Offspring birth weight and risk of mortality from
diabetes in mothers
Chung-Yi Li,
1,2Fung-Chang Sung,
3Pi-Ching Hsieh,
1Ming-Der Lee,
4Tsung-Hsueh Lu,
5Hua-Fen Chen
6ABSTRACT
Background Mothers with lower birth weight (LBW) offspring have been found to be associated with cardiovascular disease (CVD) morbidity, which shares many risk factors with diabetes.
Aims To investigate the relation between offspring birth weight and maternal risk of mortality from diabetes. Methods A total of 1 400 383 singletons of primigravida registered in Taiwan between 1978 and 1987 were followed to the end of 2006. The offspring birth weight was assessed with and without standardisation for the gestational age of offspring. Cox model was used to estimate the HR of maternal diabetes mortality in relation to offspring birth weights.
Results Altogether, 812 (5.8%) mothers died of diabetes. Mothers with LBW (<2500 g) and
macrosomia (>4000 g) offspring were both at increased risks of mortality from diabetes with HR 1.76 (95% CI 1.46 to 2.19) and 2.86 (95% CI 2.32 to 3.53), respectively. Similar results were seen while birth weight was standardised for gestational age.
Conclusions This cohort study found that mothers with LBW and macrosomia offspring had an increased mortality risk of diabetes. This relationship could be attributable to the possible pathway of intergenerational effects or maternal insulin resistance due to
maladaptation to pregnancy.
INTRODUCTION
Epidemiological evidence has indicated a significant relation between mothers having low birth weight (LBW; <2500 g) infants and an elevated risk for cardiovascular disease (CVD).1This association has been commonly interpreted as the indicative of an intergenerational correlation between the birth weights of a mother and her offspring,2and of the
‘Barker’s early origin of adult disease hypothesis’.3
The association between maternal and offspring birth weights is well-established in a number of studies.4e7A woman born as small for gestational age (SGA) is 2e4 times more likely to deliver a SGA baby.6 7 Such intergenerational association prob-ably involves both environmental and genetic processes.7 Additionally, the Barker’s fetal programming hypothesis postulates that fetal under-nutrition usually limits fetal growth, which may in turn increase the cardiovascular disease (CVD) risk in adulthood.3
Apart from CVD mortality studies, previous studies also reported that bearing LBW offspring was related inversely to systolic blood pressure8 9 and levels of the inflammatory markers, such as interleukin 6 and C reactive protein concentration.8
These studies suggest that these women may be predisposed to upregulation of inflammation that has been found to be associated with increased CVD risk,10 which further substantiates the observed associations between offspring size at birth and maternal CVD mortality.
LBW and its components, idiopathic preterm delivery and intrauterine growth restriction, shared many risk factors with CVD and diabetes. These risk factors included obesity, cigarette smoking and hypertension.11 Additionally, previous studies also indicated that mother’s unsuccessful adaptation to the profound biological demands of pregnancy may result in not only growth restriction of the fetus but also maternal insulin resistance.2 9 12 It has been proposed that the reasons for maladaptation to pregnancy could involve both vascular disease and metabolic pathways.13 The aforementioned
study findings may lead to the speculation that women who had LBW offspring are at elevated risk for CVD and at a greater risk of metabolic disorders like diabetes. The associations between bearing LBW infants and risk of diabetes in mothers were scarcely investigated previously.5 14 Therefore, we used the national birth and death registry datasets of Taiwan to conduct a cohort analysis and to investigate the associations between offspring birth size and the risk of maternal mortality from diabetesda disease with an increasing public health importance worldwide.
METHODS
This study used a retrospective cohort design linking between the Taiwan Birth Registry (TBR) and Taiwan Death Registry (TDR). It is required by law that all live births and deaths in Taiwan must be registered within 10 days following the birth or death. Between 1978 and 1987, a total of 1 422 286 singletons from primigravida were registered in the TBR. We employed the Tuckey’s rule15
to exclude 21 903 (1.54%) records with possibly implausible birth weight for gestational age, leaving 1 400 383 singletons in the analysis.
