T
aiwan's National Health Insurance Program (NHIP) began on March 1, 1995 to remove financial barriers to health care and to enhanceaccessibility to comprehensive medical care for all citizens. Many goals set for the nascent stage had been achieved 7 years after its inception. For
exam-Relationships between Length of Stay and Hospital
Characteristics under the Case-Payment System in
Taiwan: Using Data for Vaginal Delivery Patients
Herng-Ching Lin, PhD; Yu-Chi Tung
1, MHA; Chu-Chieh Chen
1,2, MHA;
Chao-Hsiun Tang, PhD
Background: Case payment has been implemented since the beginning of Taiwan's
National Health Insurance Program in 1995. This study selected patients undergoing a vaginal delivery to explore the relationships between maternal length of stay (LOS) and hospital characteristics under the case-payment sys-tem in Taiwan.
Methods: The National Health Insurance Research Database of 1999 from Taiwan's National Health Research Institutes was used in this study. In total, 5456 patients who underwent a vaginal delivery in 1999 meeting the selection cri-teria were drawn from the database. A multiple regression analysis was per-formed in which LOS was regressed against the variables of hospital level, hospital location, hospital ownership, and teaching status.
Results: The regression model indicated that hospital level, hospital ownership, and hospital location were significantly related to LOS after adjustment for patient age, principal procedure, and the presence of a secondary diagnosis. The LOS for patients undergoing a vaginal delivery in private hospitals was shorter than those in public and non-profit proprietary hospitals. Patients admitted to medical centers or regional hospitals were more likely to have a longer mean LOS in comparison with their counterparts admitted to district hospitals. The LOS for patients hospitalized in northern Taiwan tended to be significantly longer on average than those in central and southern Taiwan.
Conclusions: This study demonstrates that wide variations in LOS exist among hospitals in
Taiwan under the case-payment system. It is recommended that the Bureau of the National Health Insurance develop a national system to monitor cer-tain hospitals that have an unusually short LOS.
(Chang Gung Med J 2003;26:259-68)
Key words: case payment, length of stay, vaginal delivery.
From the Graduate Institute of Health Care Administration, Taipei Medical University, 1Graduate Institute of Health Care Organization, National Taiwan University, 2Department of Health Care Management, National Taipei College of Nursing, Taipei. Received: Jun. 25, 2002; Accepted: Jan. 23, 2003
Address for reprints: Assoc. Prof. Chao-Hsiun Tang, Graduate Institute of Health Care Administration, Taipei Medical University. 250, Wu-Hsing St., Taipei, Taiwan 110, R.O.C. Tel.: 886-2-2736-1661 ext. 3610; Fax: 886-2-2378-9788; E-mail: chtang@tmu.edu.tw
ple, at the end of December 2001, the coverage rate had reached 96.16%, up from 92% at the end of the inaugural year (Bureau of the National Health Insurance, BNHI, 2002). However, due to the dra-matic rise in medical expenses accompanying the expedited expansion of coverage rates and increased access to medical care, the NHIP was acknowledged to have gone into debt in 1999. In order to minimize deficits and to make better use of medical resources, the BNHI adopted more-efficient and economical strategies such as incessant expansion of the scope of diseases paid for by case payment to control medical expenditures.
