury (OR, 1.83; 95% CI, 1.13 to 2.97), hepatic injury (OR, 4.39; 95% CI, 3.09 to 6.24), heart injury (OR, 4.48; 95% CI, 2.02 to 0.98), or diaphragmatic injury (OR, 3.16; 95% CI, 1.15 to 8.65) were higher compared with patients who did not, after adjusting for other factors and clustering effect among particular hospitals. Interestingly, patients treated in regional hospitals were 1.30 times more likely to die within 24 hours than patients treated in district hospitals.
Comment
In the modern era, motor vehicles are widespread and the incidence of traffic continues to rise. Rib fractures have been reported as the most common disorder asso-ciated with chest trauma, and almost 70% of these pa-tients were hospitalized [7–9]. Our study explored the risk factors associated with 24-hour mortality after blunt chest trauma with fractured ribs resulting from motor vehicle accidents. We found that a total of 827 patients (4.4%) with traumatic rib fractures died within 30 days and 459 of these (55%) died within 24 hours. This is consistent with findings by Acosta and coworkers [5],
who reported that 70% of trauma patients died within the first 24 hours after admission.
In human populations, men are usually more active and are injured more frequently than women, even in different countries or cultures. Liman and coworkers[8]
in Turkey reported 1,053 men (70.6%) among 1,490 pa-tients with blunt chest injuries; Bergeron and associates
[10] in Canada showed 268 men (66.1%) among 405 patients with rib fractures; Kulshrestha and colleagues
[11] in Massachusetts documented that 1,359 chest trauma patients included 964 male (70.9%) and 395 fe-male (29.1%) patients. Consistent with the above reports, this study also shows that male patients account for 70.1% of all sampled patients in this category, although there is no difference in 24-hour mortality between sexes. The higher mortality rate among the elderly (ⱖ65 years of age) found by our study is consistent with the reports by Sirmali and colleagues[9]and Bergeron and cowork-ers[10]. However, the report by Bergeron and associates
[10] recorded that 72% of ensuing mortality occurred more than 72 hours after admission and was associated with pneumonia in older patients, whereas our study recorded deaths within 24 hours only. Our findings suggest the elderly have a higher risk of death even immediately after a motor vehicle accident.
We found that increasing numbers of fractured ribs are associated with a higher percentage of comorbidities (not shown in the tables). Our finding is in agreement with a study by Sirmali and associates[9], which also reported a relationship between number of fractured ribs and in-creased complication rates. In addition, Kulshrestha and colleagues[11] concluded that more than five rib frac-tures was adversely related to mortality after chest trauma. We likewise found that 24-hour mortality is associated with increased number of fractures. In partic-ular, patients with six or more rib fractures had more than three times the odds of 24-hour mortality than patients with only one rib fracture.
Blunt thoracic injury is almost always caused by the rapid deceleration of crashing in motor vehicle collisions. The pattern of injury sustained from direct impact may include fracture of the sternum, scapula, or vertebral column with hemothorax, pneumothorax, or both; ante-rior flail chest with cardiac and pulmonary contusion; fracture of extremities or pelvic or head injuries; and rupture of liver, spleen, or diaphragm. In the current study, head injuries (including fracture of skull or facial bones, cerebral laceration and contusion, and intracra-nial hemorrhage) occurred in 25.4% of patients. In addi-tion, similar to the 20% reported by Kulshrestha and coworkers[11], we found 24.6% of the sampled patients sustained hemothorax or pneumothorax. And in our study, 14.6% of traumatic rib fractures were associated with fractures of the extremities. These three leading associated injuries all were associated with increased 24-hour mortality.
Kulshrestha and associates[11, 12]found an incidence of 1.5% to 6% of cardiac injuries among chest trauma patients in a single unit. In our series, the occurrence of cardiac injuries (0.4%) was far lower. Their sampled
patients were selected from a single trauma center, which was more likely to admit severely ill patients in contrast to the nationwide population-based sample used in our study.