Exposure measures of interest included preterm delivery (<37 completed weeks of gestation), LBW, macrosomia ($4000 g), SGA (smaller than the 10th percentile of the calendar sex-gestation-specific birth weight distribution) and large-for-gestational age (LGA; larger than the 10th percentile of the calendar sex-gestation-specific birth weight distri-bution). Outcome measures were all-causes mortality, diabetes mortality (underlying cause of death (UCOD) of 250 based on the International Classification of Disease 9th version, Clinical Modification (ICD-9-CM)) and deaths from other
1Department of Health Care
Management, National Taipei College of Nursing, Taipei, Taiwan
2Department of Public Health,
College of Public Health, China Medical University, Taichung, Taiwan
3
Graduate Institute of Environmental Health College of Public Health, China Medical University, Taichung, Taiwan
4
Graduate Institute of Long-Term Care, National Taipei College of Nursing, Taipei, Taiwan
5Graduate Institute of Public
Health, College of Medicine, National Cheng Kung University, Tainan, Taiwan
6Department of Endocrinology,
Far-Eastern Memorial Hospital, Taipei, Taiwan
Correspondence to Dr Hua-Fen Chen, Department of Endocrinology, Far Eastern Memorial Hospital, 21, Sec 2, Nan-Ya South Road, Panchiao 220, Taipei County, Taiwan; hfchen@mail.femh.org.tw Chung-Yi Li and Fung-Chang Sung contributed equally to this manuscript.
Accepted 26 February 2010 Published Online First 27 June 2010
metabolic and immunity disorders (ICD-9-CM: 240e279, excluding 250), which were obtained from TDR for 1978e2006. Due to mandatory registration of all deaths in Taiwan and all death certificates completed by physicians, the TDRs are also generally complete. Lu et al assessed the agreement between official coders and a panel of physicians on determining UCOD given the information of death certificates, and found that the agreement was substantial for cancer and CVD with Kappa statistics of 0.83 and 0.73, respectively, but was moderate for pulmonary disease.16
The potential confounders considered included year of delivery (10 y), maternal age at the time of delivery (<20, 20e24, 25e29, 30e34, $35 y), marital status (married, other-wise), educational level (elementary or less, junior high, senior high, college or more), employment status (actively employed, otherwise) and level of urbanisation for mother’s residential district. The information on potential confounders was obtained from the TBR. We categorised mother’s place of living into three levels of urbanisation (ie, metropolitan, satellite city or town, and rural area). The purpose of adjusting maternal socioeco-nomic background and urbanisation of living district was to remove the possible social and urban-rural differences in acces-sibility to medical care in Taiwan.
Wefirst calculated the cumulative mortality risk of diabetes according to various maternal characteristics, including year of delivery, age group, marital status, education level, employment status and urbanisation of residential area. We then used the Cox proportional hazard model without and with adjustment for potential confounders to calculate the crude and adjusted HRs of all-causes death, diabetes mortality and death from metabolic and immunity disorders other than diabetes associated with various exposure measures separately.
In performing the Cox proportional hazard regression anal-ysis, the index dates for all mothers were the dates of delivery. The study endpoint was the possible mortality from all causes, diabetes or other metabolic and immunity disorders encountered by the study mothers. If the mothers did not encounter any mortality before the end of follow-up (ie, 31 December 2006), they were considered censored on the last day of follow-up. For those who encountered mortality from causes other than deaths of interest, they were also censored on the date of death. We also performed log ( log) test and confirmed that proportionality between hazards is assumed for our data. The statistical anal-yses were performed with SAS V9.1. A p value <0.05 was considered statistically significant for hypothesis testing included in this study.
RESULTS
By the end of 2006, the minimum and maximum length of follow-up for the study subjects was 19.38 and 28.92 years, respectively, with a mean and SD of 23.94 and 3.23 years, respectively. The study cohort was observed for a total of 33 500 370 person-years. By the end of 2006, a total of 32 130 women died of all causes with a cumulative death risk of 22.9& and a mortality rate of 9.59 per 10 000 person-years. The correspondingfigures for death from diabetes were 0.58& and 0.24 per 10 000 person-years. Diabetes accounted for 2.53% of total deaths and was ranked the sixth leading cause of death after female breast cancer (ICD-9-CM: 174; 9.08%), multiple fracture of upper limbs (ICD-9-CM: 819; 8.05%), lung cancer (ICD-9-CM: 162;4.22%), cervical cancer (ICD-9-CM: 180;3.77%) and gastric cancer (ICD-9-CM: 151; 3.03%).