Case payment, similar to diagnosis-related groups (DRGs) used in the US, has been implement-ed since the beginning of the NHIP. Under case pay-ment, hospitals are allowed to keep the discrepancy or must absorb the differential between their costs and the reimbursement rate established for providing patient care by the BNHI. Therefore, the case pay-ment system provides hospitals with financial incen-tives to discharge patients as quickly as medically feasible in order to obtain maximal profits. Studies have confirmed that implementation of DRGs led to significant decreases in the length of stay (LOS) for all DRGs in the US.(1) Similar to the US experience, the LOS for some case payment items also decreased after implementation of case payment in Taiwan.(2)
In addition to the reduction in LOS with the advent of DRGs, hospitals responded to the financial incentives created by third-party payers to different degrees as reflected in LOS data based on the US experience. Many studies have identified that wide variations in LOS exist among hospitals under a per-case-based payment system. For example, Leung et al. found that hospitals differed significantly in maternity LOS even after adjusting for the patient case mix.(3) Lutjens observed that wide variations in LOS existed among hospitals.(4) Specifically, studies have indicated that hospital characteristics such as hospital ownership, hospital location, teaching status, hospital size, and other factors can cause variations in LOS.(1,3,5-10)
Based on experience with DRGs, wide varia-tions exist in LOS among hospitals under a per-case-based payment system in the US. However, little research has been conducted to investigate the rela-tionships between LOS and such hospital character-istics as hospital type, hospital ownership, hospital
location, and hospital teaching status under imple-mentation of case payment in Taiwan. To explore the relationships between hospital characteristics and LOS may not only help hospital administrators understand the possible effects of case payment on hospitals, but may also help policy makers identify those hospitals in which patients are more likely to have shorter stays. There is an imperative need for investigations of hospital characteristics that may be associated with hospital LOS under the case-pay-ment system. Therefore, this study used patients undergoing a vaginal delivery to explore the relation-ships between LOS and hospital characteristics under the case-payment system in Taiwan. The reasons for selecting vaginal delivery as a target case payment item were that: (1) vaginal delivery is the most fre-quent cause of hospital admissions in Taiwan; (2) vaginal delivery was one of the first three diseases paid for on a case-payment basis; and (3) patients undergoing a vaginal delivery are described as being a fairly homogeneous group because of gender, age, and low complication or comorbidity rates compared with patients treated under other case-payment items.
METHODS
Database and subjects
This study used the National Health Insurance Research Database (NHIRD) of 1999, which was published by Taiwan's National Health Research Institutes. As to the sampling of the NHIRD, Taiwan's National Health Research Institutes used a systematic sampling method to randomly select a representative subgroup from the entire database due to the large number of inpatient and outpatient med-ical benefit claims in a year. The sampling bases of outpatient medical benefit claims and inpatient med-ical benefit claims were 0.2% and 5% of the entire database, respectively. The sampled subgroup was similar with regards to age, gender, and costs to those of the entire population.
In total, 8602 patients who underwent a vaginal delivery in 1999 meeting the selection criteria were identified on the basis of the case-payment code for vaginal delivery (0373A). After excluding patients who had a LOS of longer than 6 days (N=10), who were less than 15 years of age (N=10), who were over 40 years of age (N=20), and who were dis-charged from obstetrics and gynecology clinics
(N=3106), the remaining eligible sample size amounted to 5456 in the analysis. Since this study focused on the relationship between hospitals and patients undergoing a vaginal delivery, those patients who were discharged from obstetrics and genecology clinics were excluded from the study.
Variables
The dependent variable was maternity LOS in the hospital. This continuous variable was opera-tionalized as the time, in days, from patient admis-sion to the hospital until discharge. Hospital charac-teristics described by hospital level, hospital owner-ship, hospital location, and teaching status of hospi-tals were selected as independent variables. Hospital level was classified into medical center, regional hos-pital, and district hospital. Hospital ownership was recorded as 1 of 3 types: public (including veterans hospitals), non-profit proprietary, and private. Based on the site of division of the BNHI where hospitals claimed medical benefits, hospital location was divided into northern, central, southern, and eastern. The hospital teaching status was treated as a dichoto-mous category on the basis of whether or not a hos-pital was accredited as a teaching hoshos-pital by the Department of Health in 1999. The principal proce-dure codes for patients undergoing a vaginal delivery are 73.6 (episiotomy), 72.71 (a vacuum extraction with episiotomy), 73.59 (other manually assisted delivery), and others. Age and whether or not a sec-ondary discharge diagnosis was present were also included as control variables to adjust the LOS in the analysis. Patient age was used as a continuous vari-able. The variable of the presence of a secondary discharge diagnosis was used with intent to control whether a patient had complications or comorbidity because there is no severity index of illness currently available in Taiwan. The variable of the presence of a secondary discharge diagnosis was divided into the 2 categories of "yes" and "no".