Diaphragm injuries increased the 24-hour mortality rate among patients with traumatic rib fractures, but the incidence was only 0.2% in our study—lower than the incidence of 2.3% to 5% reported in the literature[11, 13]. Reporting the incidence of cardiac and diaphragm inju-ries associated with chest trauma is not common and is usually reported by a single center [11–13]. The lower incidence found by our study may be explained by the fact that we used nationwide population-based data rather than data from a single medical center. In our study, patients with traumatic rib fractures associated with heart injuries, hepatic injuries, and head injuries and those who were older than 74 years of age initially had more than four times the mortality rate once a traffic accident happened. These seem to be the four leading factors causing death within 24 hours of admission.
Usually, flail chest is a serious problem in patients with rib fractures and has been associated with 11% to 40% mortality rate [9, 14 –16]. Flail chest causes paroxysmal chest movement and respiratory insufficiency and may lead to subsequent death. Among the 66 patients with flail chest in our study, 2 (3%) died within 24 hours after admission and 26 (39.4%) were managed with mechanical ventilation. Eighteen (69.2%) of these 26 patients had continuous mechanical ventilation for 96 consecutive hours or more. Our data also showed the patients with flail chest did not have an increased 24-hour mortality rate. This suggests patients with traumatic rib fractures and flail chest have no higher mortality rate than those without flail chest in the initial 24 hours after a traffic accident. In addition, patients with traumatic rib frac-tures associated with fracfrac-tures of the vertebral column or sternum did not have increased odds of 24-hour death. Interestingly, the patients with scapula fractures had a significant lower mortality rate in the first 24 hours. Scapular fractures may indicate the majority of the force of the traffic accident impacted the patient’s back with the scapula absorbing part of the force and protecting vis-ceral organs, accounting for lower initial rates of death.
In Taiwan, the northern district has the most abundant health-care resources compared with other areas, espe-cially the eastern region (accounting for only 2.6% of all patients). In our study, hospital location was not related to 24-hour mortality rate. In addition, the patients sent to medical centers had a lower 24-hour mortality rate than those sent to regional hospitals. But patients sent to district hospitals had also a lower 24-hour mortality rate than those sent to regional hospitals. “Prehospital selec-tion” may explain this pattern. In Taiwan, the drivers of emergency vehicles and emergency-care system staff, as well as families, may avoid sending patients with obvious severe injuries to district hospitals, with the result that fewer severely injured patients end up at district hospi-tals than regional hospihospi-tals, accounting for their lower 24-hour mortality rate.
It is also worth noting the effects of helmets, seat belts, and air bags on reducing risk of traumatic injury in motor vehicle accidents[17]. Although air bag deployment may increase the risk of upper and lower extremity injuries during traffic accidents [18 –20], air bag deployment is associated with approximately 25% to 30% mortality reduction [21, 22]. Information regarding vehicle types, use of seat belts, and deployment of air bags was unavail-able in our data set. However, most cars in Taiwan are equipped with air bags. The law also stipulates an NT$1,500 fine (about 50 US dollars) if a driver or front-seat passenger does not have the front-seat belt fastened. During the past decades, seat belts and air bags are considered to be significant contributors to the decreas-ing trend of mortality from motor vehicle collisions in some countries[17]. Furthermore, the mandatory motor-cycle helmet law was implemented in Taiwan since 1997. Helmets were found to significantly reduce the number of motorcycle-related head injuries by 33%[23]and lead to a 71% reduction in the risk of death caused by head and neck injuries[24].
A particular strength of this study is the use of two nationwide population-based data sets, allowing us to trace medical services received by sampled patients after traffic accidents. However, our findings need to be inter-preted within the context of three limitations. First, patients with severe injuries would be admitted and treated in hospitals. However, each hospital may have different criteria for patient admission. Second, the co-morbidity diagnoses, which rely totally on claims data reported by physicians or hospitals, may be less accurate than if all individuals were assessed through a single standardized procedure. Finally, information regarding type of vehicles, and seat belt and air bag use, as well as numbers of patients ejected or extricated from vehicles, was not available in the claims data set. The severity of organ injuries was not graded owing to the lack of such information in the current coding system of ICD-9.
We conclude that heart injuries, hepatic injuries, head injuries, and advanced age are the most important deter-minants of 24-hour mortality after traumatic rib fractures as a result of motor vehicle accidents. The presence of hemothorax or pneumothorax, fractures of the extremi-ties, pelvis fractures, spleen injuries, diaphragm injuries, or more than six ribs fractured also increased the risk of 24-hour mortality after chest trauma. A true profile of mortality associated with traumatic rib fractures should be useful for increasing efficacy of the emergency rescue system. Our study supplies a guide for identifying those at highest risk of death immediately after traumatic rib fractures as a result of motor vehicle accidents, allowing medical personnel to concentrate on these patients to improve the treatment outcomes.