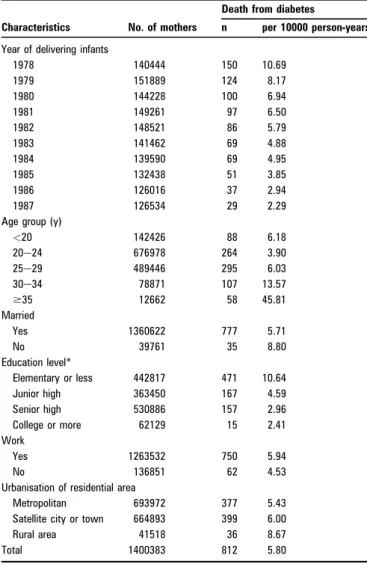
Table 1 shows death rates from diabetes according to selected mother’s characteristics. There was obvious variation in age-specific
mortality rates with a particularly highfigure noted in mothers aged 30 y or more (13.57 and 45.81 per 10 000 person-years for age group of 30e34 and $35 y, respectively). Unmarried and less- educated mothers also had higher mortality rates. On the other hand, employed mothers and mothers from less urbanised areas were both at increased mortality rates of diabetes postpartum.
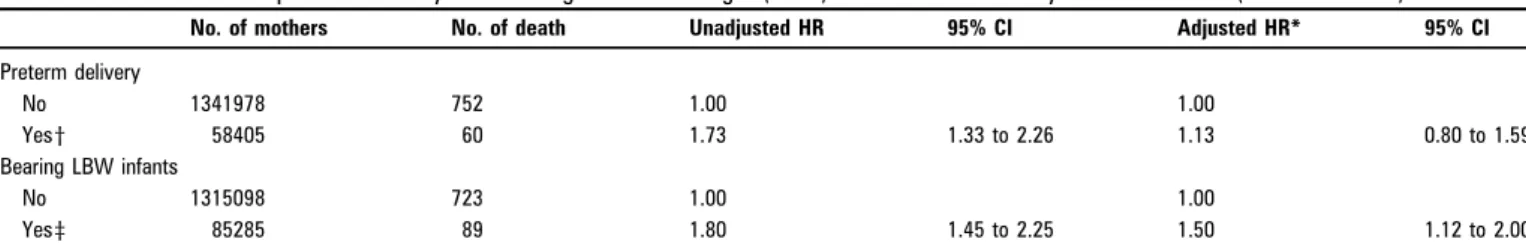
We found that bearing LBW infants was significantly associ-ated with an elevassoci-ated risk of all-causes mortality (HR 1.31, 95% CI 1.25 to 1.38) after taking potential confounders, including gestational age, into account. Additionally, we also noticed increased risk of mortality from metabolic and immunity causes other than diabetes, but such increased risk was compared to null statistically (adjusted HR 1.86, 95% CI 0.87 to 3.99) (data not shown in table). There was a significant crude relation between preterm delivery and risk of mortality from diabetes (HR 1.73, 95% CI 1.33 to 2.26). However, such significantly elevated RR estimate disappeared as the potential confounders, including infant’s birth weight, were considered in the analysis (HR 1.13, 95% CI 0.80 to 1.59). Similarly, preterm delivery did not show significantly independent influences on the risk of mortality from metabolic and immunity disorders other than diabetes (adjusted HR 0.91, 95% CI 0.34 to 2.40). On the other hand, bearing LBW infants was associated with a significantly increased risk of mortality from diabetes even after the potential Table 1 Death rate of diabetes according to selected maternal characteristics
Characteristics No. of mothers
Death from diabetes
n per 10000 person-years Year of delivering infants
1978 140444 150 10.69 1979 151889 124 8.17 1980 144228 100 6.94 1981 149261 97 6.50 1982 148521 86 5.79 1983 141462 69 4.88 1984 139590 69 4.95 1985 132438 51 3.85 1986 126016 37 2.94 1987 126534 29 2.29 Age group (y)
<20 142426 88 6.18 20e24 676978 264 3.90 25e29 489446 295 6.03 30e34 78871 107 13.57 $35 12662 58 45.81 Married Yes 1360622 777 5.71 No 39761 35 8.80 Education level* Elementary or less 442817 471 10.64 Junior high 363450 167 4.59 Senior high 530886 157 2.96 College or more 62129 15 2.41 Work Yes 1263532 750 5.94 No 136851 62 4.53 Urbanisation of residential area
Metropolitan 693972 377 5.43 Satellite city or town 664893 399 6.00 Rural area 41518 36 8.67 Total 1400383 812 5.80
confounders were taken into consideration (adjusted HR 1.50, 95% CI 1.12 to 2.00) (table 2).