Statistical methods
Statistical analysis was conducted using the Statistical Package for the Social Sciences (SPSS 10.0 for Windows, 1997, SPSS, Chicago, IL). Descriptive statistical analyses including the fre-quency, percentage, mean, and standard deviation were performed on all identified variables. A multi-ple regression analysis was also performed in which
LOS was regressed against the independent variables of hospital level, hospital ownership, hospital loca-tion, and whether or not a hospital was a teaching hospital. In the case of categorically independent variables, dummy variables were created to account for the effect that the variable might have on the response. Hospital level, hospital ownership, hospi-tal location, hospihospi-tal teaching status, principal proce-dure code, and whether or not a secondary discharge diagnosis was present were treated as sets of dummy variables, while district hospital, private hospital, northern hospital, non-teaching hospital, others (principal procedure code), and the presence of a sec-ondary discharge diagnosis were selected as refer-ence groups, respectively. The interaction variables of teaching status and hospital level, teaching status and hospital ownership, teaching status and hospital location, hospital level and hospital ownership, hos-pital level and hoshos-pital location, and hoshos-pital owner-ship and hospital location were also assessed in this multiple regression model. A 2-sided p value of ≤ 0.05 was required for statistical significance.
In addition, since severe multicollinearity leads to unreliable coefficient estimates and large standard errors in a multiple regression model, the effects of multicollinearity of the parameter estimates were also evaluated using a variance inflation factor (VIF). Glantz and Slinker stated that values of VIF exceeding 10 are a sign of serious multicollineari-ty.(11) Therefore, if the VIF of an independent vari-able was greater than 10 in this study, this varivari-able was dropped from the multiple regression model.
RESULTS
Descriptive analysis
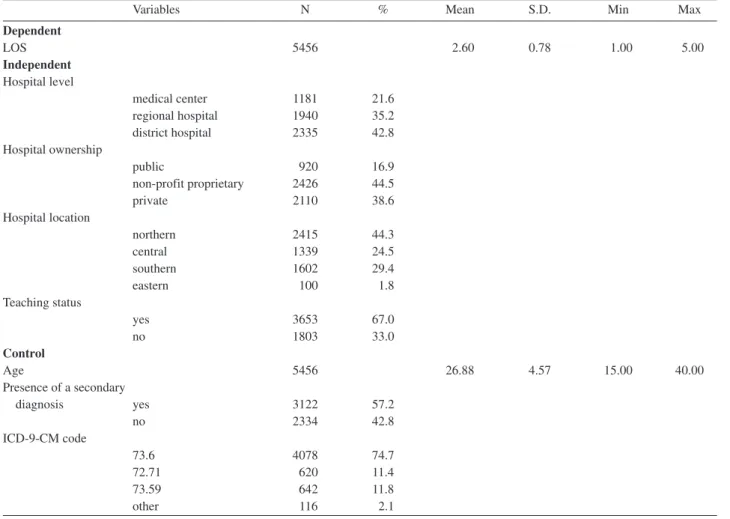
Frequency distributions and sample percentages were calculated for each variable. In the sample, patients ranged in age from 15 to 40 years (Table 1), with a mean age of 26.88 years and a standard devia-tion (SD) of 4.57 years. The maternity LOS of patients in the study, ranged form 1 to 5 days, with a mean LOS of 2.60 days and a SD of 0.78 days.
With regards to hospital level, the percentage of sample patients discharged from medical centers was 21.6%, from regional hospitals was 35.2%, and from district hospitals was 42.8%. As to hospital owner-ship, the majority of patients (44.5%) were admitted to non-profit proprietary hospitals, 16.9% to public
hospitals, and the remaining 38.6% to private hospi-tals. With respect to hospital location, 44.3% were admitted to hospitals located in northern Taiwan, fol-lowed by those admitted to hospitals located in southern Taiwan (29.4%). Only 1.8% of the sampled patients were admitted to hospitals located in eastern Taiwan. Among all sampled patients, 67% were treated in teaching hospitals, with the other 33% in non-teaching hospitals (Table 1).