References
1. LoCicero J, Mattox KL. Epidemiology of chest trauma. Surg Clin North Am 1989;69:15–9.
2. Ziegler DW, Agarwal NN. The morbidity and mortality of ribs fractures. J Trauma 1994;37:975–9.
GENERAL
3. Grimes OF. Nonpenetrating injuries to the chest wall and esophagus. Surg Clin North Am 1972;52:597– 609.
4. Shorr RM, Crittenden M, Indeck M, et al. Blunt thoracic trauma: analysis of 515 patients. Ann Surg 1987;206:200 –5. 5. Acosta JA, Yang JC, Winchell RJ, et al. Lethal injuries and
time to death in a level I trauma center. J Am Coll Surg 1998;186:528 –33.
6. Ceran S, Sunam GS, Aribas OK, et al. Chest trauma in children. Eur J Cardiothorac Surg 2002;21:57–9.
7. Calhoon JH, Grover FL, Trinkle JK. Chest trauma: approach and management. Clin Chest Med 1992;13:55– 67.
8. Liman ST, Kuzucu A, Tastepe AI, et al. Chest injury due to blunt trauma. Eur J Cardiothorac Surg 2003;23:374 – 8. 9. Sirmali M, TüRüt H, Topcu S, et al. A comprehensive
analysis of traumatic rib fractures: morbidity, mortality and management. Eur J Cardiothorac Surg 2003;24:133– 8. 10. Bergeron E, Lavoie A, Clas D, et al. Elderly trauma patients
with rib fractures are at greater risk of death and pneumo-nia. J Trauma 2003;54:478 – 85.
11. Kulshrestha P, Munshi I, Wait R. Profile of chest trauma in a level I trauma center. J Trauma 2004;57:567– 81.
12. Kulshrestha P, Das B, Jyer KS, et al. Cardiac injuries: a clinical and autopsy profile. J Trauma 1990;30:203–7. 13. Kish G, Kozloff L, Joseph WL, et al. Indications for early
thoracotomy in management of chest trauma. Ann Thorac Surg 1967;22:23– 8.
14. Thomas AN, Blaisdell FW, Lewis FR Jr, et al. Operative stabilization for flail chest after blunt trauma. J Thorac Cardiovasc Surg 1978;75:793– 801.
15. Richardson JD. Indications for thoracotomy in thoracic trauma. Curr Surg 1985;42:361– 4.
16. Freedland M, Wilson RF, Bender JS, et al. The management of flail chest injury: factors affecting outcome. J Trauma 1990;30:1460 – 8.
17. Cummins JS, Koval KJ, Cantu RV, Spratt KF. Risk of injury associated with the use of seat belts and air bags in motor vehicle crashes. Bull NYU Hosp Jt Dis 2008;66:290 – 6. 18. McGovern MK, Murphy RX Jr, Okunski WJ, Wasser TE. The
influence of air bags and restraining devices on extremity injuries in motor vehicle collisions. Ann Plast Surg 2000;44: 481–5.
19. Huelke DF, Moore JL, Compton TW, et al. Upper extremity injuries related to airbag deployments. J Trauma 1995;38: 482– 8.
20. Estrada LS, Alonso JE, McGwin G Jr, et al. Restraint use and lower extremity fractures in frontal motor vehicle collisions. J Trauma 2004;57:323– 8.
21. Braver ER, Ferguson SA, Greene MA, Lund AK. Reductions in deaths in frontal crashes among right front passengers in vehicles equipped with passenger air bags. JAMA 1997;278: 1437–9.
22. Crandall CS, Olson LM, Sklar DP. Mortality reduction with air bag and seat belt use in head-on passenger car collisions [see comment]. Am J Epidemiol 2001;153:219 –24.
23. Chiu WT, Kuo CY, Hung CC, Chen M. The effect of the Taiwan motorcycle helmet use law on head injuries. Am J Public Health 2000;90:793– 6.
24. Keng SH. Helmet use and motorcycle fatalities in Taiwan. Accid Anal Prev 2005;37:349 –55.