Further analyses of offspring birth size in relation to diabetes mortality risk of mothers are presented in table 3. Compared to mothers with infants of 2500e3999 g, those who delivered LBW and macrosomia ($4000 g) infants were both at increased risks of diabetes mortality (HR 1.99, 95% CI 1.59 to 2.48 and HR 3.03, 95% CI 2.45 to 3.74, respectively). The significantly elevated HRs sustained after potential confounders were considered (adjusted HR 1.76, 95% CI 1.46 to 2.19 and HR 2.86, 95% CI 2.32 to 3.53, respectively). Almost identical results were found in the analysis when offspring birth weight was alterna-tively categorised into SGA (adjusted HR 1.24, 95% CI 1.01 to 1.53), appropriate gestational age (reference) and LGA (adjusted HR 2.77, 95% CI 2.27 to 3.38).
DISCUSSION
We found that mothers bearing smaller offspring were at elevated risk (by 76%) for diabetes mortality. However, preterm birth posed no significantly independent influence on the risk of diabetes mortality after potential confounders, including birth weight, was adjusted. Additionally, mothers bearing a macro-somia were also at increased risk of diabetes mortality with an even greater RR estimate (2.86-fold). The potential public health implication offindings from this study should not be overlooked since bearing LBW infants or macrosomia is not uncommon and diabetes has been one of the most prevalent non-communicable diseases globally.
The potential link between bearing a LBW infant and maternal risk of diabetes in later life was rarely studied. Davey Smithet al14tested the fetal insulin hypothesis by exploring the
associations between offspring birth characteristics and parental diabetes. The results showed a strong inverse association between offspring birth weight and maternal diabetes mortality with a weaker association among the fathers. The association observed in the father probably reflects common genetic factors that increase the risk of diabetes in the father and are also related to lower birth weight in the fetus. Given the greater strength of the inverse association observed in the mother, the study also argued that it is likely that, in addition to common genetic factors, intra-uterine environment could also play a part in the association between maternal diabetes mortality and offspring birth weight. Catov et al8 found that women who delivered a LBW infant were more insulin resistant, had greater fasting insulin levels, but had no greater risks of diabetes. However, this study was likely to be underpowered by recruiting only 446 women. Besides, the authors also argued that the presence of insulin resistance without diabetes mellitus may reflect a recent pathophysiological state that has not progressed.8
The association between bearing LBW infants and increased risk of diabetes mortality in mothers can be multifaceted. The
intra-uterine programming theory argued that women who themselves had poor growth and LBW tend to have smaller offspring.3 A number of studies did clearly demonstrate that women who were low birth weight themselves were at increased risk of delivering low birth weight offspring even after adjusting the confounding effects of pre-pregnant weight and height.6 7This effect may be related to maternal pelvic restric-tion, poor placenta grow, and fetal under-nutrition.17Moreover,
the association between slow fetal growth and increased CVD risk has been consistently replicated in epidemiological studies,1 with stronger evidence noticed if there is over-nutrition and accelerated growth in the postnatal period.12 Because women with LBW infants have greater fasting insulin level and insulin resistance,8 and because CVD shares many risk factors with diabetes, our findings might also result from intergenerational influences. Therefore, it can be interpreted as demonstrating the establishment during fetal development of processes with long-term consequences for metabolic function.17 Additionally, maternal genetic factors related to diabetes risk may also influ-ence offspring birth weight via effects on the intra-uterine environment. For example, maternal genes related to greater height of the mother could influence offspring birth weight via an effect on the intra-uterine environment.14
In addition to intergenerational influences, fetal programming theory and genetic influence, certain behaviour and clinical factors are also plausible reasons for the observed risk of diabetes in mothers with small offspring. For example, mothers who smoke are expected to be strongly related to lower offspring birth weight and also to have greater likelihood of developing diabetes in later adulthood. In addition, certain clinical attributes such as depressive disorder18were found to be associated with bearing
LBW infants. Many studies have concluded that depressive symptoms may increase the mortality risk of diabetes mainly due to the association of depression with poor adherence to diabetes treatment and poor glycaemic control,19and an increased risk for microvascular and macrovascular disease complications.