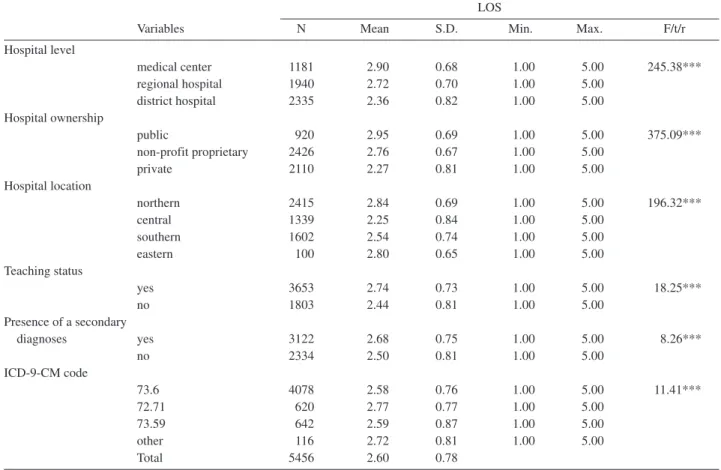
Unadjusted LOS for patients by hospital level, hospital ownership, hospital location, and hospital teaching status is shown in Table 2. ANOVA showed that LOS for patients hospitalized to undergo a vaginal delivery was significantly related to hospi-tal level ( p = 0.000), hospihospi-tal ownership ( p = 0.000), hospital location ( p = 0.000), teaching status ( p = 0.000), age ( p = 0.000), whether or not a
sec-ondary diagnosis was present ( p = 0.000), and princi-pal procedure ( p = 0.000).
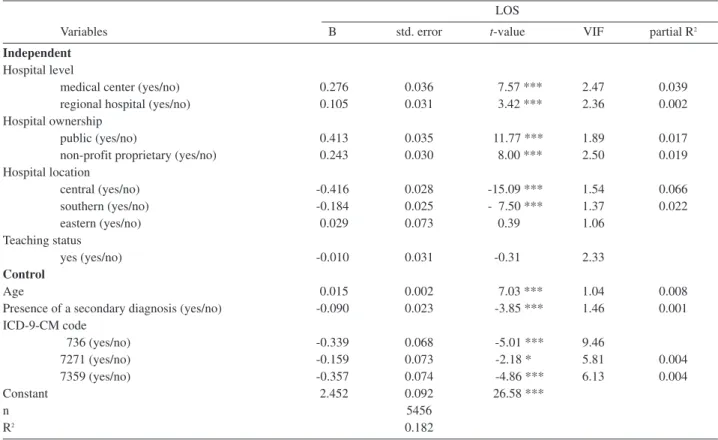
Multiple regression analysis
Multiple regression analysis revealed that 18.2% of the observed variation in LOS was explained with the help of independent variables (Table 3). The results show that variables of age ( p = 0.000), the presence of a secondary diagnosis ( p = 0.000), and being a medical center ( p = 0.000), regional hospital ( p = 0.000), public hospital ( p = 0.000), non-profit proprietary hospital ( p = 0.000), central hospital ( p = 0.000), and southern hospital ( p = 0.000) were significantly related to LOS.
That is, 2 dummy variables of hospital level were significantly positively associated with LOS after controlling for age and the presence of a
sec-Table 1. Characteristics of Sampled Patients and Hospitals
Variables N % Mean S.D. Min Max
Dependent LOS 5456 2.60 0.78 1.00 5.00 Independent Hospital level medical center 1181 21.6 regional hospital 1940 35.2 district hospital 2335 42.8 Hospital ownership public 920 16.9 non-profit proprietary 2426 44.5 private 2110 38.6 Hospital location northern 2415 44.3 central 1339 24.5 southern 1602 29.4 eastern 100 1.8 Teaching status yes 3653 67.0 no 1803 33.0 Control Age 5456 26.88 4.57 15.00 40.00 Presence of a secondary diagnosis yes 3122 57.2 no 2334 42.8 ICD-9-CM code 73.6 4078 74.7 72.71 620 11.4 73.59 642 11.8 other 116 2.1
ondary diagnosis. This shows that patients undergo-ing a vaginal delivery admitted to medical centers or regional hospitals were more likely to have a longer mean LOS in comparison with their counterparts admitted to district hospitals. Two dummy variables of hospital ownership were also significantly posi-tively associated with LOS. This reveals that those patients undergoing a vaginal delivery admitted to public hospitals or non-profit proprietary hospitals were apt to have a longer LOS on average than were patients undergoing a vaginal delivery admitted to private hospitals. Two dummy variables of hospital location were also observed to have significant nega-tive relationships with LOS. This indicates that lengths of stay for patients hospitalized to undergo a vaginal delivery in northern Taiwan tended to be sig-nificantly longer on average than those in central or southern Taiwan. In summary, private district hospi-tals located in central Taiwan had a shorter mean
LOS than did other kinds of hospitals.
In addition, this study found that the VIFs of interaction variables between teaching status and hospital level, teaching status and hospital owner-ship, teaching status and hospital location, hospital level and hospital ownership, and hospital level and hospital location were greater than 10. This suggests that the partial effects of these interaction variables on other independent variables cannot be ignored in the interpretation of the regression coefficients in this multiple regression model. Therefore, these interac-tion variables were dropped from the model.
DISCUSSION
The purpose of this study was to explore the relationships between maternal LOS and hospital characteristics for patients undergoing a vaginal delivery under the case-payment system in Taiwan.
Table 2. Relationships between LOS and Hospital Characteristics
LOS
Variables N Mean S.D. Min. Max. F/t/r
Hospital level medical center 1181 2.90 0.68 1.00 5.00 245.38*** regional hospital 1940 2.72 0.70 1.00 5.00 district hospital 2335 2.36 0.82 1.00 5.00 Hospital ownership public 920 2.95 0.69 1.00 5.00 375.09*** non-profit proprietary 2426 2.76 0.67 1.00 5.00 private 2110 2.27 0.81 1.00 5.00 Hospital location northern 2415 2.84 0.69 1.00 5.00 196.32*** central 1339 2.25 0.84 1.00 5.00 southern 1602 2.54 0.74 1.00 5.00 eastern 100 2.80 0.65 1.00 5.00 Teaching status yes 3653 2.74 0.73 1.00 5.00 18.25*** no 1803 2.44 0.81 1.00 5.00 Presence of a secondary diagnoses yes 3122 2.68 0.75 1.00 5.00 8.26*** no 2334 2.50 0.81 1.00 5.00 ICD-9-CM code 73.6 4078 2.58 0.76 1.00 5.00 11.41*** 72.71 620 2.77 0.77 1.00 5.00 73.59 642 2.59 0.87 1.00 5.00 other 116 2.72 0.81 1.00 5.00 Total 5456 2.60 0.78
The regression model indicated that hospital level, hospital ownership, and hospital location were sig-nificantly related to LOS after adjustment for patient age and the presence of a secondary diagnosis. The findings are consistent with those reported earlier that hospital characteristics cause variations in LOS after having adjusted for differences in patient char-acteristics in the US.(3,4,7,8)
Hospital ownership and LOS
With respect to hospital ownership, our observa-tion that patient LOS was expected to be shorter in private hospitals than in non-profit proprietary hospi-tals or in public hospihospi-tals under the case-payment system is in line with findings by Mawajdeh et al. in Jordan and by Thomas et al. and Wolinsky et al. in the US.(5,12,13) However, a recent study conducted by Huang and his colleagues failed to find a significant relationship between LOS and hospital ownership.(14) The possible reasons contributing to differences in
LOS caused by hospital ownership can be attributed to financial incentives created by the prospective payment system for hospitals, to a change in physi-cian behaviors, and to hospital efficiency.