In Taiwan, all residents are covered by the National Health Insurance (NHI) programme, which has been introduced since March 1995. This state-run Bureau of NHI (BNHI) has contracted with 97% of hospitals as well as 90% of clinics all over the nation.20 The NHI provides free prenatal care and recommends 10 prenatal visits for all pregnant Taiwanese women in order to reduce the risk of poor pregnancy outcomes and to decrease the need for paediatric care after birth. A recent Taiwanese study, using Taiwan’s NHI data, found that women with a history of depressive disorders had fewer prenatal care visits (8.50 vs 9.17 time, p<0.001) but higher prenatal care costs.21 Fewer prenatal care visits have been found to be asso-ciated with higher risk of delivering LBW infants; and women who co-morbid with depression and diabetes are vulnerable to experience higher mortality risk of diabetes because of their poor Table 2 Associations of preterm delivery and bearing low birth weight (LBW) infants with mortality risk of diabetes (ICD-9-CM: 250)
No. of mothers No. of death Unadjusted HR 95% CI Adjusted HR* 95% CI Preterm delivery No 1341978 752 1.00 1.00 Yesy 58405 60 1.73 1.33 to 2.26 1.13 0.80 to 1.59 Bearing LBW infants No 1315098 723 1.00 1.00 Yesz 85285 89 1.80 1.45 to 2.25 1.50 1.12 to 2.00
*Based on Cox proportional hazard regression model with adjustment for year of delivery, maternal age at the time of delivery, marital status, education level, employment status, level of urbanisation for residential district and preterm delivery (or bearing low birth weight infant).
y<37 completed weeks of gestation. z<2500 g.
compliance to glucose control and treatment. Due to a lack of information on environmental, behavioural and clinical risk factors for diabetes, we were unable to evaluate the roles of these factors in explaining the offspring LBW and maternal diabetes association. There were only nine deaths from diabetes that occurred during the first 5 y postpartum, and all these nine deaths were from the non-LBW group. We re-analysed the data by excluding these nine deaths and yielded essentially the same risk estimates, suggesting that thefindings noted in this study should not merely be interpreted as most LBW infants were delivered by sick women.
In addition to LBW, this study also demonstrated that prior delivery of a macrosomia increased maternal mortality risk for diabetes. However, thisfinding is not surprising, as a high birth weight infant is likely to be born by mothers with gestational diabetes who in turn may be at greater risk of developing type 2 diabetes subsequently. A follow-up observational study noted that mothers of heavier babies were taller and more obese than mothers of lighter babies at the 8th year postpartum.22 Addi-tionally, increasing offspring birth weight may predict higher homeostasis model assessment for insulin resistance and meta-bolic syndrome in mothers after adjusting for offspring sex and birth order, maternal age and socioeconomic status,22which was consistent to ourfindings.
There are several methodological strengths to our study. First, this study was based on national registry data, which ensures the representativeness of the study cohort. Additionally, linkage between birth and death registries also effectively reduces the likelihood of loss to follow-up, which provides reassurance that the potential selection bias associated with this study is believed to be minimal. Second, the study cohort was consisted of more than 1.4 millions of mothers and was followed for up to nearly 30 y, which allows this study to have adequate statistical power to detect small effect-size of interest. Third, both birth and death registries have been considered valid and complete and we have excluded those births with implausible birth weight for gestation, which further provides reassurance on the accuracy of birth weight.