Since hospitals are reimbursed a fixed amount for each treated patient based on codes rather than on actual resources used under case payment, hospitals have strong financial incentives to discharge patients as quickly as medically feasible; this is especially true for private hospitals.(15) Unlike public hospitals and non-profit proprietary hospitals financially sup-ported by government funding or philanthropic dona-tions, private hospitals have to seek any feasible means to increase revenues in order to stay competi-tive in the healthcare market. Consequently, private hospitals inevitably tend to shorten patients’ LOS on the basis of financial considerations regardless of their health status upon discharge. The gray zones of medical judgments concerning the appropriate tim-ing of patient discharge provide many opportunities
Table 3. LOS Regression Results
LOS
Variables B std. error t-value VIF partial R2
Independent
Hospital level
medical center (yes/no) 0.276 0.036 7.57 *** 2.47 0.039 regional hospital (yes/no) 0.105 0.031 3.42 *** 2.36 0.002 Hospital ownership
public (yes/no) 0.413 0.035 11.77 *** 1.89 0.017
non-profit proprietary (yes/no) 0.243 0.030 8.00 *** 2.50 0.019 Hospital location central (yes/no) -0.416 0.028 -15.09 *** 1.54 0.066 southern (yes/no) -0.184 0.025 - 7.50 *** 1.37 0.022 eastern (yes/no) 0.029 0.073 0.39 1.06 Teaching status yes (yes/no) -0.010 0.031 -0.31 2.33 Control Age 0.015 0.002 7.03 *** 1.04 0.008
Presence of a secondary diagnosis (yes/no) -0.090 0.023 -3.85 *** 1.46 0.001 ICD-9-CM code 736 (yes/no) -0.339 0.068 -5.01 *** 9.46 7271 (yes/no) -0.159 0.073 -2.18 * 5.81 0.004 7359 (yes/no) -0.357 0.074 -4.86 *** 6.13 0.004 Constant 2.452 0.092 26.58 *** n 5456 R2 0.182 *p < 0.05; **p < 0.01; ***p < 0.001.
for profitability by private hospitals.
Physicians have also perceived increased finan-cial pressures from hospital administrators to offer the least-expensive medical procedures after the implementation of case payment.(16) This pressure has forced physicians to change their practice behav-iors in a way favorable to a hospital’s finances. That the changes in physician practice patterns can result in variations in LOS was also confirmed by the find-ings of List et al.(17)and Fortney et al.(18)
Aside from the reasons discussed above, hospi-tal efficiency also plays an important role in LOS. Brooks et al. indicated that providing more-efficient care is one of the major factors decreasing LOS.(19) Many studies concerning the relationships between hospital ownership and efficiency have been con-ducted in Taiwan. They have all consistently report-ed that private hospitals are more efficient than pub-lic hospitals in providing a range of medical care.(20,21) The convergent findings provide evidence that the low efficiency in public hospitals has led to longer LOSs under case payment in Taiwan. Efficiency in providing medical care is considered an important predictor of average LOS in a hospital.
Hospital Level and LOS
As expected, patients admitted to medical cen-ters and regional hospitals had a longer average LOS than did patients admitted to district hospitals. This can partly be explained by medical centers and regional hospitals tending to receive a relatively high proportion of patients suffering from more-serious illnesses than do district hospitals. Although advanced adjustments were made in this study for patients who had a secondary discharge diagnosis, there were no means to assure that the sampled patients all had the same unmeasured severity of ill-ness. Horn et al. reported that severity-adjusted DRGs explained 61% of the variability in resource use; a higher severity of illness undoubtedly results in a longer hospital stay.(22)
This can also partly be attributed to patient dumping. Once a hospital identifies that a pregnant woman is unprofitable, it will transfer such a patient to another hospital. Schlesinger et al. described the phenomenon of "the transfers of patients from the treating hospital to other healthcare providers solely on economic grounds" with the term "patient dump-ing".(23) Patient dumping might lead to an average
longer LOS in medical centers compared to district hospitals.
Teaching Status and LOS
This study also reveals that there was no signifi-cant relationship between LOS and whether a hospi-tal was a teaching hospihospi-tal for patients undergoing a vaginal delivery. This indicates that patients under-going a vaginal delivery stayed in teaching hospitals the same amount of time as in non-teaching hospi-tals. This result is not consistent with the finding of Rosenthal et al. that risk-adjusted LOS was 9% lower among patients in major teaching hospitals rel-ative to non-teaching hospitals.(7) A possible expla-nation may be that teaching hospitals have seriously ill patients, but due to their good management strate-gies such as implementation of clinical pathways or evidence-based medicine, the average length of time patients need to recover in teaching hospitals is almost the same as that in non-teaching hospitals. Many studies have supported that the implementa-tion of clinical pathways is related to reduced LOSs.(24-26) Further research using patients treated under other case-payment items is needed to clarify the relationship between LOS and the teaching status of hospitals.
Hospital Location and LOS
Another noteworthy finding is that patients admitted to hospitals located in central or southern Taiwan had shorter LOSs than did patients admitted to hospitals located in northern Taiwan. One possi-ble explanation is that there is a high density of hos-pitals concentrated in northern Taiwan compared to central or southern Taiwan. For example, 4300 of 16,168 hospitals and clinics in Taiwan are located in Taipei City and Taipei County (Department of Health, 2000). Competitive pressures may encour-age hospitals in northern Taiwan to accommodate patient preferences for longer LOSs. Otherwise, they may be faced with loss of patients or be forced to close because of failure to provide the most cost-effective treatments. This postulation is supported by the finding of Robinson et al. that competitive pressures lead to longer LOSs.(27)
Overall, the power of the data used in this study is approximate to 1. Therefore, we are able to reject the null hypothesis when it is false. In other words, very small differences could reach statistically
sig-nificance in the analyses used in this study.
Conclusions
Traditional cost-based reimbursement was blamed for wide variations among hospitals for treat-ing similar diagnoses. However, this study demon-strates that wide variations in LOS still exist among hospitals in Taiwan under the financial incentives offered by the case-payment system. Proprietary hospitals and district hospitals have significantly shorter LOSs than do public hospitals and medical centers. Concerns have been raised about whether the overall quality of hospital care for inpatients has declined due to the short LOSs in proprietary hospi-tals and district hospihospi-tals. Therefore, it is recom-mended that the BNHI develop a national system like peer review organizations in the US to monitor the discharge status of patients whose care is paid for under case payment and to oversee certain hospitals which have unusually short LOSs.
Limitations
There are several limitations to this study. First, the findings of this study are limited to patients undergoing a vaginal delivery, so they cannot be gen-eralized to other case-payment disease items. Further research using other case payment items is needed to explore the relationships between LOS and hospital characteristics. Second, this study was designed as a cross-sectional study rather than a lon-gitudinal study, so cause-effect relationships cannot be determined. Future research should focus on a longitudinal study to further explore the relationship between LOS and hospital characteristics. Finally, patient identification information is not released to the public in this database for confidentiality con-cerns, and this prevents researchers from exploring the relationships between maternity LOS and infant outcomes. Further research is needed to explore the possible effects of a reduction in maternity LOS on the health status of infants.
Acknowledgements
This study is based in part on data from the National Health Insurance Research Database pro-vided by the Bureau of National Health Insurance, Department of Health and managed by National Health Research Institutes, ROC. The interpretations
and conclusions contained herein do not represent those of the Bureau of National Health Insurance, Department of Health, or the National Health Research Institutes, ROC.
REFERENCES
1. Lave JR, Frank RG. Effect of the structure of hospital payment on length of stay. Health Serv Res 1990;25:327-47.
2. Chiang HC. Construction of physician performance model under case payment and its application on clinical pathway variance control. M.A. Thesis; Taipei Medical University, Taipei, Taiwan. 2001.
3. Leung LM. Hospital- and patient-related characteristics determining maternity length of stay: a hierarchical linear model approach. Am J Public Health 1998;88:377-81. 4. Lutjens LR. Determinants of hospital length of stay. J
Nurs Adm 1993;23:14-8.
5. Yuan Z, Cooper GS, Einstadter D, Cebul RD, Rimm AA. The association between hospital type and mortality and length of stay: a study of 16.9 million hospitalized Medicare beneficiaries. Med Care 2000;38:231-45. 6. Thomas JW, Bates EW, Hofer T, Pekins A, Foltz-Murphy
N, Webb C. Interpreting risk-adjusted length of stay pat-terns for VA hospitals. Med Care 1998;36:1660-75. 7. Rosenthal GE, Harper DL, Quinn LM, Cooper GS.
Severity-adjusted mortality and length of stay in teaching and nonteaching hospitals. Results of a regional study. JAMA 1997;278:485-90.
8. Rissanen P, Aro S, Paavolainen P. Hospital- and patient-related characteristics determining length of hospital stay for hip and knee replacements. Int J Technol Assess Health Care 1996;12:325-35.
9. Shwartz M, Iezzoni LI, Ash AS, Mackiernan YD. Do severity measures explain differences in length of hospital stay? The case of hip fracture. Health Serv Res 1996;31:365-85.