Our study also has limitations. First, we ascertained diabetes mortality solely from the information of UCOD registered in TDR. McEwenet al have indicated that diabetes was significantly less likely to be reported on the death certificates of decedents with diabetes dying of cancer, but is much more likely to be reported on the death certificates of diabetic individuals who die of cardio-vascular causes.23 Additionally, although all death certificates
were certified by physicians and the coding system was the same during the study period, the likelihood of erroneous recording of UCOD cannot be entirely excluded over such a long observational period. Nonetheless, the potential UCOD misclassification incurred would not be dependent on offspring birth weight, and
was likely to be non-differential, which may not be a valid argu-ment for the associations observed in this study. Second, we used mortality data rather than incidence data as the endpoint, which might entail certain degree of bias in the study. This is because previous Taiwanese studies have reported that LBW infants are less prevalent in urban areas than in rural area24; and other studies
showed diabetic patients have higher risks of both macrovascular complications and hip fracture that could be lethal.25 26
None-theless, we have attempted to control for this sort of potential confounding by adjusting for urbanisation of the study subject’s residential district. Third, although we had taken several potential confounders into account, like most previous studies using regis-tries of delivery data matched to mortality data,8our study still
had limited ability to comprehensively adjust for potential confounders such as lifetime smoking exposure and weigh gain. Fourth, the information on history of diabetes was not available for the study women who might have diabetes prepartum, which could have led to large babies and later diabetes mortality.
In conclusion, our results confirmed that women who had afirst-pregnancy complicated by LBW or macrosomia may both have significantly higher diabetes mortality risks. There is a need for future studies to illustrate the mechanism relevant to our findings. Additionally, our results may have important implica-tions for policies aimed at contemplating public health inter-ventions to improve fetal growth. Moreover, having a LBW Table 3 Associations of offspring birth weight with risk of mortality from diabetes (ICD-9-CM: 250) in mothers
N Death from diabetes Unadjusted HR 95% CI Adjusted HR* 95% CI Infant’s birth weight (g)
<2500 85285 89 1.99 1.59 to 2.48 1.76 1.46 to 2.19
2500e3999 1251176 623 1.00 1.00
$4000 63922 100 3.03 2.45 to 3.74 2.86 2.32 to 3.53 Infant’s gestation standardised birth weight
SGA 161084 105 1.31 1.06 to 1.61 1.24 1.01 to 1.53
AGA 1105175 551 1.00 1.00
LGA 83230 118 2.91 2.38 to 3.54 2.77 2.27 to 3.38
*Based on Cox proportional hazard regression model with adjustment for year of delivery, maternal age at the time of delivery, marital status, education level, employment status and level of urbanisation for residential district.
AGA, appropriate for gestational age; LGA, large for gestational age; SGA, small for gestational age;.
What this paper adds?
< Mothers with low birth weight (LBW) offsprings have been found to be associated with an increased risk of developing cardiovascular disease (CVD), which could be accounted by both genetic predisposition and intra-uterine environment. Because LBW and its components, idiopathic preterm delivery and intrauterine growth restriction, share many risk factors with CVD and diabetes, it has been proposed that LBW offspring could also be associated with an increased risk of diabetes in mothers. Nevertheless, such association has rarely been investigated.
< This large-scale cohort study found that mothers bearing LBW offspring may suffer from an increased risk of mortality from diabetes. Such a finding is consistent with the hypotheses that common genetic factors and intra-uterine environment may play a role in the association between offspring birth weight and maternal diabetes. Having a LBW infant can be used to mark women for intensive screening for diabetes and for appropriate intervention that can prevent or reduce the mortality risk of diabetes in mothers.
infant or macrosomia can be used to mark women for intensive screening for diabetes and for appropriate intervention that can prevent or reduce the mortality risk of diabetes in mothers.
Funding This work was supported by a grant from the National Scientific Council of Taiwan (NSC 96-2314-B-227-005-MY2).
Competing interests None.
Ethics approval This study was conducted with the approval of the Department of Health, Taiwan.
Provenance and peer review Not commissioned; externally peer reviewed.
REFERENCES
1. Smith GD, Sterne J, Tynelius P, et al. Birth weight of offspring and subsequent cardiovascular mortality of the parents. Epidemiology 2005;16:563e9. 2. Hennessy E, Alberman E. Intergenerational influences affecting birth outcome. I.