10. Tielsch JM, Parver LM. Determinants of hospital charges and length of stay for ocular trauma. Ophthalmology 1989;97:231-7.
11. Glantz SA, Slinker B. Applied regression & analysis of variance.2nd ed, McGraw-Hill, Inc, 2001
12. Mawajdeh S, Hayajneh Y, al-Qutob R. The effect of type of hospital and health insurance on hospital length of stay in Irbid, North Jordan. Health Policy Plan 1997;2:166-72. 13. Wolinsky FD, Coe RM, Mosely RR. Length of stay in the
VA. Long-term care in short-term hospitals. Med Care 1987;25:250-3.
14. Huang ZJ, LaFleur BJ, Chamberlain JM, Guagliardo MF, Joseph JG. Inpatient childhood asthma treatment: rela-tionship of hospital characteristics to length of stay and cost: analyses of New York State discharge data, 1995. Arch Pediatr Adolesc Med 2002;156:67-72.
15. Friedman B, Shortell S. The financial performance of selected investor-owned and not-for-profit system hospi-tals before and after Medicare prospective payment. Health Serv Res 1988;23:237-67.
16. Lin HC, Amidon RL. Use factor analysis to identify diffi-culties in implementing a case payment reimbursement system in Taiwan. Chin Med J 2001;64:629-40.
17. Badham J, Brandrup J. Length of stay comparisons for private and public hospitals. Aust Health Rev 2000;23:162-70.
18. Brooks AD, Marcus SG, Gradek C, Newman E, Shamamian P, Gouge TH, Pachter HL, Eng K. Decreasing length of stay after pancreatoduodenectomy. Arch Surg 2000;135:823-30.
19. Fortney JC, Booth BM, Smith GR. Variation among VA hospitals in length of stay for treatment of depression. Psychiatr Serv 1966;47:608-13.
20. Shih KS, Lo JC, Chen KL. A study on the efficiency dif-ference between public and private general hospitals. Taiwan Public Health Journal 1996;15:469-82.
21. Lo JC, Shih KS, Chen KL. Technical efficiency of the general hospitals in Taiwan--an application of DEA. Economic Journal 1996;24:375-96.
22. Horn SD, Horn RA, Sharkey PD, Chambers AF. Severity of illness within DRGs. Homogeneity study. Med Care 1986;24:225-35.
23. Schlesinger M, Dorwart R, Hoover C, Epstein S. The determinants of dumping: a national study of economical-ly motivated transfers involving mental health care. Health Serv. Res 1997;32:561-90.
24. Huerta S, Heber D, Sawicki MP, Liu CD, Arthur D, Alexander P, Yip I, Li ZP, Livingston EH. Reduced length of stay by implementation of a clinical pathway for bariatric surgery in an academic health care center. Am Surg 2001;67:1128-35.
25. Wazeka A, Valacer DJ, Cooper M, Caplan DW, DiMaio M. Impact of a pediatric asthma clinical pathway on hos-pital cost and length of stay. Pediatr Pulmonol 2001;32: 211-6.
26. Pritts TA, Nussbaum MS, Flesch LV, Fegelman EJ, Parikh AA, Fischer JE. Implementation of a clinical pathway decreases length of stay and cost for bowel resection. Ann Surg 1999;230:728-33.
27. Robinson JC, Luft HS, McPhee SJ, Hunt SS. Hospital competition and surgical length of stay. JAMA 1988; 259:696-700.
1,2 1 1999 5456 (ܜطᗁᄫ 2003;26:259-68) ᄂΔᗁጯ̂ጯ ᗁચგநրၱࡁտٙĂ1έ៉̂ጯ ᗁᒚ፟ၹგநࡁտٙĂ2έΔ᜕நጯੰ ᗁ᜕გநր צ͛͟ഇĈϔ઼91ѐ6͡25͟ćତצΏྶĈϔ઼92ѐ1͡23͟Ą ৶פ٩ОώĈ഼፦ᖤҁरĂᄂΔᗁጯ̂ጯ ᗁચგநրၱࡁտٙĄ110έΔξӓᎸූ250ཱི Tel.: (02)27361661ᖼ3610; Fax: (02)23789788; E-mail: chtang@tmu.edu.tw