Birthweight for gestational age in the children of the 1958 British Birth Cohort. Paediatr Perinat Epidemiol 1998;12(Suppl 1):45e60.
3. Barker DJP. Fetal and infant origins of adult disease. London: British Medical Journal, 1992.
4. Magnus P, Gjessing H, Skronral A, et al. Paternal contribution to birth weight. J Epidemiol Community Health 2002;55:873e7.
5. Ramakrishnan U, Martorell R, Schroeder DG, et al. Role of intergenerational effects on linear growth. J Nutr 1999;129(Suppl 2S):544Se9S.
6. Sanderson M, Emanuel I, Holt VL. The intergenerational relationship between mother’s birthweight, infant birthweight and infant mortality in black and white mothers. Paediatr Perinat Epidemiol 1995;9:391e405.
7. Veena SR, Kumaran K, Swarnagowri MN, et al. Intergenerational effects on size at birth in South India. Paediatr Perinat Epidemiol 2004;18:361e70.
8. Catov JM, Newman AB, Roberts JM, et al. Association between infant birth weight and maternal cardiovascular risk factors in the health, aging, and body composition study. Ann Epidemiol 2007;17:36e43.
9. Lawlor D, Davey Smith G, Ebrahim S. Birth weight of offspring and insulin resistance in late adulthood: Cross sectional study. BMJ 2002;325:359e62.
10. Ridker P, Hennekens C, Buring J, et al. C-Reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med 2000;342:836e43.
11. Yajnik CS. The lifecycle effects of nutrition and body size on adult adiposity, diabetes and cardiovascular disease. Obes Rev 2002;3:217e24.
12. Davey Smith G, Hyppo¨nen E, Power C, et al. Offspring birth weight and parental mortality: prospective observational study and meta-analysis. Am J Epidemiol 2007;166:160e9.
13. Sattar I, Greer I. Pregnancy complications and maternal cardiovascular risk: Opportunities for intervention and screening? BMJ 2002;325:157e60.
14. Davey Smith G, Sterne JAC, Tynelius P, et al. Birth characteristics of offspring and parental diabetes: evidence for the fetal insulin hypothesis. J Epidemiol Community Health 2004;58:126e8.
15. Joseph KS, Kramer MS, Allen AC, et al. Implausible birth weight for gestational age. Am J Epidemiol 2001;153:109e23.
16. Lu TH, Chang HY, Hwu CM, et al. Comparison of official coders versus physician panel in assignment of underlying cause of death. J Formos Med Assoc 2001;100:365e9.
17. Bateson P, Barker D, Clutton-Brock T, et al. Developmental plasticity and human health. Nature 2004;430:419e21.
18. Steer RA, Scholl TO, Hediger ML, et al. Self-reported depression and negative pregnancy outcomes. J Clin Epidemiol 1992;45:1093e9.
19. Lustman PJ, Anderson RJ, Freedland KE, et al. Depression and poor glycemic control: a meta-analytic review of the literature. Diabetes Care
2000;23:934e42.
20. Chiang TL. Taiwan’s 1995 healthcare reform. Health Policy 1997;39:225e39. 21. Lin HC, Lin YJ, Hsiao FH, et al. Prenatal care visits and associated costs for
treatment-seeking women with depressive disorder. Psychiatr Serv 2009;60:1261e4.
22. Yajnik CS, Joglekar CV, Pandit AN, et al. Higher offspring birth weight predicts the metabolic syndrome in mothers but not fathers 8 years after delivery: the Pune Children’s Study. Diabetes 2003;52:2090e6.
23. McEwen LN, Kim C, Haan M, et al. Diabetes reporting as a cause of death: results from the Translating Research Into Action for Diabetes (TRIAD) study. Diabetes Care 2006;29:247e53.
24. Li CY, Sung FC. Socioeconomic inequalities in term low birth weight from singleton pregnancies in Taiwan. Public Health 2008;122:243e50.
25. Chen HF, Li CY. Effect-modifications by age and sex on the risks of coronary artery disease and revascularization procedures in relation to diabetes. Diabetes Res Clin Pract 2007;75:88e95.
26. Chen HF, Ho CA, Li CY. Increased risks of hip fracture in diabetic patients of Taiwan: A population-based study. Diabetes Care 2008;31:75e80.